Abstract
Background
While recommended by international societal guidelines in the paediatric population, the use of venoarterial extracorporeal membrane oxygenation (VA ECMO) as mechanical circulatory support for refractory septic shock in adults is controversial. We aimed to characterise the outcomes of adults with septic shock requiring VA ECMO, and identify factors associated with survival.
Methods
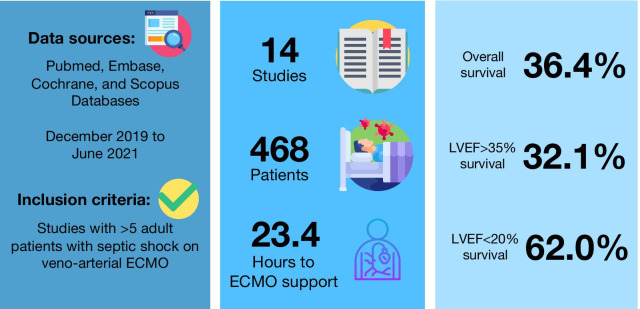
We searched Pubmed, Embase, Scopus and Cochrane databases from inception until 1st June 2021, and included all relevant publications reporting on > 5 adult patients requiring VA ECMO for septic shock. Study quality and certainty in evidence were assessed using the appropriate Joanna Briggs Institute checklist, and the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) approach, respectively. The primary outcome was survival to hospital discharge, and secondary outcomes included intensive care unit length of stay, duration of ECMO support, complications while on ECMO, and sources of sepsis. Random-effects meta-analysis (DerSimonian and Laird) were conducted.
Data synthesis
We included 14 observational studies with 468 patients in the meta-analysis. Pooled survival was 36.4% (95% confidence interval [CI]: 23.6%–50.1%). Survival among patients with left ventricular ejection fraction (LVEF) < 20% (62.0%, 95%-CI: 51.6%–72.0%) was significantly higher than those with LVEF > 35% (32.1%, 95%-CI: 8.69%–60.7%, p = 0.05). Survival reported in studies from Asia (19.5%, 95%-CI: 13.0%–26.8%) was notably lower than those from Europe (61.0%, 95%-CI: 48.4%–73.0%) and North America (45.5%, 95%-CI: 16.7%–75.8%). GRADE assessment indicated high certainty of evidence for pooled survival.
Conclusions
When treated with VA ECMO, the majority of patients with septic shock and severe sepsis-induced myocardial depression survive. However, VA ECMO has poor outcomes in adults with septic shock without severe left ventricular depression. VA ECMO may be a viable treatment option in carefully selected adult patients with refractory septic shock.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13054-021-03668-5.
Keywords: ECMO, Venoarterial, Septic shock, Septic cardiomyopathy, Mechanical circulatory support
Background
Sepsis is a leading cause of death among critically ill patients and a global public health burden, leading to high healthcare costs [1, 2]. In 2017 alone, there were 48.9 Million cases of sepsis and 11.0 Million deaths (19.7% of all global deaths) related to sepsis [3]. The burden of sepsis is highest in early childhood, followed by a second peak in incidence in late adulthood [4]. Recognising sepsis as a global health priority, the World Health Assembly adopted a resolution to reduce its burden through better awareness, early diagnosis, and aggressive management [2]. This is reflected in national healthcare efforts, one example being the German Quality Network Sepsis which aims to decrease sepsis-related mortality [5].
Approximately, 15% of patients with sepsis develop septic shock, defined as persistent hypotension requiring vasopressors and elevated lactate levels despite adequate fluid resuscitation, where hospital mortality is in excess of 40% [3]. A subset of adult patients with septic shock develops concomitant left ventricular dysfunction, often described as septic cardiomyopathy [6]. However, septic cardiomyopathy is poorly defined in the literature and may be an underdiagnosed entity due to a lack of formal diagnostic criteria [6–10]. Adult patients with septic cardiomyopathy have 2–3 times increased mortality compared with those with septic shock alone [7]. Single-centre studies have shown dismal survival rates (10–30%) when severe left ventricular (LV) dysfunction coexisted in patients with septic shock [11].
Unlike many aetiologies of cardiomyopathy, septic cardiomyopathy is reversible, and early detection and intervention of septic cardiomyopathy in patients with septic shock may reduce mortality [11]. The encouraging outcomes of extracorporeal membrane oxygenation (ECMO) in paediatric septic shock have led to it being recommended as a potential therapy in some societal guidelines [12–18]. However, the haemodynamic pattern of septic shock is markedly different across age groups: new-born infants typically present with pulmonary hypertension and right heart failure, young children with left heart failure, and adolescents and adults with distributive shock [16]. Given the contrast in haemodynamic status between adult and paediatric shock, the use of ECMO, and in particular venoarterial ECMO (VA ECMO), in adult septic shock remains controversial.
VA ECMO has been found to be a risk factor for mortality when compared to venovenous ECMO (VV ECMO) in patients with sepsis [19–21]. This might be due to the differing indications for ECMO in sepsis (concomitant hypoxemia and right ventricular dysfunction in VV ECMO vs. cardiomyopathy and vasoplegia in VA ECMO), potentially reflecting less severe disease for patients supported with VV ECMO. Nonetheless, single-centre observational studies have shown that a subset of septic adults (specifically those with septic cardiomyopathy) may benefit from VA ECMO for mechanical circulatory support [22–24]. We conducted a systematic review of literature on the outcomes and complications of VA ECMO as mechanical circulatory support in adult patients with septic shock.
