Abstract
Objective.
To ascertain whether hospital type is associated with differences in total cost and outcomes for inpatient tonsillectomy.
Study Design.
Cross-sectional analysis of the 2006, 2009, and 2012 Kids’ Inpatient Database (KID).
Subjects and Methods.
Children ≤18 years of age undergoing tonsillectomy with/without adenoidectomy were included. Risk-adjusted generalized linear models assessed for differences in hospital cost and length of stay (LOS) among children managed by (1) non–children’s teaching hospitals (NCTHs), (2) children’s teaching hospitals (CTHs), and (3) nonteaching hospitals (NTHs). Risk-adjusted logistic regression compared the odds of major perioperative complications (hemorrhage, respiratory failure, death). Models accounted for clustering of patients within hospitals, were weighted to provide national estimates, and controlled for comorbidities.
Results.
The 25,685 tonsillectomies recorded in the KID yielded a national estimate of 40,591 inpatient tonsillectomies performed in 2006, 2009, and 2012. The CTHs had significantly higher risk-adjusted total cost and LOS per tonsillectomy compared with NCTHs and NTHs ($9423.34/2.8 days, $6250.78/2.11 days, and $5905.10/2.08 days, respectively; P < .001). The CTHs had higher odds of complications compared with NCTHs (odds ratio [OR], 1.48; 95% CI, 1.15–1.91; P = .002) but not when compared with NTHs (OR, 1.19; 95% CI, 0.89–1.59; P = .23). The CTHs were significantly more likely to care for patients with comorbidities (P <.001).
Conclusion.
Significant differences in costs, outcomes, and patient factors exist for inpatient tonsillectomy based on hospital type. Although reasons for these differences are not discernable using isolated claims data, findings provide a foundation to further evaluate patient, institutional, and system-level factors that may reduce cost of care and improve value for inpatient tonsillectomy.
Keywords: cost of care, cost variation, tonsillectomy, children’s hospitals, academic medical centers, teaching hospitals
With over half million cases performed annually, tonsillectomy, ± adenoidectomy, is one of the most common pediatric surgical procedures in the United States.1 Great variation in tonsillectomy rates across geographic regions, as well as variation in cost among surgeons, has been described.2 Variation in cost of tonsillectomy at the facility level has also been shown.3,4 In a cohort of 4824 same-day adenotonsillectomies performed at a tertiary children’s hospital, average facility cost by surgeon ranged from $1156 to $1828/case, primarily due to supply cost variation related to tonsillectomy technique.3 For the same hospital network, variation in average same-day cost of adenotonsillectomies ranged, between hospitals, from $1029 to $2385/case.4
Variation also exists among perioperative practices for tonsillectomy. Studies using the Pediatric Health Information System (PHIS) database have revealed for patients ages 2 to 3 years old, admission rates vary from 10% to 90%,5 as does use of perioperative steroids, ranging from 0.3% to 98.8%, and antibiotics, ranging from 2.7% to 92.6%.6
Despite the frequency of tonsillectomies performed at both teaching and nonteaching hospitals, as well as freestanding children’s hospitals or adult and child facilities, cost variation and outcomes by hospital type and teaching status have not been previously explored. The objective of this study was to ascertain whether differences in hospital type are associated with differences in total hospital cost and outcomes following inpatient tonsillectomy care.
Methods
Data on patient encounters were analyzed from the Agency for Healthcare Research and Quality (AHRQ)–sponsored Healthcare Cost and Utilization Project Kids’ Inpatient Database (KID) from 2006, 2009, and 2012.7 The KID is an administrative data set of patients, age ≤20 years, and contains data on >10 million hospitalizations from 44 states (2012). The KID uses a sampling of pediatric discharges. To obtain national estimates, discharge weights were created according to an AHRQ protocol based on poststratification of hospitals attributed to 6 characteristics found in the American Hospital Association (AHA) hospital files: ownership or control, bed size, teaching status, rural or urban location, US region, and freestanding children’s hospital, and various outcomes of interest, such as charges/cost and length of stay (LOS), have been used to compare children’s teaching hospitals (CTHs) with other institutions.8–11 The KID is limited to inpatient hospitalization and contains discharge summary level of data.
Patients who underwent overnight hospital admission following tonsillectomy ± adenoidectomy were identified in the KID using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) principle procedures codes: 28.2 and 28.3.12 Patients were limited to those ≤18 years of age at the time of admission after surgery. Outcomes were grouped relative to the type of hospital from which patients received care: (1) CTH, (2) non–children’s teaching hospital (NCTH), or (3) nonteaching hospital (NTH). To maintain consistency across all 3 databases, a CTH designation was assigned for those hospitals with a KID_STRATUM variable (4-digit stratum used to poststratify hospital) value of 9999 and a HOSP_TEACH value of 1 (2006, 2009; 0 = nonteaching, 1 = teaching) or HOSP_LOCTEACH variable value of 3 (2012; 1 = rural, 2 = urban nonteaching, 3 = urban teaching). An NCTH designation was given if KID_STRATUM ≠ 9999 and HOSP_TEACH = 1 or HOSP_LOCTEACH = 3. An NTH designation was given if KID_STRATUM ≠ 9999 and HOSP_TEACH = 0 or HOSP_LOCTEACH = 1 or 2. The Partners Human Research Committee deemed the study exempt from ethical review.
