Abstract
Introduction and importance
Cecal bascule is a rare form of a cecal volvulus characterized by an anterior and superiorly displaced cecum in turn causing compression of the ascending colon that can result in a large bowel obstruction. We report a case of cecal bascule in a newly postpartum patient, with emphasis on clinical presentation, radiologic findings and treatment.
Case presentation
A 37-year-old female who underwent an uncomplicated c-section and bilateral salpingectomy developed severe abdominal pain, vomiting, and peritonitis 12 h after surgery. A computerized tomography of the abdomen and pelvis revealed a dilated and superiorly displaced cecum. The diagnosis of cecal bascule was confirmed intraoperatively and a right hemicolectomy was performed. The patient recovered appropriately and was discharged on postoperative day six.
Discussion
Cecal bascule is the rarest form of cecal volvulus. In the context of obstetrics and gynecology, it has mostly been mentioned perioperatively after cesarean, but was also reported in an antepartum patient. It usually occurs in patients with redundant or mobile cecum, which is a result of incomplete fixation of the cecum to the retroperitoneum during embryogenesis. Other risk factors include recent surgery, previous abdominal surgery, ileus, chronic constipation, and distal colonic obstruction. An association has also been shown with pregnancy or the postpartum abdomen and is hypothesized to be due to mass effect.
Conclusion
Cecal bascule is a serious entity requiring a high index of suspicion and warranting greater awareness in the post-natal patient. Clinical diagnosis, prompt imaging, and surgery are important to avoid bowel ischemia and perforation.
Keywords: Postpartum care, Gastrointestinal disorders, Surgery, Case report
Highlights
-
•
Any patient with a redundant cecum who undergoes delivery could potentially be at risk of developing a cecal bascule.
-
•
The importance of clinical diagnosis as well as prompt imaging in the post-natal patient with obstructive symptoms.
-
•
A right hemicolectomy is the gold standard in the treatment, whereas a cecopexy or cecostomy tube can be used in unstable patients.
1. Introduction
Cecal bascule is a rare form of a cecal volvulus characterized by an anterior and superiorly displaced cecum in turn causing compression of the ascending colon that can result in a large bowel obstruction [1], [2]. Bascule derives from French, meaning ‘seesaw’, or counterbalanced bridge [3]. It usually occurs in patients with redundant or mobile cecum, which allows for the anterior and superior displacement of the cecum. It accounts for 0.01% of adult large bowel obstructions, and with a competent ileocecal valve can lead to a closed loop obstruction with the associated risk of ischemia, perforation, and sepsis [4]. There seems to be an association of post-operative state with development of a cecal bascule including after cardiac surgery [4], [5], ventral hernia repair [6], and pelvic surgery [7]. This case report has been reported according to the SCARE checklist in 2020 [8].
2. Case presentation
Our patient was a 37-year-old multiparous LatinX female with a normal BMI, who presented at 36 weeks 6 days gestation for a scheduled cesarean section for suspected focal placenta accreta and bilateral salpingectomy for undesired future fertility. She had one prior spontaneous abortion and three previous cesarean sections (c-section). Her pregnancy had been complicated by ultrasonic findings suggesting morbid placentation. Prior to her surgery, she received a course of late preterm antenatal corticosteroids. She underwent an uncomplicated repeat c-section as well as bilateral salpingectomy. A moderate degree of serosal adhesions to the anterior abdominal wall required sharp dissection. Bowel adhesions were not present. Inspection of the adnexa revealed grossly normal fallopian tubes and ovaries. The hysterotomy was repaired in situ, as was the salpingectomy. The bowel protruded into the field once during the right salpingectomy but was gently and successfully pushed away. The cecum was not visualized during the procedure. Following the surgery, she was moved to the postpartum floor.
Twelve hours after her operation the patient became nauseated, her abdomen became distended, and she reported severe generalized abdominal pain. An abdominal radiograph was obtained which demonstrated air fluid levels concerning for an obstruction or ileus (Fig. 1). She was made nil per os, started on intravenous hydration, and a general surgery consultation was placed. Upon examination the patient had a distended abdomen with generalized tenderness to palpation as well as rebound and guarding. Her vital signs were within normal limits. Laboratory evaluation revealed a leukocytosis to 18,200 k/μL, a lactic acidosis to 3.6 mmol/L, and a hemoglobin of 9.4 g/dL. A nasogastric tube was placed with immediate return of 800 cc of bilious fluid and an urgent computerized tomography (CT) of the abdomen and pelvis was performed. The CT scan demonstrated decompressed small bowel with cecal dilation up to 10.4 cm and superior displacement of the cecum without pneumatosis, concerning for a cecal bascule (Fig. 2). Given the patient's worsening symptoms and concerning CT scan findings, she was taken to the operating room, roughly 16 h after her index operation, for urgent abdominal exploration.
