Abstract
Objectives
To gain insight into willingness and its influencing factors to vaccinate against COVID-19 among health care workers (HCWs), and provide a scientific basis for more reasonable epidemic prevention and control strategies.
Methods
A comprehensive literature search was conducted in 4 English databases (PubMed, EMBASE, Web of Science and the Cochrane Library) and 4 Chinese databases (Chinese National Knowledge Infrastructure (CNKI), the Chongqing VIP Chinese Science (VIP), Wanfang Database and China Biomedical Literature Database (CBM)) to collect the related studies. Quality evaluation was carried out for papers meeting the inclusion criteria using 6 items from the Downs and Black assessment checklist. The STATA statistical software version 15.1 was hired to perform meta-analysis.
Results
Nine records with a total of 24,952 subjects were included in this meta-analysis. The results of this meta-analysis revealed that the pooled effect value of COVID-19 vaccination willingness among HCWs using a random-effects model was 51% (95% confidence interval (CI) 0.41-0.62). Male, aged 30 years or older, having a history of prior influenza vaccination were facilitators for HCWs’ intention to vaccinate against COVID-19 (odds ratio (OR) 1.82, 95% CI 1.37-2.41, P = .000, I2 = 59.4%; OR 1.32, 95% CI 1.16-1.51, P = .000, I2 = 31.7%; OR 2.97, 95% CI 1.82-4.84, P = .000, I2 = 88.1%). The impact of occupation on HCWs’ intention to get vaccinated could not yet be definitively confirmed (OR 0.85, 95% CI 0.69-1.06, P = .160, I2 = 85.5%).
Conclusion
COVID-19 vaccination acceptance of HCWs was at moderate level. Strengthening awareness of COVID-19 vaccine among HCWs, particularly female HCWs under 30 years who have no history of prior influenza vaccination, is crucial to eliminate concerns about vaccination and promote the application of COVID-19 vaccine in this population.
Key words: COVID-19, Willingness, Influencing factors, Acceptance
Introduction
Coronavirus disease 2019 (COVID-19) is a serious and lethal contagious disease caused by infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which is mainly transmitted from human to human through respiratory droplets.1 The clinical picture of COVID-19 is dominated by the presence of fever, fatigue, cough, headache, diarrhea, hemoptysis and dyspnea.2 COVID-19 is spreading across the world at an alarming rate, being formally declared as a pandemic and a public health emergency of international concern (PHEIC) by the World Health Organization (WHO).3 , 4 As on 6th April 2021, the global prevalence data of COVID-19 collected from the WHO website revealed 131,309,792 confirmed cases and 2,854,276 deaths.5 Of note, it is a pity that the availability of only limited symptomatic support therapy options and the absence of specific antiviral medicine for COVID-19 has led to the dependence of current disease control policies on active immunization.
HCWs were proposed to be given priority for vaccination by the Advisory Committee on Immunization Practices (ACIP) in December, 2020.6 The rationales behind it are the followings. Firstly, health care workers (HCWs) have easier access to COVID-19 patients population in their daily diagnosis and treatment activities, and are at much greater risk of developing COVID-19 than other groups. In the United Kingdom and the United States, the COVID-19 test results showed that front-line HCWs have a 11-fold increased positive rates as compared to the general community.7 Secondly, a previous study assessing the risk of infection transmission from physicians to patients through the hands, equipment and enclosing surfaces showed that physicians played an important role in spreading of nosocomial infections.8 Therefore, the prevention and control of the infection among HCWs have protective effect both on patients and medical staff. Thirdly, results from a recent cross-sectional study have revealed that in addition to gender, marital status, perceived risk, history of prior influenza vaccination, the number of confirmed and suspected cases in local areas, vaccine efficacy, vaccination convenience and vaccine price, the recommendation from doctors is an independent predictor for the general population to receive COVID-19 vaccine.9 Likewise, these results were verified in another cross-sectional study in Italy. The results of this survey demonstrated that recommendation from pediatricians to vaccinate their children is a significant factor in promoting the parental support for vaccine.10 Last but not least, it is encouraging that COVID-19 vaccine have proven 95% efficacy in the prevention of COVID-19 infection in a multinational, large sample size randomized controlled trial.11
Accordingly, the principal objective of this meta-analysis was to investigate the intention to vaccinate against COVID-19 and its influencing factors among HCWs and provide the rationale for the promotion of COVID-19 vaccine.
