Abstract
Objective
To assess the association between learning disability and risk of hospital admission and death from covid-19 in England among adults and children.
Design
Population based cohort study on behalf of NHS England using the OpenSAFELY platform.
Setting
Patient level data were obtained for more than 17 million people registered with a general practice in England that uses TPP software. Electronic health records were linked with death data from the Office for National Statistics and hospital admission data from NHS Secondary Uses Service.
Participants
Adults (aged 16-105 years) and children (<16 years) from two cohorts: wave 1 (registered with a TPP practice as of 1 March 2020 and followed until 31 August 2020); and wave 2 (registered 1 September 2020 and followed until 8 February 2021). The main exposure group consisted of people on a general practice learning disability register; a subgroup was defined as those having profound or severe learning disability. People with Down’s syndrome and cerebral palsy were identified (whether or not they were on the learning disability register).
Main outcome measure
Covid-19 related hospital admission and covid-19 related death. Non-covid-19 deaths were also explored.
Results
For wave 1, 14 312 023 adults aged ≥16 years were included, and 90 307 (0.63%) were on the learning disability register. Among adults on the register, 538 (0.6%) had a covid-19 related hospital admission; there were 222 (0.25%) covid-19 related deaths and 602 (0.7%) non-covid deaths. Among adults not on the register, 29 781 (0.2%) had a covid-19 related hospital admission; there were 13 737 (0.1%) covid-19 related deaths and 69 837 (0.5%) non-covid deaths. Wave 1 hazard ratios for adults on the learning disability register (adjusted for age, sex, ethnicity, and geographical location) were 5.3 (95% confidence interval 4.9 to 5.8) for covid-19 related hospital admission and 8.2 (7.2 to 9.4) for covid-19 related death. Wave 2 produced similar estimates. Associations were stronger among those classified as having severe to profound learning disability, and among those in residential care. For both waves, Down’s syndrome and cerebral palsy were associated with increased hazards for both events; Down’s syndrome to a greater extent. Hazard ratios for non-covid deaths followed similar patterns with weaker associations. Similar patterns of increased relative risk were seen for children, but covid-19 related deaths and hospital admissions were rare, reflecting low event rates among children.
Conclusions
People with learning disability have markedly increased risks of hospital admission and death from covid-19, over and above the risks observed for non-covid causes of death. Prompt access to covid-19 testing and healthcare is warranted for this vulnerable group, and prioritisation for covid-19 vaccination and other targeted preventive measures should be considered.
Introduction
Identifying high risk groups for severe outcomes from covid-19 is critically important for risk stratification, which informs vaccine prioritisation initiatives and other targeted preventive measures. People with learning disability, who total more than one million people in England alone or 2% of the adult population, are one such vulnerable group.1 People with learning disability have a lower intellectual ability (usually IQ<70) and impaired social and adaptive functioning, with the onset in childhood. Learning disabilities are usually classified using a wide severity range (mild, moderate, severe, or profound), and consequently intensity of support needs differs widely.
As of February 2021, the Learning from Death Reviews programme reported that 1405 people with a learning disability had died from covid-19 in England since February 2020.2 The true number is probably far higher because of gaps in learning disability registration. The latest estimates from 2015 suggest that 23% of people with learning disability are included on the learning disability register.1 Emerging evidence from the first wave of the covid-19 pandemic in the United Kingdom showed that people with learning disability were at higher risk from mortality3 4 5 6 7 than people in the general population. For instance, the Oxford RCGP Research and Surveillance Centre sentinel network reported an odds ratio of 1.96 (95% confidence interval 1.22 to 3.18) for mortality during the first wave of infection in the UK among people with learning disability compared with those without.4 People with Down’s syndrome might be at particularly high risk; an analysis of primary care data from eight million adults reported a hazard ratio of 10.4 (7.1 to 15.2) for covid-19 death associated with Down’s syndrome.8 However, existing studies on the association of learning disability with severe outcomes from covid-19 do not include the second wave of the pandemic. Additionally, these studies frequently adjusted for variables that might be partly a consequence of the learning disability, such as deprivation and comorbidities, complicating interpretation of the results.4 A lack of clarity also exists on the increased risk of covid-19 deaths among people with milder learning disability, and this aspect needs exploration.9
The higher risk of premature death among people with learning disability in England is well known1 10 and triggered the establishment of general practice learning disability registers to allow for better provision of their healthcare. A number of mechanisms exist which could increase the risk of covid-19 mortality in this group. People with learning disability have a higher prevalence of covid-19 mortality risk factors, including obesity, diabetes, epilepsy, and poverty.11 12 13 Medical conditions underlying the learning disability might confer additional risk; for instance, people with Down’s syndrome are more vulnerable to impaired cellular immunity, congenital heart disease, and respiratory conditions.14 15 Many people with learning disability in England live in residential care or supported accommodation, or receive community based social care16; therefore, they have frequent contact with carers and other care recipients, and face challenges in physical distancing. Difficulties understanding the protective measures needed, compounded by a lack of accessible information, further increase the vulnerability of this group to infection.17 Healthcare access and quality, including prevention and treatment, are frequently worse for people with learning disability, leading to avoidable deaths.10 Treatment failures,10 including do not resuscitate orders,18 might increase their risk of death once infected.
Until 24 February 2021, the national recommendations for prioritisation of covid-19 vaccination in England included all adults with cerebral palsy, severe to profound learning disability, Down’s syndrome, and the whole resident population in care settings where a high proportion of residents would be eligible for vaccination (for example, due to learning disability).19 20 This guidance means that not everyone on the learning disability register would be eligible for covid-19 vaccination, including people with mild to moderate learning disability from causes other than Down’s syndrome or cerebral palsy who are not living in residential care. This work was undertaken rapidly in response to an urgent need to inform policy making on vaccination prioritisation in the UK and elsewhere.
The aim of this study was to use linked electronic health records within the OpenSAFELY platform to rapidly describe the risk of covid-19 related hospital admissions and deaths among children and adults with learning disability in England compared with the general population. A subsidiary aim was to separate the risk by type of learning disability (severe to profound, cerebral palsy, Down’s syndrome, on the learning disability register), including people with learning disability not originally included in the first six groups of the phase 1 vaccination priority list in the UK.
Methods
Study design
We performed two population based, observational cohort studies of patients in England using data within the OpenSAFELY platform.
Data
We used data from primary care linked to secondary care and mortality records in England. Records were linked to the NHS England inpatient activity datasets from Secondary Uses Service (SUS) data extracts, including data from inpatient activity datasets for determining covid-19 related hospital admissions.21 Office for National Statistics (ONS) death data were used to determine covid-19 related deaths. The dataset analysed within OpenSAFELY is based on 24 million people currently registered with general practice surgeries that use TPP SystmOne software—approximately 40% of the population in England. All data are pseudonymised and include coded diagnoses (using Read version 3, CTV3 codes), drugs, and physiological parameters. No free text data are included. The OpenSAFELY platform is a new data source and validation studies are not yet available. Other datasets based on primary care records in England have been shown to have high validity.22
Study population
The first cohort comprised male and female patients (aged ≤105 years) registered as of 1 March 2020 in a general practice that uses the TPP system and followed until 31 August 2020. We excluded patients with missing age or a recorded age >105 years, missing sex, or missing postcode (from which much of the household and geographical information is calculated). Patients in the second cohort were similarly defined, but included those registered as of 1 September 2020 and followed until 8 February 2021. Patients in the two cohorts might differ slightly due to patients leaving and joining TPP practices, and patients dying prior to the start of the second cohort. These two time periods correspond to the two main waves of covid-19 infection experienced in England during 2020.23 In particular, 1 September 2020 had the lowest daily number of covid-19 related deaths since the start of the pandemic.24
Exposures
All codelists used to define exposure groups are provided online, with links given in the supplementary appendix. The main exposure group comprised people on the learning disability register. This register contains a subset of people with learning disability; it is not a comprehensive list. However, the register provides a simple and practical means of identifying people for vaccine prioritisation or implementation of other public health measures. A subset of the codes used to define the learning disability register classified the learning disability as severe to profound, and were used to classify a subset of patients as having severe to profound learning disability.
Because a comprehensive indicator of residential care is lacking, those living in a household containing at least five people identified as being on the learning disability register were classed as being in residential care. Households were identified based on general practice registered addresses as of 1 February 2020, standardised and corrected using publicly available house sale data to remove registrations that are probably not current. We use the term residential care throughout, although we note that this includes a range of settings (care homes, educational settings, sheltered accommodation) and misclassification also probably exists. People with Down’s syndrome and cerebral palsy were identified based on general practice codes, which were reviewed by clinicians specialising in the care of people with learning disability (details in supplementary appendix).