Fig. 1.
Two-view abdominal radiograph showing markedly dilated colon.
Fig. 2.
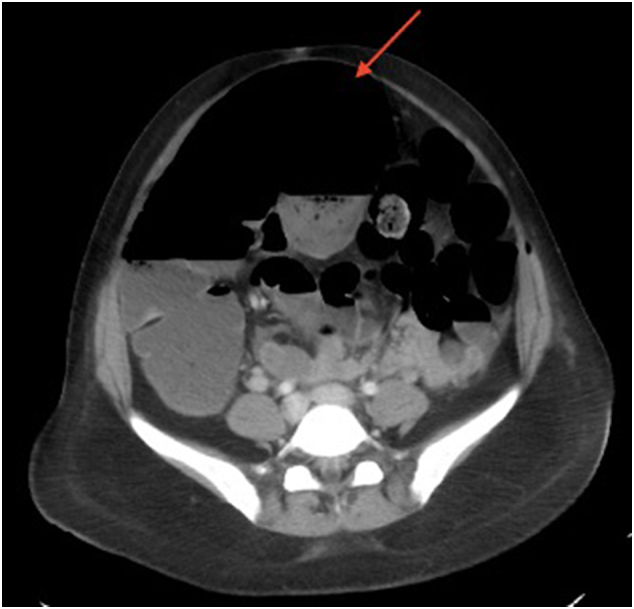
Computerized tomorgraphy (CT) scan of the abdomen and pelvis showing cecal dilation and superior displacement of the cecum (red arrow), concerning for cecal bascule.
Upon laparotomy, a dilated cecum with anterior and superior displacement was found, consistent with a cecal bascule (Fig. 3). The cecum and ascending colon were edematous, injected, and appeared dusky with a localized 3-cm area of necrosis without frank perforation. We elected to perform a right hemicolectomy. Using gastrointestinal (GIA) stapler loaded with a 60 mm blue load the ileum was transected 10 cm proximal to the ileocecal valve. The colon was transected at the level of the transverse colon proximal to the right branch of the middle colic. The mesentery was taken with a cautery. An ileocolic anastomosis was created with a 60 mm linear GIA stapler and the common enterotomy was closed with a running PDS suture. The remainder of the abdomen was explored without any abnormal findings. Post operatively, the patient did well with advancement of her diet upon return of GI function. She was discharged on postoperative day 6. Informed consent was obtained from the patient for this study and patient anonymity was preserved.
Fig. 3.
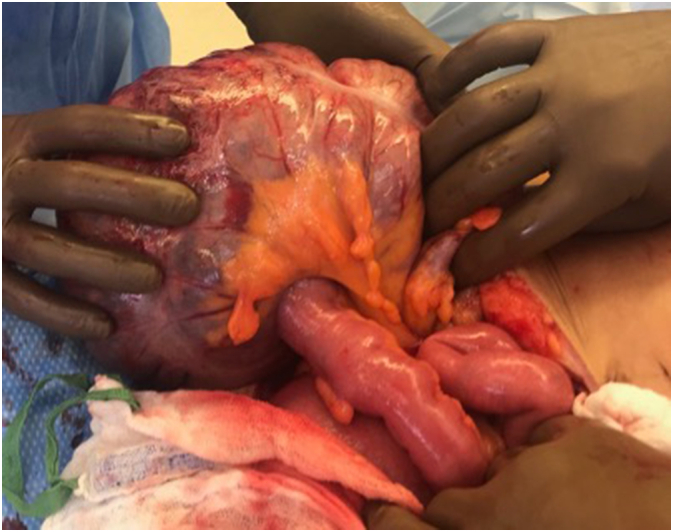
Intraoperative findings of a dilated, superiorly displaced, and partially ischemic cecum.
3. Discussion
First mentioned in 1899, cecal bascule is the rarest form of cecal volvulus, described mostly through case reports in the literature and one systematic review [2]. In the context of obstetrics and gynecology, it has mostly been mentioned perioperatively after cesarean [3], [9], [10], but was also reported in an antepartum patient [4]. It usually occurs in patients with redundant or mobile cecum, which is a result of incomplete fixation of the cecum to the retroperitoneum during embryogenesis [5], [6]. Other risk factors include recent surgery, previous abdominal surgery, ileus, chronic constipation, and distal colonic obstruction [4], [6]. An association has also been shown with pregnancy or the postpartum abdomen and is hypothesized to be due to mass effect [1].