Method
We prospectively registered key features on International Prospective Register of Systematic Reviews (PROSPERO) with unique identifying number (CRD42021237987) and performed this meta-analysis in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.12
Search strategy
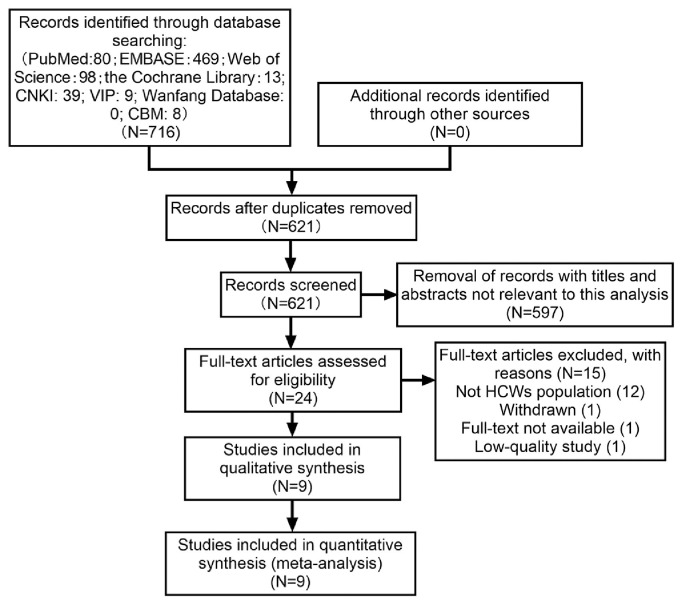
Four English databases (PubMed, EMBASE, Web of Science and the Cochrane Library) and 4 Chinese databases (Chinese National Knowledge Infrastructure (CNKI), the Chongqing VIP Chinese Science (VIP), Wanfang Database and China Biomedical Literature Database (CBM)) were comprehensively retrieved for relevant literature published from their date of inception to February 19, 2021. The following Medical Subject Heading (MeSH) terms and MeSH-derived topical terms were utilized as key phrases in various combinations: “COVID-19,” “SARS-CoV-2,” “2019-nCoV,” “vaccination,” “immunization,” “medical staff,” “medical staff, hospital,” “health personnel,” “physicians” and “nurses.” We did not use any explicit language restriction, although we used only English and Chinese search terms in this meta-analysis. Manual search of reference lists were conducted to find potential relevant articles. Two investigators independently performed the literature screening and the detailed steps of selection process is presented in Figure 1 . Any divergences in screening results were resolved by discussion between reviewers and, if necessary, consulting a senior reviewer to reach a consensus. The software Endnote (version X9.1) was used for reference management.
Fig 1.
Flow chart depicting literature screening process.
Inclusion and exclusion criteria
Inclusion criteria were as follows: (1) published cross-sectional studies on acceptance of COVID-19 vaccination among HCWs employed in inpatient or outpatient medical settings or long-term care centers; (2) the outcome measures of interest were vaccination acceptance and its influencing factors. We defined vaccination acceptance as the percentage of HCWs who are willing to undergo vaccination once it is available, which was assessed through self-report; (3) provided raw data or odds ratios (ORs) for the outcome measures of interest, with confidence intervals; (4) cross-sectional designs.
Exclusion criteria were as follows: (1) not relevant articles; (2) reviews, commentaries, editorials, letters, case reports, protocols, conference abstracts and animal experiments; (3) duplicated articles; (4) full text not available; (5) low-quality studies.
Quality assessment and data extraction
The methodological quality of the literature was evaluated with reference to the following 6 items from the Downs and Black assessment checklist reported in literature13 , 14: (1) clearly stated aim; (2) clearly defined study population; (3) study sample representative of the source population; (4) attempt made to adjust for confounding; (5) attempt made to validate survey responses to institutional records where possible; and (6) discussion of study limitations. One point for items rated as yes, and zero for items rated as no or unable to determine. We classified a total score of 5-6 as high-quality studies, 3-4 as moderate-quality studies and 1-2 as low-quality studies, respectively. After independently assessing the quality of the documents, 2 reviewers carried out a quality discussion on each of the included studies on the basis of the above evaluation criteria and reached an agreement to form a ultimate literature quality evaluation.
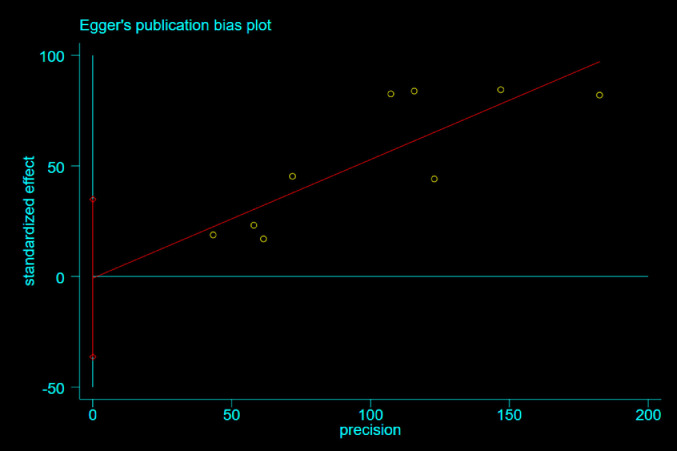
Statistical analysis
The data analysis and statistical software STATA version 15.1 (StataCorp, College Station, TX) was applied to perform meta-analytical calculations. Egger's test with a level of significance set at P<0.05 were further applied to examine possible publication bias.
Results
Screening process
Electronic search and additional evaluation of reference lists yielded a total of 716 potentially relevant articles, which were reduced to 621 after omitting duplicates. There were only 24 remaining papers found to be relevant after a preliminary screening of titles and abstracts, and full-text review were further conducted for confirmation of each study's eligibility. In the full-text investigation phrase, twelve records were removed as subjects did not meet the inclusion criteria. One record was removed as full-text not available. One was removed as withdrawn. In the quality assessment phrase, one was removed as low quality.15 Eventually, nine studies16, 17, 18, 19, 20, 21, 22, 23, 24 with an aggregate sample size of 24,952 individuals published from 2020 to 2021 conformed to our inclusion criteria, of which eight in English16, 17, 18, 19, 20, 21, 22, 23 and one in Chinese.24
Study characteristics
All of the literatures involved in this meta-analysis were cross-sectional designs. Of nine papers included, 3 were from Europe,16 , 18 , 22 3 were from Asia17 , 23 , 24 and 3 were from America.19, 20, 21 All studies were published between 2020 and 2021. The sample size ranged from 461 to 8243 subjects interviewed. The proportion of HCWs who were willing to undergo vaccination reported in the selected literature varied from 28% to 77% (median 0.45, mean 0.51). As for the evaluation of vaccine hesitancy, all study instruments were administered by a questionnaire of various types (on-line, e-mail, telephone, text message, personal interview and paper-based). Six of the included studies utilized self-designed questionnaires,18 , 20, 21, 22, 23, 24 and the other 3 adopted questionnaires previously reported in the literature.16 , 17 , 19 The characteristics of included studies are listed in Table 1 . The average quality score was 3.7 points, with a maximum score of 5 points and a minimum score of 3 points. One study were judged to be of high-quality21 and eight of moderate quality.16, 17, 18, 19, 20 , 22, 23, 24 The detailed quality appraisal results for each study are provided in Table 2 .
