Abstract
Introduction and importance
Cecal volvulus is uncommon cause of intestinal obstruction. It affects the ascending colon and the terminal part of the ileum which are twisted around the mesenteric pedicle.
Case presentation
We report the case of 37-year-old male who underwent emergency laparotomy for intestinal obstruction and found a twisted cecum with ileal knotting and anterior part of cecum necrosed. Resection of cecum and terminal ilium followed by end-to-end anastomosis of ileum to ascending colon were performed.
Clinical discussion
Cecal volvulus remains an uncommon cause of intestinal obstruction with a surgical incidence of 2.8–7.1 cases per year per 1 million people. Delay in diagnosis can lead to complications such as necrosis and perforation of the cecum.
Conclusion
We present a rare case of cecal volvulus in a 37-year-old male with necrosed part of the cecum without perforation. Early diagnosis and management can prevent perforation and reduce morbidity related to the cecal perforation.
Keywords: Twisted cecum, Bowel obstruction, Manual untwisting, Resection and anastomosis
Highlights
-
•
We report a 37years-old male with intestinal obstruction due to cecal volvulus without perforation
-
•
The patient underwent resection of cecum and terminal ilium followed by end-to-end anastomosis
-
•
A plain x-ray reported features of intestinal obstruction of no specific origin
-
•
Early management of cecal volvulus can help in prevention of peritonitis secondary to cecal perforation
1. Introduction
Cecal volvulus, first described by Rokitansky in 1837 as a cause of intestinal strangulation [1], is an uncommon cause of intestinal obstruction [2]. It presents when the ascending colon and the terminal part of the ileum is twisted around its mesenteric pedicle [1].
Cecal volvulus is rare and accounts for 1–1.5% of all adult intestinal obstructions [3].
The clinical signs may be highly variables and can be responsible of delays in diagnostic and treatment with consequent intestinal necrosis or perforation [4]. The mortality ranges from 10 to 40% depending on the presence of viable or gangrenous intestine [2], [3], [4].
We present a 37-year-old male who underwent emergency laparotomy for intestinal obstruction with intraoperative finding of cecal volvulus. This case report has been reported in line with the SCARE 2020 criteria [5].
2. Case presentation
A 37-year-old male presented at emergency department of a referral hospital with three days history of colicky abdominal pain associated with obstipation, not passing stool and flatus for the past three days. He also complained of nausea, hiccups and two episodes of bilious vomiting for the past two days before admission.
On general examination a sick looking patient, diaphoretic, dehydrated with stable vital signs. Abdominal examination revealed moderate diffused abdominal distension with a firm and tympanic mass in suprapubic region, there was diffuse tenderness.
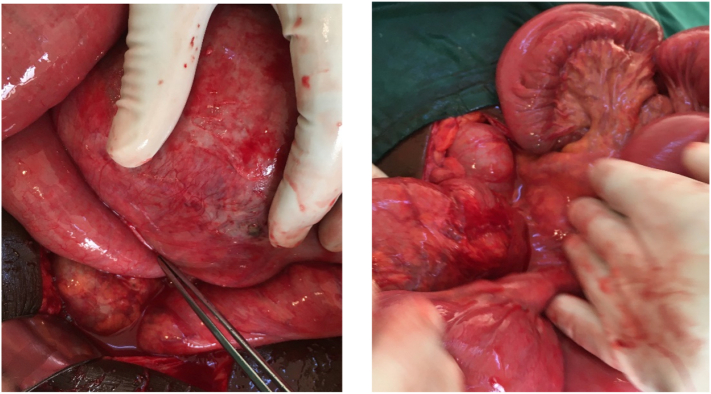
Laboratory tests showed hyponatremia and mild leukocytosis. Plain radiography showed dilated gas-filled segment of the small bowel in the central and left side of abdomen (Fig. 1), features of small bowel obstruction.
Fig. 1.
Photography of a plain radiography revealed distended bowel in central and the left abdomen.
