Abstract
Introduction:
Tapes have been used to aid fresh wound closure. For hypertrophic scars, the use of tapes as a therapy to reduce the mechanical forces that stimulate excessive and long-term scarring is yet to be evaluated. The aim of this comprehensive review was to explore the current clinical application of tapes, as a minimally invasive option, as purposed specifically for the management of hypertrophic scarring, regardless of scar causation.
Method:
Databases were searched using MeSH terms including one identifier for hypertrophic scar and one for the intervention of taping. Studies included the following: patients who received tape for a minimum of 12 weeks as a method of wound closure specifically for the purpose of scar prevention; those who received tape as a method of scar management after scar formation; reported outcomes addressing subjective and/or objective scar appearance; and were available in English.
Results:
With respect to non-stretch tapes, their use for the prevention of linear surgical scarring is evident in reducing scar characteristics of height, colour and itch. Statistically significant results were found in median scar width, reduction in procedure times and overall scar rating. Tapes were predominately applied by participants themselves, and incidence of irritation was infrequently reported. After 12 months, significance with respect to scar pain, itch, thickness and overall scar elevation was reported in one study investigating paper tape. Two papers reported the use of high stretch tapes; however, subjective results limited formal analysis. Although the use of taping for abnormal hypertrophic scar management is in its infancy, emerging research indicates tapes with an element of stretch may have a positive impact.
Conclusions:
Non-stretch tapes, for the prevention of linear surgical scarring, are effective in reducing scar characteristics of height, colour and itch. Paper tapes have shown effectiveness when applied during wound remodelling or even on mature scarring, with reported subjective changes in scar colour, thickness and pliability. Preliminary evidence of the benefits of high-stretch, elasticised tapes for scar management in the remodelling phase of wound healing have also been reported.
Lay Summary
Patients are often concerned about unsightly scars that form on their bodies after trauma, especially burn injuries. These scars can be thick, red and raised on the skin, and can impact on the patient’s quality of life. For some scars, the process of skin thickening continues for up to two years after an injury.
Unfortunately, scar formation is a part of the body’s healing process, whereby there is a constant pull or tension under and along the skin’s surface. The use of simple tapes, such as microporetm, to help with wound closure are sometimes used as a therapy to reduce the tension on the skin’s surface when a wound is healing to minimise scar formation. However, the effectiveness of taping has not been proven. This paper looks at the available evidence to support the use of taping to reduce scar features of height, thickness and colour. Initial evidence of mixed levels, suggests some benefits of tapes for scar management and show preliminary efficacy for reduction of scar height, thickness and colour. More research is required to determine the direct impact, comparison to other treatments available and patient viewpoint for this therapy.
Keywords: cicatrix, scar, tape, review
Introduction
Abnormal skin scarring affects an estimated 100 million people in high-income countries each year.1–4 Hypertrophic scarring is a global health problem that can result in severe disfigurement and functionally disabling contracture formation for individuals, regardless of scar size. 5 As Young and colleagues 2 found, scarring as a result of elective and aesthetic surgical procedures can cause substantial concern for patients, even in body areas not easily visible to other people. The aim of this comprehensive review was to evaluate the current clinical application of tapes as purposed specifically for the management of hypertrophic scarring, their time to commencement and impact on scar modulation. Given hypertrophic scarring can occur as a result of any insult to the cutaneous organ, hypertrophic scarring will be explored irrespective of scar causation. First, though, we discuss wound healing, the concept of mechanotransduction and the use of tapes applied at the time of wound closure versus tapes that may be applied after wound closure has been achieved. We propose taping to be comparable with current scar management techniques and postulate the mechanisms whereby these techniques may mitigate scarring.
Wound healing
Wound healing is a complex, multifactorial biochemical and cellular process involving the disruption of homeostasis, inflammation, prolifer-ation and remodelling. 6 An imbalance in the metabolism within the extracellular matrix (ECM) and prolonged inflammatory phase is a clinical determinant of pathological hypertrophic scarring. 7 Collagen bonds laid down in the initial three weeks of scar healing are only at 20% of their final strength and, as such, once staples or sutures are removed, the tensile skin strength acting upon the wound bed can overcome the initial collagen bonds. 8 As a result, a prolonged inflammatory phase can stimulate an increase in fibroblast activity, thus increasing collagen production, and resulting in haphazard formation of scar tissue and hypertrophic scarring.8,9
Hypertrophic cutaneous scarring can be classified as abnormal and raised. 1 These scars may present as linear in nature, usually a surgical outcome or potentially widespread after a burn injury. 1 On the spectrum of scarring, a surgical scar resulting in an unnoticeable fine line is clinically desired and is the result of undisturbed wound healing. 10 Genetic predisposition may result in pathological scarring irrespective of undisturbed wound healing. 11 After a traumatic injury, such as a burn, where healing time is lengthy and wound edges irregular, the healing process can become haphazard, and as a consequence, so too does the resulting scar.12–14
Mechanotransduction
Pathophysiological principles suggest tension is one of the main triggers for increased disorganised collagen laydown during the inflammatory phase of wound healing, delaying wound regeneration.5,13,15–22 Constant pull from a thickening scar is one form of mechanical stimulus that may trigger abnormal ECM reconstruction leading to the formation of a hypertrophic scar.8,23 Current research indicates that altering the mechanical forces that impact the skin during wound healing influences scar outcome.24–26 It is accepted that intrinsic tension is necessary for initial wound closure and is well defined in the literature as being assisted using staples, sutures and even wound closure tapes such as Steri Strips™.23,27
Mechanotransduction is defined as a process of cell transmission whereby the biochemical responses, namely wound tension, received by a healing wound trigger fibrotic tissue deposition.6,14,28 The process of haphazard tissue formation occurs after the wound is epithelised, in the remodelling phase, as an immature scar.22,23,29 Chemical signals transmitted through the ECM prolong the inflammatory phase, triggering unwanted deposition of fibroblasts, myofibroblasts, epithelial cells and endothelial cells.27,30,31 The orientation of the fibrous matrix is important as it describes the nature of scar to be defined as normal or abnormal.22,23 In abnormal scarring, the disorganised fibrous matrix comprises increased collagen density and larger fibres compared to normal tissue.8,23,27,32 Wound healing in an abnormal manner may be altered by mechanical stimulus, such as the long-term application of tape, minimising signals sensed by the ECM and thus reducing wound tension.6,14,28
Levi et al. 33 found that tapes allowed for even strain distribution along linear incisions made on Yorkshire pigs when comparing the efficacy of tape-based wound closure versus suturing. It has been hypothesised that relief of scar tension, for a prolonged time period, in addition to scar hydration may minimise hypertrophic or fibrotic scar development.8,18,19,24,34–36 The process of re-establishing homeostasis of a wound healed under tension has been shown to be achieved through passive mechanical stabilisation with paper tape application.5,6,8,13,14,16,17,20–22,37–39 To translate mechanotransduction into clinical therapies, a number of therapeutic options have been proposed that are adaptable to the nature and location of a scar.6,8,24,25,32,34–36,39–42
Taping
Taping is one scar management technique that is utilised by clinicians alongside compression, massage and silicone products. 43 Although each technique varies with respect to existing physiological rationales, each has been used to alter a scar that is linear in nature. 1 For scars of an irregular shape or that are red, raised, painful and itchy, the use of taping is one clinical intervention that is yet to be thoroughly explored. Previous studies have shown that the use of tape applied directly over a wound or scar, for the purposes of scar management, can reduce skin tension in humans.8,24–26,34,35,39 Tapes, as a low-stretch or high-stretch material backed adhesive, have been used to aid wound closure, by pulling fresh wound edges together, but the use of tapes as a therapy that reduces the mechanical forces that stimulate excessive and long-term scarring is yet to be examined. Additionally, factors such as surgeon preference for tape type, e.g. adhesive strips or paper tape, wound healing time, patient adherence and overall satisfaction with treatment options offered can impact overall scar outcomes.6,8,24,25,39 It has been established by several researchers that combinations of different types of sutures, coupled with either additional sutures, a dressing, adhesive strips or a form of paper tape can heal a linear surgical wound neatly within three months.8,24,25,32,39,40,43–48 Consistent with pathophysiology principles of wound healing and scar formation, tapes with differing levels of stretch may be an effective long-term scar treatment, applied either over or around a scar to reduce skin tension. It remains necessary to identify the application method, scar outcomes, impact of treatment and long-term patient satisfaction of taping.