Table 1.
Characteristics of included studies
| Study and year published | Country | Study period | Population studied | Total N | Intended to accept N (%) | Administration channel | Evaluation Tool | Type of questions | Response rate % |
|---|---|---|---|---|---|---|---|---|---|
| Gagneux-Brunon 2021 | France | March to July 2020 | HCWs at university hospital and center for COVID-19 diagnosis | 2047 | 1574 (76.9) | On-line and paper-based | Questionnaire developed by Dominique et al25 | Closed | - |
| Kwok 2021 | China | March to April 2020 | Nurses | 1205 | 759 (63.0) | On-line | Questionnaire developed by Betsch et al26 | Likert-type scale | - |
| Papagiannis 2020 | Greece | February 2020 | HCWs in 5 public hospitals | 461 | 200 (43.4) | Personal interviews | Self-designed questionnaire | Likert-type scale | 92.2% |
| Shaw 2021 | US | November to December 2020 | HCWs at an academic medical center | 5277 | 3032 (57.5) | Questionnaire developed by Opel et al27 | Closed | 55% | |
| Shekhar 2021 | US | October to November 2020 | HCWs at 5 major hospital systems | 3479 | 1247 (35.8) | On-line | Self-designed questionnaire | Closed | - |
| Unroe 2021 | US | November 2020 | Nursing home staff | 8243 | 3704 (44.9) | Text message | Self-designed questionnaire | Closed | 33% |
| Verger 2021 | France, Belgium, Canada | October to November 2020 | General practitioners and nurses | 2678 | 1939 (72.4) | On-line and telephone | Self-designed questionnaire | Likert-type scale | - |
| Wang 2020 | China | February to March 2020 | Nurses | 806 | 322 (40.0) | Self-designed questionnaire | Closed | 5.2% | |
| Zhang 2021 | China | September to October 2020 | Hospital staff and CDC's staff | 756 | 209 (27.6) | On-line | Self-designed questionnaire and net promoter score | Likert-type scale | - |
CDC, centers for disease control and prevention; HCW, health care worker; US, United States; -, missing data.
Table 2.
Characteristics of included studies
| Study and year published | Clearly stated aim | Clearly defined study population | Study sample representative of the source population | Attempt made to adjust for confounding | Attempt made to validate survey responses to institutional records where possible | Discussion of study limitations | Quality grading |
|---|---|---|---|---|---|---|---|
| Gagneux-Brunon 2021 | Yes | Yes | Unable to determine | Unable to determine | No | Yes | 3 |
| Kwok 2021 | Yes | Yes | Yes | Unable to determine | No | Yes | 4 |
| Papagiannis 2020 | Yes | Yes | Unable to determine | Unable to determine | No | Yes | 3 |
| Shaw 2021 | Yes | Yes | Yes | Unable to determine | No | Yes | 4 |
| Shekhar 2021 | Yes | Yes | Unable to determine | Unable to determine | No | Yes | 3 |
| Unroe 2021 | Yes | Yes | Yes | Yes | No | Yes | 5 |
| Verger 2021 | Yes | Yes | Yes | Unable to determine | No | Yes | 4 |
| Wang 2020 | Yes | Yes | Yes | Unable to determine | No | Yes | 4 |
| Zhang 2021 | YesUS, | Yes | Unable to determine | Unable to determine | No | Yes | 3 |
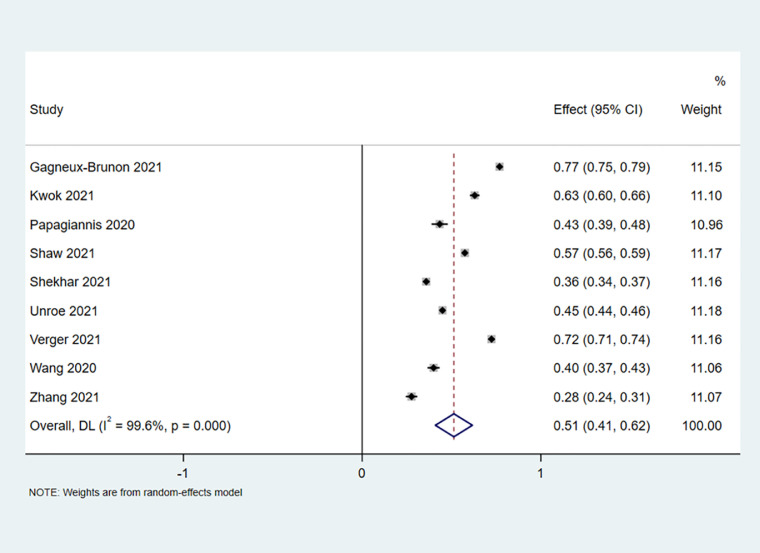
Meta-analysis of vaccination acceptance
Nine accounts16, 17, 18, 19, 20, 21, 22, 23, 24 reported the acceptance of COVID-19 vaccine in a total of 24,952 HCWs. Since the Cochrane Q test for heterogeneity demonstrated high heterogeneity among the included studies (I2 = 99.6%, Cochrane Q test P = .000), random-effect model was applied. As is shown in Fig 2 , the pooled effect value of vaccination willingness was 51%, with a 95% CI of 0.41-0.62. No significant publication bias was noted on Egger's test (t = -0.05, Egger's test P = .961, Fig 3 ).