Methods
Search strategy and selection criteria
This study was registered with PROSPERO (CRD42020161827), and was conducted in adherence with the Preferred Reporting Items for Systematic Reviews and Meta-analyses Statement [25]. We searched Medline, Embase, Cochrane, and Scopus databases from inception to 1st June, 2021, using the following keywords and their variations: “extracorporeal membrane oxygenation”, “extracorporeal life support”, “adult” and “septic shock” (Additional File 1). We assessed all relevant studies and their citation lists to identify articles for inclusion.
All studies written in English or with English translation, reporting on five or more adult patients (≥ 18 years) with septic shock supported with VA ECMO were included [18]. We excluded any non-human or paediatric studies, and any case reports to avoid publication bias. Many centres that have published case series and observational studies also report data to the Extracorporeal Life Support Organisation (ELSO) registry. To avoid duplication of patient data, we excluded studies utilising the ELSO registry data. In the case of overlapping patient data across two or more studies in our primary meta-analysis, we included the larger study. Two reviewers (RRL and WHP) independently screened the articles for eligibility; any conflicts were resolved by consensus or by a third reviewer (KR).
Data collection
Data were collected independently by two reviewers (RRL and WHP) using a prespecified data extraction form; any conflicts were resolved by consensus or by a third reviewer (KR). Data collection covered study characteristics, pre-ECMO characteristics, survival to hospital discharge, and other relevant clinical outcomes. Details on the data extraction form are summarised in Additional File 2. Individual participant data (IPD) were also collected for four studies that presented data individually for each patient.
Risk of bias assessment
Using the Joanna Briggs Institute (JBI) checklists for case series and cohort studies (Additional File 3), two reviewers (RRL and WHP) independently assessed the eligibility of studies; any conflicts were resolved by consensus or by a third reviewer (KR). The possibility of publication bias was assessed using Egger’s test.
Statistical analysis
Statistical analyses were performed on R3.6.1, using the meta (v4.12-0), dmetar (v0.0.9000), and lme4 (v1.1-23) packages [26–28]. For continuous variables, we pooled the means from the aggregate data presented in each study as per Wan et al. [29]. The primary outcome was survival to discharge. Secondary outcomes included ICU LOS, ECMO duration, complications during ECMO, and source of infection.
We anticipated significant interstudy heterogeneity given the varied presentation of sepsis and septic shock and general lack of guidelines for patient selection and management for ECMO. As such, random-effects meta-analyses (DerSimonian and Laird) were conducted, and 95% confidence intervals (CIs) were computed using the Clopper–Pearson method [30–32]. Survival outcomes are presented as pooled proportions and 95% CIs, while dichotomous outcomes are presented as pooled risk ratios (RR) and 95% CIs. Planned subgroup analyses were conducted with continuity correction to include studies with zero events, and include: geographical location (Asia, Europe, and North America), pre-ECMO serum lactate (above and below 5 mmol/l), LVEF (< 20%, 20% to 35%, > 35%), and cardiopulmonary resuscitation (CPR) before or during ECMO. As inter-study heterogeneity can be misleadingly large when assessed using I2 statistics for observational studies, we used the Grading of Recommendations, Assessments, Developments and Evaluations (GRADE) approach and the tau-squared (T2) statistic to assess the inter-study heterogeneity [33, 34]. A sensitivity analysis was performed for all analyses by omitting one study at a time to identify outliers or influential studies.
Summary-level meta-regression was conducted when at least six data points [35, 36] were collected to explore potential sources of heterogeneity or prognostically relevant study-level covariates. One-stage IPD meta-regression was conducted using the binomial distribution and logit link to compute adjusted and unadjusted ORs [37]. Intrastudy nesting of patients was accounted for by including a random slope term that allows the treatment effect to vary between studies. Fixed effects logistic regression was conducted when intrastudy patient correlation was found to be negligible. p value ≤ 0.05 was considered as statistically significant.
Results
Study details and demographics
Of 2748 references screened, our search yielded 87 potentially relevant studies across the four databases. Sixteen studies reporting on 534 adult patients with septic shock undergoing VA ECMO were included in our systematic review [20, 22, 38–51]. All studies were retrospective and observational in nature: there was one multi-centre propensity score matched study, Eleven single-centre retrospective cohort studies, and four single-centre retrospective case series. There were nine studies from Asia, five studies from Europe, and one study from North America. One study reported on patients from both Europe and North America. There were four studies with overlapping data; two of them were excluded from the primary meta-analysis. In total, 14 studies (468 patients) were included in our primary meta-analysis (Additional File 4). The pooled mean age (13 studies, 396 patients) was 53.2 years (95%-CI: 50.6–55.9), while the pooled prevalence of male patients (13 studies, 396 patients) was 63.0% (95%-CI: 55.5%–70.3%). Pneumonia was reported in 56.7% (95%-CI; 44.0%–69.0%) of patients as the primary diagnosis. The pooled pre-ECMO serum pH (11 studies, 337 patients) and lactate (14 studies, 407 patients) were 7.15 (95%-CI: 7.13–7.17) and 7.58 mmol/L (95%-CI: 6.05–9.12 mmol/L), respectively. Patients were predominantly cannulated peripherally (11 studies femoro-femoral, 2 studies jugulo-femoral). Cardiopulmonary resuscitation (CPR) before or during ECMO was conducted in 28.9% (95%-CI: 16.9%–42.5%) of patients (9 studies, 384 patients). The pooled time to ECMO cannulation from onset of septic shock was 23.4 h (95%-CI: 20.1–26.8). Baseline demographics and patient outcomes of the included studies are summarised in Additional Files 5 and 6.