Outcome Measures
The primary outcome measure was total hospital cost for tonsillectomy-related inpatient care in 2015 US dollars. Hospital costs were calculated from total hospital charges by multiplying charges by hospital-specific cost-to-charge ratios (CCRs, created by dividing the inpatient costs by the inpatient charges; does not include professional fees) for the corresponding year.7 Costs were converted to 2015 US dollars using annual Hospital Consumer Price Indices.
Secondary outcome measures included LOS in days and the occurrence of at least 1 of 3 major perioperative complications of tonsillectomy during the same admission. Major complications included immediate posttonsillectomy hemorrhage (secondary ICD-9-CM procedure code 28.7), respiratory failure requiring invasive mechanical ventilation (secondary ICD-9-CM procedure codes 96.70, 96.71, and 96.72), and in-hospital mortality. Use of mechanical ventilation was chosen as a proxy for respiratory complications due to its use in other studies investigating complications following tonsillectomy6,13 and its frequent use in the treatment of postoperative pulmonary edema.
Demographic Characteristics
Additional covariate information was abstracted on patient age (categorized as 1–3, 4–6, 7–12, and 13–18 years), sex, race/ethnicity (categorized as non-Hispanic White, non-Hispanic Black, Hispanic, Asian/Pacific Islander, non-Hispanic other, or misreported/unreported), primary payer (categorized as private, Medicaid, self-pay, or other), median income quartile, year, and indication for tonsillectomy (categorized as obstructive sleep apnea [OSA, ICD-9-CM codes 320.20 327.23, 474.10, 474.11, and 786.09], infectious [463, 474.00, 474.02, and 475], both, or other).
To characterize the burden of comorbidity for each individual patient, a multispecialty pediatric surgical risk score, created and validated in 2013 by Rhee et al14 for use in pediatric surgical populations, was used. Sixty-nine clinical categories, sex, and age <2 years were used to generate this risk score. In their training data set, a risk score of 0 was associated with a <0.001% mortality rate, and a score of ≥6 was associated with a 33.5% mortality rate. Further details regarding generation of this score can be found in the cited work by Rhee et al.14 Obesity (278.00, 278.01) was not accounted for and was therefore added as a separate risk factor.
Institutional factors extracted included geographical region of the hospital (Northeast, Midwest, South, West), teaching status, and children’s hospital designation.
Statistical Analyses
Statistical analyses were performed using Stata software, version 13.1 (StataCorp LP, College Station, Texas). All tests of significance were 2-sided (P < .05). Generalized linear models (family gamma, link log) followed by postestimation of average marginal effects were used to attain risk-adjusted predicted mean differences and standard errors for nonnormally distributed continuous total hospital cost and LOS. Multivariable logistic regression was used to attain risk-adjusted odds ratios (ORs) and corresponding 95% confidence intervals (95% CIs) for the binary outcome of complication. Multivariable linear regression was used to attain the absolute percentage point difference in complications attributable to each covariate. For example, linear regression resulting in a coefficient of 0.1 represents an absolute percentage point increase of 10 points compared with the reference value. All models were risk-adjusted, using included covariates. Multilevel models with robust standard errors accounted for clustering of patients within hospitals. Models were further weighted using KID-provided design weights to attain nationally representative effects. Akaike’s information criterion was used to determine appropriateness of model fit.
Results
Patient Characteristics
An unweighted total of 25,685 pediatric discharges following overnight admission for tonsillectomy were included: 8914 in 2006, 9172 in 2009, and 8808 discharges in 2012. The weighted national sample consisted of a total of 40,591 pediatric tonsillectomy patients for all 3 years combined. Table 1 presents differences in patient demographic characteristics by hospital type: CTH, NCTH, or NTH. Of inpatient tonsillectomies, 53.8% were performed at 826 NCTHs (weighted 20,176 pediatric discharges), 24.6% (n = 10,220) at 80 CTHs, and 21.6% (n = 8235) at 1368 NTHs. Within each geographical region, CTHs made up 2% to 4.5% of all hospitals in that region.
Table 1.