Outcomes
The outcomes for this study are covid-19 related death (defined as a covid-19 ICD-10 (international classification of diseases, 10th revision) code of U07.1 or U07.2 anywhere on the death certificate, determined from ONS death certificate data), and covid-19 related hospital admission (defined as admissions with any ICD-10 admission diagnosis, not restricted to primary diagnosis, of U07.1 or U07.2, determined from SUS data). People who had a covid-19 related hospital admission and then died contributed to both outcomes. An additional outcome of non-covid-19 death was also considered, determined from ONS death certificate data and excluding deaths classed as covid-19 related.
Covariates
Covariates included demographics (age, sex, ethnicity, and geographical area), which could act as potential confounders, and current deprivation (index of multiple deprivation) as a potential mediator. To consider mediation by physical comorbidities that are also indications for vaccination we included body mass index ≥40, chronic cardiac disease, atrial fibrillation, deep vein thrombosis or pulmonary embolism, diabetes (further grouped by level of control, as measured by the latest glycated haemoglobin (HbA1c) measurement or lack of a measurement), chronic liver disease, stroke, transient ischaemic attack, dementia, asthma requiring use of oral corticosteroids, other chronic respiratory disease, reduced kidney function, dialysis, organ transplant, asplenia, other conditions leading to immunosuppression, and haematological cancer. We also included non-haematological cancer diagnosed in the past year, rheumatoid arthritis or lupus or psoriasis, and inflammatory bowel disease as common indications for immunosuppressing drugs. These conditions aim to map to the existing physical indications for vaccination among people aged 16-64 years in England; however data on epilepsy were not available for this analysis. We also identified other neurological conditions and serious mental illness to exclude people already prioritised for vaccination. We obtained these measures from medical records (details in supplementary appendix).
Statistical methods
Analysis was undertaken separately for adults aged ≥16 years and children aged <16 years. We repeated analyses for the following exposures: being on the learning disability register (total, then divided into severe to profound v mild to moderate, and residential care v non-residential care), Down’s syndrome, and cerebral palsy.
The two cohorts for each wave were analysed separately. We used Cox proportional hazards for covid-19 related mortality and covid-19 related hospital admission, stratified by local geographical area as measured by the Sustainability and Transformation Partnership to account for differing patterns of infection over time in different regions, with days in study as the timescale. Follow-up was censored at competing events (non-covid death for mortality analyses and any cause death for hospital admission analyses) to target the cause specific hazard. Models adjusted for confounders (age, sex, ethnicity), additionally for deprivation, residential care status and physical comorbidities (described above), and then adjusted for all of these factors simultaneously. We explored exposure interactions with broad age ranges (16-64, 65-74, ≥75), sex, and deprivation. Tests based on Schoenfeld residuals were used to assess the proportional hazards assumption.
Similar Cox models were fitted for covid-19 related hospital admissions, after excluding people who were already prioritised for vaccination because of age or comorbidities as part of the first six priority groups of phase 1 in the UK. These were people aged ≥65 years and people with codes for physical conditions indicating priority for vaccination, other neurological conditions, severe mental illness, Down’s syndrome, cerebral palsy, and severe to profound learning disability. These Cox models adjusted for the confounders, then separately for deprivation and residential care status. Finally, Cox models for non-covid deaths were fitted, adjusting for the same variables as previous models.
For children <16 years, these analyses were undertaken separately. We omitted analyses looking at death, full adjustment for comorbidities, and interaction analyses because of smaller numbers of outcomes.
Missing data
The main analysis took a complete case approach for missing ethnicity data (around 25% of records). Previous analyses using these data suggest the assumption required for complete case analysis for ethnicity—that missingness is unrelated to outcome given covariates—is approximately satisfied here.12
There were also missing data for body mass index, serum creatinine, and HbA1c measurements. For each of these variables, previous research into their recording in UK primary care records suggested that multiple imputation would not be appropriate because the assumption that the data are missing at random is not met: for example, people who are underweight and overweight will be more likely to have their body mass index recorded in primary care25; serum creatinine measurement typically reflects monitoring because of underlying risk factors for chronic kidney disease or a known diagnosis26; and social disparities in monitoring of HbA1c among people with diabetes.27 People with missing body mass index were assumed to be non-obese. People with no serum creatinine measurement were included in the category “no evidence of poor kidney function,” an approach which has been found to produce prevalence estimates of chronic kidney disease comparable to those from other sources.28 When categorising people with diabetes according to glycaemic control, those with no HbA1c measurement were included in a separate group “diabetes, no Hba1c” as an indicator for diabetes with poorly monitored glycaemic control.
We undertook two sensitivity analyses. Firstly, multiple imputation was performed, creating 10 imputed datasets separately for adults and children, and imputing ethnicity using a multinomial regression model that included all covariates, outcome indicators, and a Nelson-Aalen estimate of the cumulative hazard in the imputation model. Estimates were combined by using Rubin’s rules. Secondly, a complete case analysis was performed discarding people with no body mass index measurement; when data are missing not at random, complete case analysis might be less biased than multiple imputation.29
Software and reproducibility
The prespecified study protocol is archived with version control (https://github.com/opensafely/Published-Protocols/blob/master/Learning_Disability_Covid_Protocol_2021_10_02.pdf). All code and codelist data are shared openly for review and reuse under the MIT open license (https://github.com/opensafely/absolute-risks-covid-research, https://codelists.opensafely.org/). The OpenSAFELY framework guarantees that the analytic code, clinical codelists, data processing logic, and all dependent libraries remain available and executable against randomly generated dummy data. The full analysis can be rerun against real data with one click by any person with the necessary information governance approvals.
Patient and public involvement
We have developed a publicly available website (https://opensafely.org/) through which we invite any patient or member of the public to contact us about this study or the broader OpenSAFELY project. We were not able to undertake extensive patient or public involvement during the short time frame for producing results. However, we did consult with three clinicians specialising in the care of people with learning disabilities. An online Health Protection Research Unit (HPRU) in Vaccines and Immunisation public engagement event in December 2020 discussing the use of pseudonymised medical records to investigate who is at higher risk of severe covid-19 found that this research approach was supported and expected as part of the pandemic response.
Results
Table 1 shows the baseline characteristics of people included in the analysis, given separately for those aged ≥16 years and those aged <16 years (characteristics in wave 2 were similar). Figure A1 in the supplementary appendix shows a flowchart of participant numbers through the study selection process.
Table 1.
