Abstract
Introduction and importance
Gallstone ileus is an uncommon complication of cholelithiasis. It is usually presented as a small bowel obstruction. Elderly patients are commonly affected. The diagnosis is challenging, since needs a high index of suspicion and imagenology is key. Surgery is the mainstay management, most commonly performed by laparotomy, but laparoscopy is summing cases. Nevertheless the approach is still controversial. We report a gallstone ileus case, that was managed totally laparoscopic in our medium complex public institution.
Case presentation
An 71 years-old male patient, with symptomatic cholelithiasis, consulted in emergency department with symptoms and signs of small bowel obstruction. Computed tomography of abdomen and pelvis showed the classical Rigler's triad. Totally laparoscopic enterolithotomy alone was performed successfully. Postoperative evolution was without incidents, being discharge at fifth day.
Clinical discussion
Gallstone ileus represents around 0,3–0,5% of cholelithiasis complications. Mostly affect elderly women patients, with comorbidities. Mortality and morbidity is still high nowadays. The classical management of gallstone ileus is the open surgery, but the laparoscopic approach has been described and it can be done.
Conclusion
The laparoscopic management of gallstone ileus is effective and secure procedure and seems reasonable to attempt if the conditions and skills are available.
Keywords: Gallstone ileus, Enterolithotomy, Laparoscopy, Small bowel obstruction, Case report
Highlights
-
•
Gallstone ileus is an uncommon complication of cholelithiasis.
-
•
Mostly affect elderly women patients, with comorbidities.
-
•
Mortality and morbidity is still high nowadays.
-
•
The diagnosis is difficult to accomplish.
-
•
The classical management of gallstone ileus is the open surgery, but the laparoscopic management of gallstone ileus is effective and secure procedure.
1. Introduction
Gallstone ileus (GI) is an uncommon complication of cholelithiasis, representing around 0,3–0,5% of them [1], [2], [3], [4], [5].
It occurs when a gallstone becomes lodged between the gallbladder and the bowel, forming a cholecysto-enteric fistula, with impaction of the gallstones at different levels of the gastrointestinal tract [1], [2], [3], [4], [6], [7], [8], [9], [10], [11].
The mortality and morbidity is still high nowadays, mostly given by the elderly population affected, late presentation from the onset of symptoms and the difficulty to make the diagnosis [1], [2], [3], [8], [12], [13].
The mainstay management is the open surgery, but in recent years the laparoscopy approach is summing cases; giving benefits of shorter hospital stay, faster recovery, less postoperative pain, among others [2], [4], [5], [6], [12], [14].
We report a GI case, that was managed totally laparoscopically in our medium complex public institution with review of the literature. This case report is in line with SCARE 2020 guidelines [15].
2. Clinical case
A 71-year-old male patient with a medical history of arterial hypertension and multiple visits to the emergency department due to biliary colic in the last 2 years. No surgeries and important family background of diseases are reported. He presented to the emergency department with 7 days history of hypochondrial colicky pain, abdominal distention and lack of stool and gas.
On physical examination, he was dehydrated, his abdomen was distended, with no signs of peritoneal irritation and his vital signs were normal. Laboratories showed elevation of serum creatinine and leukocytosis.
He was initially treated with intravenous fluids and analgesics. Computed tomography (CT) of abdomen and pelvis was performed, revealing signs of small bowel obstruction (SBO), with a change of caliber secondary to a calculi, near to the ileocecal valve (Fig. 1).
Fig. 1.
CT abdomen and pelvis showing dilated small bowel loops (arrow), cholecysto-duodenal fistula (arrow head) and impacted gallstone (star).
Due to stable status of patient, we decided a laparoscopic approach, performed by two experienced general surgeons. After general anesthesia, pneumoperitoneum was made using a Veress needle in Palmer's point. The first 10-mm trocar was placed in the umbilicus, second 10-mm trocar in the left flank and a third 5-mm trocar in left iliac fossa. At exploration, we found dilated intestinal loops, and the site of obstruction was identified at 10 cm of ileocecal valve (Fig. 2). We proceeded to clamp the proximal bowel, with an atraumatic grasper and a longitudinal enterotomy was performed to extirpate 4 cm gallstone (Fig. 3, Fig. 4). The enterotomy was closed transversely with 3/0 vicryl sutures (Fig. 5).