Primary meta-analysis
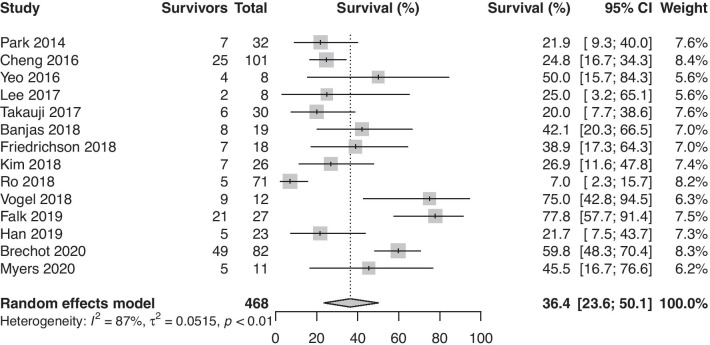
The pooled survival to hospital discharge (14 studies, 468 patients) was 36.4% (95%-CI: 23.6%–50.1%, Fig. 1). Leave-one-out (LOO) analysis did not yield any potential outliers.
Fig. 1.
Proportion of survivors among adult patients with septic shock requiring venoarterial extracorporeal membrane oxygenation
Subgroup analysis
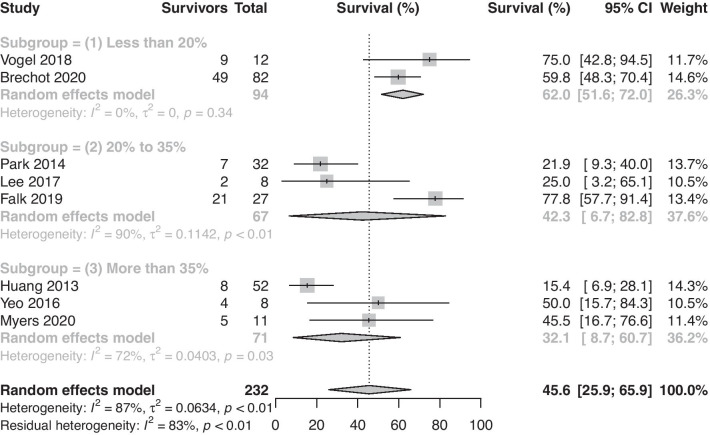
Subgroup analysis yielded significant differences when considering the geographical region. Survival reported by studies from Asia (nine studies, 19.5%, 95%-CI: 13.0%–26.8%) was notably lower than in those from Europe and North America (six studies, 57.8%, 95%-CI: 44.8%–70.3%). Among five studies (190 patients), 24.4% (21 of 86) of patients undergoing CPR before or during ECMO survived, while 27.3% (54 of 144) of patients without CPR before or during ECMO survived. CPR prior to or during VA ECMO was not associated with lower survival (RR: 0.90, 95%-CI: 0.62 to 1.29, p = 0.55). Finally, survival reported by studies in which LVEF < 20% (three studies, (62.0%, 95%-CI: 51.6%–72.0%) was significantly higher than those where LVEF > 35% (three studies, 32.1%, 95%-CI: 8.7%–60.7%, p = 0.05) Survival reported by studies where LVEF was between 20 and 35% was 42.3% (95%-CI: 6.7%–82.8%, Fig. 2) Pre-ECMO serum lactate (14 studies, 407 patients) was not significantly associated with increased survival (p = 0.21). The results of the subgroup analysis are summarised in Table 1.
Fig. 2.
Proportion of survivors among adult patients with septic shock requiring venoarterial extracorporeal membrane oxygenation stratified by ejection fraction
Table 1.
Results of subgroup analysis
| Subgroup | Pooled survival (%) | 95% CI (%) | |
|---|---|---|---|
| Geographical region (p < 0.001) | Asia | 19.5 | 13.0 to 26.8 |
| Europe and North America | 57.8 | 44.8 to 70.3 | |
| Presence of CPR (p = 0.55) | CPR | Survival = 24.4% (21 of 86) | |
| No CPR | Survival = 27.3% (54 of 144) | ||
| LVEF (p = 0.09) | < 20% | 62.0 | 51.6 to 72.1 |
| 20 to 35% | 42.3 | 6.70 to 82.8 | |
| > 35% | 32.1 | 8.70 to 60.7 | |
| Serum lactate (p = 0.20) | < 5 mmol/l | 50.5 | 29.8 to 71.2 |
| > 5 mmol/l | 32.2 | 16.2 to 50.7 | |
CI confidence interval; VA Venoarterial; VV venovenous; CPR cardiopulmonary resuscitation; LVEF left ventricular ejection fraction
Univariable and IPD meta-regression analyses
The details of the univariable meta-regression analysis are summarised in Table 2. Age, sex, SOFA score, lactate levels, LVEF, and CPR were not associated with increased survival (Table 2). Four studies (134 patients) provided IPD on age, gender, pre-ECMO SOFA score, CPR, serum lactate, LVEF and duration of ECMO. Multivariable one-stage IPD meta-regression (Table 3) analyses revealed that age was an independent risk factor for mortality (unadjusted OR for survival: 0.974, 95% CI: 0.949–0.999, p = 0.04), but this association was not observed when accounting for the other covariates (adjusted OR: 0.972, 95% CI: 0.941–1.002, p = 0.07). Other factors were not associated with survival benefits on IPD analysis.
Table 2.
Results of univariable meta-regression analysis
| Covariate | Number of studies | Odds ratio | Lower 95% CI | Upper 95% CI | p value |
|---|---|---|---|---|---|
| Age | 13 | 0.990 | 0.979 | 1.006 | 0.06 |
| LVEF | 8 | 0.991 | 0.978 | 1.002 | 0.13 |
| Male sex | 12 | 0.512 | 0.148 | 1.770 | 0.29 |
| Lactate | 14 | 0.978 | 0.926 | 1.034 | 0.43 |
| SOFA | 14 | 0.982 | 0.935 | 1.031 | 0.46 |
| CPR | 9 | 0.873 | 0.385 | 1.980 | 0.75 |
| Patients with pneumonia | 12 | 1.078 | 0.435 | 2.673 | 0.87 |
| Publication year | 16 | 1.025 | 0.970 | 1.083 | 0.38 |
CI confidence interval, CPR cardiopulmonary resuscitation; LVEF left ventricular ejection fraction, SOFA sequential organ failure assessment
Table 3.
