Abstract
Infertility is on a rise, and so is the availability of assisted reproductive technique (ART) centres. The sole aim of these centers is to help these unfortunate couples achieve pregnancy. Hence, the concentration of the treatment is on the female partner, while the male is relegated to just being a source for sperm. In the era of intracytoplasmic sperm injection, when pregnancy is possible even with a single mature sperm, evaluation and management of male factor infertility (MFI) is often neglected. MFI and poor semen parameters are markers of male health. He could be suffering from erectile or ejaculatory issues or with correctable obstructive azoospermia. A simple timely varicocele correction may help resolve the issue. It is important to understand that MFI is not a disease but may be a symptom of major underlying clinical condition like testicular or brain tumors. Infertility treatment could be the only occasion when a male seeks health-care evaluation. India has a large pool of qualified urologists trained in andrological care. In contrast, gynecologists may not be trained in the management of male patients, hence there is an important place for andrological services to be an integral part of ART centers. Andrologists would offer minimal andrological evaluation and condition-specific treatment. This could avoid or reduce the need for invasive and expensive ART. Andrologists could also choose the most appropriate mode of sperm retrieval. Undoubtedly, availability of andrological services would improve the overall quality of care, reduce the costs and complications, and would also be medicolegally safe.
KEYWORDS: Andrologist, andrology, artificial reproductive techniques, in vitro fertilization, male factor infertility, surgical sperm retrieval
INTRODUCTION
The patriarchal social system puts a heavy price on fertility as the family needs an heir and the man needs to prove his masculinity. Needless to say, childless couples face rampant oppression and humiliation.[1] Although male factor as a cause for infertility is implicated in about one-third to one-half of all infertile couples, male factor infertility (MFI) is underrepresented as a disease. Often MFI is neglected both by the literature and the media.[2] With scant underutilized resources, male partner does not get the same attention in infertility evaluation as the female partner.[3] Further, the MFI evaluation may be performed by gynecologists, who may not have the necessary clinical skills and training.[4] With the advent of assisted reproductive technique (ART) such as intrauterine insemination (IUI), in vitro fertilization (IVF), and intracytoplasmic sperm injection (ICSI), the management of MFI is mainly performed by gynecologists. ICSI is a powerful “dramatic” tool of ART.[3] ICSI receives a huge media attention because successful pregnancy can be achieved in the most severe cases of MFI even if a single motile sperm is present. It does away with the confrontation in fertilization by zona pellucida and oolemma. The success of ICSI is determined by the maternal age, oocyte quality, and number. It is indeed a paradox that the outcomes of severe MFI are determined by the egg and not the sperm![5]
Andrology is the branch of medicine that deals with physiology and diseases of male reproductive system including infertility, sexual dysfunction, cancers of the reproductive tract, and male contraception.[6] With a powerful tool like ART at our disposal, it is common to find an infertile couple proceeding directly to ART without formal male factor evaluation, hence even andrologists are gradually losing interest in the management of MFI.[7] The surgical procedures performed for MFI have also shown a steady decline.[8] ART is an expensive tool that needs to be used judiciously to save valuable resources. This article is aimed at defining the role of an andrologist in the management of MFI in ART setting.
MATERIALS AND METHODS
For this narrative review, a nonsystematic review of the literature was performed. The search was done on Medline, PubMed, Google Scholar, Scopus, ScienceDirect, SpringerLink, and DiscoverEd. The keywords used were male infertility, urology, azoospermia, andrology, andrologist, ART, IVF, ICSI, and sperm retrieval. In addition, individual terms were also searched. Abstracts in English were scanned, and relevant full-text articles were retrieved and reviewed. Various government, organization, and association websites were searched for relevant details. Books and monographs on the topic were referenced. In addition, reference lists of relevant papers were also searched for additional details. There were no specific exclusion criteria. Editorials, reviews, opinions, debates, letters to editors, and personal communications were included [Figure 1]. No separate segregation of articles from developing or developed countries was made. However, more relevance was placed on studies and data from India. There was no particular time frame applied for the literature. Most of the literature was combined in a simple narrative fashion.