Other therapies
Based on similar theoretical foundations to mechanotransduction, the use of compression therapy for scarring with patients after burn injury is one of the most frequently used treatment modalities. 1 Compression is considered to be an effective treatment for pathological scarring, regardless of the size of the scar. 48 As an adjunct to compression therapy, silicone gel products have been shown to flatten scar tissue supposedly through occlusion and hydration. 1 Each method of scar treatment comes with its own challenges including: low adherence rates; skin irritation; and sensory sensitivity.49–51 When compression garments are used, the requirement that these be worn for long periods of time can be challenging for individuals, impacting their quality of, and participation in, everyday life.49,50
In this comprehensive review, we examine the evidence surrounding the use of taping, as a non-invasive option, for the management of hypertrophic scarring as a result of surgical incision or traumatic injury. As an adjunct, this review will attempt to determine if taping is shown to be an efficacious clinical modality, comparable to traditional scar treatment options.
Methods
Search strategy
Seven databases (PubMed, MEDLINE, Cochrane, CINAHL, OT Seeker, Embase, Web of Science) were searched from inception to April 2021. The search included one identifier for hypertrophic scar and one for the intervention of taping, with the aim to alter scar. The following Medical Subject Heading (MeSH) keywords were applied: ‘hypertrophic’ OR ‘scar’ OR ‘cicatrix’ OR ‘abnormal cicatrix/scar’ OR ‘trauma scar’ AND ‘tape’. To capture all relevant data, numerous additional searches with a wider scope were conducted by the authors. The following keywords were applied: ‘scar’ or ‘cicatrix’ or ‘hypertrophic’ and ‘tape’, ‘surgical tape’, ‘adhesive surgical tape’, ‘paper tape’, ‘MeFix’ or ‘Fixomull’ or ‘Hypafix’, ‘cloth tape’, ‘athletic tape’, ‘kinesio tape’, ‘orthotic tape’, ‘skin tape’, or ‘athletic tape’. Lastly, and before full text review, a hand search of all reference lists and bibliographies was conducted by two reviewers.
Criteria for inclusion
Studies were included if they were: (1) published or translated into English; (2) identified as original, relevant and empirical research; (3) involved participants aged 18 years and over, or under the age of 18 years where there was a consenting adult; (4) included patients who, as indicative of maximum scar strength, received tape for a minimum of 12 weeks commencing at time of wound closure specifically for the purpose of scar prevention, or who received tape as a method of scar management after scar formation; and (5) reported outcomes addressing subjective and/or objective scar appearance. Theses or ‘unpublished’ works, letters to the editor or letter replies, and animal studies were not included. Eligibility for inclusion, based on title and abstract, was assessed independently by two reviewers. A third reviewer was available if required. This review specifically aimed to evaluate tapes for scar management, not as a method of wound closure. Tissue adhesive strips commonly used for short-term wound closure were excluded from this review unless they were identified to have been used for scar management purposes or worn for a minimum of 12 weeks. Additionally, due to duration of wear, tissue glues were excluded from this review. Abstracts meeting the inclusion criteria or requiring more information from the full text to clarify inclusion were retained. Differences were resolved by discussion between the first two reviewers, with no third-party review required.
Data extraction
Customised and structured data extraction forms were developed. Study design, number of participants, type of taping and scar characteristics are summarised in Table 1.
Table 1.
Summary of included studies.
| Author, year | Country | Study design | Participants (n) | Control group | Tape type | Procedure / Diagnosis |
|---|---|---|---|---|---|---|
| Atkinson et al., 2005 | Australia | RCT | 39 | No intervention | Paper tape | Post-caesarean |
| Daya, 2011 | South Africa | Case series | 29 patients (42 scars) |
N/A | Micropore tape | Mixed (burn, surgical, trauma) |
| Karwacińska et al., 2012 | Poland | Case series | 54 | N/A | Kinesio tape | Burn scar |
| Kim et al., 2015 | Korea | Non-RCT | 77 | Suturing | Leukosan Skin link (tape) | Facial laceration |
| Lin et al., 2020 | Taiwan | RCT (within patient) | 47 | Silicone sheet | Steri Strip™ | Post-caesarean |
| Rosengren et al., 2013 | Australia | RCT | 136 | No intervention | Paper tape | Skin excision (torso) |
| Sawada et al., 1998 | Japan | Case series | 9 | N/A | Blenderm™ | Burn scar |
| Toscano et al., 2016 | Italy | Case series | 1 | N/A | Kinesio tape | Burn scar |
| Widgerow et al., 2009 | South Africa | RCT (within patient) | 10 patients (20 scars) |
Paper tape + gel | Paper tape | Breast surgery |
N/A, not applicable; RCT, randomized controlled trial.
Methodological quality assessment
The methodological quality of included studies was rated independently by two reviewers. The 27-item modified Downs and Black checklist was used to appraise articles that reported on randomised or non-randomised controlled trials. 52 The remaining studies were appraised using a modified Critical Appraisal Skill Program (CASP) tool as a methodological checklist providing key criteria relevant to cohort studies.