Most cecal bascule reports found in the literature are case reports (Table 1). There have been a few reports of cecal bascule after c-section [3], [9], [10]. During a c-section, the uterus can be exteriorized to facilitate additional procedures, control of bleeding, and hysterotomy closure. In this case, however, the uterus was not exteriorized, suggesting that in patients with a redundant cecum, a sudden change in the spatial constraints of the pelvis can predispose them to developing cecal bascule. Physiologically, the uterus markedly involutes following delivery, resulting in a significant void in the abdomen, in a very short period of time. Any patient, therefore, with a redundant cecum at baseline who undergoes delivery- either vaginal or via cesarean- could potentially be at risk of developing a cecal bascule. Similarly, patients who undergo hysterectomy may also be at risk.
Table 1.
Review of the literature.
| Author | Country | Year | Type of study | N | Previous surgery | Surgery performed |
|---|---|---|---|---|---|---|
| Bobrof et al. [11] | USA | 1972 | Case report | 2 | None | Cecopexy (1), cecal decompression (1) |
| Chinoy et al. [12] | USA | 1984 | Case report | 1 | Appendectomy | Cecopexy |
| Fanning et al. [10] | USA | 1988 | Case report | 1 | Cesarean section | Cecostomy and cecopexy |
| Pousada et al. [13] | USA | 1992 | Case report | 1 | No previous surgery; previous chest wall trauma | Cecostomy |
| Rozycki et al. [14] | USA | 2001 | Case report | 1 | No previous surgery; 3° burns to 45% of TBSA | Right colectomy |
| Thangasamy et al. [3] | Australia | 2010 | Case report | 1 | Cesarean section | Right colectomy |
| Nwanguma et al. [15] | USA | 2011 | Case report | 1 | Previous Ogilvie's syndrome | Right colectomy |
| Lazar et al. [16] | USA | 2012 | Case report | 1 | Laparoscopic Nissen fundoplication | Cecopexy and cecal decompression |
| Veigel et al. [7] | USA | 2012 | Case report | 1 | Hysterectomy | Right colectomy |
| Datta et al. [17] | USA | 2012 | Case report | 1 | Cesarean section | Right colectomy |
| Kim et al. [6] | USA | 2013 | Case report | 1 | Lap Ventral hernia repair | Right colectomy |
| Makarawo et al. [18] | USA | 2014 | Case report | 1 | Hysterectomy | Cecopexy |
| Ramsingh et al. [19] | United Kingdom | 2014 | Case report | 1 | None | Right colectomy |
| Reznichenko et al. [20] | USA | 2015 | Case report | 1 | Recurrent ventral hernia | Right colectomy |
| Ruiz de la Hermosa et al. [21] | Spain | 2016 | Case report | 1 | None | Right colectomy |
| Ishida et al. [22] | USA | 2016 | Case series | 3 | None (3). Spinal cord injury (3) | Cecopexy (1); Cecostomy and cecopexy (1); Right colectomy (1) |
| Park et al. [1] | Australia | 2018 | Case series | 4 | None (2), multiple laparotomies (1), laparoscopic cholecystectomy (1) | Right Colectomy (3), Loop ileostomy (1) |
| Shah et al. [5] | USA | 2019 | Case report | 1 | coronary artery bypass | Conservative treatment |
| Johnson et al. [23] | USA | 2020 | Case report | 1 | Coronary artery bypass | Conservative treatment |
| Basendowah et al. [9] | Saudi Arabia | 2020 | Case report | 1 | Cesarean section | Right colectomy |
We hypothesize, however, that the etiology of the cecal bascule may be due in part to relaxation from anesthesia as well as the post-operative state in someone predisposed (with a mobile cecum). It is the combination of these entities that often lead to an ileus or slowed bowel transit, even when the abdominal cavity is not entered, as in the case of cardiac surgery. This combination may also explain why we see it after c-section rather than NSVD, suggesting that spatial constraints alone may not be the key factor.
The presentation can be nonspecific with obstructive symptoms such as nausea, vomiting, and abdominal distention which can be seen quite often in more common conditions such as a post-operative ileus or small bowel obstruction. The diagnosis is at risk of being delayed due to the broad differential diagnosis, including ileus, volvulus, obstruction, and acute colonic pseudo-obstruction (Ogilvie's syndrome) [3]. A high index of suspicion in a patient with right lower quadrant pain and obstructive symptoms must be present.