Figure 1.
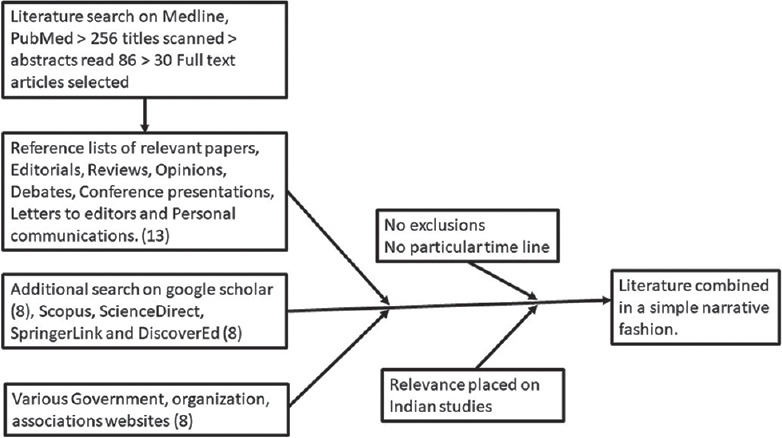
Flowchart for search strategy
WHAT IS ANDROLOGY? WHO IS ANDROLOGIST? DO WE NEED TO ENGAGE THEM?
It is usually believed that the term andrology was first used by a gynecologist, Dr. Harald Siebke in 1952, although andrology as a specialty was recognized as early as October 1891 in an editorial in JAMA. The editorial paralleled andrology with gynecology and also raised concerns about the neglect of male-specific diseases.[9] While a common man is aware about gynecology, most are ignorant about andrology. Even today, andrology as a separate specialty is unknown in most countries except Germany, Italy, Poland, Egypt, and Indonesia.[6] Clinical andrology deals with examination, evaluation, and management of MFI, and in some centers, the andrologist is also called as reproductive urologist.
The Indian Council of Medical Research (ICMR) has published the National Guidelines for ART Clinics in India in 2005.[10] Proper functioning of an ART clinic requires a teamwork between the gynecologist, andrologist, clinical embryologist, counselor, and a program coordinator. The guidelines do not necessitate the involvement of an andrologist at the ART clinics, rather it permits a confident and competent gynecologist to manage such centers. Although the guidelines stress that a qualified urologist must receive additional training in andrology, most gynecologists, as is largely the case with medical specialties, have very little training outside their own branch and are not qualified or trained to examine or treat MFI.[7] It cannot be overemphasized that any person not trained in basic clinical skills of this disorder should not treat it, hence a gynecologist must acquire training in andrology to manage MFI. Sadly, there are very limited opportunities for such training. On the contrary, almost all the prescribed urology curricula over the world (MCh Urology,[11] DNB Urology,[12] Diplomate of American Board of Urology,[13] and FRCS Urology[14]) have extensive andrology training.
An urologist is far better qualified than a gynecologist to manage andrology cases. While there are andrology fellowships in the US, any interested urologist can practice andrology. Most academic centers would hire a fellowship-trained andrologist, but there are no rules or committees that control what an urologist can or cannot do. Someone trained in urology in the US, even without a fellowship, can do anything a fellowship-trained urologist does.
There is a misbelief that andrologists are very few in number. In 2010, Nangia et al. reported that in the USA, many ART centers did not have andrology backup. For a total of 390 ART centers, the authors identified only 197 male infertility specialists.[15] In this study, only American resident members of the Society for the Study of Male Reproduction and the Society for Male Reproduction and Urology were qualified as an andrologist. The author in a personal communication agreed that the denominator in this study is not representative of the urology population in the USA as all urologists in the USA have some andrology training. The society membership directories may underestimate the numbers as interest in a subspecialty does not require fellowship.