Results of one-stage individual patient data (IPD) meta-regression analysis
| Factor | Unadjusted | Adjusted | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |
| ECMO duration | 0.997 | 0.940–1.059 | 0.91 | 1.024 | 0.951–1.115 | 0.55 |
| Lactate | 0.980 | 0.905–1.060 | 0.61 | 0.934 | 0.845–1.029 | 0.17 |
| CPR | 0.919 | 0.292–3.261 | 0.89 | 0.526 | 0.086–3.006 | 0.32 |
| SOFA score | 1.030 | 0.929–1.136 | 0.55 | 1.028 | 0.878–1.211 | 0.74 |
| Age | 0.974 | 0.949–0.999 | 0.04 | 0.972 | 0.941–1.002 | 0.07 |
| Male gender | 0.609 | 0.293–1.248 | 0.18 | 0.742 | 0.309–1.769 | 0.46 |
| LVEF | 1.026 | 0.982–1.065 | 0.14 | 1.022 | 0.978–1.072 | 0.34 |
OR odds ratio; CI confidence interval; ECMO extracorporeal membrane oxygenation; SOFA sequential organ failure assessment; CPR cardiopulmonary resuscitation; LVEF left ventricular ejection fraction
Secondary outcomes
The pooled ICU LOS (8 studies, 209 patients) was 19.38 days (95%-CI: 11.56–27.19). The pooled ECMO duration (10 studies, 337 patients) was 5.78 days (95%-CI: 4.11–7.45). Among 8 studies (396 patients), survivors also had significantly longer ECMO durations (+ 2.18 days, 95%-CI: 0.27–4.10, p = 0.03) than non-survivors. After LOO analysis, the pooled mean difference was + 2.84 days (95%-CI: 1.09–4.58, p = 0.002). A total of 124 complications were reported across 6 studies (198 patients). Haemorrhagic (49, 39.5%), infectious (36, 29.0%), and mechanical (23, 18.5%) were the most commonly reported complications while receiving ECMO. 9 studies (262 patients) reported on the pathogens cultured from the patients (Additional File 6). In some instances, the temporal relationship between the initiation of ECMO and positive microbiological cultures results was unclear. We could not exclude the possibility that a proportion of the cultured pathogens may have been nosocomial in origin during ECMO, rather than the inciting organism.
Assessment of study quality
Appraisal using the JBI checklists for cohort studies and case series suggested a high level of quality across the included studies for this review, with the majority of the studies receiving at least 9/10 in the appropriate checklist (Additional File 3). Egger’s test yielded non-significant results for publication bias. A summary of the GRADE assessment for certainty of evidence is provided in Additional File 7. As the outcome was survival, the starting level of evidence for observational studies was high. Certainty for pooled survival was high, the certainty for ECMO duration was downgraded to moderate for serious imprecision, and the certainty for ICU LOS was downgraded to low for serious inconsistency and imprecision.
Discussion
This systematic review and meta-analysis quantitatively summarised the evidence for survival of adult patients with septic shock requiring VA ECMO. Pooled survival across 14 studies and 468 patients was 36.4%. Subgroup analyses revealed that pre-ECMO LVEF significantly influenced survival rates of patients with septic shock initiated on ECMO in addition to variations in survival by geographic region of study origin.
While data are scarce, studies investigating VA ECMO adult patients with preserved LVEF have reported dismal outcomes [40, 46, 49]. It has been proposed that septic patients who have hyperdynamic left ventricular function on echocardiography have poorer outcomes than those with normo- or hypo-kinetic profiles, and this stratification may permit better patient selection for VA ECMO in septic shock [6]. A propensity-score weighted analysis found that select patients with severe myocardial dysfunction (very low LVEF) receiving VA ECMO during the first four days of septic shock had significantly lower mortality than those without ECMO [50], with similar findings among observational case series reporting on VA ECMO for adult and paediatric septic cardiomyopathy [12, 13, 47]. Concordant with these observations, our analysis found that survival among patients with LVEF > 35% was significantly lower than those with LVEF < 20% (62.0% Vs 32.1%). Patients with LVEF between 20 and 35% had intermediate survival (42.3%), suggesting a possible graded effect of LVEF on outcomes. While plausible, further research investigating pre-ECMO LVEF and its relation with mortality on VA ECMO for adult septic shock is needed to conclusively substantiate our findings.
Currently, the diagnostic criteria for adult septic cardiomyopathy are not fully established, due to the complexity and variations in the cardiovascular response to infection [52, 53]. It is also difficult to determine how well myocardial dysfunction correlates with organ dysfunction in general, and how much it independently contributes to poorer outcomes [53]. This is compounded by the lack of longitudinal echocardiography data to ascertain cardiac function at premorbid, disease, and recovery states [9]. Nonetheless, it is understood that transient and reversible myocardial depression is common in septic patients, and is associated with low or normal LV filling pressures despite depressed systolic function [54, 55]. Three broad criteria were proposed to characterise septic cardiomyopathy: LV dilatation with normal- or low-filling pressure, reduced ventricular contractility, and ventricular dysfunction with reduced response to volume infusion [8]. While increasing perfusion and cardiac output can improve survival among these patients [56, 57]. the use of very high-dose vasopressors might contribute to a vicious circle of vasoconstriction and refractory cardiovascular failure [22]. By providing mechanical circulatory support, VA ECMO can potentially restore systemic perfusion pressure and increase oxygen delivery. This corrects the cellular hypoxia and metabolic acidosis during septic cardiomyopathy, ameliorating vasopressor dependence and potentially improving the chances of survival.