Fig 2.
Forest plot depicting COVID-19 vaccine acceptance among health care workers (HCWs).
Fig 3.
Egger regression plot of COVID-19 vaccine acceptance among HCWs.
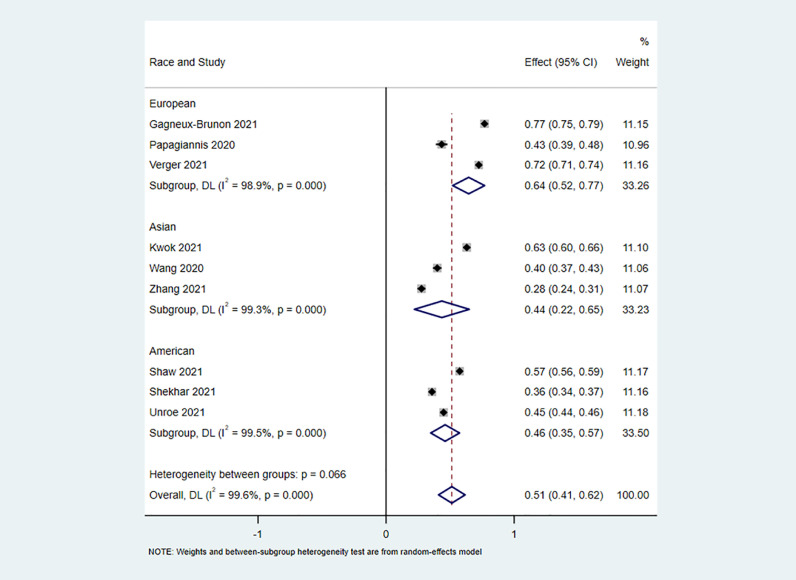
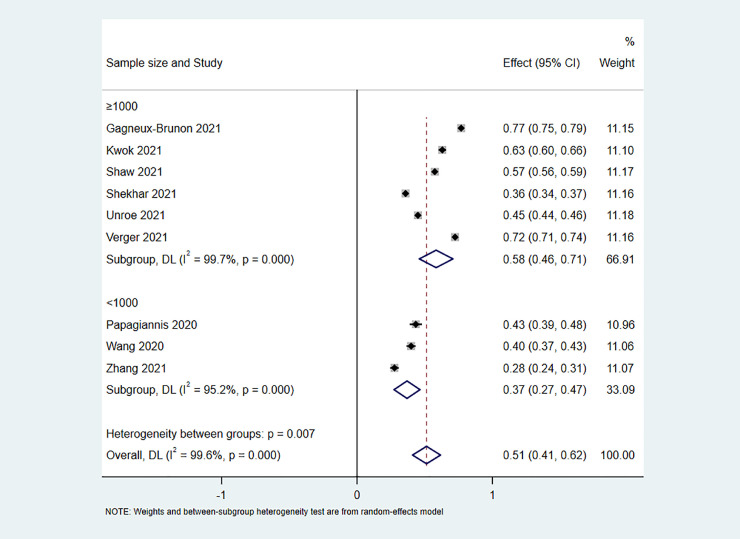
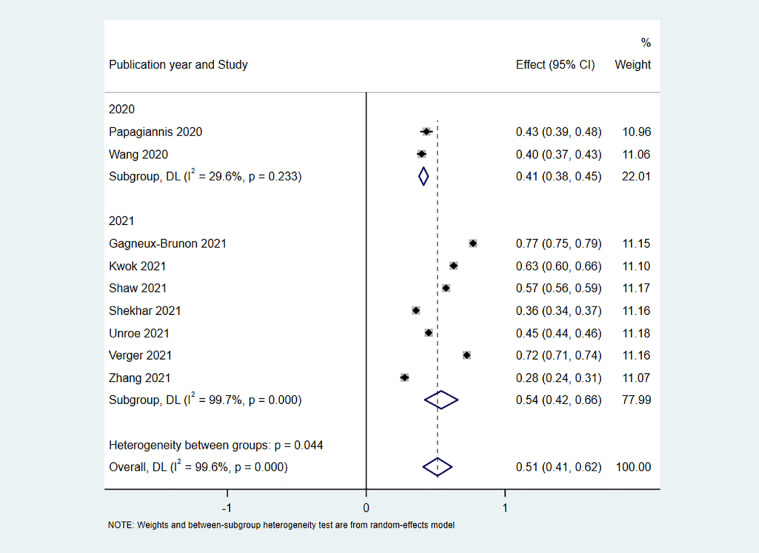
Subgroup analysis of vaccination acceptance
Due to severe heterogeneity observed among selected studies, additional subgroup analyses for the meta-analysis was implemented to clarify the source of heterogeneity. Nevertheless, no apparent difference between overall heterogeneity and subgroup heterogeneity occurred in subgroup analyses, indicating that the heterogeneity was not correlated with race, sample size and publication year (Fig 4 , Fig 5 , Fig 6 ).
Fig 4.