Demographic Characteristics by Hospital Designation, Weighted Frequencies, and Percentages.a
| Characteristic | Children’s Teaching Hospital (n = 10,220) | Non–Children’s Teaching Hospital (n = 20,176) | Nonteaching Hospital (n = 8235) |
|---|---|---|---|
| Age, mean (SD), y | 4.74 (4.16) | 5.08 (4.36) | 6.10 (5.29) |
| Categorical age, y | |||
| 0–3 | 5657 (56.00) | 10359 (51.84) | 4059 (49.77) |
| 4–6 | 1917 (18.98) | 4299 (21.51) | 1365 (16.74) |
| 7–12 | 1701 (16.84) | 3388 (16.95) | 1309 (16.05) |
| 13–18 | 826 (8.18) | 1939 (9.70) | 1422 (17.44) |
| Sex | |||
| Male | 6004 (59.24) | 11,773 (59.04) | 4523 (56.10) |
| Female | 4131 (40.76) | 8169 (40.96) | 3539 (43.90) |
| Race/ethnicity | |||
| Non-Hispanic white | 3330 (32.58) | 7645 (37.89) | 4091 (49.68) |
| Non-Hispanic black | 1844 (18.05) | 4297 (21.30) | 767 (9.31) |
| Hispanic | 2119 (20.73) | 3586 (17.78) | 966 (11.73) |
| Asian/Pacific Islander | 209 (2.05) | 435 (2.16) | 117 (1.42) |
| Non-Hispanic other | 551 (5.39) | 1184 (5.87) | 341 (4.14) |
| Missing/unreported | 2167 (21.20) | 3029 (15.01) | 1953 (23.72) |
| Income quartile | |||
| First—lowest | 2922 (28.88) | 5590 (28.69) | 2266 (28.16) |
| Second | 2331 (23.04) | 4538 (23.29) | 2243 (27.89) |
| Third | 2592 (25.62) | 4508 (23.14) | 1726 (21.46) |
| Fourth—highest | 2271 (22.45) | 4848 (24.88) | 1809 (22.49) |
| Primary payer | |||
| Private | 4153 (40.71) | 9324 (46.36) | 4547 (55.44) |
| Medicaid | 5434 (53.26) | 9611 (47.79) | 3194 (38.94) |
| Self-pay | 182 (1.78) | 458 (2.28) | 90 (1.09) |
| Other | 434 (4.24) | 719 (3.58) | 372 (4.53) |
| Pediatric surgical risk score, mean (SD) | 0.3427 (0.68) | 0.252 (0.55) | 0.161 (0.44) |
| Score >1 | 2629 (26.24) | 4166 (20.89) | 6947 (13.82) |
| Obesity | 676 (6.61) | 1227 (6.08) | 277 (3.36) |
| Indications for tonsillectomy | |||
| Obstructive sleep apnea | 8643 (84.57) | 15,283 (75.75) | 4161 (50.53) |
| Infectious | 878 (8.59) | 2505 (12.41) | 2782 (33.78) |
| Both | 544 (5.32) | 1978 (9.8) | 1144 (13.89) |
| Other | 155 (1.52) | 410 (2.03) | 147 (1.79) |
| KID year of tonsillectomy | |||
| 2006 | 2989 (29.25) | 7453 (36.94) | 3486 (42.33) |
| 2009 | 3263 (31.92) | 6097 (30.22) | 2982 (36.22) |
| 2012 | 3968 (38.83) | 6626 (32.84) | 1767 (21.45) |
Abbreviation: KID, Kids’ Inpatient Database.
Values are presented as number (%) unless otherwise indicated.
Figure 1 shows patient characteristics by hospital designation. The CTHs had the highest proportion of patients 3 years of age and younger (56%, P < .001). Children managed by NTHs were significantly more likely to be non-Hispanic white with lower percentages of non-Hispanic black and Hispanic patients relative to CTHs and NCTHs. Both CTHs and NCTHs had a higher percentage of obese patients (6.61% and 6.1%, respectively) compared with NTHs (3.36%, P < .001). Sex, median income quartile, and pediatric surgical risk score were comparable among hospital types. However, the percentage of patients with a risk score of 1 or greater was highest at CTHs (26.24%) compared with NCTHs (20.89%) and NTHs (13.82%, P < .001). The proportion of Medicaid patients significantly increased going from NTHs to NCTHs to CTHs; the converse trend was seen among privately insured patients.
Figure 1.
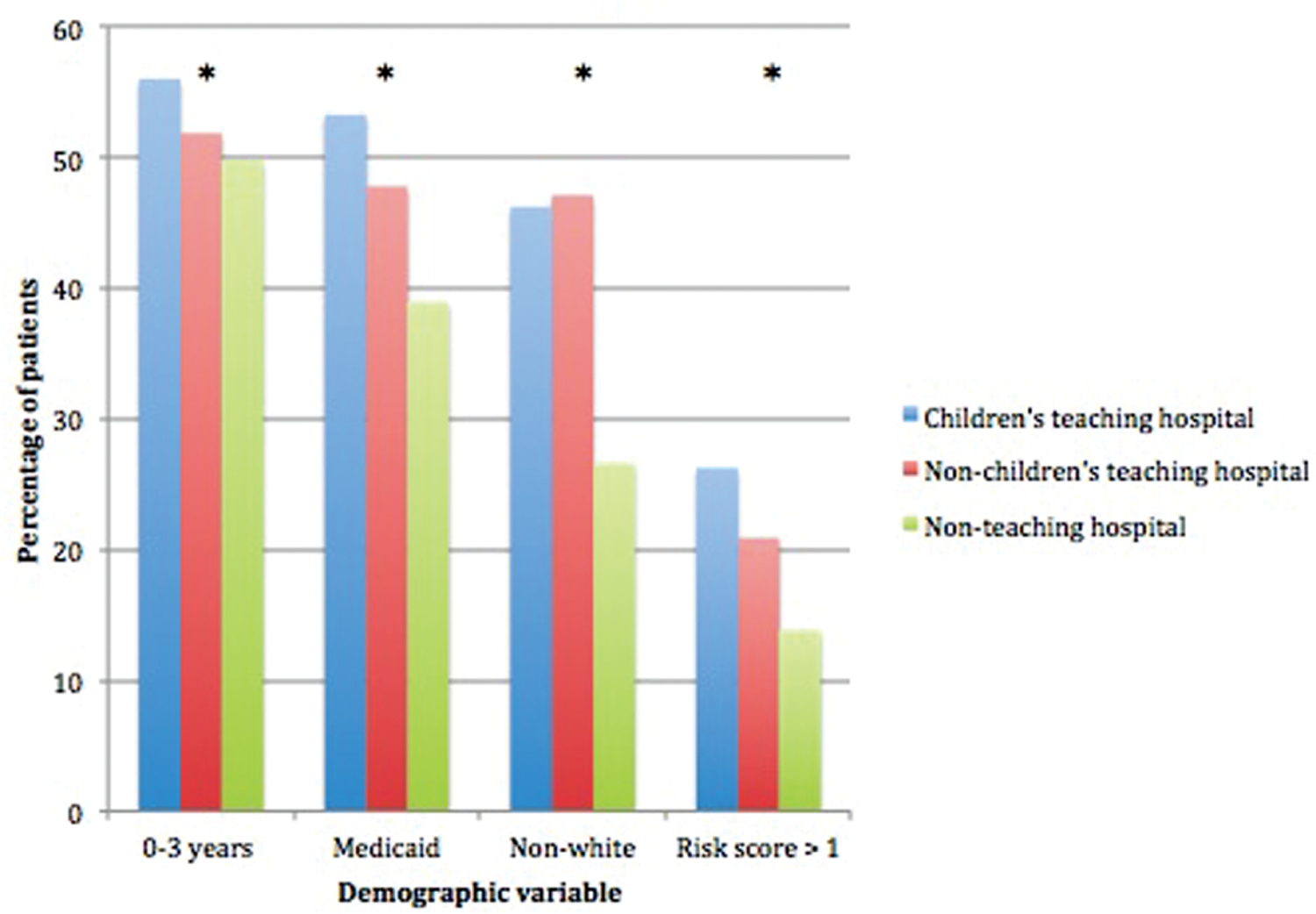
Patient characteristics by hospital designation demonstrate a significant difference in the demographics of patients seen at each hospital type. *P <.001.