In septic patients with preserved cardiac function, VA ECMO may be contraindicated as it reduces preload, and increases afterload, eventually decreasing cardiac output [58]. Of note were six patients from the study by Falk and colleagues, who underwent VV ECMO and then converted to VA ECMO. All six patients had LVEF > 35% and none of them survived to discharge. Similarly, patient profiles described by studies from Asia were characterised by distributive shock and relatively preserved LV function. On the other hand, patients in studies from Europe typically presented with severe myocardial depression, which might explain why survival reported by studies from Europe was higher than those from Asia. Apart from this, the proportion of patients undergoing CPR prior to or during ECMO, that is associated with greater mortality, was also higher in studies from Asia.
Strengths of this study include the broad inclusion criteria and relevant exclusion criteria. Our review included 14 studies, pooling data from eight different countries across three regions. We elucidated factors correlating with survival via subgroup analysis and meta-regression, reducing confounding. Coupled with non-significant results from Egger’s test, we sourced for unpublished data for IPD meta-analysis, limiting publication bias. Nonetheless, we recognise several limitations of this study. The absence of randomised studies increases the risks of confounding and bias, in particular, confounding by indication. Furthermore, there are different initiation thresholds and varying protocols and practices between individual institutions, which can introduce confounding factors given the lack of risk adjustment or propensity-scoring techniques. In addition, there was limited data on vasopressor scores or cardiac index in most of the studies. Some of the pertinent sequelae to VA ECMO such as differential oxygenation and its impact on organ dysfunction in adult septic patients could not be fully elucidated due to lack of granular data. Finally, the need for VA ECMO in adult septic cardiomyopathy is uncommon, which makes these results applicable to a narrow spectrum of patients in clinical practice. While it would be most appropriate to perform a prospective randomised clinical trial in this patient population, there would be considerable challenges in doing so, including the low incidence of patients with septic shock and septic cardiomyopathy, and the ethical challenges surrounding randomisation in ECMO studies [59–61].
Conclusions
Our systematic review and meta-analysis of the current literature suggests that VA ECMO may be a viable salvage therapy among select patients with septic shock and concomitant myocardial depression, characterised by persistently low cardiac output refractory to inotropes. By contrast, ECMO is associated with especially poor outcomes among patients with septic shock but without severe ventricular dysfunction. Overall pooled survival in our meta-analysis was 36.4%. Patients with septic cardiomyopathy had considerably better survival than those with normal LV function. While the results of this review might only be translatable to a small population of patients with septic shock and concomitant cardiomyopathy, judicious selection of these patients for VA ECMO could improve mortality.
Supplementary Information
Additional file 1. Search strings for respective databases.
Additional file 2. Data extraction template.
Additional file 3. Joanna Briggs Institute (JBI) checklists for included studies.
Additional file 4. Preferred Reporting Items for Systematic Review and Meta-analyses (PRISMA) flowchart for study selection.
Additional file 5. Baseline demographics of studies included for systematic review.
Additional file 6. Patient outcomes of studies included for systematic review.
Additional file 7. Grading of Recommendations, Assessments, Developments and Evaluations (GRADE) approach for certainty in evidence.
Acknowledgements
The authors acknowledge Suei Nee Wong from the Medical Library, National University of Singapore and Nicholas Syn from the Yong Loo Lin School of Medicine, National University of Singapore for their contributions.
Abbreviations
- LV
Left ventricular
- ECMO
Extracorporeal membrane oxygenation
- VA
Venoarterial
- VV
Venovenous
- LVEF
Left ventricular ejection fraction
- SOFA
Sequential organ failure assessment
- ICU
Intensive care unit
- LOS
Length of stay
- IPD
Individual participant data
- JBI
Joanna Briggs Institute
- RR
Risk ratio
- CPR
Cardiopulmonary resuscitation
- GRADE
Grading of recommendations, assessment, development, and evaluations
Authors’ contributions
The study was designed by KR and GM. RRL and WHP screened the articles, assessed the risk of bias and extracted the data under the supervision of KR. RRL analysed and interpreted the data under the supervision of CST and KR. Tables and figures were produced by RRL. RRL and KR shared the primary responsibility of writing the manuscript, to which all authors contributed to and revised. GM, NB, DB, AC and KR critically revised the manuscript for important intellectual content. All authors provided critical conceptual input, interpreted the data analysis, read, and approved the final draft.
Funding
There was no funding source for this study.
Availability of data and materials
The dataset generated and analysed during the current study can be found in the included studies and their supplementary information files.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
DB receives research support from ALung Technologies. He has been on the medical advisory boards for Baxter, Abiomed, Xenios and Hemovent. All other authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Ryan Ruiyang Ling and Kollengode Ramanathan have contributed equally to this work
References
- 1.York Health Economic Consortium. The Cost of Sepsis Care in the UK. http://allcatsrgrey.org.uk/wp/wpfb-file/yhec-sepsis-report-17-02-17-final-pdf/. Accessed 12 May 2021.
- 2.World Health Organisation. Improving the prevention, diagnosis and clinical management of sepsis. https://www.who.int/servicedeliverysafety/areas/sepsis/en/. Accessed 12 May 2021.
