Abstract
Morgagni hernia is the rarest type of congenital diaphragmatic hernia, which can present late in adulthood. Here, we report a case of Morgagni hernia in an elderly woman who presented as an acute coronary syndrome with raised troponin level. X-ray of the chest (CXR) showed air–fluid level in the right lower hemithorax with loss of right diaphragmatic outline and subsequently confirmed strangulated Morgagni hernia with CT. She was treated with emergency laparotomy to reduce the hernia content and surgical repair with mesh done. In conclusion, Troponin can be falsely positive in Morgagni hernia patients, possibly due to strain on the heart by herniated bowel contents. Basic imaging such as a (CXR) is useful in the case of chest pain to rule out the non-cardiac causes. Although ‘time is the myocardium’ in the setting of all cases of chest pain with raised troponin, CXR should be done before treatment that poses bleeding risk and unnecessary delay in laparotomy.
Keywords: gastrointestinal surgery, radiology, general surgery
Background
Morgagni hernia is the rarest of four types of congenital diaphragmatic hernia, where the bowel contents herniate into the thoracic cavity. It was first described by the Italian anatomist and pathologist Giovanni Battista Morgagni in 1769.1 It represents 2% of all diaphragmatic hernias.2 It is due to a congenital defect in the retrosternal trigone due to the absence of muscle fibres in the diaphragm and the lack of fusion of the anterior pleuroperitoneal membrane. Typical symptoms associated with this hernia include shortness of breath, cough, chest tightness, postprandial emesis, recurrent pneumonia, gastro-oesophageal reflux disorder, dysphagia, abdominal cramping, distension and non-specific abdominal pain. Congenital diaphragmatic hernia in adults may be incidental, symptomatic or acute surgical emergency presentation. Late diagnosis of this condition is very rare and there are only few cases of symptomatic hernia in adult reported so far in the literature. Here, we report a 60-year-old woman who presented with chest pain with false-positive troponin due to strangulated Morgagni hernia.
Case presentation
A 60-year-old woman presented to the emergency department with 1-day history of severe chest pain. The pain started gradually and radiated to both shoulders, abdomen and pelvis. The pain was initially squeezing in nature, and not relieved by non-steroidal anti-inflammatory drug. She does not have any medical history. She has a strong family history of ischaemic heart disease of which her father died at the age of 50. She is a non-smoker and denied any illicit drug use. She drinks a glass of alcohol every night. On examination, her blood pressure was 165/80 mm Hg, heart rate of 75 beats per minutes, respiratory rate of 16 breaths per minutes, temperature of 36.5⁰C and pulse oximeter showed 94% oxygen saturation. There was reduced air entry at the right base area of the lung. She was well perfused with a good volume pulse. Abdominal examination showed no sign of peritonism. The abdomen was soft but tender in the epigastric region and right upper quadrant. Murphy’s sign was positive and normal bowel sounds were present.
Investigations
Blood investigation showed haemoglobin of 153 (normal range: 115–160 g/L), white cell count of 9 (normal range: 4–11×109/L), platelet count of 354 (normal range: 150–400×109/L), C reactive protein of 1 (normal range <1 mg/L), amylase 30 (normal range: 30–110 U/L), troponin of 110 (normal range <14 ng/L), normal kidney and liver function test. Resting ECG showed sinus rhythm with incomplete right bundle branch block (figure 1). Radiograph of the chest (CXR) showed evidence of air–fluid level in the right lower hemithorax with loss of right diaphragmatic outline (figure 2). It has proceeded with contrast-enhanced CT of the thorax, abdomen and pelvis, which showed right anterior diaphragmatic defect (Morgagni hernia) with the evidence of dilated small bowel loops, mesenteric fat pad and part of the hepatic dome seen in right hemithorax (figure 3). The herniated bowel loops were seen indenting the right aspect of the heart and causing a mediastinal shift to the left side. Also, subsequent appreciable dilatation of the stomach was noted. There was evidence of marked right pleural effusion, subsequent small basal right-sided lung consolidation and collapse as well.
Figure 1.