Baseline characteristics of adults and children in main analysis (with complete ethnicity data). Data are numbers (%)
| Characteristics | Adults (≥16 years) | Children (<16 years) | |||
|---|---|---|---|---|---|
| On learning disability register | Not on learning disability register | On learning disability register | Not on learning disability register | ||
| Total | 90 307 (100) | 14 221 716 (100) | 9298 (100) | 2 617 720 (100) | |
| Age group | |||||
| 0-15 | 0 (0) | 0 (0) | 9298 (100) | 2 617 720 (100) | |
| 16-44 | 52 333 (58) | 6 360 525 (45) | 0 (0) | 0 (0) | |
| 45-64 | 29 114 (32) | 4 633 383 (33) | 0 (0) | 0 (0) | |
| 65-69 | 3870 (4) | 889 199 (6) | 0 (0) | 0 (0) | |
| 70-74 | 2704 (3) | 894 793 (6) | 0 (0) | 0 (0) | |
| 75-79 | 1371 (2) | 622 787 (4) | 0 (0) | 0 (0) | |
| ≥80 | 915 (1) | 821 029 (6) | 0 (0) | 0 (0) | |
| Sex | |||||
| Female | 36 801 (41) | 7 356 253 (52) | 3013 (32) | 1 276 612 (49) | |
| Male | 53 506 (59) | 6 865 463 (48) | 6285 (68) | 1 341 108 (51) | |
| Ethnicity | |||||
| White | 81 261 (90) | 12 044 684 (85) | 7120 (77) | 2 071 494 (79) | |
| Black | 1710 (2) | 402 235 (3) | 379 (4) | 96 181 (4) | |
| South Asian | 5499 (6) | 1 179 377 (8) | 1271 (14) | 279 286 (11) | |
| Mixed | 1125 (1) | 206 860 (1) | 307 (3) | 99 517 (4) | |
| Other | 712 (1) | 388 560 (3) | 221 (2) | 71 242 (3) | |
| Region | |||||
| East | 18 479 (20) | 3 280 536 (23) | 1850 (20) | 618 211 (24) | |
| London | 3619 (4) | 1 166 888 (8) | 565 (6) | 167 329 (6) | |
| Midlands | 21 480 (24) | 3 162 698 (22) | 2202 (24) | 609 609 (23) | |
| North East, Yorkshire and The Humber | 19 655 (22) | 2 709 851 (19) | 2071 (22) | 493 405 (19) | |
| North West | 10 228 (11) | 1 243 972 (9) | 981 (11) | 224 084 (9) | |
| South East | 5256 (6) | 862 061 (6) | 570 (6) | 170 246 (7) | |
| South West | 11 590 (13) | 1 795 710 (13) | 1059 (11) | 334 836 (13) | |
| Index of multiple deprivation | |||||
| 1 (least deprived) | 9719 (11) | 2 804 359 (20) | 1239 (13) | 486 452 (19) | |
| 2 | 13 589 (15) | 2 850 388 (20) | 1373 (15) | 464 177 (18) | |
| 3 | 17 339 (19) | 2 910 085 (20) | 1648 (18) | 492 125 (19) | |
| 4 | 21 635 (24) | 2 877 452 (20) | 2116 (23) | 533 117 (20) | |
| 5 (most deprived) | 28 025 (31) | 2 779 432 (20) | 2922 (31) | 641 849 (25) | |
| Learning disability and related | |||||
| Mild-moderate learning disability | 74 116 (82) | — | 7909 (85) | — | |
| Severe-profound learning disability | 16 191 (18) | — | 1389 (15) | — | |
| Not in residential care* | 82 274 (91) | 14 220 351 (100) | 9235 (99) | 2 617 669 (100) | |
| Residential care* | 8033 (9) | 1365 (<1) | 63 (1) | 51 (<1) | |
| No Down’s syndrome | 83 179 (92) | 14 220 854 (100) | 8387 (90) | 2 615 994 (100) | |
| Down’s syndrome | 7128 (8) | 862 (<1) | 911 (10) | 1726 (<1) | |
| No cerebral palsy | 83 357 (92) | 14 210 368 (100) | 8789 (95) | 2 613 598 (100) | |
| Cerebral palsy | 6950 (8) | 11 348 (<1) | 509 (5) | 4122 (<1) | |
| Comorbidities | |||||
| Body mass index≥40 | 5897 (7) | 382 625 (3) | 71 (1) | 4412 (<1) | |
| Asthma (with OCS use) | 879 (1) | 129 455 (1) | — | — | |
| Cystic fibrosis | 35 (<1) | 3731 (<1) | — | — | |
| Respiratory disease | 3521 (4) | 574 387 (4) | — | — | |
| Chronic cardiac disease | 5637 (6) | 915 988 (6) | — | — | |
| Atrial fibrillation | 2311 (3) | 507 890 (4) | — | — | |
| Deep vein thrombosis or pulmonary embolism | 2072 (2) | 291 929 (2) | — | — | |
| Diabetes | |||||
| With HbA1c <58 mmol/mol | 6793 (8) | 855 216 (6) | — | — | |
| With HbA1c ≥58 mmol/mol | 3417 (4) | 401 014 (3) | — | — | |
| With no recent HbA1c measure | 1324 (1) | 160 068 (1) | — | — | |
| Liver disease | 459 (1) | 85 620 (1) | — | — | |
| Stroke | 1966 (2) | 287 098 (2) | — | — | |
| Transient ischaemic attack | 931 (1) | 217 105 (2) | — | — | |
| Dementia | 1887 (2) | 169 050 (1) | — | — | |
| Other neurological disease | 8857 (10) | 129 745 (1) | — | — | |
| Poor kidney function | |||||
| Stage 3a/3b, eGFR 30-60 | 2817 (3) | 714 502 (5) | — | — | |
| Stage 4/5, eGFR <30 | 518 (1) | 68 534 (<1) | — | — | |
| Dysplenia | 141 (<1) | 23 082 (<1) | — | — | |
| Organ transplant | 191 (<1) | 12 990 (<1) | — | — | |
| Conditions leading to immunosuppression | 484 (1) | 40 802 (<1) | — | — | |
| Haematological malignancy | |||||
| Diagnosed in past year | 25 (<1) | 7138 (<1) | — | — | |
| Diagnosed 2-5 years ago | 80 (<1) | 21 673 (<1) | — | — | |
| Diagnosed >5 years ago | 283 (<1) | 49 569 (<1) | — | — | |
| Cancer (non-haematological) in past year | 196 (<1) | 63 011 (<1) | — | — | |
| RA/SLE/psoriasis | 4277 (5) | 710 575 (5) | — | — | |
| Inflammatory bowel disease | 871 (1) | 178 869 (1) | — | — | |
| Serious mental illness | 8026 (9) | 168 342 (1) | — | — | |
eGFR=estimated glomerular filtration rate; HbA1c=glycated haemoglobin; OCS=oral corticosteroid; RA=rheumatoid arthritis; SLE=systemic lupus erythematosus.
Living in household containing at least five people identified as being on learning disability register.
Among 14 312 023 adults aged ≥16 years, 90 307 (0.63%) were identified as being on the learning disability register (table 1). The largest group consisted of people with mild to moderate learning disability (74 116, 82%). Additionally, 16 191 (18%) were identified as having severe to profound learning disability, and 8033 (9%) as being in residential care. In total, 7990 adults were identified as having Down’s syndrome, of whom 7128 (89%) were on the learning disability register; 18 298 adults were identified as having cerebral palsy, of whom 6950 (38%) were on the learning disability register. Those on the learning disability register were more likely to be male, younger, and living in more deprived areas. Comorbidities were similar across groups; more people with diabetes, obesity, other neurological disease, and diagnoses of serious mental illness were among those on the learning disability register.
Among 2 627 018 children aged <16 years (table 1), 9298 (0.35%) were identified as being on the learning disability register. Of the 2637 children identified as having Down’s syndrome, only 911 (35%) were on the learning disability register. Of the 4631 children identified as having cerebral palsy, 509 (11%) were on the learning disability register.
Covid-19 related hospital admissions and deaths among adults ≥16 years
Adults aged ≥16 years were followed up for 7.1 million person years (mean 0.5 years per person) during wave 1 (1 March 2020-31 August 2020; 183 days). Among adults on the learning disability register, 538 (0.6%) had a covid-19 related hospital admission; there were 222 (0.25%) covid-19 related deaths and 602 (0.7%) non-covid deaths. Among adults not on the register, 29 781 (0.2%) had a covid-19 related hospital admission; there were 13 737 (0.1%) covid-19 related deaths and 69 837 (0.5%) non-covid deaths.
Adults were followed up for 6.3 million person years (mean 0.4 years per person) during wave 2 (1 September 2020-8 February 2021; 160 days). Among 91 358 adults on the learning disability register, 1004 (1.1%) had a covid-19 related hospital admission; there were 286 (0.3%) covid-19 related deaths and 524 (0.6%) non-covid deaths. Among 14 260 586 adults not on the register, 63 053 (0.4%) had a covid-19 related hospital admission; there were 19 778 (0.1%) covid-19 related deaths and 58 021 (0.4%) non-covid deaths.
Figure 1 shows cumulative covid-19 related deaths and hospital admissions among adults during the study period, accounting for sex, age, and ethnicity for people on the learning disability register and those who were not. Both graphs show a clear increase in events among those on the learning disability register, with a flattening off apparent during the period between waves of infection.
Fig 1.