Forest plot depicting COVID-19 vaccine acceptance among HCWs after subgroup analysis according to race.
Fig 5.
Forest plot depicting COVID-19 vaccine acceptance among HCWs after subgroup analysis according to sample size.
Fig 6.
Forest plot depicting COVID-19 vaccine acceptance among HCWs after subgroup analysis according to publication year.
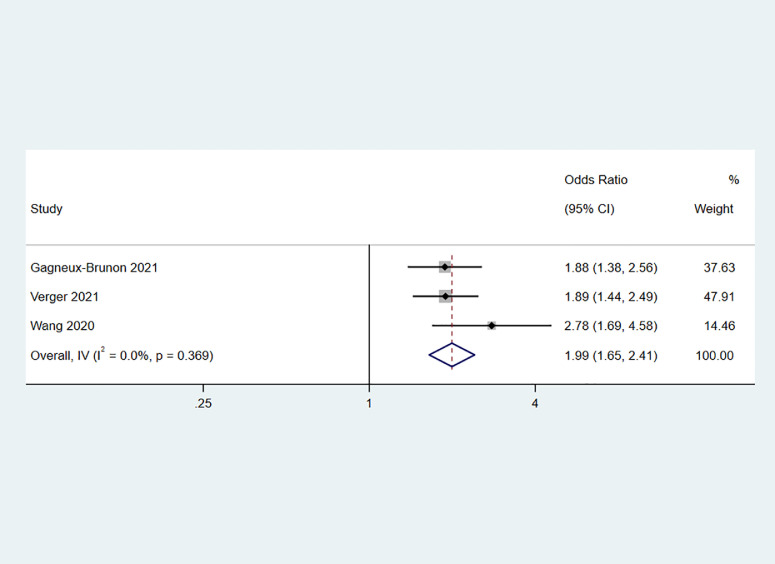
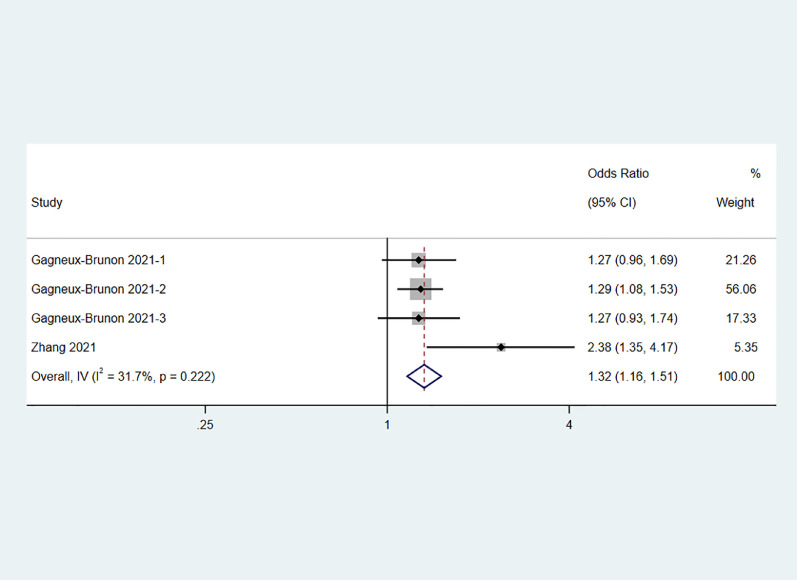
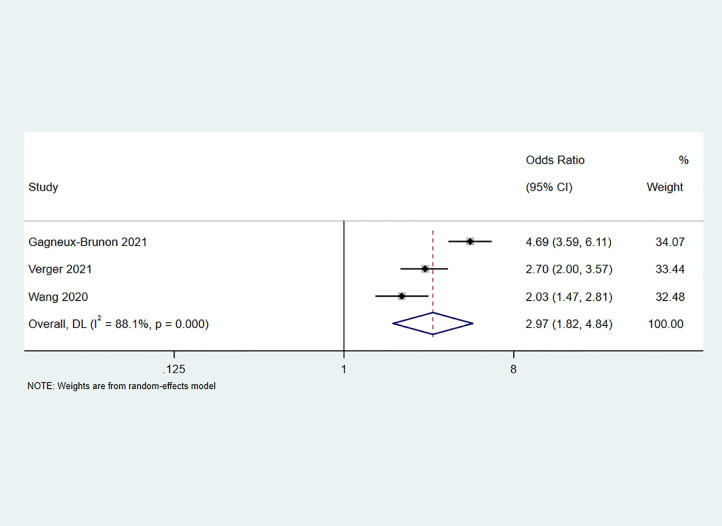
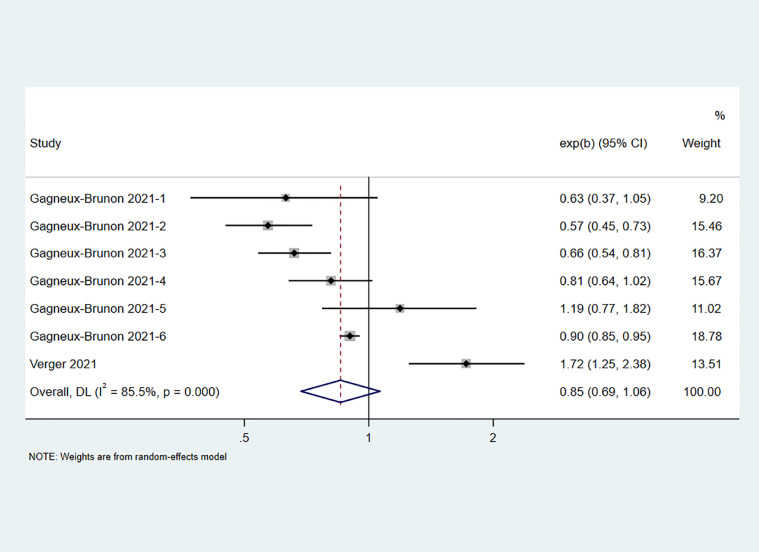
Meta-analysis of factors associated with COVID-19 vaccine acceptance
Meta-analysis was carried out for the 4 potentially determinants involved in the selected studies. As there were statistically significant heterogeneities present for occupation and history of prior influenza vaccination, a random-effects model was adopted for the meta-analysis (I2 = 85.5%, Cochrane Q test P = .000; I2 = 88.1%, Cochrane Q test P = .000). In contrast, a fixed-effects model was adopted given no obvious heterogeneity for gender and age (I2 = 0.0%, Cochrane Q test P = .369; I2 = 31.7%, Cochrane Q test P = .222). The meta-analysis results showed that male, aged 30 years or older, having a history of prior influenza vaccination were facilitating factors affecting the HCWs’ intention of COVID-19 vaccination (OR 1.99, 95% confidence interval (CI) 1.65-2.41, P = .000, Fig 7 ; OR 1.32, 95% CI 1.16-1.51, P = .000, Fig 8 ; OR 2.97, 95% CI 1.82-4.84, P = .000, Fig 9 ). Whereas, the relationship between occupation and the willingness of COVID-19 vaccination cannot be determined (OR 0.85, 95% CI 0.69-1.06, P = .160, Fig 10 ). Also, there were too few studies reported outcomes of interest to permit sensitivity analysis and Egger's test.
Fig 7.
Forest plot depicting the relationship between gender and COVID-19 vaccine acceptance among HCWs.
Fig 8.
Forest plot depicting the relationship between age and COVID-19 vaccine acceptance among HCWs.
Fig 9.
Forest plot depicting the relationship between history of prior influenza vaccination and COVID-19 vaccine acceptance among HCWs.
Fig 10.
Forest plot depicting the relationship between occupation and COVID-19 vaccine acceptance among HCWs.
Discussion
We found in the present study that the overall acceptance of COVID-19 vaccine in HCWs population was 51%, which was somewhat lower than that of the general population reported by Robinson et al.28 One possible contributor for this finding is that HCWs are exposed to more professional information, and therefore has more concerns about the effectiveness and safety of COVID-19 vaccine, which may affect their decision to get vaccinated and hinder their recommendation of vaccination to patients.
The results of this meta-analysis found that COVID-19 vaccination acceptance among HCWs were influenced by the following factors. Firstly, we found that vaccination intention did vary with gender. Male participants were more likely to receive the COVID-19 vaccine compared to females when it was available. This result is in agreement with those of several other studies.29, 30, 31 Possible explanations for this phenomenon could be because of the high morality rates in males than females.32 Secondly, age-based differences in vaccination intention especially merit attention, with more participants aged 30 years or older than those under 30 years being vaccinated. Some of reasons can possibly relate to the relatively high prevalence and morality rates of COVID-19 in the elderly people.32 Thirdly, as foreseen, the results revealed that those with a history of prior influenza vaccination also had significantly greater intention to get vaccinated against COVID-19. This may be attributed to the fact that those who have