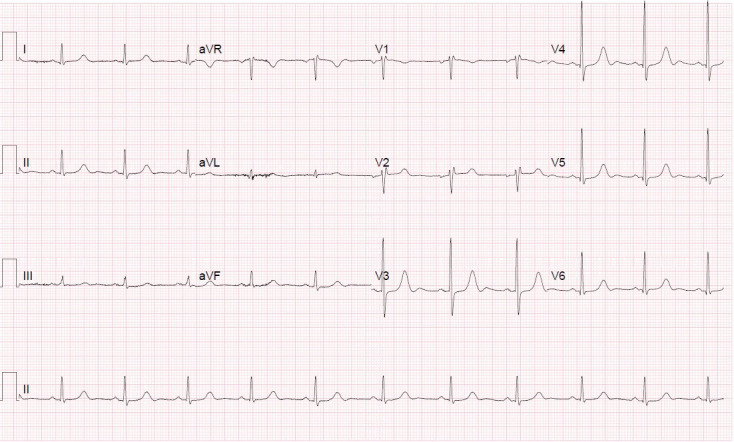
Resting ECG showed sinus rhythm with incomplete right bundle branch block.
Figure 2.
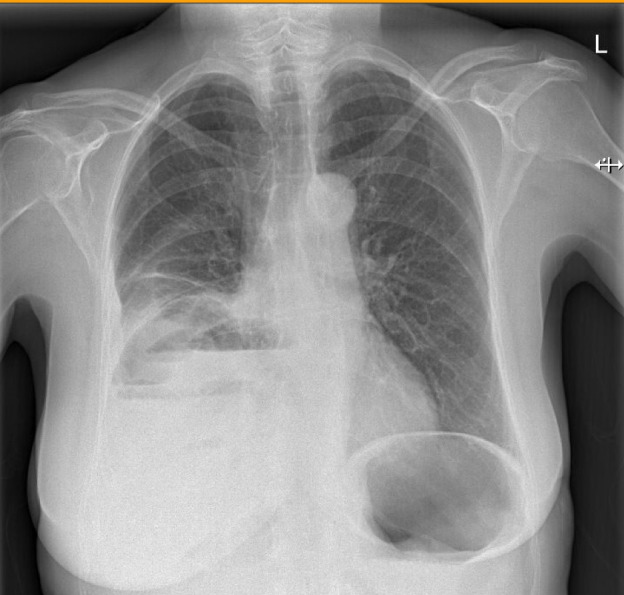
Radiograph of the chest showed evidence of air–fluid level in right lower hemithorax with loss of right diaphragmatic outline.
Figure 3.
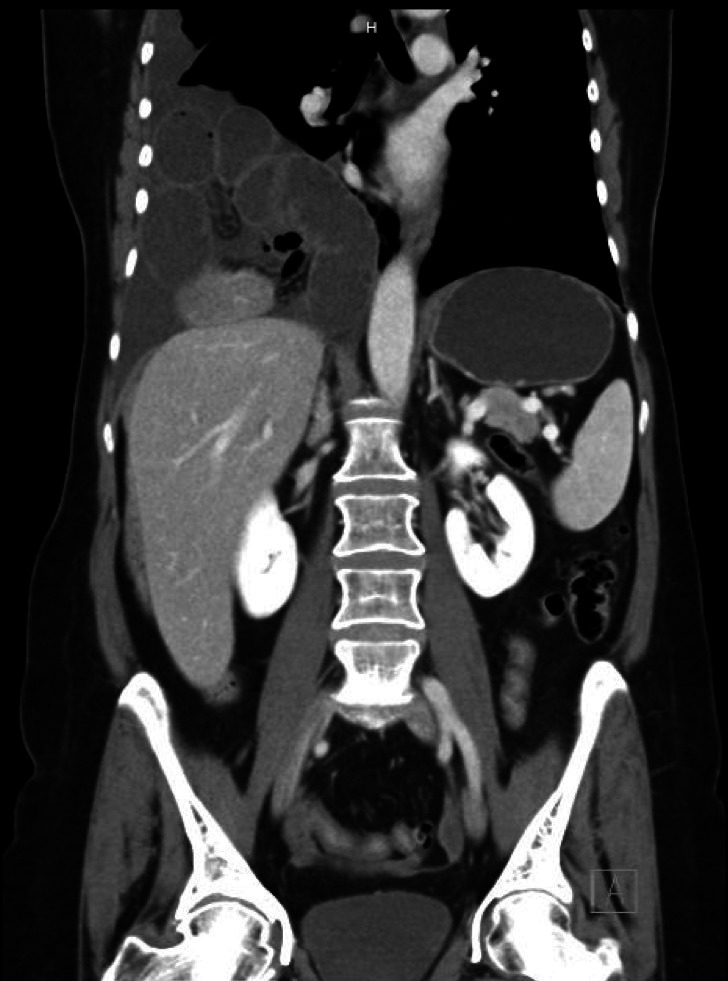
Contrast-Enhanced CT of the thorax, abdomen and pelvis in coronal view showed right anterior diaphragmatic defect (Morgagni hernia) with the evidence of dilated small bowel loops, mesenteric fat pad and part of the hepatic dome seen in right hemithorax. Also, subsequent appreciable dilatation of the stomach was noted.