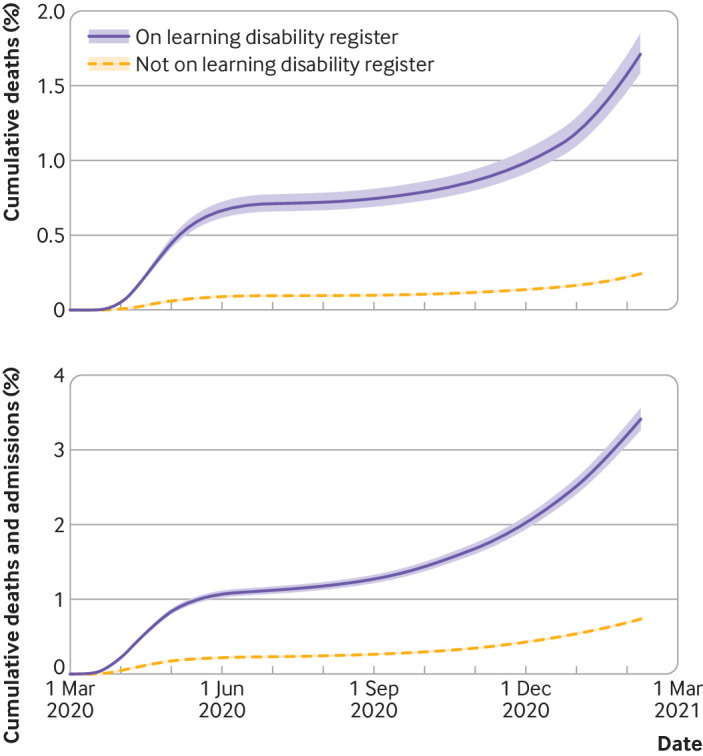
Cumulative covid-19 related deaths, and covid-19 related hospital admissions and deaths with 95% confidence intervals for adults aged ≥16 years through two waves of infection. People on learning disability register and those not on register shown separately. Estimates are standardised by age, sex, and ethnicity
Covid-19 related hospital admissions and deaths among children <16 years
Among children <16 years, 286 covid-19 related hospital admissions occurred in wave 1 during 1.3 million person years of follow-up (mean 0.5 years per person) and 529 in wave 2 during 1.1 million person years of follow-up (mean 0.4 years per person). Among 9298 children on the learning disability register during wave 1, there were five or fewer (≤0.05%) covid-19 related hospital admissions; we cannot provide the exact number because of stringent redaction rules applied to protect patient privacy. Among 9429 children on the learning disability register during wave 2, there were 20 (0.2%) covid-19 related hospital admissions. In total, across both waves, there were nine non-covid deaths among children on the register and 151 non-covid deaths among children not on the register. For covid-19 related deaths, there were five or fewer among children on the register and five or fewer among those not on the register. The number of deaths classed as covid-19 related was low among children overall.
Hazard ratios for covid-19 hospital admissions and deaths among adults ≥16 years
For wave 1, the estimated hazard ratio for covid-19 related hospital admission among adults on the learning disability register (adjusted for age, sex, ethnicity, and geographical location) was 5.3 (95% confidence interval 4.9 to 5.8; table 2). The hazard ratio for covid-19 related death was 8.2 (7.2 to 9.4). Wave 2 produced similar estimates (4.3, 4.1 to 4.6 for covid-19 related hospital admission; 7.2, 6.4 to 8.1 for covid-19 related death). These associations were stronger among those with learning disability classed as severe to profound and among those in residential care. Down’s syndrome was associated with increased hazard of both events in both waves (wave 1: 10.6, 8.5 to 13.2 for covid-19 related hospital admission; 36.3, 26.7 to 49.5 for covid-19 related death; similar numbers were found for wave 2). Cerebral palsy was associated with higher hazards but to a lesser extent (wave 1: 5.0, 3.9 to 6.4 for covid-19 related hospital admission; 5.8, 4.1 to 8.3 for covid-19 related death; similar numbers were found for wave 2).
Table 2.
Estimated hazard ratios for covid-19 outcomes among adults ≥16 years and children <16 years adjusted for potential confounders (age, sex, ethnicity, geographical region)
| Exposure category | Covid-19 related hospital admission | Covid-19 related death | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Events | Person years | Crude rate* (95% CI) | Hazard ratio (95% CI) | Events | Person years | Crude rate* (95% CI) | Hazard ratio (95% CI) | ||
| Wave 1: adults (≥16 years) | |||||||||
| Learning disability register | |||||||||
| No | 29 781 | 7 133 803 | 4.2 (4.1 to 4.2) | Reference | 13 737 | 7 140 988 | 1.9 (1.9 to 2.0) | Reference | |
| Yes | 538 | 45 126 | 11.9 (11.0 to 13.0) | 5.30 (4.85 to 5.80) | 222 | 45 257 | 4.9 (4.3 to 5.6) | 8.21 (7.15 to 9.42) | |
| Severity (learning disability register) | |||||||||
| Mild | 391 | 37 070 | 10.5 (9.6 to 11.6) | 4.74 (4.30 to 5.23) | 159 | 37 167 | 4.3 (3.7 to 5.0) | 7.15 (6.12 to 8.34) | |
| Profound | 147 | 8056 | 18.2 (15.5 to 21.4) | 7.75 (6.43 to 9.33) | 63 | 8090 | 7.8 (6.1 to 10.0) | 13.14 (9.94 to 17.39) | |
| Residential care status | |||||||||
| Not in residential care | 438 | 41 141 | 10.6 (9.7 to 11.7) | 4.87 (4.44 to 5.34) | 182 | 41 249 | 4.4 (3.8 to 5.1) | 7.81 (6.77 to 9.02) | |
| In residential care | 100 | 3984 | 25.1 (20.6 to 30.5) | 8.72 (6.77 to 11.25) | 40 | 4008 | 10.0 (7.3 to 13.6) | 10.65 (7.08 to 16.03) | |
| Down’s syndrome | |||||||||
| No | 30 244 | 7 174 961 | 4.2 (4.2 to 4.3) | Reference | 13 918 | 7 182 261 | 1.9 (1.9 to 2.0) | Reference | |
| Yes | 75 | 3968 | 18.9 (15.1 to 23.7) | 10.59 (8.47 to 13.23) | 41 | 3983 | 10.3 (7.6 to 14.0) | 36.34 (26.67 to 49.51) | |
| Cerebral palsy | |||||||||
| No | 30 221 | 7 169 773 | 4.2 (4.2 to 4.3) | Reference | 13 929 | 7 177 063 | 1.9 (1.9 to 2.0) | Reference | |
| Yes | 98 | 9156 | 10.7 (8.8 to 13.0) | 4.95 (3.86 to 6.36) | 30 | 9181 | 3.3 (2.3 to 4.7) | 5.83 (4.12 to 8.26) | |
| Wave 1: children (<16 years) | |||||||||
| Learning disability register | |||||||||
| No | >200† | 1 318 599 | 0.2 (0.2 to 0.2) | Reference | —‡ | —‡ | —‡ | —‡ | |
| Yes | ≥5† | 4700† | 1.1 (0.4 to 2.6) | 6.21 (2.75 to 14.05) | —‡ | —‡ | —‡ | —‡ | |
| Wave 2: adults (≥16 years) | |||||||||
| Learning disability register | |||||||||
| No | 63 053 | 6 262 945 | 10.1 (10.0 to 10.1) | Reference | 19 778 | 6 270 857 | 10.1 (10.0 to 10.1) | Reference | |
| Yes | 1004 | 40 002 | 25.1 (23.6 to 26.7) | 4.32 (4.05 to 4.61) | 286 | 40 121 | 25.1 (23.6 to 26.7) | 7.22 (6.41 to 8.13) | |
| Severity (learning disability register) | |||||||||
| Mild | 722 | 32 856 | 22 (20.4 to 23.6) | 3.82 (3.55 to 4.11) | 197 | 32 943 | 22.0 (20.4 to 23.6) | 6.07 (5.29 to 6.96) | |
| Profound | 282 | 7146 | 39.5 (35.1 to 44.3) | 6.52 (5.77 to 7.37) | 89 | 7177 | 39.5 (35.1 to 44.3) | 12.42 (10.06 to 15.33) | |
| Residential care status | |||||||||
| Not in residential care | 813 | 36 637 | 22.2 (20.7 to 23.8) | 3.92 (3.64 to 4.21) | 231 | 36 735 | 22.2 (20.7 to 23.8) | 6.73 (5.91 to 7.66) | |
| In residential care | 191 | 3365 | 56.8 (49.3 to 65.4) | 7.73 (6.51 to 9.19) | 55 | 3385 | 56.8 (49.3 to 65.4) | 10.37 (7.61 to 14.12) | |
| Down’s syndrome | |||||||||
| No | 63 898 | 6 299 465 | 10.1 (10.1 to 10.2) | Reference | 19 998 | 6 307 480 | 10.1 (10.1 to 10.2) | Reference | |
| Yes | 159 | 3482 | 45.7 (39.1 to 53.3) | 9.66 (8.28 to 11.27) | 66 | 3498 | 45.7 (39.1 to 53.3) | 38.50 (30.13 to 49.18) | |
| Cerebral palsy | |||||||||
| No | 63 865 | 6 294 857 | 10.1 (10.1 to 10.2) | Reference | 20 030 | 6 302 862 | 10.1 (10.1 to 10.2) | Reference | |
| Yes | 192 | 8,090 | 23.7 (20.6 to 27.3) | 4.23 (3.67 to 4.87) | 34 | 8116 | 23.7 (20.6 to 27.3) | 4.40 (3.14 to 6.17) | |
| Wave 2: children (<16 years) | |||||||||
| Learning disability register | |||||||||
| No | 509 | 1 137 827 | 0.4 (0.4 to 0.5) | Reference | —‡ | —‡ | —‡ | —‡ | |
| Yes | 20 | 4152 | 4.8 (3.1 to 7.5) | 9.18 (5.89 to 14.29) | —‡ | —‡ | —‡ | —‡ | |
Wave 1: 1 March 2020-31 August 2020; wave 2: 1 September 2020-8 February 2021.