The most common indication for inpatient tonsillectomy varied. Of patients admitted to CTHs, 84.6% underwent tonsillectomies for OSA relative to 75.8% at NCTHs and 50.5% at NTHs (P < .001). In contrast, 38.9% of patients at NTHs underwent tonsillectomy for infectious indications (8.59% at CTHs and 12.4% at NCTHs, P < .001). Supplemental Tables S1 and S2 (available online at www.oto-journal.org) present unadjusted and risk-adjusted results comparing differences in demographic covariates, respectively.
Unadjusted Cost and Outcome Results
Unadjusted total hospital costs, LOS, and major postoperative complications by hospital type are presented in Table 2. Weighted differences in 2015 US dollars reveal costs were highest for patients admitted at CTHs with total median hospital costs of $6000 (interquartile range [IQR], $4200–$9300). Patients treated at NCTHs and NTHs had similar median costs of $4200 (IQR, $3100–$5800) and $3800 (IQR, $2800–$5400), respectively. CTHs were associated with a longer median LOS of 2 days (IQR, 1–3 days), compared with both NCTHs and NTHs, which had a median LOS of 1 day (IQR, 1–2 days). (Note: One day indicates 23-hour admissions.) CTHs had a higher percentage of major postoperative complications during the admission (2.94%) compared with NCTHs (1.9%) or NTHs (1.91%, P < .001).
Table 2.
Unadjusted Outcome Measures by Managing Hospital Designation, Unweighted Frequencies, and Weighted Percentages.
| Outcome | Children’s Teaching Hospital (n = 10,220) | Non–Children’s Teaching Hospital (n = 20,176) | Nonteaching Hospital (n = 8235) |
|---|---|---|---|
| Total hospital costs, median (IQR) | 6040.63 (4183.92–9270.56) | 4155.35 (3077.19–5769.43) | 3798.94 (2823.94–5364.43) |
| Length of stay in days, median (IQR) | 2 (1–3) | 1 (1–2) | 1 (1–2) |
| Complications, No. (%) | 248 (2.94) | 384 (1.9) | 158 (1.91) |
| Hemorrhage | 143 (1.4) | 192 (0.95) | 111 (1.34) |
| Respiratory failure | 147 (1.44) | 189 (0.93) | 47 (0.57) |
| Death | ≤10 | ≤10 | ≤10 |
Abbreviation: IQR, interquartile range.
Univariate regression revealed that, relative to NCTHs, children managed at CTHs experienced an unadjusted predicted mean difference (mean increase or decrease compared with the reference category—in this case, NCTHs) in total hospital costs that was $4700 higher per patient (95% CI, $3200–$6300). Relative to NTHs, the unadjusted predicted mean difference in total hospital cost per patient was nearly $5700 (95% CI, $4100–$7240) higher at CTHs. Relative to NCTHs, children managed at CTHs experienced an unadjusted predicted mean difference in LOS that was longer by an average of 0.95 days (95% CI, 0.58–1.32), with an average LOS at CTHs, NCTHs, and NTHs of 3.04, 2.09, and 1.88 days, respectively. CTHs had a 56% higher unadjusted odds of major postoperative complications (OR, 1.56; 95% CI, 1.22–1.99) compared with NCTHs. NTHs exhibited marginally shorter LOS (−0.213; 95% CI, −0.42 to −0.009 days) and no difference in the unadjusted odds of a major complication compared with NCTHs (Table 3).
Table 3.