received influenza vaccination tend to pay more attention to the prevention of respiratory diseases and have more knowledge regarding vaccines. Fourthly, Clinicians seem to be less likely to take the COVID-19 vaccine but no significant relationship was found between occupation and intention to take the COVID-19 vaccine. Taken together, targeted strategies of COVID-19 vaccination need to be formulated and implemented for female health care workers under the age of 30 years who have no history of influenza vaccination in order to address the issue of vaccine hesitancy among HCWs.
Given the moderate level of intention to COVID-19 vaccination among HCWs, there is a need to increase vaccine acceptance in this population. Currently, most countries recommend that HCWs be vaccinated against COVID-19. Italy has become the first country in Europe to introduce a mandatory vaccination policy for HCWs, requiring those who refuse to be vaccinated to transfer to jobs without the risk of spreading the virus or suspend their work without pay for more than a year, after suffering from the most severe effects of COVID-19 among European countries. A recent report revealed that only about one in 10,000 health workers refused to be vaccinated in Italy.33 Serbia are considering doing the same.34 Moreover, a previous meta-analysis showed that the majority of HCWs could accept a mandatory vaccination policy, suggesting that it could be accepted if necessary.35 Furthermore, free vaccination policy may also contribute to increase vaccination rates and the result has been validated by a study conducted in China.36
The strength of the present study lies in its rapid analysis about willingness and its influencing factors of COVID-19 vaccination among HCWs to provide useful insight for the implementation of COVID-19 vaccination in the future. In the meantime, we must acknowledge that our study was subject to certain limitations that warrant mention. Firstly, owing to the limited data available, this meta-analysis assessed vaccination intention rather than actual vaccination. Even though intention was believed to be the most immediate antecedent of subsequent behaviour,37 previous investigation suggested that intention did not necessarily translate into behaviour.38 As a result, measuring vaccine completion appears more important especially for COVID-19 vaccine that need several doses.39 Further researches are required to examine vaccine uptake and completion. Secondly, although we scanned systematically for published peer-reviewed journal articles in this meta-analysis, whereas possibly valuable unpublished data, gray literature and non-peer-reviewed papers was excluded to ensure quality, which may inevitably cause some publication bias. However, Egger's test suggested that there was no evidence for publication bias. Thirdly, apparent heterogeneity was detected in this meta-analysis. Apart from using the random-effect model, we tried to perform subgroup analyses by race, sample size and publication year in order to compensate for this deficiency to some extent, however, the source of heterogeneity was not found through subgroup analyses based on the above confounding factors. Therefore, a broader range of potential confounders should be considered in the future analyses which incorporate more original studies. Besides, a measurement bias exists due to different resources for assessing vaccine hesitancy among studies. Consequently, we recommend that further studies employ well-validated and uniform questionnaires to enhance inter-study comparability.40 Last but not least, population studied were primarily in economically developed areas, which reduce the generalizability of the study results.