Even in Indian context, there is no shortage of andrologists for ART clinics. The January 2021 National Registry of ART Clinics maintained by ICMR lists 542 ART clinics.[16] Most of the cities having these ART clinics have qualified urology services by the full members (Indian citizen with postgraduate qualification in urology) of the Urological Society of India (USI).[17] As of March 2021, there are 2843 full members of the USI, thus there are more than 5 qualified urologists per ART center!
ARE MEN DENIED ANDROLOGY SERVICES?
Semen analysis is usually the only investigation performed for evaluation of MFI. Even when indicated, most men do not undergo any specific detailed evaluation for infertility. Leung presented a cross-sectional study of patient-directed websites of infertility centers in the USA.[18] Only 78% of the websites acknowledged MFI. Of these, 86% of the websites mentioned evaluation of male partner and only 63% mentioned treatment options. Only 23% of the websites discussed referral to an urologist. It is discouraging to note that these websites meant for the infertile couples denied them information regarding importance of MFI. The neglect of MFI is highlighted in a case report by Canale and Caietti[19] of failed testicular sperm aspiration (TESA) in a man with severe oligospermia. While concentrating on sperm retrieval, the important history of receiving testosterone injections for poor sexual drive was missed. This case may just be a tip of iceberg, as in this era of ICSI, without proper history and evaluation, the only credit the infertile male receives is in the number of sperms retrieved.
There is a law in Italy recommending diagnosis and treatment of MFI before offering ART to the couple. ART is allowed only as a last resort when no other therapeutic interventions are available. Duca et al.[20] in a multicenter cross-sectional survey evaluated young Italian couples who were considered for ART. In the 320 couples studied, 75 (23%) men had untreated oligoasthenoteratozoospermia. Forty-five (14%) men had a clinically significant varicocele. Sixty-two (19%) men had untreated leukocytospermia or urogenital infections. Hence, more than half of these couples had MFI which was potentially correctable. The authors rightly recommend minimal andrological evaluation and specific treatment rather than invasive and expensive ART in these couples.
ROLE OF AN ANDROLOGIST IN ART
The success of management for MFI is difficult to assess as the treatment is given to a male, but the outcome or endpoint is assessed by pregnancy in the female. To overcome this issue, many reports have used improvement in semen parameter as the surrogate outcome measure, knowing very well that the semen parameters have no absolute correlation with the pregnancy rate. There are literature reports refuting any predictive value of routine examination of the male partner.[21] Hargreave et al.[22] evaluated various prognostic factors for male infertility. Although the authors could identify major prognostic factors impacting male infertility, attending the infertility clinic had no impact on future fertility. Over three decades since this honest article, there have been significant inroads into the understanding of male infertility. With improved understanding of the pathophysiology, the andrologist has an important role in the management of infertile couples.[23] Today, an andrologist plays many significant roles in the management of MFI in an ART clinic as below:
Evaluation of Male Partner
With the rapid advances in ART, evaluation of male partner is limited to just a semen analysis. With a perception that MFI is usually not treatable, referral to an andrologist is rarely done. In men with semen abnormalities, resorting to ART circumventing the male problem is an easier way out. Male evaluation is usually delayed till either ART is planned or has failed. Honig et al.[24] performed a retrospective analysis of 1236 new MFI patients with an intent to devise a basic screening protocol to identify patients with significant medical pathology. Thirteen patients had major pathologies such as testicular tumors, brain tumors (such as craniopharyngiomas, pituitary adenoma, and prolactinoma), seminal vesicle cyst, Klinefelter's syndrome, ureterocele, and sacral ependymoma. Doing only semen analysis without formal evaluation by an urologist would have missed these life-threatening conditions. Although serious condition was detected in just 1.1% of this study population, infertility in these patients was just one symptom that led to proper diagnosis. A delay in evaluation of these men may have had an adverse effect on their prognosis, as both testicular tumor and pituitary tumor are fast growing but potentially curable.[24] Similarly, Kolettis and Sabanegh found significant medical pathologies in 6% of the patients including cystic fibrosis mutations, karyotypic abnormalities, testis cancer, prostate cancer, diabetes mellitus, and hypothyroidism. These pathologies do threaten the health of male partner and potential offspring.[25]