- 3.Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, et al. The Third international consensus definitions for sepsis and septic shock (Sepsis-3) JAMA. 2016;315(8):801–810. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rudd KE, Johnson SC, Agesa KM, Shackelford KA, Tsoi D, Kievlan DR, Colombara DV, Ikuta KS, Kissoon N, Finfer S, et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: analysis for the Global Burden of Disease Study. Lancet. 2020;395(10219):200–211. doi: 10.1016/S0140-6736(19)32989-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schwarzkopf D, Rüddel H, Gründling M, Putensen C, Reinhart K. The German Quality Network Sepsis: study protocol for the evaluation of a quality collaborative on decreasing sepsis-related mortality in a quasi-experimental difference-in-differences design. Implement Sci. 2018;13(1):15. doi: 10.1186/s13012-017-0706-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vieillard-Baron A. Septic cardiomyopathy. Ann Intensive Care. 2011;1(1):6. doi: 10.1186/2110-5820-1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ehrman RR, Sullivan AN, Favot MJ, Sherwin RL, Reynolds CA, Abidov A, Levy PD. Pathophysiology, echocardiographic evaluation, biomarker findings, and prognostic implications of septic cardiomyopathy: a review of the literature. Crit Care. 2018;22(1):112. doi: 10.1186/s13054-018-2043-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Martin L, Derwall M, Al Zoubi S, Zechendorf E, Reuter DA, Thiemermann C, Schuerholz T. The septic heart: current understanding of molecular mechanisms and clinical implications. Chest. 2019;155(2):427–437. doi: 10.1016/j.chest.2018.08.1037. [DOI] [PubMed] [Google Scholar]
- 9.Sanfilippo F, Orde S, Oliveri F, Scolletta S, Astuto M. The Challenging diagnosis of septic cardiomyopathy. Chest. 2019;156(3):635–636. doi: 10.1016/j.chest.2019.04.136. [DOI] [PubMed] [Google Scholar]
- 10.Sato R, Nasu M. A review of sepsis-induced cardiomyopathy. J Intensive Care. 2015;3:48. doi: 10.1186/s40560-015-0112-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lin H, Wang W, Lee M, Meng Q, Ren H. Current status of septic cardiomyopathy: basic science and clinical progress. Front Pharmacol. 2020;11:210. doi: 10.3389/fphar.2020.00210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maclaren G, Butt W. Extracorporeal membrane oxygenation and sepsis. Crit Care Resusc. 2007;9(1):76–80. [PubMed] [Google Scholar]
- 13.Schlapbach LJ, Chiletti R, Straney L, Festa M, Alexander D, Butt W, MacLaren G. Defining benefit threshold for extracorporeal membrane oxygenation in children with sepsis-a binational multicenter cohort study. Crit Care. 2019;23(1):429. doi: 10.1186/s13054-019-2685-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meyer DM, Jessen ME. Results of extracorporeal membrane oxygenation in children with sepsis. The Extracorporeal Life Support Organization. Ann Thorac Surg 1997, 63(3):756–761. [DOI] [PubMed]
- 15.Skinner SC, Iocono JA, Ballard HO, Turner MD, Ward AN, Davenport DL, Paden ML, Zwischenberger JB. Improved survival in venovenous vs venoarterial extracorporeal membrane oxygenation for pediatric noncardiac sepsis patients: a study of the Extracorporeal Life Support Organization registry. J Pediatr Surg. 2012;47(1):63–67. doi: 10.1016/j.jpedsurg.2011.10.018. [DOI] [PubMed] [Google Scholar]
- 16.Davis AL, Carcillo JA, Aneja RK, Deymann AJ, Lin JC, Nguyen TC, Okhuysen-Cawley RS, Relvas MS, Rozenfeld RA, Skippen PW, et al. American College of Critical Care medicine clinical practice parameters for hemodynamic support of pediatric and neonatal septic shock. Crit Care Med. 2017;45(6):1061–1093. doi: 10.1097/CCM.0000000000002425. [DOI] [PubMed] [Google Scholar]
- 17.Martin K, Weiss SL. Initial resuscitation and management of pediatric septic shock. Minerva Pediatr. 2015;67(2):141–158. [PMC free article] [PubMed] [Google Scholar]
- 18.Ramanathan K, Yeo N, Alexander P, Raman L, Barbaro R, Tan CS, Schlapbach LJ, MacLaren G. Role of extracorporeal membrane oxygenation in children with sepsis: a systematic review and meta-analysis. Crit Care. 2020;24(1):684. doi: 10.1186/s13054-020-03418-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ramanathan K, Tan CS, Rycus P, MacLaren G. Extracorporeal membrane oxygenation for adult community-acquired pneumonia: outcomes and predictors of mortality. Crit Care Med. 2017;45(5):814–821. doi: 10.1097/CCM.0000000000002320. [DOI] [PubMed] [Google Scholar]
- 20.Takauji S, Hayakawa M, Ono K, Fujita S. Venoarterial extracorporeal membrane oxygenation for severe sepsis and septic shock in 3,195 adults. Crit Care Med. 2017;44(12):440. doi: 10.1097/01.ccm.0000510133.72892.75. [DOI] [Google Scholar]
- 21.Takauji S, Hayakawa M, Ono K, Makise H. Respiratory extracorporeal membrane oxygenation for severe sepsis and septic shock in adults: a propensity score analysis in a multicenter retrospective observational study. Acute Med Surg. 2017;4(4):408–417. doi: 10.1002/ams2.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bréchot N, Luyt CE, Schmidt M, Leprince P, Trouillet JL, Léger P, Pavie A, Chastre J, Combes A. Venoarterial extracorporeal membrane oxygenation support for refractory cardiovascular dysfunction during severe bacterial septic shock. Crit Care Med. 2013;41(7):1616–1626. doi: 10.1097/CCM.0b013e31828a2370. [DOI] [PubMed] [Google Scholar]
- 23.Jenkins CR, Gomersall CD, Leung P, Joynt GM. Outcome of patients receiving high dose vasopressor therapy: a retrospective cohort study. Anaesth Intensive Care. 2009;37(2):286–289. doi: 10.1177/0310057X0903700212. [DOI] [PubMed] [Google Scholar]
- 24.Martin C, Medam S, Antonini F, Alingrin J, Haddam M, Hammad E, Meyssignac B, Vigne C, Zieleskiewicz L, Leone M. Norepinephrine: not too much. Not Too long Shock. 2015;44(4):305–309. doi: 10.1097/SHK.0000000000000426. [DOI] [PubMed] [Google Scholar]
- 25.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P: Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ (Clin Res ed) 2009, 339:b2535. [DOI] [PMC free article] [PubMed]
- 26.Github. lme4: Mixed-Effects Modelling in R. https://github.com/lme4/lme4/]. Accessed 19 Oct 2020.