Our patient was initially misdiagnosed as having a post-operative ileus. Suspicion for a more serious pathology was high, however, prompting a general surgery consult and an urgent CT of the abdomen and pelvis. Imaging modalities which can aid in diagnosis include abdominal x-ray and CT abdomen. A dilated cecum can be seen, with the distal colon appearing decompressed, as was seen in this patient [5]. This step led to the diagnosis of a cecal bascule.
The management of a cecal bascule ranges from nonoperative (nasogastric tube decompression and colonoscopic decompression) to operative management. The overall clinic picture and patient's comorbidities should dictate management. For example, nonoperative management has a high recurrence rate, as well as the risk of colonic perforation with colonoscopic decompression. However, in a patient who may not tolerate an operative intervention, nonoperative means may be attempted. Two case reports of a cecal bascule in postoperative cardiac bypass patients demonstrated successful management with nasogastric tube decompression and colonoscopic decompression [4], [5].
Operative intervention is the preferred method with procedures ranging from cecopexy to right hemicolectomy [2]. A right hemicolectomy is the gold standard, whereas a cecopexy or cecostomy tube may be tried in unstable or debilitated patients [4], [5].
Cecal bascule is a rare and difficult to diagnose, entity, which, if missed, can result in colonic ischemia, perforation, and overwhelming sepsis. A high index of suspicion must therefore be present, for pregnant and non-pregnant patients, alike. We believe that this case report adds to the existing literature in both Obstetrics and General Surgery, because it highlights how an undiagnosed congenital defect can complicate the differential diagnosis of postoperative abdominal distension and pain. Thus, employing standard surgical technique can still lead to this post-operative complication. A multidisciplinary approach to treatment is important, emphasizing the early involvement of our General Surgery colleagues. In this case, we hi-light the importance of clinical diagnosis, as well as prompt imaging in the post-natal patient with obstructive symptoms, right lower quadrant pain, and abdominal distention. When these symptoms arise, immediate management with nasogastric tube decompression, early diagnosis with CT imaging, and expedient operative management when indicated, are prudent.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Sources of funding
There was no funding for this project.
Ethical approval
An IRB was not necessary for this study.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Research registration
Not applicable.
Guarantor
Dr. Flavio Malcher.
CRediT authorship contribution statement
Conception and design: CB, XP, NM, DLL, MPS, FM.
Acquisition of data: CB, XP, NM, DLL, MPS,
Analysis and Interpretation of Data: CB, XP, NM, DLL, MPS, FM.
Drafting of the manuscript: CB, XP, NM, DLL, MPS, FM.
Critical revision of the manuscript for important intellectual content: CB, XP, NM, DLL, MPS, FM.
Administrative technical or material support: MPS, FM.
Supervision: MPS, FM.
Declaration of competing interest
CB, XP, NM, DLL, MPS disclose no financial relationships with industry or conflicts of interest.
FM discloses consulting fees from BD & Medtronic, outside the submitted work.
References
- 1.Park J.-S., Ng K.-S., Young C.J. Caecal bascule: a case series and literature review. ANZ J. Surg. 2017;88(5) doi: 10.1111/ans.13898. [DOI] [PubMed] [Google Scholar]
- 2.Lung B.E., Yelika S.B., Murthy A.S., Gachabayov M., Denoya P. Cecal bascule: a systematic review of the literature. Tech. Coloproctol. 2017;22(2):75–80. doi: 10.1007/s10151-017-1725-6. [DOI] [PubMed] [Google Scholar]