Results
Search results
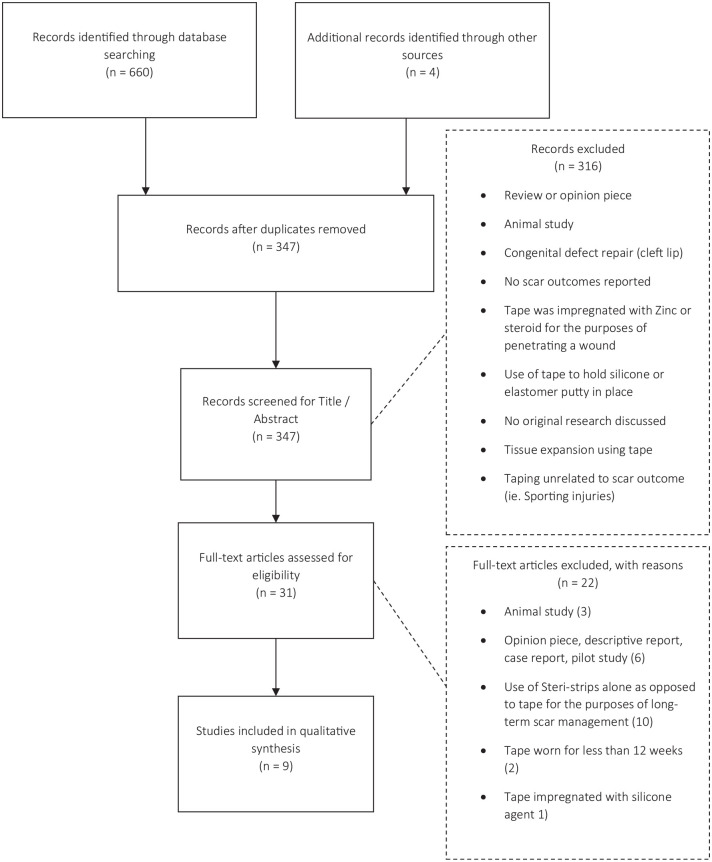
A total of 347 unique articles were identified using the aforementioned search strategy, including four additional articles identified through hand searching. Nine studies published between 1998 and 2015 from eight countries were included in the final analysis (Figure 1). A total of 402 participants with 425 scars were evaluated within the nine studies. Frequent reasons for exclusion of articles were that the use of tape was to hold a silicone product or elastomer putty in situ, the tape was worn for a short time period (<12 weeks), or the tape was impregnated with zinc or steroid for the purposes of wound penetration only. Of the included studies, four randomised controlled trials, one non-randomised controlled trial and four case studies were identified and reviewed.
Figure 1.
PRISMA flow diagram. Please swap over the figures.
Quality assessments
Five studies appraised using the Downs and Black tool (Table 2) rated highly in terms of reporting and external validity.8,24,41,43 Internal validity was found to be average, with three out of five articles not meeting the criteria of a blinded assessor.35,41,43 Given the nature of the intervention under examination, the blinding of subjects was not possible in any of the studies. One study allowed participants to nominate their allocation, adversely impacting intervention randomisation. 41 Seven out of nine studies reported reliable and valid outcome measures and all studies recruited participants over the same period of time. Of the four studies assessed using the CASP tool (Table 3), one study rated highly overall, presenting sound methodological quality and application within a local clinical setting. 38 The remaining three studies failed to describe adequate reporting of individual participant results and neglected formal analysis, impacting local utility.11,35,53
Table 2.
Critical appraisal of included studies using Downs and Black (n = 6).
| Reporting | External validity | Internal validity | ||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | 25 | 26 | 27 | ||
| Study | Hypothesis/ Aims | Outcome measures | Patient characteristics | Interventions | Distribution of confounders | Main findings | Estimation of random variability | Adverse events | Attrition | Actual probability values | Generalisable population | Subjects selected representative | Intervention representative | Blinding of subjects | Blinding of assessors | Data dredging results | Analysis adjustment for follow-up | Appropriate statistical tests | Compliance to intervention reliable | Valid reliable outcome measures | Same population | Same period of time | Randomised to intervention group | Randomised concealment | Adjustment for confounders | Attrition explained | Sufficient power calculation met | Total score X/28 |
| Atkinson et al., 2005 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | U | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 27 |
| Kim et al., 2015 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | × | U | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | × | × | ✓ | ✓ | ✓ | 24 |
| Lin et al., 2020 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | × | ✓ | ✓ | ✓ | ✓ | ✓ | × | × | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | × | ✓ | ✓ | × | 23 |
| Rosengren et al., 2013 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | × | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 27 |
| Widgerow et al., 2009 | ✓ | ✓ | × | ✓ | × | ✓ | ✓ | × | × | ✓ | U | U | ✓ | × | U | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | × | U | U | U | 15 |
✓, yes; ×, no; U, unable to determine.
Table 3.
Critical appraisal of included studies using CASP (n = 4).
| Validity | Results | Local application | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | ||
| Study | Address a clearly focussed issue | Acceptable cohort recruitment | Accurate exposure measurement | Accurate outcome measure | Confounding factors identified | Confounding factors accounted for | Subjects follow-up completeness | Subjects follow-up time frame | Results | Precision of results | Believability of results | Local application | Other evidence available | Study implications | Total score X/14 |
| Daya, 2011 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | U | 13 |
| Karwacińska et al., 2012 | ✓ | ✓ | × | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | × | ✓ | ✓ | ✓ | U | 11 |
| Sawada et al., 1998 | ✓ | ✓ | U | × | × | × | ✓ | ✓ | U | × | × | × | ✓ | × | 5 |
| Toscano et al. 2016 | ✓ | ✓ | U | U | ✓ | × | ✓ | ✓ | ✓ | U | U | U | ✓ | × | 7 |
✓, yes; ×, no; U, unable to determine.
Study characteristics
Study characteristics are outlined in Table 1. Further detailed tables were created to describe the nature of the interventions (Table 4). Essential considerations for clinical practice, namely, tape type used, duration of wear, incidence of irritation, outcome measures used and details regarding results of patient satisfaction and scar assessments are summarised in Table 5. Two studies did not differentiate between tapes applied to keloid scarring or to hypertrophic scarring and, thus, results from tape use on both keloid scars and hypertrophic scars were pooled. Given both studies utilising tapes offered intervention outcomes per the inclusion criteria, they were included. Intervention outcomes were separated into two categories: early application, where taping was introduced at the time of wound closure; and late application, where tapes were commenced following the initial healing stage of wound closure following re-epithelisation of the wound bed. Taping was then continued for a minimum of 12 weeks as per the inclusion criteria.
Table 4.
Description of interventions.
| Author, year | Tape type used | Commencement time frame | Scar age | Duration of wear | Length of wear until changed | Applied by |
|---|---|---|---|---|---|---|
| Atkinson et al., 2005 | MicroporeTM | Early | 4–6 days | 12 weeks | 3–5 days | Patient |
| Daya, 2011 | MicroporeTM | Late | 1–20 years | Different for all depending on follow-up adherence | Weekly | Patient |
| Karwacińska et al., 2012 | Kinesio tapes | Late | <1 year (n = 37) >1 year (n = 17) |
12 weeks | Weekly, off for 3–4 in-between applications | Patient |
| Kim et al., 2015 | Leukosan Skin Link™ tape + Steri Strips™ | Early | 0 | 10 days then Steri Strips™ for 3 months | Not reported | Patient |
| Lin et al., 2020 | Steri Strips™ | Early | 1 week | 12 weeks | Daily | Patient |
| Rosengren et al., 2013 | Leukosan Skin Link™ tape | Early | 0 | 12 weeks | Weekly | Patient |
| Sawada et al., 1998 | Blenderm™ | Late | 1 month | 4–6 months (mean = 5.2 months) | Daily | Parent/carer of patient |
| Toscano et al. 2016 | Kinesio tape | Late | 4 months | 15 months | Weekly | Therapist |
| Widgerow et al., 2009 | MicroporeTM | Early | 0 | 3–6 months | 7–10 days | Patient |
Table 5.