- 27.Harrer M, Cuijpers P, Furukawa T, Ebert DD. Doing Meta-Analysis in R. http://dmetar.protectlab.org]. Accessed 19 Oct 2020.
- 28.Schwarzer G, Carpenter J, Rücker G. General Package for Meta-Analysis http://meta-analysis-with-r.org. Accessed 19 Oct 2020.
- 29.Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135. doi: 10.1186/1471-2288-14-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Clopper CJ, Pearson ES. The use of confidence or fiducial limits illustrated in the case of the binomial. Biometrika. 1934;26(4):404–413. doi: 10.1093/biomet/26.4.404. [DOI] [Google Scholar]
- 31.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 32.Miller JJ. The inverse of the Freeman–Tukey double arcsine transformation. Am Stat. 1978;32(4):138. [Google Scholar]
- 33.Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, Alonso-Coello P, Glasziou P, Jaeschke R, Akl EA et al: GRADE guidelines: 7. Rating the quality of evidence--inconsistency. J Clin Epidemiol 2011, 64(12):1294–1302. [DOI] [PubMed]
- 34.Iorio A, Spencer FA, Falavigna M, Alba C, Lang E, Burnand B, McGinn T, Hayden J, Williams K, Shea B et al: Use of GRADE for assessment of evidence about prognosis: rating confidence in estimates of event rates in broad categories of patients. Bmj 2015, 350:h870. [DOI] [PubMed]
- 35.Jia D, Yang IX, Ling RR, Syn N, Poon WH, Murughan K, Tan CS, Choong A, MacLaren G, Ramanathan K. Vascular complications of extracorporeal membrane oxygenation: a systematic review and meta-regression analysis. Crit Care Med. 2020;48(12):e1269–1277. doi: 10.1097/CCM.0000000000004688. [DOI] [PubMed] [Google Scholar]
- 36.Mitra S, Ling RR, Tan CS, Shekar K, Maclaren G, Ramanathan K. Concurrent use of renal replacement therapy during extracorporeal membrane oxygenation support: a systematic review and meta-analysis. J Clin Med. 2021;10(2):241. doi: 10.3390/jcm10020241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tierney JF, Vale C, Riley R, Smith CT, Stewart L, Clarke M, Rovers M: Individual participant data (IPD) meta-analyses of randomised controlled trials: guidance on their use. PLoS Med 2015, 12(7):e1001855. [DOI] [PMC free article] [PubMed]
- 38.Huang CT, Tsai YJ, Tsai PR, Ko WJ. Extracorporeal membrane oxygenation resuscitation in adult patients with refractory septic shock. J Thorac Cardiovasc Surg. 2013;146(5):1041–1046. doi: 10.1016/j.jtcvs.2012.08.022. [DOI] [PubMed] [Google Scholar]
- 39.Park TK, Yang JH, Jeon K, Choi SH, Choi JH, Gwon HC, Chung CR, Park CM, Cho YH, Sung K, et al. Extracorporeal membrane oxygenation for refractory septic shock in adults. Eur J Cardiothorac Surg. 2014;47(2):e68–74. doi: 10.1093/ejcts/ezu462. [DOI] [PubMed] [Google Scholar]
- 40.Cheng A, Sun HY, Tsai MS, Ko WJ, Tsai PR, Hu FC, Chen YC, Chang SC. Predictors of survival in adults undergoing extracorporeal membrane oxygenation with severe infections. J Thorac Cardiovasc Surg. 2016;152(6):1526–1536. doi: 10.1016/j.jtcvs.2016.08.038. [DOI] [PubMed] [Google Scholar]
- 41.Yeo HJ, Jeon D, Kim YS, Cho WH, Kim D. Veno-veno-arterial extracorporeal membrane oxygenation treatment in patients with severe acute respiratory distress syndrome and septic shock. Crit Care. 2016;20:28. doi: 10.1186/s13054-016-1205-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lee KW, Cho CW, Lee N, Choi GS, Cho YH, Kim JM, Kwon CHD, Joh JW. Extracorporeal membrane oxygenation support for refractory septic shock in liver transplantation recipients. Ann Surg Treat Res. 2017;93(3):152–158. doi: 10.4174/astr.2017.93.3.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Banjas N, Hopf HB, Hanisch E, Friedrichson B, Fichte J, Buia A. ECMO-treatment in patients with acute lung failure, cardiogenic, and septic shock: mortality and ECMO-learning curve over a 6-year period. J Intensive Care. 2018;6:84. doi: 10.1186/s40560-018-0352-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Friedrichson B, Fichte J, Banjas N, Schutz M, Hopf HB. Extracorporeal membrane oxygenation in adult patients with septic shock. Anasthesiologie und Intensivmedizin. 2018;59(12):698–704. [Google Scholar]
- 45.Kim HS, Cheon DY, Ha SO, Han SJ, Kim HS, Lee SH, Kim SG, Park S. Early changes in coagulation profiles and lactate levels in patients with septic shock undergoing extracorporeal membrane oxygenation. J Thorac Dis. 2018;10(3):1418–1430. doi: 10.21037/jtd.2018.02.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ro SK, Kim WK, Lim JY, Yoo JS, Hong SB, Kim JB. Extracorporeal life support for adults with refractory septic shock. J Thorac Cardiovasc Surg. 2018;156(3):1104–1109. doi: 10.1016/j.jtcvs.2018.03.123. [DOI] [PubMed] [Google Scholar]