Unadjusted Cost and Outcomes, Univariate Regression Results by Hospital Type, Weighted Data.a
| Total Hospital Cost, Univariate Regression (2015 Dollars) |
Length of Stay, d |
Hemorrhage |
Respiratory Failure |
Overall Complications |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Hospital Designation | Mean Difference | 95% CI | Mean Difference | 95% CI | Odds Ratio | 95% CI | Odds Ratio | 95% CI | Odds Ratio | 95% CI |
| Non-children’s teaching hospital | Reference | Reference | Reference | Reference | Reference | |||||
| Children’s teaching hospital | 4734.06 | 3201.13 to 6266.99b | 0.951 | 0.581 to 1.322b | 1.50 | 1.10 to 2.04b | 1.57 | 1.08 to 2.28b | 1.56 | 1.22 to 1.99b |
| Nonteaching hospital | −964.63 | −1611.04 to −318.21b | −0.214 | −0.418 to −0.009b | 1.39 | 1.03 to 1.87b | 0.60 | 0.36 to 1.00 | 1.01 | 0.77 to 1.31 |
Interpretation: mean difference—for example, average total hospital costs for pediatric tonsillectomies preformed at children’s teaching hospitals were $4730 (95% CI, $3200–$6270) higher than average total hospitals costs for pediatric tonsillectomies performed at non–children’s teaching hospitals. Odds ratio—the odds of complications at children’s teaching hospitals were 1.56 (95% CI, 1.32–1.94) times higher than the odds of complications at non–children’s teaching hospitals.
Indicates statistical significance (2-sided P <.05).
Multivariable Cost and Outcomes Results
Risk-adjusted total hospital cost and outcomes by hospital type are presented in Table 4 (NCTH reference group) and Table 5 (NTH reference group). Average adjusted cost per patient for inpatient tonsillectomy using regression analysis was $9403.65, $6247.78, and $5919.63 for CTHs, NCTHs, and NTHs, respectively. Pediatric tonsillectomy patients managed by CTHs cost a risk-adjusted average of $3156 more per patient (95% CI, $2170–$4142) compared with NCTHs; compared with patients admitted at NTHs, patients admitted to CTHs cost a risk-adjusted average of $3484 more per patient (95% CI, $2504–$4463). Differences between NCTHs and NTHs were not significant. Risk-adjusted covariate results presented in Supplemental Table S2 (available online) reveal significant increases in predicted mean cost associated with decreasing age, male sex, non-Hispanic black or Asian race/ethnicity, Medicaid insurance coverage, and year. Each point increase in pediatric surgical risk score resulted in an increase in total hospital cost of $4500 (95% CI, $4100–$5000). Presence of obesity led to an increase in total hospital costs by $1030 (95% CI, $467–$1593).
Table 4.
Risk-Adjusted Cost and Outcome Regression Results by Managing Hospital Designation, Weighted.a
| Total Hospital Cost (2015 Dollars) |
Length of Stay, d |
Hemorrhage |
Respiratory Failure |
Overall Complications |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Hospital Designation | Mean Difference | 95% CI | Mean Difference | 95% CI | Odds Ratio | 95% CI | Odds Ratio | 95% CI | Odds Ratio | 95% CI |
| Non–children’s teaching hospital | Reference | Reference | Reference | Reference | Reference | |||||
| Children’s teaching hospital | 3155.87 | 2169.75 to 4141.99b | 0.69 | 0.45 to 0.93b | 1.58 | 1.14 to 2.20b | 1.32 | 0.86 to 2.03 | 1.48 | 1.15 to 1.91b |
| Nonteaching hospital | −328.16 | −811.24 to 154.92 | −0.023 | −0.18 to 0.136 | 1.33 | 0.95 to 1.86 | 0.95 | 0.58 to 1.55 | 1.24 | 0.94 to 1.63 |
Interpretation: mean difference—for example, average total hospital costs for pediatric tonsillectomies preformed at children’s teaching hospitals were $3160 (95% CI, $2170–$4150) higher than average total hospitals costs for pediatric tonsillectomies performed at non–children’s teaching hospitals. Odds ratio—the odds of complications at children’s teaching hospitals were 1.48 (95% CI, 1.32–1.94) times higher than the odds of complications at non–children’s teaching hospitals.
Indicates statistical significance (2-sided P <.05).
Table 5.
Risk-Adjusted Cost and Outcome Regression Results by Managing Hospital Designation, Weighted Data.a
| Total Hospital Cost (2015 Dollars) |
Length of Stay, d |
Hemorrhage |
Respiratory Failure |
Overall Complications |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Hospital Designation | Mean Difference | 95% CI | Mean Difference | 95% CI | Odds Ratio | 95% CI | Odds Ratio | 95% CI | Odds Ratio | 95% CI |
| Nonteaching hospital | Reference | Reference | Reference | Reference | Reference | |||||
| Non–children’s teaching hospital | 328.16 | −154.92 to −811.24 | 0.023 | −0.14 to 0.18 | 0.75 | 0.54 to 1.05 | 1.05 | 0.64 to 1.73 | 0.81 | 0.61 to 1.07 |
| Children’s teaching hospital | 3484.03 | 2504.79 to 4463.26b | 0.71 | 0.46 to 0.96b | 1.19 | 0.84 to 1.69 | 1.4 | 0.81 to 2.42 | 1.24 | 0.89 to 1.59 |
Interpretation: mean difference—for example, average total hospital costs for pediatric tonsillectomies preformed at children’s teaching hospitals were $3520 (95% CI, $2540–$4500) higher than average total hospitals costs for pediatric tonsillectomies performed at non–children’s teaching hospitals. Odds ratio—the odds of complications at children’s teaching hospitals were 1.24 (95% CI, 0.89–1.59) times higher than the odds of complications at non–children’s teaching hospitals.
Indicates statistical significance (2-sided P <.05).