- 3.Thangasamy I., Silcock R. Caecal bascule: a rare complication following emergency caesarean section. J. Surg. Case Rep. 2010 Sep 1;2010(7):8. doi: 10.1093/jscr/2010.7.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Johnson A., Park S., Lytle F. Cecal bascule after cardiac surgery: a case report. Ann. Card. Anaesth. 2020;23(2) doi: 10.4103/aca.aca_171_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shah F., Elsayed M., Sekhar A. Cecal bascule as a cause of postoperative nausea and abdominal pain. Radiol. Case Rep. 2019;14(6):697–699. doi: 10.1016/j.radcr.2019.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim J., Nguyen S., Leung P., Divino C. Cecal bascule after laparoscopic ventral hernia repair. JSLS J. Soc. Laparoendosc. Surg. 2013;17(3):484–486. doi: 10.4293/108680813x13693422521917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Veigel M.C., Dhillon G., Andresen K.J. Multimodality imaging of cecal bascule: report of a case following pelvic surgery. Clin. J. Gastroenterol. 2012;5(3):225–229. doi: 10.1007/s12328-012-0306-5. [DOI] [PubMed] [Google Scholar]
- 8.for the SCARE Group. Agha R.A., Franchi T., Sohrabi C., Mathew G. The SCARE 2020 guideline: updating Consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 9.Basendowah M., Alabdulqader M.H., Abdulqader O., Hakami M. Cecal volvulus post cesarean section: a case report. Cureus. 2020;12(1) doi: 10.7759/cureus.6644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fanning J., Cross C.B. Post-cesarean section cecal volvulus. Am. J. Obstet. Gynecol. 1988;158(5):1200–1202. doi: 10.1016/0002-9378(88)90254-2. [DOI] [PubMed] [Google Scholar]
- 11.Bobroff L.M., Messinger N.H., Subbarao K., Beneventano T.C. The cecal bascule. Am. J. Roentgenol. Radium. Ther. Nucl. Med. 1972 Jun;115(2):249–252. doi: 10.2214/ajr.115.2.249. [DOI] [PubMed] [Google Scholar]
- 12.Chinoy M., Reyes C.V. Cecal bascule. Arch Surg. 1984 Sep;119(9):1099. doi: 10.1001/archsurg.1984.01390210089021. [DOI] [PubMed] [Google Scholar]
- 13.Pousada L. Cecal bascule: an overlooked diagnosis in the elderly. J. Am. Geriatr. Soc. 1992 Jan;40(1):65–67. doi: 10.1111/j.1532-5415.1992.tb01832.x. [DOI] [PubMed] [Google Scholar]
- 14.Rozycki G.S. Special feature: image of the month. Cecal bascule. Arch. Surg. 2001 Jul;136(7):835–836. doi: 10.1001/archsurg.136.7.835. [DOI] [PubMed] [Google Scholar]
- 15.Nwanguma O.R., Matsushima K., Grunfeld R., Frankel H.L. Colonic pseudo-obstruction (Ogilvie’s syndrome) evolving into cecal bascule. J. Trauma. 2011 Oct;71(4):1082–1084. doi: 10.1097/TA.0b013e318224da21. [DOI] [PubMed] [Google Scholar]
- 16.Lazar D.A., Cohen S.A., Evora D.K., Losasso B.E., Bickler S.W. Cecal bascule in a child: an unusual cause of postoperative bowel obstruction. J. Pediatr. Surg. 2012 Mar;47(3):609–611. doi: 10.1016/j.jpedsurg.2011.12.026. [DOI] [PubMed] [Google Scholar]
- 17.Datta J., Sakran J.V. Cecal bascule with a mesenteric band acting as a ‘point of basculation’. IJCRI. 2012;3:54–56. [Google Scholar]
- 18.Makarawo T., Macedo F.I., Jacobs M.J. Cecal bascule herniation into the lesser sac. World J. Clin. Cases. 2014 Dec 16;2(12):903–906. doi: 10.12998/wjcc.v2.i12.903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ramsingh J., Hodnett R., Coyle T., Al-Ani A. Bascule caecal volvulus: a rare cause of intestinal obstruction. J. Surg. Case Rep. 2014 Apr 11;2014(4) doi: 10.1093/jscr/rju025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reznichenko A.A., Macaluso F., Zulim R. Cecal volvulus in giant ventral hernia. Int. J. Surg. Case Rep. 2015;10:25–29. doi: 10.1016/j.ijscr.2015.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ruiz de la Hermosa A., Ortega-Domene P., Fuenmayor-Valera M.L., Pérez-Morera A., Seoane-González J.B. Caecal bascule, an unusual cause of intestinal obstruction. Cir. Cir. 2016 Dec;84(6):513–517. doi: 10.1016/j.circir.2015.10.004. [DOI] [PubMed] [Google Scholar]
- 22.Ishida Y., McLean S.F., Tyroch A.H. Cecal bascule after spinal cord injury: a case series report. Int. J. Surg. Case Rep. 2016;22:94–97. doi: 10.1016/j.ijscr.2016.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Johnson A.M., Park S., Lytle F.T. Cecal bascule after cardiac surgery: a case report. Ann. Card. Anaesth. 2020 Jun;23(2):216–217. doi: 10.4103/aca.ACA_171_18. [DOI] [PMC free article] [PubMed] [Google Scholar]