Per 1000 person years.
Rounded to avoid inadvertent disclosure of small event numbers. Median person years (25th-75th percentile): 0.504 (0.504 to 0.504) in wave 1 and 0.44 (0.44 to 0.44) in wave 2 for children and adults.
Insufficient events for analysis.
Further adjustment for deprivation, residential care, and physical comorbidities only slightly attenuated these associations (supplementary appendix). For wave 1, the confounder adjusted hazard ratio for covid-19 related hospital admission for those on the learning disability register was 5.3 (95% confidence interval 4.9 to 5.8), reducing to 3.9 (3.6 to 4.3) after full adjustment. However, for Down’s syndrome, adjustment for residential care and comorbidities greatly attenuated hazard ratios (for example, the wave 1 hazard ratio for covid-19 related hospital admission reduced from 10.6 (8.5 to 13.2) to 6.4 (4.9 to 8.3) after adjustment for residential care, 7.2 (5.8 to 9.0) after adjustment for physical comorbidities, and 4.7 (3.6 to 6.0) after adjustment for all factors.
Tests of the proportional hazards assumption showed some evidence of non-proportionality (P values <0.001 for covid-19 related death and 0.176 for covid-19 related hospital admission in wave 1; corresponding values for wave 2 were 0.12 and 0.09, respectively). Therefore, the results reflect average hazard ratios over the follow-up periods.
Hazard ratios for covid-19 hospital admission among children <16 years
Among children <16 years, being on the learning disability register was associated with increased hazard of covid-19 related hospital admission (wave 1: hazard ratio 6.2, 95% confidence interval 2.8 to 14.1; wave 2: 9.2, 5.9 to 14.3).
Effect modification among adults ≥16 years
In wave 1, an interaction was observed between age and being on the learning disability register on the hazard of covid-19 related death: hazard ratio for being on the learning disability register 12.3, 95% confidence interval 10.0 to 15.1 for people aged 16-64; 10.5, 8.3 to 13.2 for people aged 65-74; and 4.2, 3.2 to 5.5 for people aged ≥75; similar estimates were observed for wave 2 (supplementary appendix). A similar interaction was not observed for covid-19 related hospital admission in waves 1 or 2. No interaction was observed by sex. Larger hazard ratios for covid-19 related hospital admission and death were observed for adults living in the least deprived areas compared with those in the more deprived areas, with similar patterns seen in both waves. Insufficient data were available to explore interactions by ethnicity.
Hazard ratios among adults ≥16 years not prioritised for vaccination
After excluding people aged ≥65 years and those with defined comorbidities, the estimated hazard of covid-19 related hospital admission was 4.1 (95% confidence interval 3.3 to 5.2) after adjustment for age, sex, ethnicity, and geographical location, with little change after adjustment for deprivation or residential care status. Slightly attenuated associations were seen in wave 2 (3.0, 2.5 to 3.5) after adjustment for age, sex, ethnicity, and geographical location.
Hazard ratios for non-covid death among adults ≥16 years
The estimated hazard ratio for non-covid death among adults (adjusted for age, sex, ethnicity, and geographical location) was 3.7 (95% confidence interval 3.4 to 4.0) in wave 1 and 4.0 (3.7 to 4.3) in wave 2. Associations were stronger among those classed as having severe to profound learning disability. Associations were slightly stronger among those classed as being in residential care. Down’s syndrome was associated with an increased hazard of non-covid death (wave 1: 12.3, 9.9 to 15.1; similar numbers were observed for wave 2). Cerebral palsy was associated with higher hazards to a lesser extent (wave 1: 3.2, 2.6 to 3.9 for covid-19 related death; similar numbers were observed for wave 2).
Sensitivity analyses for missing data
Before excluding those with missing ethnicity data in wave 1, missing data occurred in 6 706 630 (28%) people for ethnicity, 7 027 371 (30%) for body mass index, and 221 283 (12% of 1 643 973 people with diabetes) for HbA1c. The measurement of serum creatinine typically reflects monitoring because of underlying risk factors for chronic kidney disease or a known diagnosis, reflected in approximately half of the sample (11 315 631, 48%) not having a serum creatinine measurement in the past five years. Wave 2 numbers were similar.
For adults, multiple imputation for missing ethnicity data made little difference to the results (supplementary appendix). When we analysed only people with recorded body mass index, the hazard ratios were slightly attenuated, but the pattern remained similar. For children, hazard ratios were slightly attenuated in wave 1 but similar in wave 2 when multiple imputation was performed to handle missing ethnicity data. Overall, our conclusions were robust to the method used to address missing data.
Discussion
Our data show higher risk of hospital admission and death for all groups with learning disability compared with the general population. Generally, the pattern of hazard ratios is consistent for waves 1 and 2. For hospital admissions and deaths, slightly weaker associations were observed for wave 2 than for wave 1. Additionally, we found higher risks among those with severe to profound learning disability compared with those with mild to moderate learning disability, which was not explained by measured physical comorbidities or residential care status. However, the absolute number of deaths was higher among people with mild to moderate learning disability.
For patients with Down’s syndrome or cerebral palsy, we observed higher risks among those on the learning disability register. Higher risks remained among those on the learning disability register who do not have Down’s syndrome or cerebral palsy compared with the general population. This observation is not explained by measured physical comorbidities or residential care status. After we excluded people who were prioritised for vaccination (first six groups of the phase 1 vaccination priority list in England due to age or comorbidities), those on the learning disability register still had a substantially increased risk of covid-19 related hospital admission. We also observed a higher risk of non-covid deaths in people with learning disability, though associations were weaker than for covid-19 related deaths. This finding is in contrast to most other risk factors that appear to have a similar magnitude of association with covid-19 related deaths and non-covid deaths.30
Findings in context
Our findings are consistent with the existing literature, yet make an important contribution by including outcomes from the second wave of the pandemic and by showing the importance of the learning disability register in identifying people for vaccination prioritisation. The Oxford RCGP Research and Surveillance Centre sentinel network, which includes 4.4 million people who are nationally representative of the population in England, reported twofold higher mortality rates among people with learning disability (odds ratio 1.96, 95% confidence interval 1.22 to 3.18, P<0.01) after extensive adjustment.4 Public Health England used different sources of data and estimated that, up to June 2020, the mortality rate in people with learning disability was approximately 6.3-fold higher than that of the general population.31 Data from Scotland also showed that adults with intellectual disabilities had higher rates of covid-19 infection, severe infection, and mortality.5 Increased risks remained after adjusting for age, sex, and deprivation (standardised severe infection ratio: 2.59, 95% confidence interval 1.80 to 3.39; standardised mortality ratio 3.20, 2.1 to 4.25). Higher mortality rates among people with learning disability have also been reported in Wales,6 New York State,7 and the United States more broadly.3 Not only are death rates higher for people with learning disability, but deaths occur at younger ages.3 8 9 31 The increased mortality rates among younger people with learning disability observed in our study have also been reported in the US.3 The younger age at death among people with learning disability is also well established for non-covid deaths.10
The high risk for people with Down’s syndrome was shown for the first wave by Clift and colleagues by using the QResearch population level primary care database8. In their cohort of eight million adults in England from January to June 2020, the age and sex adjusted hazard ratio for covid-19 death for adults with Down’s syndrome versus those without was 24.94 (95% confidence interval 17.08 to 36.44), which reduced to 10.39 (7.08 to 15.23) after extensive adjustment (deprivation, body mass index, cardiovascular, pulmonary and other disease, residential status, ethnicity). Data for cerebral palsy are more limited, but the QResearch analyses showed a higher mortality rate for this group (2.66, 1.62 to 4.36). Clift and colleagues obtained a fully adjusted hazard ratio of 1.27 (1.16 to 1.40) for covid-19 related death in those with learning disabilities other than Down’s syndrome, in contrast to our higher estimates. This discrepancy is probably because of differences in adjustment. We chose not to adjust for many comorbidities, viewing most of them as consequences of the learning disability and therefore part of the causal pathway. In our analyses, children with learning disability had a higher risk of hospital admission for covid-19. Existing studies also indicate that children with learning disability are more likely to require hospital admission and critical care because of covid-19 outcomes.32 33 34 35 36 However, it is important to note that the absolute risk of covid-19 related hospital admission experienced by children on the learning disability register was low.