Average risk-adjusted LOS were 2.11, 2.80, and 2.08 days for NCTHs, CTHs, and NTHs, respectively. Adjusted differences in LOS suggested that, relative to NCTHs and NTHs, children admitted to CTHs stayed in the hospital 0.69 (95% CI, 0.45–0.93) and 0.72 (95% CI, 0.47–0.97) additional days, respectively (Tables 4 and 5). NTHs did not demonstrate a significant difference in LOS compared with NCTHs. Age younger than 13 years was correlated with significantly shorter LOS, while non-Hispanic black race and Medicaid insurance were associated with marginally significant increase in LOS (Suppl. Table S2, available online). Increasing income quartile was significantly associated with progressively shorter LOS. A 1-point increase in pediatric surgical risk score corresponded to a significant increase in LOS of 1.43 additional days (95% CI, 1.30–1.57), and the presence of obesity was associated with a 0.23-day increase in LOS (95% CI, 0.022–0.434).
Inpatient tonsillectomy at a CTH was associated with 1.48 times higher risk-adjusted odds of experiencing a tonsillectomy-related major postoperative complication (95% CI, 1.15–1.91) relative to patients admitted at NCTHs (Table 4). In terms of absolute percentage point difference in rate of major complications, CTHs saw a 0.54% (95% CI, 0.13%−0.95%) increase in posttonsillectomy hemorrhage and a 0.84% (95% CI, 0.28%−1.39%) increase in overall major complication rate (Table 6). No significant differences were found comparing patients managed at NCTHs vs NTHs or CTHs vs NTHs (Tables 4 and 5).
Table 6.
Multivariate Linear Regression Results for Complications by Hospital Type, Weighted Data.a
| Hemorrhage |
Respiratory Failure |
Overall Complications |
||||
|---|---|---|---|---|---|---|
| Hospital Designation | Percent Increase | 95% CI | Percent Increase | 95% CI | Percent Increase | 95% CI |
| Non–children’s teaching hospital | Reference | Reference | Reference | |||
| Children’s teaching hospital | 0.54 | 0.13 to 0.95b | 0.25 | −0.18 to 0.68 | 0.84 | 0.28 to 1.39 |
| Nonteaching hospital | 0.32 | −0.07 to 0.7 | 0.19 | −0.13 to 0.52 | 0.54 | 0.03 to 1.06 |
Interpretation: percent increase—for example, absolute percentage point increase in rate of posttonsillectomy hemorrhage for pediatric tonsillectomies performed at children’s teaching hospitals was 0.54 points higher than average rate of posttonsillectomy hemorrhage for pediatric tonsillectomies performed at non–children’s teaching hospitals.
Indicates statistical significance (2-sided P <.05).
Significant covariate differences in the risk-adjusted odds of complications were found comparing patients aged 0 to 3 years vs patients aged 13 to 18 years, as well as by sex, income, and year (Suppl. Table S2, available online). Non-Hispanic black patients had 37% higher odds of major complications (95% CI, 1.05–1.77) relative to non-Hispanic white patients. Each point in the surgical risk score corresponded to 2.87-times odds of major complications (95% CI, 2.55–3.23). Obesity was not associated with increased odds of complications.
Discussion
Although the steadily increasing cost of health care in the United States has recently begun to slow its ascent,15 the United States continues to be one of the most expensive countries in which to receive care.16 Therefore, the high cost of care at teaching hospitals without obvious improvement in outcomes is still debated.17 The results of this study demonstrate significant differences in hospital type associated with cost and outcomes of inpatient tonsillectomy care, with the adjusted cost at CTHs $3500 to $4700 higher per patient. This represents a 30% to 40% increase in cost in this subset of patients. By conservatively estimating that 500,000 pediatric tonsillectomies are performed annually, inpatient tonsillectomies represent ~3% of all tonsillectomies.
CTHs offer increased availability of subspecialists and advanced treatment technology thought to be beneficial in severe surgical cases.18–21 These resources undeniably benefit certain patients, including children with severe disease, complex or uncommon medical conditions, and children who undergo surgeries requiring specialized training.8,9,22,23 Results of our study suggest cost is higher at CTHs for tonsillectomy. This finding may be due to the complexity of patients treated at CTHs, inclusive of OSA severity, age, and comorbidities. Perhaps healthier patients treated at CTHs are more likely to undergo outpatient tonsillectomy, as opposed to those treated at NCTHs or NTHs. In that case, it is possible that overall cost/tonsillectomy may be lower when all tonsillectomies are included.
Previous studies in both the adult and pediatric literature have found differences in the cost of care at teaching vs nonteaching and at children’s vs non–children’s teaching hospitals.8,9,22–25 Whether claiming clear benefit24 or calling for better implementation of lessons learned,8,9,22,23,25 differences in the cost of pediatric care by hospital type appear to play a considerable role. One study looking at medical conditions requiring admission at children’s vs non–children’s hospitals demonstrated no significant difference in median LOS between the 2 groups despite an overall increase in charges associated with admission to a CTH.8 In the pediatric surgery literature, studies looking at cost and outcomes of care for various surgeries/surgical conditions, including appendicitis,26,27 pyloromyotomy,9 congenital cardiac surgery,28,29 and intussusception,30 have shown significant variation between costs and outcomes both between children’s and non–children’s hospitals and within freestanding children’s hospitals. For example, pyloromyotomy at CTHs resulted in increased cost of care but statistically shorter LOS and lower complication rate (although clinically, these were low at all hospitals).9 For appendicitis, cost was again higher at CTHs, but the odds of complications were half that of non–children’s hospitals.26 Like our study, these studies have all determined that reasons for these differences should be explored, and best practices should be identified to improve value-based care for our patients.