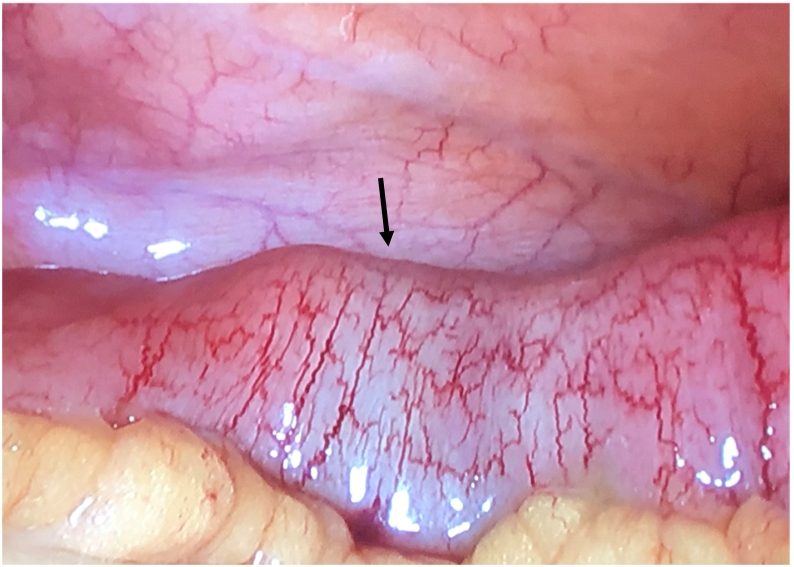
Fig. 2.
Impacted gallstone located in terminal ileum (arrow).
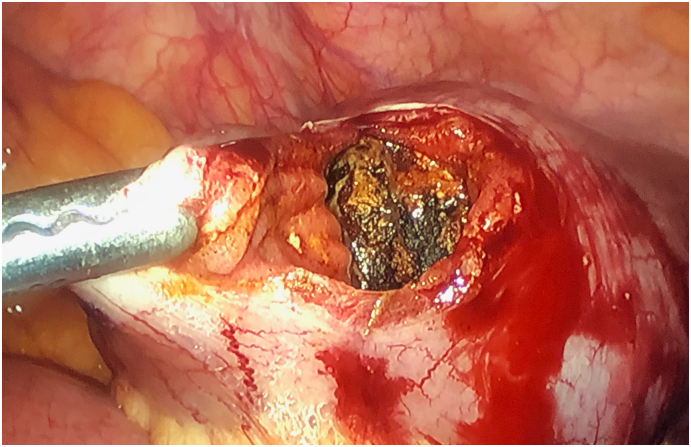
Fig. 3.
Enterotomy with the gallstone impacted in the ileum.
Fig. 4.
Gallstone extracted and measured.
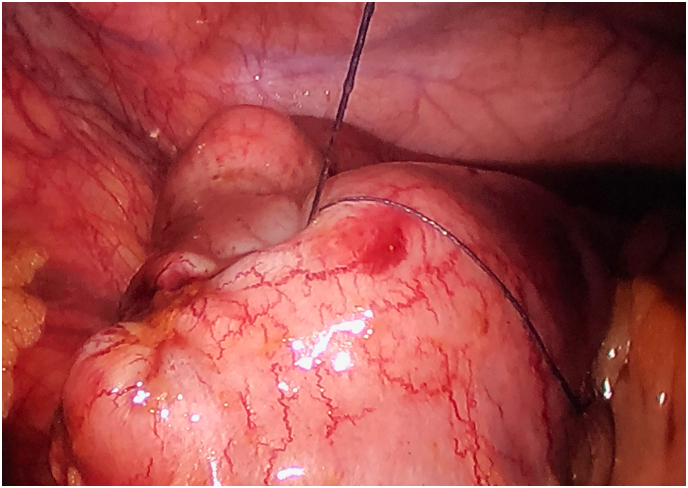
Fig. 5.
Laparoscopic closure of enterotomy transversely.
The patient postoperatively received fluid therapy, normalizing his kidney function. Oral fluids were administrated at third day, solid diet at fourth and was discharged on postoperative day 5.