Differential diagnoses
Initially, it was thought to be acute coronary syndrome due to chest pain in the context of advanced age, strong family history, abnormal ECG and marked raised troponin. Cardiology consultation was performed and it was felt that raised troponin was believed to be leaked from the strained heart from bowel contents in the chest. Further urgent surgical consultation was performed with the possible differential diagnoses of obstructed/strangulated/perforated diaphragmatic hernia, cholecystitis, gastritis or aortic aneurysm. Finally, contrasted-enhanced tomography of the thorax, abdomen and pelvis was requested while the initial acute coronary syndrome treatment plan was withheld.
Treatment
The patient underwent emergency laparotomy with the release of incarcerated small bowel through the diaphragmatic hernia of Morgagni with mesh repair. An upper midline laparotomy was performed. Congested dusky loops of small bowel incarcerated into large right hemithorax with bruised congested mesentery and haemorrhagic fluid were present in the hernia cavity. Bowel were viable and non-gangrenous. Unfortunately, the photos were not taken during the emergency operation.
Outcome and follow-up
Her chest pain was completely resolved after the operation. The patient was treated with intravenous antibiotics, analgesia and fluids for 48 hours. She recovered completely and discharged after 5 days from the hospital.
Discussion
Causes of diaphragmatic hernia can be traumatic or congenital, in which the former is way more common. Congenital diaphragmatic hernia commonly presents in the neonatal period, as one of the surgical cause of neonatal respiratory distress, in which Bochdalek constitutes 90% of the cases. Being the rarest among this rare pathology, Morgagni hernia often presents late in adulthood as in our case, in contrast to its counterpart Bochdalek hernia. The reason for this late presentation despite being a congenital condition is believed to be due to the weak point for Morgagni hernia, namely sternocostal or Larrey triangle which is so small, and occurs more commonly when the muscle becomes weaker in corresponding to ageing.3 Being more common in female, Morgagni hernia commonly presents with two systemic symptoms, either gastrointestinal or respiratory symptoms, but remarkably respiratory symptom especially shortness of breath or dyspnoea is the most common symptom according to Arikan et al’s study.4 Few papers reported Morgagni hernia presenting as recurrent lower respiratory tract infection, and thus proper CXR with delicate interpretation is important for correct diagnosis.5 6 Other than abdominal pain with nausea and vomiting or intestinal obstruction picture, Morgagni hernia is reported to present even with gastric outlet obstruction in a case where stomach is the content and upper gastrointestinal bleeding with unknown pathology.3 7 Few other papers suggested suspecting diaphragmatic hernia in an adult with the presentation of concurrent intestinal obstruction with respiratory distress as well.8 9 As highlighted in our case here, it is worth noting that Morgagni hernia can even masquerade as an acute coronary syndrome by presenting with chest pain, complicating the diagnosis and treatment even more complex, and to the best of our knowledge, we are one of the few cases to report this rare presentation of Morgagni hernia.10
Notably, a CXR is good enough as basic and easily available imaging to investigate for common presentations of chest pain and to suspect for Morgagni hernia when there is elevated hemidiaphragm or loss of diaphragmatic outline with the presence of bowel loops in hemithorax. To date, CT remains the best diagnostic tool for Morgagni hernia as the content of hernia and size of the defect can be visualised and useful for management purpose. Troponin is a highly sensitive and specific cardiac biomarker that indicates myocardial cell injury. Raised troponin level in a patient with chest pain, in the context of advanced age and positive family history as in this case, falsely alarms the possibility of an acute coronary syndrome, which can lead to wrong antiplatelet and anticoagulant management if CXR was not done and correctly interpreted. Due to possible atypical presentation of Morgagni hernia, proper clinical assessment with basic investigations such as CXR and ECG are more superior to specific biomarker investigations such as troponin level, which can be falsely positive in several non-coronary causes of cardiac myocyte necrosis such as sepsis, renal failure, pulmonary embolism, mesenteric ischemia, bowel obstruction and so on. As such, we postulate that compression of cardiac chambers from herniated bowel contents triggered myocardial cell injury, which leads to raised troponin in this case. Being a rare case, there is no proper guideline or consensus on management of Morgagni hernia; however, as a common practice, surgery remains the best treatment for Morgagni hernia, even when it is asymptomatic without any complications due to a high risk of strangulation and obstruction.3 4 11 12 Surgical repair for Morgagni hernia can be either done open, through laparotomy or thoracotomy or endoscopic through laparoscopic or thoracoscopic. The repair can be done with or without mesh as well. There is no proper research on the comparison of the approaches or techniques to date; however, laparoscopic repair with mesh is the common practice nowadays if the patient is haemodynamic stable.