Strengths of this study include a large sample size and professional coding used by the AHRQ in the KID. Administrative databases have the ability to support a well-powered study, provide patient-level data, use weights to provide a nationally representative sample, and show variation between hospitals, as opposed to single-institution retrospective studies.31 Given the consistency of the findings, the degree of significance of the findings, and this large sample size, we feel the results accurately represent important differences in costs seen between the different types of hospitals.
There are limitations to this analysis. First, other factors might have contributed to increased cost despite risk adjustment. Moreover, the surgical risk scores cannot account for severity of OSA. Due to the lack of patient-level clinical data available, it is possible there is an underlying difference in the populations of children treated at each type of hospital, such as severity of OSA (ie, severity of OSA may correlate with increased LOS and cost in obese patients). Use of an administrative database is limited by lack of potentially important clinical data that may be able to explain some of these observed differences. Facility-level factors, such as case mix index, were not assessed using this database and could represent an unaccounted for selection bias. Use of data coded by ICD-9-CM codes does have limitations on the analysis, as the data set includes missing data, miscoded diagnoses, and miscoded procedures. Last, because long-term outcomes cannot be assessed with this database, clinically relevant measures, such as quality of life and improvement of OSA, cannot be reported.
Future patient-oriented research should ascertain whether children who are otherwise healthy accrue the same costs as children with severe OSA, very young age, and comorbidities at a CTH after tonsillectomy. In addition, gathering data on patient-reported outcomes, including shared decision making and patient/family experience in a CTH setting, which might directly translate to improved quality at a higher cost, could provide further insight.32 Assessment of costs and outcomes for outpatient tonsillectomy based on hospital type should be determined in the same manner. Differences in admission criteria at different types of hospitals may drive disparities in cost and outcomes, and generation of a more uniform recommendation for admission after tonsillectomy may lead to a decrease in admissions and overall savings to the health care system.
Conclusion
Significant differences in cost of care and outcomes exist for inpatient tonsillectomy based on hospital type. Further studies evaluating patient- and facility-level factors that contribute to this variation will help determine why differences exist. Current existing national databases do not appear to provide the level of data necessary to carry out this analysis. Creation of a registry, such as that proposed by the American Academy of Otolaryngology-Head and Neck Surgery or expansion of the pediatric National Surgical Quality Improvement Program to include tonsillectomy, may allow this question to be answered in the future. This increased knowledge regarding value-based care can help reduce overall costs to the health care system.
Supplementary Material
Acknowledgments
The authors thank Fizan Abdullah, MD, PhD, who provided the statistical support necessary to use the multispecialty pediatric surgical risk score in this study for risk adjustment.
Disclosures
Competing interests: Emily F. Boss received a grant (1K08 HS22932–01) from the Agency for Healthcare Research and Quality, the Johns Hopkins Clinician Scientist Award, and the American Society of Pediatric Otolaryngology Career Development Award. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
Sponsorships: None.
Funding source: None.
Footnotes
Supplemental Material
Additional supporting information may be found at http://otojournal.org/supplemental.
References
- 1.Baugh RF, Archer SM, Mitchell RB, et al. Clinical practice guideline: tonsillectomy in children. Otolaryngol Head Neck Surg. 2011;144(1)(suppl):S1–S30. [DOI] [PubMed] [Google Scholar]
- 2.Boss EF, Marsteller JA, Simon AE. Outpatient tonsillectomy in children: demographic and geographic variation in the United States, 2006. J Pediatr. 2012;160:814–819. [DOI] [PubMed] [Google Scholar]
- 3.Meier JD, Duval M, Wilkes J, et al. Surgeon dependent variation in adenotonsillectomy costs in children. Otolaryngol Head Neck Surg. 2014;150:887–892. [DOI] [PubMed] [Google Scholar]
- 4.Meier JD, Zhang Y, Greene TH, Curtis JL, Srivastava R. Variation in pediatric outpatient adenotonsillectomy costs in a multihospital network. Laryngoscope. 2015;125:1215–1220. [DOI] [PubMed] [Google Scholar]
- 5.Goyal SS, Shah R, Roberson DW, Schwartz ML. Variation in post-adenotonsillectomy admission practices in 24 pediatric hospitals. Laryngoscope. 2013;123:2560–2566. [DOI] [PubMed] [Google Scholar]
- 6.Mahant S, Keren R, Localio R, et al. Variation in quality of tonsillectomy perioperative care and revisit rates in children’s hospitals. Pediatrics. 2014;133:280–288. [DOI] [PubMed] [Google Scholar]