3. Discussion
GI is a rare complication of cholelithiasis, with an incidence of 0.9 per 100,000 per-year [1], [2], [3], [4], [5]. It is more prevalent in women (ratio of 1:3–7), with history of cholelithiasis and mainly occurs in elderly patients, predominantly with comorbidities, which are usually frail, increasing the morbidity and mortality of the disease [1], [3], [4], [5], [6], [7], [10], [13], [14].
The GI is secondary at the migration of a gallstone to the bowel through a fistula [7], [9], [10], [13], formed due a chronic inflammation in the gallbladder and the local pressure by the gallstone against, most frequently, the small bowel [8], [9], [13]. The cholecytoduodenal fistula is the most common, in 85% of the cases, followed by cholecystogastric, cholecystojejunal and cholecystocolonic [1], [3], [5], [12], [13], [14]. There are other rarest cases, such a fistula originated directly from the biliary tract, with a higher rate of cholangitis [7], the passage of gallstones through the ampulla of Vater followed by in-situ growth or inadvertent iatrogenic migration of gallstone during manipulation of gallbladder or ducts [1], [3], [13], [14].
To cause an obstruction the stone must be at least 2 cm in diameter [1], [4], [5], [12], [14] and the sites affected usually have significant narrowing in the bowel lumen; the most common are: terminal ileum and ileocecal valve (60–75%), proximal ileum and jejunum (20–40%), stomach (14%), sigmoid colon (4%) and duodenum (3–10%), the so-called Bouveret syndrome [2], [3], [6], [7], [12], [13], [14]. Also impaction at sites of strictures, such as Crohn's disease, diverticulitis or at the neck of Meckel's diverticulum, has been described [3].
The diagnosis of GI is difficult, with a 43–73% made preoperative, and a median between admission and surgical intervention of 2–37 days, becoming an independent prognostic factor to the high mortality of this disease (7–30%) [3], [5], [7], [9], [12], [13]. This is explained because the nonspecific presentation, lack of clear history of previous biliary disease and the typical radiological features being overlooked, if they are not supported by a clinical suspicion [2], [5], [10], [12].
Patients with GI usually presents with SBO symptoms and 40–50% have history of recent episodes of biliary colic, jaundice or acute cholecystitis. On physical examination, the patient may be acutely ill and often dehydrated, jaundice could also be part of the findings; fever, toxicity and signs of peritonitis can be found in advance stage of the disease [1], [3], [4], [9], [12], [13], [14]. Classically Mordor triad is described as gallstone history, signs of cholecystitis and sudden onset of SBO. If present, GI has to be suspected [1], [13].
The laboratory studies are also nonspecific, difficulting the diagnosis, so the use of imagenology is key. Rigler's triad, described as a radiologic sign of pneumobilia, intestinal obstruction and ectopic gallstone, evident as radiopaque shadow, is pathognomonic for GI [1], [2], [5], [6], [11], [12] although pneumobilia can be found in recent endoscopic retrograde cholangiopancreatography, Oddi sphincterotomy and biliary-digestive anastomosis [1], [13], and the suspicion of an impacted calculi could be a foreign body [16].
Plain abdominal radiography could be valuable as initial workup of a SBO, with sensibility of 40–70% and positive predictive value that approaches 80% in patients with a high-grade intestinal obstruction [1], [2], [3], [12], [13], [14]. However, GI is easily missed on plain radiographs, because most gallstones are radiolucent and Rigler's triad is present in only 15% of cases [4].
Abdominal ultrasound is the method of choice for detection of gallstone disease, with efficacy of 95% and could enable the detection not only of impacted stone, but also the fistula. Nevertheless is highly operator-dependent and the performance on a patient with SBO is difficult, because of the discomfort, the bowel full of gas and fluid and the possible instability of patients; but it can be helpful if there is no availability of further imaging studies, or if the patient has an important renal failure [3], [6], [13].
CT with intravenous contrast is considered the definitive study in SBO, being accurate in diagnosing GI. It can show pneumobilia, signs of SBO, anatomic site affected and intestinal intraluminal gallstone. For GI has sensitivity of 90–93% and specificity of 100%, also helping in planning further management [1], [2], [3], [4], [7], [9], [13], [14]. With CT Rigler's triad is found in 78% of cases [9].