Summary of outcomes.
| Author, year | Scar type | Tape type used | Duration of wear | Incidence of irritation | Outcome measure used | Patient satisfaction details | Scar outcome |
|---|---|---|---|---|---|---|---|
| Atkinson et al., 2005 | Linear / hypertrophic | MicroporeTM | 12 weeks | 4/34 0.12% | Ultrasound Scar Classification Scale (Mustoe) |
Not reported | None of the treatment group developed HTS on completion of 12 weeks 12 patients (41%) developed HTS in control HTS after tape removal: 1/39 Stretched scars after tape removal: 3/39 |
| Daya, 2011 | Hypertrophic / keloid | MicroporeTM | Different for all depending on follow-up adherence | 2/29 (0.006%) | Modified POSAS Scar appearance (photographic score) |
Not reported | Pain reduction*
Itch reduction* Thickness reduction* 69% decrease in scar elevation* 29% no change in scar † Reduced scar redness, height and shine on study completion |
| Karwacińska et al., 2012 | Hypertrophic / keloid | Kinesio tapes | 12 weeks | Not reported | Thickness: digital calliper Patient satisfaction Personal observations (author) Colour change |
Change in appearance and scar perception after 3 weeks (37 patients), 6 weeks (10 patients), 9 weeks (5 patients), 12 weeks (2 patients) 77% reported 100% satisfaction |
(All subjective parameters) Height: 50% reduced height Colour: 40% significant change Scar tissue mobility: 33% had 50% improvement, 27% had 100% improvement |
| Kim et al., 2015 | Linear | Leukosan Skin Link™ tape AND Steri Strips™ | 10 days then Steri Strips™ for 3 months | 1/77 (0.012%) |
POSAS Patient satisfaction Procedure times |
Taping group more satisfied on 4-point scale (3.19/4) | Both groups scored POSAS ~20/60
‡
Procedure time shorter* |
| Lin et al., 2020 | Linear | Steri Strips™ | 12 weeks | Not reported | VSS VAS |
Significantly better scar appearance than tape at 6 and 12 months, no differences between pain and itch | No statistically significant differences found at 3 and 12 months with respect to pliability, height, vascularity and pigmentation
†
Keloid or HTS did not change outcomes on the VSS or VAS |
| Rosengren et al., 2013 | Linear | Leukosan Skin Link™ tape | 2 weeks | 1/63 (0.015%) | Scar width, elevation, depression and colouration Scar appearance Patient satisfaction |
Subjective scar assessment same in both groups at 6 months Very satisfied 43.1% (taped group) |
Overall scar rating*
Median scar width was 1 mm narrower when taped* |
| Sawada et al., 1998 | Hypertrophic / post grafting | Blenderm™ | 4–6 months, mean = 5.2 months | Mild plaster dermatitis to surrounding normal skin, no % reported | Scar pigmentation, hardness, bulkiness, wrinkles and shrinkage | Not reported | (All subjective parameters) Reported at 18 months Pigmentation: 100% improvement † ‘Hardness’: 55% improvement † 3 participants were noted to have improvement in bulkiness, less ‘wrinkles’ and shrinkage (graft became less contracted) † |
| Toscano et al., 2016 | Hypertrophic / post grafting | Kinesio tape | 7 months | No adverse effects | ROM Photographic assessment Scar colour, extensibility, pliability, pain, and dysesthesia |
Good patient compliance noted | Faster change in scar colour during remodelling phase ‘ripening phase’
†
Pliability increase, colour improved, pain resolved, tension and hypertrophy reduced, resolution of hypersensitivity, increased functional ROM † |
| Widgerow et al., 2009 | Linear | MicroporeTM | 3–6 months | Nil | POSAS VSS |
Not reported | Scars demonstrated borderline significance with respect to stiffness, thickness, and regularity
†
No patients developed HTS |
Statistically significant result.
Not statistically significant.
POSAS scores closer to 0 are deemed a more appealing scar.
HTS, hypertrophic scarring; POSAS, Patient Observer Scar Assessment Scale; VAS, visual analogue scale; VSS, Vancouver Scar Scale.
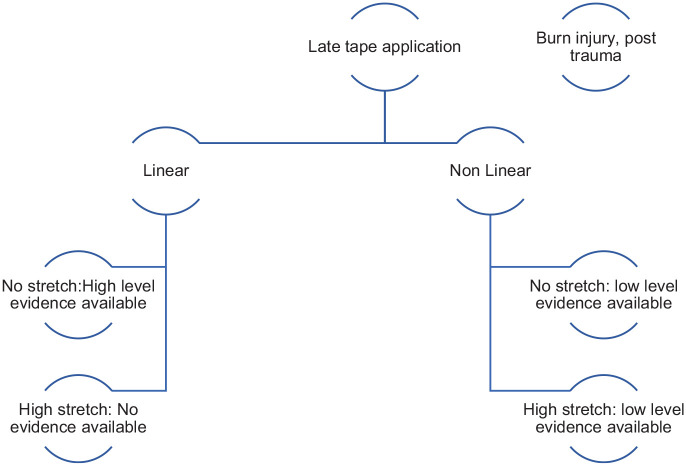
Early application
Studies were included where tapes were used in the prevention of hypertrophic or abnormal scar development after procedures involving linear surgical incisions, and when scar assessment was conducted. Figure 2 summarises evidence-based recommendations for early tape application based on quality appraisal. Tapes were routinely applied either at the time of wound closure or within one week following surgical intervention, usually upon removal of sutures following post-caesarean section, breast augmentation, removal of lesion or following traumatic facial laceration.8,24,41,43,54 Where studies employed the use of Micropore™ paper tape, they reported no development of hypertrophic scarring while the tape was in situ.8,43 Interestingly, one case of hypertrophic scarring and four cases of stretched scars occurred after removal of the paper tape after 12 weeks. 8 In the studies competed by Lin et al., 54 and Widgerow et al., 43 there were no statistically significant results found with respect to height, pliability, stiffness or scar thickness when utilising Steri Strips™ and Micropore™ tape, respectively. Length of wear until tape change did not appear to affect outcomes noted by all five studies who prescribed early tape application. Two studies examined the use of Leukosan Skin Link™ or Leukostrips™ for wound closure after facial laceration or skin excision.24,41 Both studies compared the intervention of taping to the more traditional wound closure method of suturing.23,40 Tapes were applied, in one study, perpendicularly to the sutured wound, and worn for 10 days or until they fell off, then reapplied for 12 weeks. 23 Patients involved in the study by Kim et al. 41 chose their respective skin closure allocation, and while the authors were unable to report significance with respect to Patient and Observer Scar Assessment Scale (POSAS) results, they noted a statistically significant reduction in procedure time. Rosengren et al. 24 demonstrated significance in median scar width (1 mm narrower when taped) and overall scar rating. Patients either applied Leukosan Skin Link™ for 10 days without removal followed by Steri Strips™ for 12 weeks, or received sutures for five days and were then instructed to change to Steri Strip™ application until three months had elapsed. Tapes were mostly routinely applied by participants themselves, weekly on average, and incidence of irritation was infrequently reported (0.12% of cases) in the form of an itchy rash, superficial rash, dermatitis, allergy to tapes or infection under the tape.8,24,41,43,54
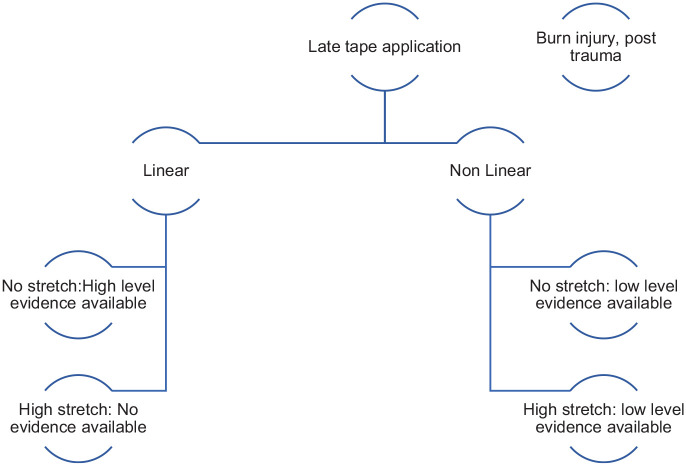
Figure 3.