While the incompleteness of the learning disability register means we will not have captured all deaths among children with learning disability, among children on the learning disability register there were fewer than five deaths per 1000 children years in each wave. Evidence about the relative risk of covid-19 related mortality associated with learning disability is lacking for children. The reason for this evidence gap is the small risk experienced by children overall—in our cohorts, few covid-19 related deaths occurred in children and so there were not enough data to analyse. Therefore, while we cannot quantify any differences in risk of covid-19 related deaths in children on the learning disability register, the absolute risk remains low.
The hazard ratios for covid-19 outcomes in our study attenuated after adjustment for deprivation. Residential status also partially explained the higher risks of severe covid-19 outcomes in people with learning disability. However, residential care for people with learning disability might not raise risk as much as in other care settings, perhaps because these facilities generally have fewer occupants.31 An important driver appears to be comorbidities, reflecting the higher prevalence of these covid-19 risk factors among people with learning disability.11 13 Comorbidities are also an important driver of increased risk of non-covid deaths.10 However, large excess mortality rates remained after extensive adjustment, which is also apparent in previous studies.8 This pattern implies that other drivers might be relevant, including inherent clinical vulnerabilities for people with certain conditions and concerns about healthcare quality, as also indicated by the higher case fatality rates among people with learning disability (Scotland: 30% v 24%13; New York: 15.0% v 7.9%7; US 18-74 year olds: 4.5% v 2.7%3). Additional mechanisms might contribute to the high risk among people with Down’s syndrome, including impaired cellular immunity.15
Strengths and weaknesses
Key strengths and weaknesses of the OpenSafely platform have been outlined previously.12 An important strength in the current analyses is that the study is large, including the records of approximately 40% of the English population, which allows disaggregation by learning disability grouping. We used comprehensive data on participants from medical records, which allowed us to adjust analyses successively to explore mechanisms for the association of learning disability and adverse covid-19 outcomes. Additionally, we were able to assess excess risks for both waves of the covid-19 pandemic, in terms of hospital admission and mortality outcomes. We also considered children and adults.
This study also has important limitations. Substantial geographical variation exists in the choice of electronic health record system,37 and so the population might not be fully nationally representative, although it is broadly representative in terms of ethnicity and deprivation.12 Identifying everyone with a learning disability from medical records alone was not possible. For instance, the most recent data, from 2015, suggest that 23% of people with learning disability are included on registers.1 The overall proportion of people on the learning disability register was 0.44% for England in 2015, slightly lower than the proportion in our study (0.63%); this potentially indicates an increase in coverage of the register in recent years. The reasons for under registration are unclear, but might include lack of perceived need and fear of stigma, among patients or clinicians. People on the learning disability register probably have more profound impairment and health conditions. For instance, in the current analyses 89% of people with Down’s syndrome were on the register and had higher mortality rates than people with Down’s syndrome who were not on the register. As a consequence, the hazard ratios might have been overestimated, although most of our sample had mild to moderate learning disability. Validation studies are not available for the Down’s syndrome and cerebral palsy codelists, although they were reviewed by clinicians specialising in the care of people with learning disability.
Our hospital admission data included only completed hospital admissions, therefore this outcome will have been under ascertained towards the end of the second wave. Defining hospital admission and death as covid-19 related depends on diagnosis, and validity of the outcome measure probably changed over time. If testing or clinical diagnosis of covid-19 differed for people with learning disability compared with the general population, this could have biased our estimates in either direction. Additionally, underlying health conditions could have been under ascertained in primary care records. Data were not available for epilepsy, which is a covid-19 risk factor and more common among people with learning disability.11 13 We also had an incomplete, and probably underestimated, measure of residential care.16 38
The consequences of do not resuscitate orders on the survival of people with learning disability have been raised as an area of concern, but we were not able to assess this impact in the current analyses. We did not have data on quality of treatment and so were not able to explore all our hypothesised pathways between learning disability and adverse covid-19 outcomes. Furthermore, these analyses focused only on severe covid-19 outcomes, and did not explore impacts on physical and mental health of people with learning disability, which probably occurred as a result of lockdown and other restrictions32 and require mitigation. We focused on the general population and so our analyses explored the combination of infection and severe outcomes once infected, therefore we were unable to disentangle associations with those two steps in the process. However, focusing on infected people only would induce biases due to unrepresentative testing.
Policy implications and interpretation
In February 2021, the Joint Committee on Vaccination and Immunisation updated its guidance36 on which groups should be prioritised for vaccination. The existing priority groups, including those with Down’s syndrome, cerebral palsy or severe or profound learning disability, were extended to include all people on the learning disability register. This change was informed by a previous version of this analysis, which showed increased risk in people on the learning disability who were not already prioritised for vaccination. However, the current learning disability registers are incomplete,1 and updating them would help to inform prioritisation programmes. Relying on codelists as an alternative to learning disability registers is not pragmatic for prioritisation given the large number of codes that are non-specific for learning disability. Many other countries (eg, Germany39 and the US40) currently focus on prioritising people living in care homes and those with Down’s syndrome for vaccination, and should consider broadening this category to include other people with learning disability. Increased risks among children <16 years suggest that vaccination in this age group warrants further consideration. These data should also be used to inform future prioritisation for subsequent vaccination initiatives in England, and international vaccine prioritisation programmes. Besides vaccination, efforts should continue to protect people with learning disability from covid-19 adverse outcomes, including consideration of non-pharmacological interventions such as shielding, and ensuring adequate support to obtain prompt access to testing for covid-19 and to appropriate healthcare.
Future research
The ONS data show that people with disabilities in general are at higher risk of covid-19 related mortality,41 but this outcome has not been explored through clinical databases, partly because of the complexity of generating codelists for broad ranges of conditions. However, using learning disability register data has highlighted the importance of public health surveillance and the need to develop indicators for disability. We used an indicator of care home residence to explore the extent to which this factor might mediate the association between learning disability and covid-19, but more detailed and accurate information on care home residence status is needed to understand how best to mitigate risk for people in residential care. More research is warranted on the excess covid-19 risks among people with Down’s syndrome. Cerebral palsy includes people with a broad range of conditions and severity, and a deeper exploration of covid-19 risk for this group is needed.
Conclusion
People with learning disabilities have markedly increased risks of hospital admission and death from covid-19. Prompt access to covid-19 testing and healthcare is warranted for this group, and prioritisation for covid-19 vaccination and other targeted preventive measures should be considered.
What is already known on this topic
Emerging evidence has shown that people with learning disability are at higher risk from covid-19 related mortality compared with the general population
Existing studies on the association of learning disability with severe outcomes from covid-19 often adjusted for variables that that might be partly a consequence of the learning disability, such as deprivation and comorbidities, which complicates interpretation of results
What this study adds
Adults with learning disability and those with Down’s syndrome or cerebral palsy have markedly increased risks of hospital admission and death from covid-19
Similar patterns were observed for children, but absolute risks of covid-19 hospital admission and death were small
Prompt access to covid-19 testing and healthcare is warranted for this group, and prioritisation for covid-19 vaccination and other targeted preventive measures should be considered
Acknowledgments
This work uses data provided by patients and collected by the NHS as part of their care and support (http://www.usemydata.org/). We are grateful for all the support received from the TPP technical operations team throughout this work, and for generous assistance from the information governance and database teams at NHS England and NHSX. We are grateful to Rose Almond, Cally Tann, and Michelle Heys for their review of codelists for learning disability, Down’s syndrome, and cerebral palsy.
Web extra.
Extra material supplied by authors
Web appendix: Supplementary appendix
Contributors: BG conceived the platform and the approach; BG and LS led the project overall and are guarantors. Contributions are as follows: design, EJW, HIM, HK, SJWE; data curation: CB, JP, JC, SH, SB, DE, PI, CEM; analysis, EJW, KB, AJW, CEM; funding acquisition: BG, LS; information governance: AM, BG, CB, JP; methodology: EJW, HIM, HK, SJWE, KB, AJW, BG, LS, CB, JP, JC, SH, SB, DE, PI, CEM; disease category conceptualisation and codelists: CEM, AJW, PI, SB, DE, CB, JC, JP, SH, HJC, KB, SB, AM, BM, LT, IJD, HIM, RM, HF; ethics approval: HJC, EJW, LS, BG; project administration: CEM, HJC, CB, SB, AM, LS, BG; resources: BG, LS, FH; software: SB, DE, PI, AJW, CEM, SD, CB, FH, JC, SH; supervision: BG, LS, SB; writing (original draft): EJW, HK, HIM, SJWE. All authors were involved in design and conceptual development and reviewed and approved the final manuscript. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. LS, BG and HK are joint principal investigators; EJW and HIM are joint first authors.