Magnetic resonance imaging is the gold-standard for visualizing the biliary tree, detecting even small gallstone missed on ultrasound, but the technique takes longer time and could be in detrimental of the unstable patient status in the emergency setting and if diagnosis is made by CT, there is no need of further imaging studies [3].
Even though, plain radiography could be a useful first approach, in our case, the first imaging study was the CT, because of the easy availability, it is a relatively fast technique and the amount of information that gives could stablished the diagnose. In our institution we do not count with MRI.
Once diagnose is performed, emergency surgery is needed. The keystone of managing GI is the gallstone extraction, this way solving the bowel obstruction. Different surgical approach are described: 1) Enterolithotomy alone; 2) One-stage surgery: enterolithotomy, cholecystectomy and fistula closure; 3) Two-stage surgery: enterolithotomy and delayed cholecystectomy with fistula closure, usually after four to six weeks [4], [11], [12]. The election still remains controversial, mainly because these patients are usually elders, with comorbidities, and a less extensive surgery is more beneficial for them [2], [9], [12], [13].
One-stage-surgery is usually indicated to reduce the recurrence risk of GI postoperatively, prevent cholecystitis and reduce the risk of gallbladder malignancy associated with retained fistula [7], [11], [12]. Among its adverse effects include association with high mortality (11.1–33.3%) and morbidity due to prolonged anesthesia, high leak risk of two intestinal procedures, compromising the outcome of elderly patients in poor general conditions [7], [10], [11].
Conversely, single enterolithotomy has been reported having mortality from 9.1–18.8%, fewer major complications and shorter hospital stay [7], [12].
Two-stage-procedure is suggested for patient with recurrent biliary symptoms. Some argue that this approach will spare patients from future complications such as cholecystitis, cholangitis, GI, and gallbladder carcinoma [7], [12]. Nevertheless, recurrence rate of GI after enterolithotomy alone is 5%, reoperation for calculous biliary disease occurs in less than 10% of patients and there are cases of spontaneous cholecysto-enteric fistula closure [1], [11]. Considering this, enterotomy with stone extraction alone is the most common surgical treatment, because of its low complication rate [2], [4], [5], [8], [9], [13].
Commonly, GI is managed by laparotomy, but with high morbidity (20–57%) and mortality (7–18%) associated [2], [5]. Laparoscopy in SBO has been evaluated and seems successful [2]. Moreover, in recent years, different reports have been published, showing efficacy of this approach in GI [2], [5], [7], [9], [11], [17]. This could be accomplished completely laparoscopic if intracorporeal suturing skills are available, as it was in our case.
Overall morbidity rate is low after laparoscopic enterolithotomy, describing few cases of wound infection and others, such as pneumonia o myocardial infarction [2]. In our patient, we preferred to do enterolithotomy only, as initial approach, because of the preoperative condition and his age, differing the cholecystectomy for an elective procedure. The importance of our case is that in sum to some previous reports, show the laparoscopic approach as feasible in the GI management.
4. Conclusion
In selected patients, the laparoscopic management of GI is effective and secure procedure and seems reasonable to attempt if the conditions and skills are available, providing faster recovery, with minimal morbidity, even in a medium complex institution like ours.
Informed consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Sources of funding
None declared.
Ethical approval
No ethical approval is required. Our institution does not demand ethical approval for case reports, as these projects are not investigational.
Research registration
This is not a “First in Man” study.
Author contribution
Matias Orellana: conceptualization, data curation, writing – original draft.
Liumariel Vegas: conceptualization, data curation, writing– original draft.
Pedro Soto: conceptualization, writing – review & editing.
Alfredo Caceres: writing – review & editing.
Marcelo Villarroel: writing – review & editing.
Guarantor
Matias Orellana.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Declaration of competing interest
None declared.