Conclusion
In conclusion, COVID-19 vaccination acceptance of HCWs was at moderate level. In the case of newly-available COVID-19 vaccine, little is known regarding its efficacy and safety at this moment for most individuals. Thus, global governments should expand and intensify their health education efforts urgently to improve knowledge, attitude and practice regarding COVID-19 vaccination that are beneficial to promotion of COVID-19 vaccination.
Footnotes
Funding/support: This work was supported by the Construction of Key Projects by Zhejiang Provincial Ministry (No. WKJ-ZJ-1915, WKJ-ZJ-2017), the Zhejiang Province Chinese Medicine Modernization Program (No. 2020ZX001), the General Project of Zhejiang Education Department (No. Y201942823) and Clinical and Experimental Research of YSHS Granule.
Conflicts of interest: None to report.
Author contributions: Chuxuan Luo designed the study. Data was extracted by Chuxuan Luo and Yuan Yang. Chuxuan Luo analysed the data. The first draft of the manuscript was wrote by Chuxuan Luo, and all authors have read, revised and approved the final version of the manuscript.
References
- 1.Wiersinga WJ, Rhodes A, Cheng AC, et al. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review. JAMA. 2020;324:782–793. doi: 10.1001/jama.2020.12839. [DOI] [PubMed] [Google Scholar]
- 2.Adhikari SP, Meng S, Wu YJ, et al. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infect Dis Poverty. 2020;9:29. doi: 10.1186/s40249-020-00646-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shrivastava SR, Shrivastava PS. 2019-nCoV outbreak declared as public health emergency of international concern: what next? Int J Prev Med. 2020;11:65. doi: 10.4103/ijpvm.IJPVM_63_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91:157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. Novel Coronavirus (COVID-19) Situation. Available at: https://covid19.who.int/. Accessed April 6, 2021.
- 6.Dooling K, Marin M, Wallace M, et al. The Advisory Committee on Immunization Practices' Updated Interim Recommendation for Allocation of COVID-19 Vaccine - United States, December 2020. MMWR Morb Mortal Wkly Rep. 2021;69:1657–1660. doi: 10.15585/mmwr.mm695152e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nguyen LH, Drew DA, Graham MS, et al. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health. 2020;5:e475–e483. doi: 10.1016/S2468-2667(20)30164-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Paduszynska K, Rucinska LG, Pomorski L. Physician as an infective vector at a department of surgery. Pol Przegl Chir. 2015;86:511–517. doi: 10.2478/pjs-2014-0091. [DOI] [PubMed] [Google Scholar]
- 9.Wang J, Jing R, Lai X, et al. Acceptance of COVID-19 Vaccination during the COVID-19 Pandemic in China. Vaccines (Basel) 2020;8:482. doi: 10.3390/vaccines8030482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Giambi C, Fabiani M, D'Ancona F, et al. Parental vaccine hesitancy in Italy - results from a national survey. Vaccine. 2018;36:779–787. doi: 10.1016/j.vaccine.2017.12.074. [DOI] [PubMed] [Google Scholar]
- 11.Polack FP, Thomas SJ, Kitchin N, et al. Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. N Engl J Med. 2020;383:2603–2615. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 13.Vasilevska M, Ku J, Fisman DN. Factors associated with healthcare worker acceptance of vaccination: a systematic review and meta-analysis. Infect Control Hosp Epidemiol. 2014;35:699–708. doi: 10.1086/676427. [DOI] [PubMed] [Google Scholar]
- 14.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377–384. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kabamba NM, Kabamba Ngombe L, Ngoie Mwamba G, et al. Acceptability of vaccination against COVID-19 among healthcare workers in the democratic republic of the congo. Pragmat Obs Res. 2020;11:103–109. doi: 10.2147/POR.S271096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gagneux-Brunon A, Detoc M, Bruel S, et al. Intention to get vaccinations against COVID-19 in French healthcare workers during the first pandemic wave: a cross-sectional survey. J Hosp Infect. 2021;108:168–173. doi: 10.1016/j.jhin.2020.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kwok KO, Li KK, Wei WI, et al. Editor's Choice: Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: A survey. Int J Nurs Stud. 2021;114 doi: 10.1016/j.ijnurstu.2020.103854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Papagiannis D, Malli F, Raptis DG, et al. Assessment of knowledge, attitudes, and practices towards new Coronavirus (SARS-CoV-2) of health care professionals in Greece before the outbreak period. Int J Environ Res Public Health. 2020;17:4925. doi: 10.3390/ijerph17144925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shaw J, Stewart T, Anderson KB, et al. Assessment of U.S. health care personnel (HCP) attitudes towards COVID-19 vaccination in a large university health care system [e-pub ahead of print] Clin Infect Dis. 2021 doi: 10.1093/cid/ciab054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shekhar R, Sheikh AB, Upadhyay S, et al. COVID-19 vaccine acceptance among health care workers in the United States. Vaccines (Basel) 2021;9:119. doi: 10.3390/vaccines9020119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Unroe KT, Evans R, Weaver L, et al. Willingness of long-term care staff to receive a COVID-19 vaccine: a single state survey. J Am Geriatr Soc. 2021;69:593–599. doi: 10.1111/jgs.17022. [DOI] [PubMed] [Google Scholar]