Late tape application clinical guide.
Late application
Where taping was commenced to a healed scar, the tapes used were paper tape such as Micropore™, non-stretch tape such as Blenderm™ and elastic tape such as Kinesio tape. Tapes were used for management of abnormal scarring as a result of surgery or burn injury.11,35,39,53 Figure 2 summarises evidence-based recommendations for late tape application based on quality appraisal. At the time of tape application, scars had been present for between one month and five years, with one study reporting a scar age of 20 years. Scar thickness, pliability / softness and colour change were notable improvements when tape was utilised on mature scars.11,35,39,53 A reduction in pain and subsequent increase in patient adherence was found in two studies where tape was applied for an average of 12.25 months.11,39 Karwacińska et al. 35 found scars that were present for more than a year required taping to be used for 3–12 weeks to observe a subjective change.
Figure 2.
Early application clinical guide.
Tension
In two studies, tapes were applied directly over the scar, overlapping by 4–5 cm.8,43 In an attempt to reduce surface skin tension, both Karwacińska et al. 35 and Daya 39 utilised body positioning and pulled surrounding skin in towards the scar. This method allowed the tape to be applied in a cross-hatched pattern, thereby reducing skin tension. Daya found a statistically significant reduction in pain, itch, thickness and scar elevation, while Karwacińska et al. subjectively reported 40% of scars had a positive scar colour change and in 50% of patients, scar height was halved. Tapes were worn for a minimum of 12 weeks, up to six months in some cases, or until a scar was deemed mature (pale, flat). Tapes were mostly changed by the patient every 3–5 days, leaving tapes off between application (usually 2–3 days), allowing the skin to breathe. Atkinson et al. 8 noted where taping was used for thicker scars, there was a greater decrease in intradermal scar volume than was the case for thinner scars. Almost all studies reported that taping was more cost-effective when comparing tapes to compression therapy or traditional suturing. The incidence or form of irritation was no different for tapes applied after re-epithelisation.
Hydration
Following a disturbance to the stratum corneum, such as after a burn injury, silicone products and tapes have been used as a method of controlling hydration, returning homeostasis to a scar. 8 Described by several authors, non-stretch tapes and even elastic Kinesio tapes applied at zero percent stretch, have been utilised for the hydration of a scar.8,53,54 Sawada et al. 53 studied the use of Blenderm™ as an impermeable barrier, worn at all times after split skin grafting, for an average of 5.2 months. Although no formal scar outcome measures were reported, the authors noted that scars were ‘soft and less pigmented’. Used to treat areas where compression was not possible, Toscano et al. 11 investigated Kinesio taping as an extension of the concept of neuromuscular taping. In a single case study, they applied elastic tapes at zero percent stretch to stimulate the skin and underlying tissues, noting a subjective positive change to scar colour, pliability and extensibility. 11 Although improved scar appearance was found to be statistically significant at six and 12 months follow-up, clinically meaningful differences were not found between tapes and silicone sheets when randomly compared by Lin et al. 54
Patient-reported outcomes
Patient satisfaction with taping was considered in three studies, where some reported a change in appearance and scar perception as early as three weeks when compared to the application of Steri Strips™, conventional suturing, or to no intervention.24,35,41 Upon study completion, taping was found to have better outcomes than the control (conventional suturing, absorbable suture + Steri Strip™, or no intervention) in terms of overall satisfaction in the same three studies.24,35,41 Karwacińska et al. 35 reported that 77% of participants reported 100% satisfaction on a subjective rating scale after 12 weeks of elastic taping on mature scars previously untreated. Similarly, 43.1% of taped participants in one study reported being ‘very satisfied’ upon study completion. 24 A significant reduction in scar thickness, from the patient’s perspective, was found in one study when assessed using the POSAS.25,39. Two of the nine studies reported improvements in scar colour and vascularity, with Karwacińska et al. reporting an improvement in 40% of participants.11,35 A statistically significant reduction in both pain and itch was found by Daya, 39 where scars as old as 10 years were treated with paper tape.
Discussion
This is the first review, to our knowledge, to examine the use of tapes (either with or without stretch) for scar prevention and correction. Findings revealed longstanding clinical relevance leaning towards the use of tapes with little stretch (i.e Micropore™ or Steri Strips™) to support closure of linear surgical wounds to reduce skin tension. The occlusive nature of both high-stretch and non-stretch tapes offer increased scar hydration and consequently positive subjective scar outcomes. Although the use of taping for scar management after traumatic injury is in its infancy, emerging research indicates tapes with an element of stretch may have a positive impact on hypertrophic scarring.