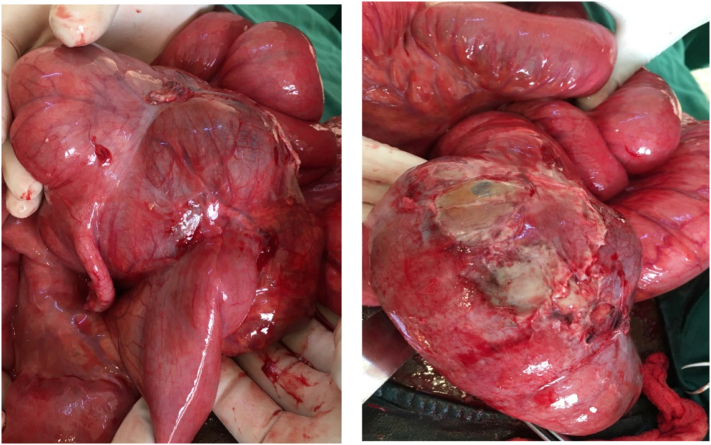
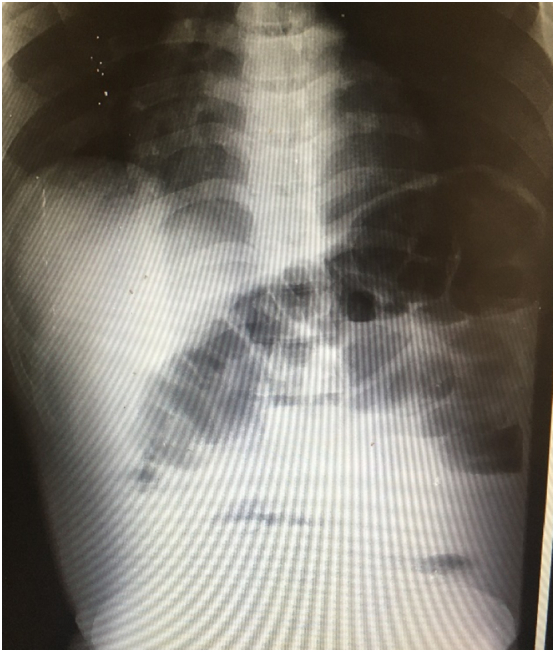
A pre-operative resuscitation, antibiotic prophylaxis followed by an emergency laparotomy were done. Surgical exploration revealed that the right iliac fossa was empty; and cecal volvulus involving cecum and terminal ileum (Fig. 2). The anterior cecal wall was necrotic without perforation (Fig. 3). A manual untwisting in a clockwise direction of about 360° followed by resection of cecum and terminal ilium and end to end anastomosis of ileum to ascending colon were performed. The patient recovered uneventfully and was discharged on the 5th postoperative day. A follow up was done a month post discharge and reported no complications.
Fig. 2.
Photos of intra-operative findings showing twisted cecum and terminal ileum with mesenteric concerned.
Fig. 3.
Photos of intra-operative findings showing normal appendix and necrosed anterior part of the cecum.
3. Discussion
Volvulus is a condition in which bowel becomes circumvolved around its mesenteric axis which can lead to partial or complete obstruction of bowel lumen and a variable degree of impairment of its blood supply [6]. Cecal volvulus is a torsion, usually of 360°, of a segment of the colon on its mesenteric axis, which causes strangulation, hence, an occlusion of the two ends of the volvulated segment compromising its blood supply, which causes an obstruction in a closed loop [7], [8]. The case presented with feature of intestinal obstruction due to cecum twisted of 360° clockwise on its mesenteric axis with necrosis of the anterior part of the cecum and dilatation.
During embryogenesis, the cecum rotates counterclockwise from the left to the right lower quadrant which will lead its mesenteric artery to be fixed to the retroperitoneal structures [7], [9].
With no predisposition related to sex, the disease predominantly affects female patients of 40–62 years of age [10]. Sufficient cecal mobility, bascule formation, adhesions from abdominal surgery, chronic constipation, pregnancy or prolonged immobility have been identified to be the leading cause of occurrence of cecal volvulus [11].