- 47.Vogel DJ, Murray J, Czapran AZ, Camporota L, Ioannou N, Meadows CIS, Sherren PB, Daly K, Gooby N, Barrett N: Veno-arterio-venous ECMO for septic cardiomyopathy: a single-centre experience. Perfusion 2018, 33(1 (Suppl)):57–64. [DOI] [PubMed]
- 48.Falk L, Hultman J, Broman LM. Extracorporeal membrane oxygenation for septic shock. Crit Care Med. 2019;47(8):1097–1105. doi: 10.1097/CCM.0000000000003819. [DOI] [PubMed] [Google Scholar]
- 49.Han L, Zhang Y, Zhang Y, Wu W, He P. Risk factors for refractory septic shock treated with VA ECMO. Ann Transl Med. 2019;7:18. doi: 10.21037/atm.2018.12.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Brechot N, Haiage D, Kimmoun A, Demiselle J, Agerstand C, Montero S, Schmidt M, Luyt C, Lebreton G, Hekimian G, et al. Venoarterial extracorporeal membrane oxygenation to rescue sepsis-induced cardiogenic shock: a retrospective, multicentre, international cohort study. The Lancet. 2020;396(10250):545–552. doi: 10.1016/S0140-6736(20)30733-9. [DOI] [PubMed] [Google Scholar]
- 51.Myers LC, Lee C, Thompson BT, Cudemus G, Raz Y, Roy N: Outcomes of adult patients with septic shock undergoing extracorporeal membrane oxygenation therapy. Ann Thorac Surg 2020:871–877. [DOI] [PubMed]
- 52.Geri G, Vignon P, Aubry A, Fedou AL, Charron C, Silva S, Repessé X, Vieillard-Baron A. Cardiovascular clusters in septic shock combining clinical and echocardiographic parameters: a post hoc analysis. Intensive Care Med. 2019;45(5):657–667. doi: 10.1007/s00134-019-05596-z. [DOI] [PubMed] [Google Scholar]
- 53.Hollenberg SM, Singer M. Pathophysiology of sepsis-induced cardiomyopathy. Nat Rev Cardiol. 2021;18(6):424–434. doi: 10.1038/s41569-020-00492-2. [DOI] [PubMed] [Google Scholar]
- 54.Parker MM, Suggredini AF, Natanson C, Ognibene FP, Shelhamer JH, Parrillo JE. Responses of left ventricular function in survivors and nonsurvivors of septic shock. J Crit Care. 1989;4(1):19–25. doi: 10.1016/0883-9441(89)90087-7. [DOI] [Google Scholar]
- 55.Vincent JL, Reuse C, Frank N, Contempré B, Kahn RJ. Right ventricular dysfunction in septic shock: assessment by measurements of right ventricular ejection fraction using the thermodilution technique. Acta Anaesthesiol Scand. 1989;33(1):34–38. doi: 10.1111/j.1399-6576.1989.tb02856.x. [DOI] [PubMed] [Google Scholar]
- 56.Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345(19):1368–1377. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- 57.Tuchschmidt J, Fried J, Astiz M, Rackow E. Elevation of cardiac output and oxygen delivery improves outcome in septic shock. Chest. 1992;102(1):216–220. doi: 10.1378/chest.102.1.216. [DOI] [PubMed] [Google Scholar]
- 58.Staudacher DL, Bode C, Wengenmayer T. Four situations in which ECMO might have a chance. Intensive Care Med. 2016;42(8):1305–1306. doi: 10.1007/s00134-016-4388-2. [DOI] [PubMed] [Google Scholar]
- 59.Ramanathan K, Cove ME, Caleb MG, Teoh KL, Maclaren G. Ethical dilemmas of adult ECMO: emerging conceptual challenges. J Cardiothorac Vasc Anesth. 2015;29(1):229–233. doi: 10.1053/j.jvca.2014.07.015. [DOI] [PubMed] [Google Scholar]
- 60.Combes A, Hajage D, Capellier G, Demoule A, Lavoué S, Guervilly C, Da Silva D, Zafrani L, Tirot P, Veber B, et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. N Engl J Med. 2018;378(21):1965–1975. doi: 10.1056/NEJMoa1800385. [DOI] [PubMed] [Google Scholar]
- 61.MacLaren G. In sepsis-induced heart failure, extracorporeal membrane oxygenation can provide support. Lancet. 2020;396(10250):515–517. doi: 10.1016/S0140-6736(20)30762-5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Search strings for respective databases.
Additional file 2. Data extraction template.
Additional file 3. Joanna Briggs Institute (JBI) checklists for included studies.
Additional file 4. Preferred Reporting Items for Systematic Review and Meta-analyses (PRISMA) flowchart for study selection.
Additional file 5. Baseline demographics of studies included for systematic review.
Additional file 6. Patient outcomes of studies included for systematic review.
Additional file 7. Grading of Recommendations, Assessments, Developments and Evaluations (GRADE) approach for certainty in evidence.
Data Availability Statement
The dataset generated and analysed during the current study can be found in the included studies and their supplementary information files.