Learning points.
It is a rare surgical case presentation of Morgagni hernia as an acute medical emergency.
This case emphasises the importance and usefulness of clinical examination and plain radiograph of the chest (CXR) for all patients with chest pain in ruling out non-cardiac differential diagnoses.
False-positive troponin can be seen in strangulated diaphragmatic hernia due to strained heart from bowel contents in the thoracic cavity.
Prognosis of Morgagni hernia is good, especially with surgical repair.
There is a high risk of bleeding and unnecessary delay in laparotomy if anti-coagulant treatment was given presuming that chest pain is due to an acute coronary syndrome without or before reviewing CXR.
Footnotes
Contributors: MHO involves in the management of the patient. She wrote the initial draft of the article. JRN and TNM performed the literature search and wrote the final draft of the article and case description. MHO has provided the appropriate guidance to write and publish the article. NPL revised the article.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Obtained.
References
- 1.Bhasin DK, Nagi B, Gupta NM, et al. Chronic intermittent gastric volvulus within the foramen of Morgagni. Am J Gastroenterol 1989;84:1106–8. [PubMed] [Google Scholar]
- 2.Li S, Liu X, Shen Y, et al. Laparoscopic repair of Morgagni hernia by artificial pericardium patch in an adult obese patient. J Thorac Dis 2015;7:754. 10.3978/j.issn.2072-1439.2015.03.15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Griffiths EA, Ellis A, Mohamed A, et al. Surgical treatment of a Morgagni hernia causing intermittent gastric outlet obstruction. BMJ Case Rep 2010;2010:bcr0120102608. 10.1136/bcr.01.2010.2608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arikan S, Dogan MB, Kocakusak A, et al. Morgagni's hernia: analysis of 21 patients with our clinical experience in diagnosis and treatment. Indian J Surg 2018;80:239–44. 10.1007/s12262-016-1580-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Santos S, Oliveira E, Monteiro N, et al. Large Morgagni hernia in an adult patient. Eur J Case Rep Intern Med 2015;3. 10.12890/2015_000322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Supomo S, Darmawan H. A rare adult Morgagni hernia mimicking lobar pneumonia. Turk J Surg 2018:1–3. 10.5152/turkjsurg.2018.3978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patial T, Negi S, Thakur V. Hernia of Morgagni in the elderly: a case report. Cureus 2017;9:e1549. 10.7759/cureus.1549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee SY, Kwon JN, Kim YS, et al. Strangulated Morgagni hernia in an adult: synchronous prolapse of the liver and transverse colon. Ulus Travma Acil Cerrahi Derg 2018;24:376–8. 10.5505/tjtes.2017.99045 [DOI] [PubMed] [Google Scholar]
- 9.Saqib SU, Hamid K, Chawla TU. Congenital Morgagni hernia presenting as complete small bowel obstruction in the adult - A case report. Int J Surg Case Rep 2020;76:390–3. 10.1016/j.ijscr.2020.10.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mohamed M, Al-Hillan A, Shah J, et al. Symptomatic congenital Morgagni hernia presenting as a chest pain: a case report. J Med Case Rep 2020;14:13. 10.1186/s13256-019-2336-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ağalar C, Atila K, Arslan Naciye Çiğdem, et al. Adult Morgagni hernia: a single center experience of 5 cases and review of literature. Turk J Surg 2019;35:321–4. 10.5578/turkjsurg.3929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Elfiky A, Daneshvar D, Krzyzak M, et al. Adult onset Morgagni hernia: medical vs. surgical management. Cureus 2019;11:e4626. 10.7759/cureus.4626 [DOI] [PMC free article] [PubMed] [Google Scholar]