- 7.Healthcare Cost and Utilization Project (HCUP). Kids’ Inpatient Database (KID). Rockville, MD: HCUP; 2006, 2009, 2012. [Google Scholar]
- 8.Merenstein D, Egleston B, Diener-West M. Lengths of stay and costs associated with children’s hospitals. Pediatrics. 2005;115: 839–844. [DOI] [PubMed] [Google Scholar]
- 9.Raval MV, Cohen ME, Barsness KA, Bentrem DJ, Phillips JD, Reynolds M. Does hospital type affect pyloromyotomy outcomes? Analysis of the Kids’ Inpatient Database. Surgery. 2010; 148:411–419. [DOI] [PubMed] [Google Scholar]
- 10.Lander L, Lu S, Shah RK. Pediatric retropharyngeal abscesses: a national perspective. Int J Pediatr Otorhinolaryngol. 2008; 72:1837–1843. [DOI] [PubMed] [Google Scholar]
- 11.Zhao SZ, Wong JM, Arguelles LM. Hospitalization costs associated with leiomyoma. Clin Ther. 1999;21:563–575. [DOI] [PubMed] [Google Scholar]
- 12.International Classification of Diseases, Ninth Revision, Clinical Modification. Chicago, IL: American Medical Association; 2007. [Google Scholar]
- 13.Sun GH, Auger KA, Aliu O, Patrick SW, DeMonner S, Davis MM. Variation in inpatient tonsillectomy costs within and between US hospitals attributable to postoperative complications. Med Care. 2013;51:1048–1054. [DOI] [PubMed] [Google Scholar]
- 14.Rhee D, Salazar JH, Zhang Y, et al. A novel multispecialty surgical risk score for children. Pediatrics. 2013;131:e829–e836. [DOI] [PubMed] [Google Scholar]
- 15.Hartman M, Martin AB, Lassman D, Catlin A; National Health Expenditure Accounts Team. National health spending in 2013: growth slows, remains in step with the overall economy. Health Aff. 2015;34:150–160. [DOI] [PubMed] [Google Scholar]
- 16.Davis K, Stremekis K, Schoen C, Squires D. Mirror, Mirror on the Wall, 2014 Update: How the U.S. Health Care System Compares Internationally. Boston, MA: The Commonwealth Fund; 2014. [Google Scholar]
- 17.Ayanian JZ, Weissman JS. Teaching hospitals and quality of care: a review of the literature. Milbank Q. 2002;80:569–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Birkmeyer JD, Siewers AE, Finlayson EVA, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346:1128–1137. [DOI] [PubMed] [Google Scholar]
- 19.Jenkins KJ, Newburger JW, Lock JE, Davis RB, Coffman GA, Iezzoni LI. In-hospital mortality for surgical repair of congenital heart defects: preliminary observations of variation by hospital caseload. Pediatrics. 1995;95:323–330. [PubMed] [Google Scholar]
- 20.Smink DS, Finkelstein JA, Kleinman K, Fishman SJ. The effect of hospital volume of pediatric appendectomies on the misdiagnosis of appendicitis in children. Pediatrics. 2004;113: 18–23. [DOI] [PubMed] [Google Scholar]
- 21.Phibbs CS, Bronstein JM, Buxton E, Phibbs RH. The effects of patient volume and level of care at the hospital of birth on neonatal mortality. JAMA. 1996;276:1054–1059. [PubMed] [Google Scholar]
- 22.Cosper GH, Hamann MS, Stiles A, Nakayama DK. Hospital characteristics affect outcomes for common pediatric surgical conditions. Am Surg. 2006;72:739–745. [PubMed] [Google Scholar]
- 23.Gupta RS, Bewtra M, Prosser LA, Finkelstein JA. Predictors of hospital charges for children admitted with asthma. Ambul Pediatr. 2006;6:15–20. [DOI] [PubMed] [Google Scholar]
- 24.Snow BW. Does surgical subspecialty care come with a higher price? Curr Opin Pediatr. 2005;17:407–408. [DOI] [PubMed] [Google Scholar]
- 25.Evans C, van Woerden HC. The effect of surgical training and hospital characteristics on patient outcomes after pediatric surgery: a systematic review. J Pediatr Surg. 2011;46:2119–2127. [DOI] [PubMed] [Google Scholar]
- 26.Tian Y, Heiss KF, Wulkan ML, Raval MV. Assessment of variation in care and outcomes for pediatric appendicitis at children’s and non-children’s hospitals. J Pediatr Surg. 2015; 50(11):1885–1892. [DOI] [PubMed] [Google Scholar]
- 27.Rice-Townsend S, Barnes JN, Hall M, Baxter JL, Rangel SJ. Variation in practice and resource utilization associated with the diagnosis and management of appendicitis at freestanding children’s hospitals: implications for value-based comparative analysis. Ann Surg. 2014;259:1228–1234. [DOI] [PubMed] [Google Scholar]
- 28.Pasquali SK, Jacobs ML, He X, et al. Variation in congenital heart surgery costs across hospitals. Pediatrics. 2014;133: e553–e560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chan T, Kim J, Minich LL, Pinto NM, Waitzman NJ. Surgical volume, hospital quality, and hospitalization cost in congenital heart surgery in the United States. Pediatr Cardiol. 2015;36: 205–213. [DOI] [PubMed] [Google Scholar]
- 30.Rice-Townsend S, Chen C, Barnes JN, Rangel SJ. Variation in practice patterns and resource utilization surrounding management of intussusception at freestanding Children’s Hospitals. J Pediatr Surg. 2013;48:104–110. [DOI] [PubMed] [Google Scholar]
- 31.Boss EF, Shah RK. An overview of administrative and national survey databases for use in otolaryngology research. Otolaryngol Head Neck Surg. 2013;148:711–716. [DOI] [PubMed] [Google Scholar]
- 32.Boss EF, Thompson RE. Patient satisfaction in otolaryngology: can academic institutions compete? Laryngoscope. 2012; 122:1000–1009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