Cecal volvulus is classified into 3 types [10]:
-
•
Type 1: This cecal volvulus forms by a clockwise axial twisting or torsion of the cecum along the long axis. The location of the cecal volvulus is in the right lower quadrant.
-
•
Type 2: This cecal volvulus develops from a twisting or torsion of a portion of the cecum and a portion of the terminal ileum. The location of the cecum gets displaced to an ectopic location (typically left upper quadrant) and is relocated in an inverted orientation. Traditionally, but not for all cases, a type 2 cecal volvulus will encounter a counterclockwise twist.
-
•
Type 3: This cecal volvulus (known as cecal bascule) is the upward folding of the cecum. There is no axial twisting like with type 1 and type 2.
Type 1 and type 2, which involve axial torsion, account for approximately 80% of all cecal volvuli. Cecal bascules account for the remaining 20% of cecal volvuli [10]. The case presenting had type I whereby the cecal volvulus was twisted clockwise on its mesenteric axis with necrosed anterior part of the cecum.
Clinically, the patient with cecal volvulus will have recurrent symptoms of generalized or localized right lower quadrant abdominal pain, abdominal distension, and pain resolution after the passage of flatus with physically high-pitched bowel sounds and right lower quadrant abdominal tenderness [12]. The patient presented with three days history of abdominal pain, constipation, distension, vomiting with suprapubic abdominal distention and tenderness with hypertympanism on percussion.
Three typical signs present were cecum dilatation; a single air-fluid level in the right lower quadrant; and absence of gas in the colon on abdominal radiography can confirm a diagnosis of cecal volvulus in 70% of cases [13]. Barium enema has been applied for cecal volvulus confirmation, with reported diagnostic accuracy of 88% for acute cecal volvulus but is not recommended for the evaluation of patients with suspected perforation and gangrenous bowel [11]. With three pathognomonic signs associated with acute cecal volvulus, “coffee bean”, “bird beak”, and “whirl signs”, CT scan is preferred imaging modality for the diagnosis of acute cecal volvulus [14]. The case presented had an abdominal radiography with signs of bowel obstruction but not specific for large bowel obstruction. No barium and CT scan done due to the clinical presentation of the patient which needed an urgent laparotomy and also due to lack of CT scan in the setting where the patient was managed. It was difficult to predict the status of the intestine prior surgery since we did not do CT abdomen which could show signs of intestinal ischemia or necrosis, which manifest as submucosal oedema, diminished or nonenhancement of intestinal wall, pneumatosis intestinalis and pneumoperitoneum [14]. However, CT scan reports do not influence the management of a confirmed or suspected intestinal obstruction due to cecal volvulus.
Different techniques have been reported for successful reduction of cecal volvulus [15], [16]. Colonoscopic reduction has a documented successful rate of only 30% with potential risk of colonic perforation [15]. Generally, the only effective treatment for cecal volvulus remains surgical intervention with different options including manual detorsion, cecopexy, cecostomy and right colectomy by open or laparoscopic approaches [17]. In case of intestinal perforation or gangrenous, resection and anastomosis is inevitable [17]. The case presented had cecal and terminal ileum resection followed by ileo-ascending colon anastomosis due to the necrosis of the anterior part of the cecum.
4. Conclusion
It is important to rule-out cecal volvulus for all patients with features of intestinal obstruction. Early diagnosis and urgent management of patient with features of intestinal obstruction can prevent occurrence of peritonitis following cecal perforation.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Ethical approval
Not applicable.
Funding
The author FKS was supported by Safe Surgery in War Zone DRC (SSWZ-DRC, Grant Number 2021-01). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Guarantor
Franck Katembo Sikakulya.
Research registration number
Not applicable.
CRediT authorship contribution statement
FKS managed the patient and wrote the first draft. SMK, RM, PO, FO and PA helped in editing and reviewing the paper. All authors read and approved the final version to be published.
Declaration of competing interest
The authors declare no conflicts of interest.