- 22.Verger P, Scronias D, Dauby N, et al. Attitudes of healthcare workers towards COVID-19 vaccination: a survey in France and French-speaking parts of Belgium and Canada, 2020. Euro Surveill. 2021;26:2002047. doi: 10.2807/1560-7917.ES.2021.26.3.2002047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang K, Wong ELY, Ho KF, et al. Intention of nurses to accept coronavirus disease 2019 vaccination and change of intention to accept seasonal influenza vaccination during the coronavirus disease 2019 pandemic: a cross-sectional survey. Vaccine. 2020;38:7049–7056. doi: 10.1016/j.vaccine.2020.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang H, Ding L, Pan X, et al. Willingness to receive novel coronavirus vaccine and factors influencing willingness among healthcare workers in Zhejiang province. Chinese J Vaccines Immuni. 2021:1–7. [Google Scholar]
- 25.Rey D, Fressard L, Cortaredona S, et al. Vaccine hesitancy in the French population in 2016, and its association with vaccine uptake and perceived vaccine risk-benefit balance. Euro Surveill. 2018;23:17–00816. doi: 10.2807/1560-7917.ES.2018.23.17.17-00816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Betsch C, Schmid P, Heinemeier D, et al. Beyond confidence: development of a measure assessing the 5C psychological antecedents of vaccination. PLoS One. 2018;13 doi: 10.1371/journal.pone.0208601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Opel DJ, Taylor JA, Mangione-Smith R, et al. Validity and reliability of a survey to identify vaccine-hesitant parents. Vaccine. 2011;29:6598–6605. doi: 10.1016/j.vaccine.2011.06.115. [DOI] [PubMed] [Google Scholar]
- 28.Robinson E, Jones A, Lesser I, et al. International estimates of intended uptake and refusal of COVID-19 vaccines: a rapid systematic review and meta-analysis of large nationally representative samples. Vaccine. 2021;39:2024–2034. doi: 10.1016/j.vaccine.2021.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Detoc M, Bruel S, Frappe P, et al. Intention to participate in a COVID-19 vaccine clinical trial and to get vaccinated against COVID-19 in France during the pandemic. Vaccine. 2020;38:7002–7006. doi: 10.1016/j.vaccine.2020.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alqudeimat Y, Alenezi D, AlHajri B, et al. Acceptance of a COVID-19 vaccine and its related determinants among the general adult population in Kuwait. Med Princ Pract. 2021;30:262–271. doi: 10.1159/000514636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rodriguez-Blanco N, Montero-Navarro S, Botella-Rico JM, et al. Willingness to be vaccinated against covid-19 in spain before the start of vaccination: a cross-sectional study. Int J Environ Res Public Health. 2021;18:5272. doi: 10.3390/ijerph18105272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41:145–151. doi: 10.3760/cma.j.issn.0254-6450.2020.02.003. [DOI] [PubMed] [Google Scholar]
- 33.Paterlini M. Covid-19: Italy makes vaccination mandatory for healthcare workers. BMJ. 2021;373:n905. doi: 10.1136/bmj.n905. [DOI] [PubMed] [Google Scholar]
- 34.Serbia Considers Mandatory Vaccination of Health Workers. London: Reuters; 2021. Available at:https://www.reuters.com/business/healthcare-pharmaceuticals/serbia-considers-mandatory-vaccination-health-workers-2021-04-09/. Accessed April 9, 2021.
- 35.Gualano MR, Corradi A, Voglino G, et al. Healthcare Workers' (HCWs) attitudes towards mandatory influenza vaccination: a, systematic review and meta-analysis. Vaccine. 2021;39:901–914. doi: 10.1016/j.vaccine.2020.12.061. [DOI] [PubMed] [Google Scholar]
- 36.Liu R, Zhang Y, Nicholas S, et al. COVID-19 vaccination willingness among Chinese adults under the free vaccination policy. Vaccines (Basel) 2021;9:292. doi: 10.3390/vaccines9030292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Albarracin D, Johnson BT, Fishbein M, et al. Theories of reasoned action and planned behavior as models of condom use: a meta-analysis. Psychol Bull. 2001;127:142–161. doi: 10.1037/0033-2909.127.1.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lavine H, Thomsen Cynthia J, Zanna Mark P, et al. On the primacy of affect in the determination of attitudes and behavior: the moderating role of affective-cognitive ambivalence. J Experimental Social Psychol. 1998;34:398–421. [Google Scholar]
- 39.Shapiro GK, Joyal-Desmarais K, Perez S, et al. A response to Fu et al.'s "Educational interventions to increase HPV vaccination acceptance". Vaccine. 2014;32:6342–6344. doi: 10.1016/j.vaccine.2014.09.045. [DOI] [PubMed] [Google Scholar]
- 40.Cella P, Voglino G, Barberis I, et al. Resources for assessing parents' vaccine hesitancy: a systematic review of the literature. J Prev Med Hyg. 2020;61:E340–E373. doi: 10.15167/2421-4248/jpmh2020.61.3.1448. [DOI] [PMC free article] [PubMed] [Google Scholar]