Early versus late tape application
It is known that healing times for hypertrophic scarring can be in the range of 6–18 months. However, most studies reviewed employed tape therapy for an average of 12 weeks. Collectively, data supported the use of tapes for improvements in linear scarring, consistent with theoretical and venerable principles of wound closure to reduce migration of collagen cells. Clinicians utilising taping as a method of hypertrophic scar prevention should commence as early as one week postoperatively for linear scarring with a non-stretch tape. There is no literature to support the use of early treatment for burn scarring. Perceived benefits of wound closure techniques for scar prevention of irregular-shaped wounds or burns could be assumed to apply the same theoretical principles whereby mechanical offloading can reduce tensile forces. Piloted by Moortgat et al., 26 high-stretch Kinesio tapes, taped around a scar, demonstrated a statistically significant skin tension reduction. This review found, with varying methodologies, that tapes with or without stretch, may be applied during the remodelling phase or later and still attract a great subjective change in scar colour, thickness and pliability. The remodelling phase takes up to one year, and as identified by several authors, clinical scar assessment is important at the one-year time point when the ordered biochemical series of events including cell migration, deposition and turnover is completed. 25 However, a longer time period of tape application such as 6–12 months may further enhance outcomes.8,24
Study quality
This review found variability and absence of robust methodologies, particularly when referencing or investigating abnormal hypertrophic scars as a result of traumatic injury such as a burn. As anticipated and pertaining to the nature of the intervention, no studies were able to offer blinding to participants. Where possible most studies randomised participants using sequentially numbered envelopes, to a treatment or control group.8,24 Confounding bias was evident in the study by Kim et al. 41 where patients self-selected their intervention group. To minimise this, the measurement of association between tape and control is required to be equivalent in both treatment arms. Single case study design, where the patient acts as their own control, was the most frequently used method reported. In these studies, one half of the wound was randomised to intervention versus usual care depending on surgeon preference. Although single case studies are helpful in providing a greater understanding of the impact of an intervention, research studies with larger samples sizes are required to ensure casual inference and generalisability to a wide population, particularly when investigating a burn injury. 55
Patients value improvement in scarring and show concern for scarring even after routine surgery. 2 Hypertrophic scars, regardless of size, detrimentally affect quality of life. 50 In all studies involved in this review, the reproducibility of clinical treatment interventions described with respect to time to commencement of therapy, length of application and identification of adherence were scant. Karwacińska et al. 35 explored Kinesio tape application when stretched from 25% to 100% and relied on patients’ and carers’ subjective evaluation of taping effectiveness. Additionally, rates of adherence to interventions were not recorded, resulting in potential bias. In order to account for bias of measurement between taping and any given intervention or control, studies should address the impact of intervention adherence. 56 If taping were a feasible option for prevention or correction of hypertrophic scarring, explicit and reproducible methodology is vital for clinical healthcare research. 57
Across all the included studies, there was a lack of detailed participant description including participant predisposition for scarring, time to wound re-epithelisation and the commencement of tape application if not at the time of surgical wound closure. Fitzpatrick skin type, as a potentially determining factor for increased scarring risk, was not identified in any of the studies within this review. Each of these elements pertain directly to clinical practice and the impact of an intervention on any given patient. It is recommended that future studies consider the impact of independent and confounding variables related to participant characteristics in order to provide a clearer clinical picture.
Scar aetiology
Although the histological and epidemiological differences between keloid and hypertrophic scarring are widely accepted, clinical similarities do not differentiate the non-invasive treatment methods offered to patients. The authors also acknowledge the use of tapes to control keloid scarring in addition to evaluating hypertrophic scarring in two studies where results were pooled.35,39 Both studies identified clinically positive subjective changes with respect to scar characteristics of pain, itch, thickness, colour, height and tissue mobility. Similarly, it is important to acknowledge the difference in healing characteristics between linear surgical wounds and traumatic, non-linear wounds where deposition of scar forming matrixes may be more abundant and difficult to control with simply one piece of tape. It is for this purpose that future research, perhaps with tapes with high-stretch properties that can navigate a variety of different directions around a wound, may be warranted.
Comparable therapies
For patients where scars are irregular in shape and hypertrophic, an investigation into taping versus other therapies of long-term scar management such as compression therapy would inform healthcare for hypertrophic scarring. Where management of existing hypertrophic scarring as opposed to prevention was studied,24,34,35,39 no other comparable therapies were researched. Although overall patient perception of taping was found to be positive in four out of seven studies, comparison was not made with other traditional therapies such as compression therapy.24,25,35,41 Nor was the impact of tapes on occupational performance or engagement in everyday activities (e.g. swimming, showering, exercising) considered. Compression is regarded as an effective treatment for pathological scarring, regardless of the size of the scar. 49 However, adherence to compression protocols has been reported to be low.49,50 Engagement in everyday activities has been found to be interrupted for some patients by compression therapy due to itch and heat intolerance, inability to wear during work, sport, intimacy and public perception.49,50,58 With tapes offering a potentially successful scar outcome, they could offer an additional treatment method for scars, particularly for those that result from small burn injuries.
Tapes could provide a method to apply pressure to reduce blood flow, accelerate fibroblast transition, enhance scar hydration, and decrease collagen laydown in addition to acting as a stabiliser for dressings or hydrating/silicone products.8,34,39 Mustoe et al. 29 proposed, for surfaces that are complex or mobile, such as the shoulder, elastic-based tapes could be useful. It would be beneficial to undertake research in a clinical field such as burn care when tape is compared to compression therapy or silicone use particularly for scarring where a compression garment may be cumbersome.
Study limitations
Although studies in this review were drawn from several countries, inclusion criteria were confined to English language studies only. Translation services were outside the scope of resources available for this study. Thus, it is acknowledged that studies published in other languages may have been missed. As an emerging area of clinical practice, the use of tapes with elastic properties for the management of irregular scarring may have been investigated on humans by parties where research is yet to be published. Animal studies, theses and unpublished works were not examined as part of this review. However, it is noted that Tollefson et al. 32 have investigated paper tape and silicone gel sheeting application for prevention of hypertrophic scarring on the rabbit ear model, with success.
Conclusion
Non-stretch tapes for the prevention of linear surgical scarring is evident in reducing scar characteristics of height, colour and itch, and should be commenced early in the healing cascade. Paper tapes have shown effectiveness when applied during wound remodelling or even on mature scarring, attracting subjective changes in scar colour, thickness and pliability. There is no literature to support the use of early treatment for burn scarring. While outcomes supporting the use of elastics tapes within one rigorous study may be utilised as preliminary evidence of the benefits of high-stretch, elasticised tapes for scar management, more rigorous research is required to determine the direct impact and patient perspective for this intervention.
Acknowledgments
The authors wish to acknowledge the support of Sue Laracy, Director of Occupational Therapy at the Royal Brisbane and Women’s Hospital, and the Royal Brisbane and Women’s Hospital Foundation.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Royal Brisbane and Women’s Hospital Foundation, through a 2020 Foundation Postgraduate Scholarship and the 2019 Metro North Collaborative for Allied Health Research, Learning and Innovation (CAHRLI) Scholarship.