References
- 1.Rokitansky C. Intestinal strangulation. Arch. Gen. Med. 1837;14:202–204. [Google Scholar]
- 2.Habre J., Sautot-Vial N., Marcotte C., Benchimol D. Caecal volvulus. Am. J. Surg. 2008;196(5):48–49. doi: 10.1016/j.amjsurg.2007.11.029. [DOI] [PubMed] [Google Scholar]
- 3.Bandurski R., Zareba K., Kedra B. Cecal volvulus as a rare cause of intestinal obstruction. Pol. Przegl. Chir. 2011;83(9):515–517. doi: 10.2478/v10035-011-0080-y. [DOI] [PubMed] [Google Scholar]
- 4.Pulvirenti E., Palmieri L., Toro A., Di Carlo I. Is laparotomy the unavoidable step to diagnose caecal volvulus? Ann. R. Coll. Surg. Engl. 2010;92(5):27–29. doi: 10.1308/147870810X12699662980231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.for the SCARE Group. Agha R.A., Franchi T., Sohrabi C., Mathew G. The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 6.Consorti E., Liu T. Diagnosis and treatment of caecal volvulus. Postgrad. Med. J. 2005;81:772–776. doi: 10.1136/pgmj.2005.035311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tejler G., Jiborn H. Volvulus of the cecum. report of 26 cases and review of the literature. Dis. Colon Rectum. 1988 Jun;31(6):445–449. doi: 10.1007/BF02552614. [DOI] [PubMed] [Google Scholar]
- 8.Peterson H.I. Volvulus of the cecum. Ann. Surg. 1967 Aug;166(2):296–299. doi: 10.1097/00000658-196708000-00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cugnenc P.H., Gayral F., Larrieu H., Garbay M. Volvulus aigu du cæcum : à propos de 10 observations. Chirurgie. 1982;108(3):279–283. [PubMed] [Google Scholar]
- 10.J Ramsingh R Hodnett T Coyle A. Al-Ani Bascule caecal volvulus: a rare cause of intestinal obstruction. J. Surg. Case Rep. 2014;2014:rju025. [DOI] [PMC free article] [PubMed]
- 11.Zabeirou A.A. Acute cecal volvulus: a diagnostic and therapeutic challenge in emergency: a case report. Ann. Med. Surg. 2019;48:69–72. doi: 10.1016/j.amsu.2019.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Agha R.A., Franchi T., Sohrabi C., Mathew G. Colonic volvulus. Diagnosis and results of treatment in 82 patients. Eur. J. Surg. 1992 Nov-Dec;158(11–12):607–611. [PubMed] [Google Scholar]
- 13.Halabi W.J., Jafari M.D., Kang C.Y., Nguyen V.Q., Carmichael J.C., Mills S. Colonic volvulus in the United States: trends, outcomes, and predictors of mortality. Ann. Surg. 2014;259(2):293–301. doi: 10.1097/SLA.0b013e31828c88ac. [DOI] [PubMed] [Google Scholar]
- 14.Delabrousse E., Sarliève P., Sailley N., Aubry S., Kastler B.A. Cecalvolvulus: CT findings and correlation with pathophysiology. Emerg. Radiol. 2007;14(6):411–415. doi: 10.1007/s10140-007-0647-4. [DOI] [PubMed] [Google Scholar]
- 15.Anderson J.R., Welch G.H. Acute volvulus of the right colon: an analysis of 69 patients. World J. Surg. 1986;10(2):336–342. doi: 10.1007/BF01658160. [DOI] [PubMed] [Google Scholar]
- 16.Tushimi T., Kurazumi H., Takemoto Y., Oka K., Inokuchi T., Seyama A. Laparoscopic cecopexy for mobile cecum syndrome manifesting as cecal volvulus: report of a case. Surg. Today. 2008;38(4):359–362. doi: 10.1007/s00595-007-3620-7. [DOI] [PubMed] [Google Scholar]
- 17.O'Mara C.S., Wilson T.H., Jr., Stonesifer G.L., Stonesifer G.L., Cameron J.L. Cecal volvulus: analysis of 50 patients with long-term followup. Ann. Surg. 1979;189(6):724–731. doi: 10.1097/00000658-197906000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]