References
- 1.Ploneda-Valencia C.F., Gallo-Morales M., Rinchon C., Navarro-Muniz E., Bautista-Lopez C.A., de la Cerda-Trujillo L.F. Gallstone ileus: an overview of the literature. Rev. Gastroenterol. Mex. 2017;82(3):248–254. doi: 10.1016/j.rgmx.2016.07.006. [DOI] [PubMed] [Google Scholar]
- 2.Zygomalas A., Karamanakos S., Kehagias I. Totally laparoscopic management of gallstone ileus–technical report and review of the literature. J. Laparoendosc. Adv. Surg. Tech. A. 2012;22(3):265–268. doi: 10.1089/lap.2011.0375. [DOI] [PubMed] [Google Scholar]
- 3.Chang L., Chang M., Chang H.M., Chang A.I., Chang F. Clinical and radiological diagnosis of gallstone ileus: a mini review. Emerg. Radiol. 2018;25(2):189–196. doi: 10.1007/s10140-017-1568-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bircan H.Y., Koc B., Ozcelik U., Kemik O., Demirag A. Laparoscopic treatment of gallstone ileus. Clin. Med. Insights Case Rep. 2014;7:75–77. doi: 10.4137/CCRep.S16512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mirza Gari M.K., Eldamati A., Foula M.S., Al-Mulhim A., Abdulmomen A.A. Laparoscopic management for gallstone ileus, case report. Int. J. Surg. Case Rep. 2018;51:268–271. doi: 10.1016/j.ijscr.2018.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jakubauskas M., Luksaite R., Sileikis A., Strupas K., Poskus T. Gallstone ileus: management and clinical outcomes. Medicina (Kaunas) 2019;55(9) doi: 10.3390/medicina55090598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patel V.G., Gonzales J.J., Fortson J.K., Weaver W.L. Laparoscopic management of gallstone ileus. Am. Surg. 2009;75(1):84–86. [PubMed] [Google Scholar]
- 8.Assali S., Mourany J., Jones B., Dudas L., Szoka N. Technical approach to laparoscopic examination of the small bowel in gallstone ileus. Case Rep. Surg. 2020;2020:8852804. doi: 10.1155/2020/8852804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gupta A.K., Vazquez O.A., Yeguez J.F., Brenner B. Laparoscopic approach for gallstone ileus in geriatric patients. Cureus. 2020;12(6) doi: 10.7759/cureus.8642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Erdas E., Medas F., Salaris C., Canu G.L., Sanna S., Gordini L. Gallstone ileus in elderly patients. Minerva Chir. 2018;73(6):620–623. doi: 10.23736/S0026-4733.18.07718-0. [DOI] [PubMed] [Google Scholar]
- 11.Coisy M., Bourgouin S., Chevance J., Balandraud P. Laparoscopic Management of Gallstone Ileus. J. Gastrointest. Surg. 2016;20(2):476–478. doi: 10.1007/s11605-015-3019-5. [DOI] [PubMed] [Google Scholar]
- 12.Joshi M., Nguyen C., Andrade J., Eisdorfer J. Feasibility of laparoscopic-assisted approach in management of gallstone ileus. Am. Surg. 2019;85(2):e93–e96. [PubMed] [Google Scholar]
- 13.Beuran M., Ivanov I., Venter M.D. Gallstone ileus–clinical and therapeutic aspects. J. Med. Life. 2010;3(4):365–371. [PMC free article] [PubMed] [Google Scholar]
- 14.Alemi F., Seiser N., Ayloo S. Gallstone disease: cholecystitis, mirizzi syndrome, bouveret syndrome. Gallstone Ileus. Surg Clin North Am. 2019;99(2):231–244. doi: 10.1016/j.suc.2018.12.006. [DOI] [PubMed] [Google Scholar]
- 15.Agha RA Franchi T., Sohrabi C The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 16.Syed A.S., Bonte A., Allaham L.A., Goodman E.R. Peach pit impaction presenting as gallstone ileus. BMJ Case Rep. 2020;13(7) doi: 10.1136/bcr-2020-235363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee M.J., Sayers A.E., Wilson T.R., Acheson A.G., Anderson I.D., Fearnhead N.S. Current management of small bowel obstruction in the UK: results from the National Audit of small bowel obstruction clinical practice survey. Color. Dis. 2018;20(7):623–630. doi: 10.1111/codi.14016. [DOI] [PubMed] [Google Scholar]