ORCID iD: Sarah O’Reilly  https://orcid.org/0000-0001-9026-5448
https://orcid.org/0000-0001-9026-5448
References
- 1. Monstrey S, Middelkoop E, Vranckx JJ, et al. Updated Scar Management Practical Guidelines: Non-invasive and invasive measures. J Plast Reconstr Aesthet Surg 2014; 67(8): 1017–1025. [DOI] [PubMed] [Google Scholar]
- 2. Young VL, Hutchison J. Insights into patient and clinician concerns about scar appearance: semiquantitative structured surveys. Plast Reconstr Surg 2009; 124(1): 256–265. [DOI] [PubMed] [Google Scholar]
- 3. Sund B. New developments in wound care. London: PJB Publications, 2000. [Google Scholar]
- 4. Bayat A, McGrouther DA, Ferguson MWJ. Skin scarring. BMJ 2003; 326(7380): 88–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Barnes LA, Marshall CD, Leavitt T, et al. Mechanical forces in cutaneous wound healing: emerging therapies to minimize scar formation. Adv Wound Care 2018; 7(2): 47–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wong VW, Akaishi S, Longaker MT, et al. Pushing back: wound mechanotransduction in repair and regeneration. J Invest Dermatol 2011; 131(11): 2186–2196. [DOI] [PubMed] [Google Scholar]
- 7. Arno AI, Gauglitz GG, Barret JP, et al. Up-to-date approach to manage keloids and hypertrophic scars: a useful guide. Burns J Int Soc Burn Inj 2014; 40(7): 1255–1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Atkinson J-AM, McKenna KT, Barnett AG, et al. A randomized, controlled trial to determine the efficacy of paper tape in preventing hypertrophic scar formation in surgical incisions that traverse Langer’s skin tension lines. Plast Reconstr Surg 2005; 116(6): 1648–1656; discussion 1657–1658. [DOI] [PubMed] [Google Scholar]
- 9. Widgerow AD, Chait LA, Stals R, et al. New innovations in scar management. Aesthetic Plast Surg 2000; 24(3): 227–234. [DOI] [PubMed] [Google Scholar]
- 10. Seifert O, Mrowietz U. Keloid scarring: bench and bedside. Arch Dermatol Res 2009; 301(4): 259–272. [DOI] [PubMed] [Google Scholar]
- 11. Toscano D, Arena D, Stella M, et al. Application of the TNM on Burn Scars: Integration with the Rehabilitation Protocol of the CTO of Turin - Clinical Case. 2016. Available at: https://eds.a.ebscohost.com/eds/detail/detail?vid=0&sid=12144680-f1c6-4770-a732-e7895df39238%40sessionmgr4006&bdata=JkF1dGhUeXBlPWlwLGF0aGVucyZzaXRlPWVkcy1saXZl#AN=118417956&db=ccm (accessed 20 November 2020).
- 12. Wong VW, Rustad KC, Akaishi S, et al. Focal adhesion kinase links mechanical force to skin fibrosis via inflammatory signaling. Nat Med 2011; 18(1): 148–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Aarabi S, Bhatt KA, Shi Y, et al. Mechanical load initiates hypertrophic scar formation through decreased cellular apoptosis. FASEB J 2007; 21(12): 3250–3261. [DOI] [PubMed] [Google Scholar]
- 14. Duscher D, Maan ZN, Wong VW, et al. Mechanotransduction and fibrosis. J Biomech 2014; 47(9): 1997–2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Costa AM, Peyrol S, Porto LCP, et al. Mechanical Forces Induce Scar Remodeling. Am J Pathol 1999; 155: 1671–1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chiang RS, Borovikova AA, King K, et al. Current concepts related to hypertrophic scarring in burn injuries. Wound Repair Regen 2016; 24(3): 466–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Chiquet M, Gelman L, Lutz R, et al. From mechanotransduction to extracellular matrix gene expression in fibroblasts. Biochim Biophys Acta 2009; 1793: 911–920. [DOI] [PubMed] [Google Scholar]
- 18. Kia KF, Burns MV, Vandergriff T, et al. Prevention of scar spread on trunk excisions: a rater-blinded randomized controlled trial. JAMA Dermatol 2013; 149(6): 687–691. [DOI] [PubMed] [Google Scholar]
- 19. Meyer M, McGrouther DA. A study relating wound tension to scar morphology in the pre-sternal scar using Langers technique. Br J Plast Surg 1991; 44: 291–294. [DOI] [PubMed] [Google Scholar]
- 20. Ogawa R, Okai K, Tokumura F, et al. The relationship between skin stretching/contraction and pathologic scarring: the important role of mechanical forces in keloid generation. Wound Repair Regen 2012; 20(2): 149–157. [DOI] [PubMed] [Google Scholar]
- 21. Rustad KC, Wong VW, Gurtner GC. The role of focal adhesion complexes in fibroblast mechanotransduction during scar formation. Differentiation 2013; 86(3): 87–91. [DOI] [PubMed] [Google Scholar]
- 22. Widgerow AD. Current concepts in scar evolution and control. Aesthetic Plast Surg 2011; 35(4): 628–635. [DOI] [PubMed] [Google Scholar]
- 23. Widgerow AD, Chait LA. Scar management practice and science: a comprehensive approach to controlling scar tissue and avoiding hypertrophic scarring. Adv Skin Wound Care 2011; 24(12): 555–561. [DOI] [PubMed] [Google Scholar]
- 24. Rosengren H, Askew DA, Heal C, et al. Does taping torso scars following dermatologic surgery improve scar appearance? Dermatol Pract Concept 2013; 3(2): 75–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Longaker MT, Rohrich RJ, Greenberg L, et al. A randomized controlled trial of the embrace advanced scar therapy device to reduce incisional scar formation. Plast Reconstr Surg 2014; 134(3): 536–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Moortgat P, Van Daele U, Anthonissen M, et al. Tension Reducing Taping as a Mechanotherapy for Hypertrophic Burn Scars - A Proof of Concept. Annals of Burns and Fire Disasters 2015. DOI: 10.13140/RG.2.1.2961.4564. [DOI] [Google Scholar]
- 27. Profyris C, Tziotzios C, Do Vale I. Cutaneous scarring: Pathophysiology, molecular mechanisms, and scar reduction therapeutics Part I. The molecular basis of scar formation. J Am Acad Dermatol 2012; 66(1): 1–10; quiz 11–2. [DOI] [PubMed] [Google Scholar]
- 28. Agha R, Ogawa R, Pietramaggiori G, et al. A review of the role of mechanical forces in cutaneous wound healing. J Surg Res 2011; 171(2): 700–708. [DOI] [PubMed] [Google Scholar]
- 29. Mustoe TA, Cooter RD, Gold MH, et al. International clinical recommendations on scar management. Plast Reconstr Surg 2002; 110(2): 560–571. [DOI] [PubMed] [Google Scholar]
- 30. Bush JA, Ferguson MWJ, Mason T, et al. Skin tension or skin compression? Small circular wounds are likely to shrink, not gape. J Plast Reconstr Aesthet Surg 2008; 61(5): 529–534. [DOI] [PubMed] [Google Scholar]