Funding: This work was supported by the Medical Research Council (MRC) grant MR/V015737/1. TPP provided technical expertise and infrastructure within their data centre pro bono in the context of a national emergency. EJW was supported by MRC project grant MR/S01442X/1. HIM and MR are funded by the National Institute for Health Research (NIHR) Health Protection Research Unit in Vaccines and Immunisation, a partnership between Public Health England and the London School of Hygiene and Tropical Medicine. HK was supported by funding from the PENDA grant from the Foreign, Commonwealth and Development Office. BG’s work on better use of data in healthcare more broadly is currently funded in part by National Institute for Health Research (NIHR) Oxford Biomedical Research Centre, NIHR Applied Research Collaboration Oxford and Thames Valley, the Mohn-Westlake Foundation, NHS England, and the Health Foundation; all DataLab staff are supported by BG’s grants on this work. The views expressed are those of the authors and not necessarily those of the NIHR, NHS England, Public Health England or the Department of Health and Social Care. Funders had no role in the study design, collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare the following: support from the Medical Research Council, TPP, NIHR Oxford Biomedical Research Centre, NIHR Applied Research Collaboration Oxford and Thames Valley, Mohn-Westlake Foundation, NHS England, NIHR Health Protection Research Unit in Vaccines and Immunisation, the Foreign, Commonwealth and Development Office, and the Health Foundation for the submitted work. EJW has received payments from AstraZeneca for providing training, unrelated to the submitted work. BG has received research funding from the Laura and John Arnold Foundation, the NHS National Institute for Health Research (NIHR), the NIHR School of Primary Care Research, the NIHR Oxford Biomedical Research Centre, the Mohn-Westlake Foundation, NIHR Applied Research Collaboration Oxford and Thames Valley, the Wellcome Trust, the Good Thinking Foundation, Health Data Research UK (HDRUK), the Health Foundation, and the World Health Organization; he also receives personal income from speaking and writing for lay audiences on the misuse of science. IJD has received unrestricted research grants and holds shares in GlaxoSmithKline (GSK) and holds grants from NIHR. LS reports grants from Wellcome, MRC, NIHR, UK Research and Innovation (UKRI), British Council, GSK, British Heart Foundation, and Diabetes UK outside this work. AS is employed by the London School of Hygiene and Tropical Medicine (LSHTM) on a fellowship sponsored by GSK. KB holds a Sir Henry Dale fellowship jointly funded by Wellcome and the Royal Society. AYSW holds a fellowship from BHF. RM holds a Sir Henry Wellcome Fellowship funded by the Wellcome Trust. HF holds a UKRI fellowship. RME is funded by HDRUK and the MRC.
Information governance: NHS England is the data controller; TPP is the data processor; and the key researchers on OpenSAFELY are acting on behalf of NHS England. This implementation of OpenSAFELY is hosted within the TPP environment which is accredited to the ISO 27001 information security standard and is NHS IG Toolkit compliant42 43; patient data have been pseudonymised for analysis and linkage using industry standard cryptographic hashing techniques; all pseudonymised datasets transmitted for linkage onto OpenSAFELY are encrypted; access to the platform is through a virtual private network (VPN) connection, restricted to a small group of researchers; the researchers hold contracts with NHS England and only access the platform to initiate database queries and statistical models; all database activity is logged; only aggregate statistical outputs leave the platform environment following best practice for anonymisation of results such as statistical disclosure control for low cell counts.44 The OpenSAFELY research platform adheres to the obligations of the UK General Data Protection Regulation (GDPR) and the Data Protection Act 2018. In March 2020, the Secretary of State for Health and Social Care used powers under the UK Health Service (Control of Patient Information) Regulations 2002 (COPI) to require organisations to process confidential patient information for the purposes of protecting public health, providing healthcare services to the public and monitoring and managing the covid-19 outbreak and incidents of exposure; this sets aside the requirement for patient consent.45 Taken together, these provide the legal bases to link patient datasets on the OpenSAFELY platform. GP practices, from which the primary care data are obtained, are required to share relevant health information to support the public health response to the pandemic, and have been informed of the OpenSAFELY analytics platform.
The lead authors (BG and LS) affirm that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Dissemination to participants and related patient and public communities: Dissemination of findings will be undertaken through a variety of routes. A lay summary and Easyread summary aimed at people with learning disability will be made available on the OpenSAFELY and HPRU in Vaccines and Immunisation websites (https://opensafely.org/ and https://immunisation.hpru.nihr.ac.uk/).
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Ethical approval
This study was approved by the Health Research Authority (REC reference 20/LO/0651) and by the LSHTM Ethics Board (reference 21863).
Data availability statement
All data were linked, stored and analysed securely within the OpenSAFELY platform (https://opensafely.org/). Data include pseudonymised data such as coded diagnoses, drugs, and physiological parameters. No free text data are included. All code is shared openly for review and reuse under MIT open license (https://github.com/opensafely/absolute-risks-covid-research). Detailed pseudonymised patient data are potentially reidentifiable and therefore not shared. We rapidly delivered the OpenSAFELY data analysis platform without prior funding to deliver timely analyses on urgent research questions in the context of the global covid-19 health emergency: now that the platform is established we are developing a formal process for external users to request access in collaboration with NHS England; details of this process will be published shortly on https://opensafely.org/.
References
- 1.Public Health England. People with Learning Disabilities in England 2015. Published 29 November 2016. https://www.gov.uk/government/publications/people-with-learning-disabilities-in-england-2015
- 2.Notification to LeDeR (Learning from Death Reviews) programme. 2021. https://www.england.nhs.uk/publication/covid-19-deaths-of-patients-with-a-learning-disability-notified-to-leder/
- 3. Turk MA, Landes SD, Formica MK, Goss KD. Intellectual and developmental disability and COVID-19 case-fatality trends: TriNetX analysis. Disabil Health J 2020;13:100942. 10.1016/j.dhjo.2020.100942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Joy M, Hobbs FR, Bernal JL, et al. Excess mortality in the first COVID pandemic peak: cross-sectional analyses of the impact of age, sex, ethnicity, household size, and long-term conditions in people of known SARS-CoV-2 status in England. Br J Gen Pract 2020;70:e890-8. 10.3399/bjgp20X713393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Henderson A, Fleming M, Cooper S-A, et al. COVID-19 infection and outcomes in a population-based cohort of 17 173 adults with intellectual disabilities compared with the general population. medRxiv. Published online 1 January 2021. 10.1101/2021.02.08.21250525 [DOI] [PubMed]
- 6.Watkins A. COVID-19-related deaths in Wales amongst people with learning disabilities from 1st March to 26th May 2020. Improvement Cymru. 2020. https://phw.nhs.wales/publications/publications1/covid-19-related-deaths-in-wales-amongst-people-with-learning-disabilities
- 7. Landes SD, Turk MA, Formica MK, McDonald KE, Stevens JD. COVID-19 outcomes among people with intellectual and developmental disability living in residential group homes in New York State. Disabil Health J 2020;13:100969. 10.1016/j.dhjo.2020.100969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Clift AK, Coupland CAC, Keogh RH, Hemingway H, Hippisley-Cox J. COVID-19 mortality risk in Down syndrome: results from a cohort study of 8 million adults. Ann Intern Med 2021;174:572-6. 10.7326/M20-4986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Perera B, Laugharne R, Henley W, et al. COVID-19 deaths in people with intellectual disability in the UK and Ireland: descriptive study. BJPsych Open 2020;6:e123. 10.1192/bjo.2020.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Heslop P, Blair PS, Fleming P, Hoghton M, Marriott A, Russ L. The Confidential Inquiry into premature deaths of people with intellectual disabilities in the UK: a population-based study. Lancet 2014;383:889-95. 10.1016/S0140-6736(13)62026-7. [DOI] [PubMed] [Google Scholar]
- 11. Emerson E, Hatton C, Baines S, Robertson J. The physical health of British adults with intellectual disability: cross sectional study. Int J Equity Health 2016;15:11. 10.1186/s12939-016-0296-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Williamson EJ, Walker AJ, Bhaskaran K, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584:430-6. 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kinnear D, Morrison J, Allan L, Henderson A, Smiley E, Cooper S-A. Prevalence of physical conditions and multimorbidity in a cohort of adults with intellectual disabilities with and without Down syndrome: cross-sectional study. BMJ Open 2018;8:e018292. 10.1136/bmjopen-2017-018292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Dard R, Janel N, Vialard F. COVID-19 and Down’s syndrome: are we heading for a disaster? Eur J Hum Genet 2020;28:1477-8. 10.1038/s41431-020-0696-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gensous N, Bacalini MG, Franceschi C, Garagnani P. Down syndrome, accelerated aging and immunosenescence. Semin Immunopathol 2020;42:635-45. 10.1007/s00281-020-00804-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mencap. Housing for people with a learning disability. https://www.mencap.org.uk/sites/default/files/2016-08/2012.108-Housing-report_V7.pdf
- 17. Courtenay K, Perera B. COVID-19 and people with intellectual disability: impacts of a pandemic. Ir J Psychol Med 2020;37:231-6. 10.1017/ipm.2020.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tapper J. Fury at “do not resuscitate” notices given to Covid patients with learning disabilities. 2021. https://www.theguardian.com/world/2021/feb/13/new-do-not-resuscitate-orders-imposed-on-covid-19-patients-with-learning-difficulties
- 19.Immunisation against Infectious Disease: The Green Book. Vol Chapter 14a. 2021. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/955548/Greenbook_chapter_14a_v6.pdf
- 20.Priority Groups for Coronavirus (COVID-19) Vaccination: Advice from the JCVI, 30 December 2020. Department of Health and Social Care. 2021. https://www.gov.uk/government/publications/priority-groups-for-coronavirus-covid-19-vaccination-advice-from-the-jcvi-30-december-2020
- 21.NHS Digital. Secondary Uses Service (SUS). 2020. https://digital.nhs.uk/services/secondary-uses-service-sus
- 22. Herrett EL, Thomas SL, Smeeth L. Validity of diagnoses in the general practice research database. Br J Gen Pract 2011;61:438-9. 10.3399/bjgp11X583092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Riley S, Ainslie KEC, Eales O, et al. High prevalence of SARS-CoV-2 swab positivity and increasing R number in England during October 2020: REACT-1 round 6 interim report. medRxiv. Published online 1 January 2020. 10.1101/2020.10.30.20223123 [DOI]
- 24.Coronavirus GOVUK. (COVID-19) in the UK. 2021. https://coronavirus.data.gov.uk/details/deaths
- 25. Bhaskaran K, Dos-Santos-Silva I, Leon DA, Douglas IJ, Smeeth L. Association of BMI with overall and cause-specific mortality: a population-based cohort study of 3·6 million adults in the UK. Lancet Diabetes Endocrinol 2018;6:944-53. 10.1016/S2213-8587(18)30288-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. McDonald HI, Shaw C, Thomas SL, Mansfield KE, Tomlinson LA, Nitsch D. Methodological challenges when carrying out research on CKD and AKI using routine electronic health records. Kidney Int 2016;90:943-9. 10.1016/j.kint.2016.04.010. [DOI] [PubMed] [Google Scholar]
- 27. Whyte MB, Hinton W, McGovern A, et al. Disparities in glycaemic control, monitoring, and treatment of type 2 diabetes in England: a retrospective cohort analysis. PLoS Med 2019;16:e1002942. 10.1371/journal.pmed.1002942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Walker JL, Grint DJ, Strongman H, et al. UK prevalence of underlying conditions which increase the risk of severe COVID-19 disease: a point prevalence study using electronic health records. BMC Public Health 2021;21:484. 10.1186/s12889-021-10427-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hughes RA, Heron J, Sterne JAC, Tilling K. Accounting for missing data in statistical analyses: multiple imputation is not always the answer. Int J Epidemiol 2019;48:1294-304. 10.1093/ije/dyz032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bhaskaran K, Bacon S, Evans S, et al. Factors associated with deaths due to COVID-19 versus other causes: population-based cohort analysis of UK primary care data and linked national death registrations within the OpenSAFELY platform. medRxiv. Published online January 1, 2021. 10.1101/2021.01.15.21249756 [DOI] [PMC free article] [PubMed]
- 31.Public Health England. COVID-19: deaths of people with learning disabilities. 2020. https://www.gov.uk/government/publications/covid-19-deaths-of-people-with-learning-disabilities
- 32. Swann OV, Holden KA, Turtle L, et al. ISARIC4C Investigators . Clinical characteristics of children and young people admitted to hospital with covid-19 in United Kingdom: prospective multicentre observational cohort study. BMJ 2020;370:m3249. 10.1136/bmj.m3249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Duarte-Salles T, Vizcaya D, Pistillo A, et al. Baseline characteristics, management, and outcomes of 55 270 children and adolescents diagnosed with COVID-19 and 1 952 693 with influenza in France, Germany, Spain, South Korea and the United States: an international network cohort study. MedRxiv Prepr Serv Health Sci. Published online 30 October 2020. 10.1101/2020.10.29.20222083 [DOI]
- 34. Götzinger F, Santiago-García B, Noguera-Julián A, et al. ptbnet COVID-19 Study Group . COVID-19 in children and adolescents in Europe: a multinational, multicentre cohort study. Lancet Child Adolesc Health 2020;4:653-61. 10.1016/S2352-4642(20)30177-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Williams N, Radia T, Harman K, Agrawal P, Cook J, Gupta A. COVID-19 Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in children and adolescents: a systematic review of critically unwell children and the association with underlying comorbidities. Eur J Pediatr 2021;180:689-97. 10.1007/s00431-020-03801-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Public Health England. JCVI advises inviting people on Learning Disability Register for vaccine. 2021. https://www.gov.uk/government/news/jcvi-advises-inviting-people-on-learning-disability-register-for-vaccine
- 37. Kontopantelis E, Stevens RJ, Helms PJ, Edwards D, Doran T, Ashcroft DM. Spatial distribution of clinical computer systems in primary care in England in 2016 and implications for primary care electronic medical record databases: a cross-sectional population study. BMJ Open 2018;8:e020738. 10.1136/bmjopen-2017-020738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Schultze A, Bates C, Cockburn J. Identifying care home residents in electronic health records - an OpenSAFELY short data report. Wellcome Open Res 2021;6. 10.12688/wellcomeopenres.16737.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lorenz-Dant K. A brief overview of the current German COVID-19 vaccination strategy. 2020. https://ltccovid.org/2020/12/18/a-brief-overview-of-the-current-german-covid-19-vaccination-strategy/
- 40.Dooling K, Marin M, Wallace M, et al. The Advisory Committee on Immunization Practices’ Updated Interim Recommendation for Allocation of COVID-19 Vaccine – United States. 2020. https://www.cdc.gov/mmwr/volumes/69/wr/mm695152e2.htm?s_cid=mm695152e2_w#T1_down [DOI] [PMC free article] [PubMed]
- 41.ONS. Updated estimates of coronavirus (COVID-19) related deaths by disability status, England: 24 January to 20 November 2020. 2021. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/articles/coronaviruscovid19relateddeathsbydisabilitystatusenglandandwales/24januaryto20november2020
- 42.NHS Digital. BETA – Data Security Standards - NHS Digital. https://digital.nhs.uk/about-nhs-digital/our-work/nhs-digital-data-and-technology-standards/framework/beta---data-security-standards
- 43.NHS Digital. Data Security and Protection Toolkit - NHS Digital. 2018. https://digital.nhs.uk/data-and-information/looking-after-information/data-security-and-information-governance/data-security-and-protection-toolkit
- 44.NHS Digital. ISB1523: Anonymisation Standard for Publishing Health and Social Care Data - NHS Digital. 2019. https://digital.nhs.uk/data-and-information/information-standards/information-standards-and-data-collections-including-extractions/publications-and-notifications/standards-and-collections/isb1523-anonymisation-standard-for-publishing-health-and-social-care-data
- 45.Secretary of State for Health and Social Care - UK Government. Coronavirus (COVID-19): notification to organisations to share information. 2020. https://web.archive.org/web/20200421171727/https://www.gov.uk/government/publications/coronavirus-covid-19-notification-of-data-controllers-to-share-information
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Web appendix: Supplementary appendix
Data Availability Statement
All data were linked, stored and analysed securely within the OpenSAFELY platform (https://opensafely.org/). Data include pseudonymised data such as coded diagnoses, drugs, and physiological parameters. No free text data are included. All code is shared openly for review and reuse under MIT open license (https://github.com/opensafely/absolute-risks-covid-research). Detailed pseudonymised patient data are potentially reidentifiable and therefore not shared. We rapidly delivered the OpenSAFELY data analysis platform without prior funding to deliver timely analyses on urgent research questions in the context of the global covid-19 health emergency: now that the platform is established we are developing a formal process for external users to request access in collaboration with NHS England; details of this process will be published shortly on https://opensafely.org/.