- 31. Rhett JM, Ghatnekar GS, Palatinus JA, et al. Novel therapies for scar reduction and regenerative healing of skin wounds. Trends Biotechnol 2008; 26(4): 173–180. [DOI] [PubMed] [Google Scholar]
- 32. Tollefson TT, Kamangar F, Aminpour S, et al. Comparison of effectiveness of silicone gel sheeting with microporous paper tape in the prevention of hypertrophic scarring in a rabbit model. Arch Facial Plast Surg 2012; 14(1): 45–51. [DOI] [PubMed] [Google Scholar]
- 33. Levi K, Ichiryu K, Kefel P, et al. Mechanics of wound closure: emerging tape-based wound closure technology vs. traditional methods. Cureus 2016; 8(10): e827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Reiffel RS. Prevention of hypertrophic scars by long-term paper tape application. Plast Reconstr Surg 1995; 96(7): 1715–1718. [DOI] [PubMed] [Google Scholar]
- 35. Karwacińska J, Kiebzak W, Stepanek-Finda B, et al. Effectiveness of Kinesio Taping on hypertrophic scars, keloids and scar contractures. Pol Ann Med 2012; 19(1): 50–57. [Google Scholar]
- 36. Gurtner GC, Dauskardt RH, Wong VW, et al. Improving cutaneous scar formation by controlling the mechanical environment: large animal and phase I studies. Ann Surg 2011; 254(2): 217–225. [DOI] [PubMed] [Google Scholar]
- 37. Wong VW, Longaker MT, Gurtner GC. Soft tissue mechanotransduction in wound healing and fibrosis. Semin Cell Dev Biol 2012; 23(9): 981–986. [DOI] [PubMed] [Google Scholar]
- 38. Huang Y, Chang K, Liou T, et al. Effects of Kinesio taping for stroke patients with hemiplegic shoulder pain: a double-blind, randomized, placebo-controlled study. J Rehabil Med 2017; 49(3): 208–215. [DOI] [PubMed] [Google Scholar]
- 39. Daya M. Abnormal scar modulation with the use of micropore tape. Eur J Plast Surg 2011; 34(1): 45–51. [Google Scholar]
- 40. Chen HH, Tsai WS, Yeh CY, et al. Prospective study comparing wounds closed with tape with sutured wounds in colorectal surgery. Arch Surg 2001; 136(7): 801–803. [DOI] [PubMed] [Google Scholar]
- 41. Kim H, Kim J, Choi J, et al. The Usefulness of Leukosan SkinLink for Simple Facial Laceration Repair in the Emergency Department. Arch Plast Surg 2015; 42(4): 431–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Doumit J, Vale R, Kanigsberg N. Dynaclose tape: a practical alternative to punch biopsy site closure. J Cutan Med Surg 2013; 17(1): 62–65. [DOI] [PubMed] [Google Scholar]
- 43. Widgerow AD, Chait LA, Stals PJ, et al. Multimodality Scar Management Program. Aesthetic Plast Surg 2009; 33(4): 533–543. [DOI] [PubMed] [Google Scholar]
- 44. Custis T, Armstrong AW, King TH, et al. Effect of Adhesive Strips and Dermal Sutures vs Dermal Sutures Only on Wound Closure: A Randomized Clinical Trial. JAMA Dermatol 2015; 151(8): 862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. van de Gevel DFD, Hamad MAS, Elenbaas TWO, et al. Is the use of Steri-StripTM S for wound closure after coronary artery bypass grafting better than intracuticular suture? Interact Cardiovasc Thorac Surg 2010; 10(4): 561–564. [DOI] [PubMed] [Google Scholar]
- 46. Yang S, Ozog D. Comparison of Traditional Superficial Cutaneous Sutures Versus Adhesive Strips in Layered Dermatologic Closures on the Back-A Prospective, Randomized, Split-Scar Study. Dermatol Surg 2015; 41(11): 1257–1263. [DOI] [PubMed] [Google Scholar]
- 47. Zempsky WT, Parrotti D, Grem C, et al. Randomized controlled comparison of cosmetic outcomes of simple facial lacerations closed with Steri Strip (TM) skin closures or Dermabond (TM) tissue adhesive. Pediatr Emerg Care 2004; 20(8): 519–24. [DOI] [PubMed] [Google Scholar]
- 48. van de Kar AL, Koolbergen DR, van Avendonk JPH, et al. Comparison of wound closure techniques in median sternotomy scars in children: subcuticular suture versus Steri-StripTM S. J Plast Surg Hand Surg 2019; 53(3): 161–166. [DOI] [PubMed] [Google Scholar]
- 49. Crofton E, Meredith P, Gray P, et al. Non-adherence with compression garment wear in adult burns patients: A systematic review and meta-ethnography. Burns 2020; 46(2): 472–482. [DOI] [PubMed] [Google Scholar]
- 50. Coghlan N, Copley J, Aplin T, et al. Patient Experience of Wearing Compression Garments Post Burn Injury: A Review of the Literature. J Burn Care Res 2017; 38(4): 260–269. [DOI] [PubMed] [Google Scholar]
- 51. Coghlan N, Copley J, Aplin T, et al. How to improve compression garment wear after burns: Patient and therapist perspectives. Burns 2019; 45(6): 1447–1455. [DOI] [PubMed] [Google Scholar]
- 52. Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 1998; 52(6): 377–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Sawada Y, Nihei Y, Urushidate S. Hydration and occlusion treatment for grafted skin on the hands of children. Eur J Plast Surg 1998; 21(7): 349–352. [Google Scholar]
- 54. Lin Y-S, Ting P-S, Hsu K-C. Comparison of Silicone Sheets and Paper Tape for the Management of Postoperative Scars: A Randomized Comparative Study. Adv Skin Wound Care 2020; 33(6): 1–6. [DOI] [PubMed] [Google Scholar]
- 55. Spieth PM, Kubasch AS, Penzlin AI, et al. Randomized controlled trials – a matter of design. Neuropsychiatr Dis Treat 2016; 12: 1341–1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Pannucci CJ, Wilkins EG. Identifying and Avoiding Bias in Research. Plast Reconstr Surg 2010; 126(2): 619–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Pearson A, Wiechula R, Court A, et al. The JBI model of evidence-based healthcare. Int J Evid Based Healthc 2005; 3(8): 207–215. [DOI] [PubMed] [Google Scholar]
- 58. Crofton E, Meredith P, Gray P, et al. Compression garment wear post-burn: measurement of how I “feel” through quantitative and self-report sensory variables impacts upon wear, a single-site study. Burns 2020; 46(8): 1903–1913. [DOI] [PubMed] [Google Scholar]
How to cite this article
- O’Reilly S, Crofton E, Brown J, Strong J, Ziviani J. Use of tape for the management of hypertrophic scar development: A comprehensive review. Scars, Burns & Healing, Volume 7, 2021. DOI: 10.1177/ 20595131211029206. [DOI] [PMC free article] [PubMed] [Google Scholar]