Life-threatening conditions can also be found during secondary infertility evaluation. Simon et al. published a case report of two patients with seminoma that presented with oligospermia and oligoasthenospermia.[26] Bieniek et al. prospectively evaluated 4088 infertile men by scrotal ultrasound and incidentally detected small testicular masses <1 cm in 120 (2.9%) of them. Among them, 18 needed extirpative surgery (six for malignancy) while the rest 102 were under surveillance. Although most of these small testicular masses could be safely observed, it is important to diagnose them.[27]
It is interesting to note that many recent reports suggest semen quality to be a surrogate marker of overall male health. In a cohort study of 11,935 men evaluated for infertility, Eisenberg et al.[28] found that men with impaired semen parameters had higher mortality rates. The same group in a cross-sectional study of 9387 infertile men found that 44% of them had additional one or more medical diagnosis unrelated to infertility like higher Charlson Comorbidity Index with endocrine, circulatory, cerebrovascular, genitourinary, and skin diseases.[29] Infertility has also been linked to increased risk of high-grade prostate cancer[30] and testicular cancer.[31]
For some men, infertility evaluation may be the only instance of evaluation by a health-care professional, hence evaluation of the male partner is of utmost importance not only for the diagnosis of infertility but for the general health of the man. This should be done irrespective of semen analysis parameters by an andrologist as infertility may be a harbinger of some serious medical conditions.
Prognostication and Counseling
Infertility is a stressful situation for the couple, and from the man's point of view, his fertility is a sign of his virility. Often during ART, men are treated as observers and women as the participants.[32] They may not be referred by their name and be called as husband of someone and may feel diminished to mere donor of the sperms for the ART cycle. There is a higher incidence of sexual problems in infertile men which gets compounded by the need for “timed intercourse” and “sex by the clock.” Unsuccessful testicular sperm extraction (TESE) also aggravates erectile dysfunction (ED).[33] Religious belief may make masturbation difficult for some of them.[34] As andrologists understand the pathology, they are in better position to understand the anguish of these men and improve their involvement in decision-making.
Glover et al.[35] analyzed the effect of medical consultation on anxiety and depression in men with MFI. Utilizing standardized scales, they found a decrease in the anxiety levels after consultation. Even the men with poor fertility prognosis were more optimistic after the consultation.[35] Surely, there is an urgent need of psychological support for these infertile men either in the andrology or infertility clinics.[36]
Role in Specific Conditions
Measures to improve spermatogenesis before ART
Patients with nonobstructive azoospermia (NOA) have a guarded prognosis for sperm yield during surgical sperm retrieval (SSR). As most of these men already have elevated gonadotrophins, hormone therapy seems paradoxical. Some authors have tried superstimulating these testes to function. Hussein has reported the usefulness of clomiphene citrate in men with NOA before SSR and found that two-thirds of the azoospermic patients produced sperms in ejaculate too![37] They further suggested a protocol of clomiphene citrate, human chorionic gonadotropin (hCG), and human menopausal gonadotropin in the treatment of non-NOA.[38] Patients responding with increased levels of follicle-stimulating hormone (FSH) and total testosterone had an increased rate of sperm in ejaculation and a better yield with microdissection testicular sperm extraction (mTESE).[38] Shiraishi et al. demonstrated that the administration of high-dose gonadotropins in patients with failed mTESE could yield sperms in 20% of the patients with repeat mTESE.[39] The evidence supporting such superstimulating therapy is, however, limited. However, Reifsnyder et al. in a retrospective study of 1054 men did not find much benefit of this therapy.[40] These are difficult cases to manage. Clinicians try too many modalities to help these patients, sometimes without much benefit. Hormonal treatment is usually considered appropriate in men with low testosterone when gonadotropins are not too elevated. In a patient with serum testosterone >400 ng/dL and gonadotropins >1.5 times the upper limit, hormonal treatment is usually not warranted.[41] Hypogonadotropic hypogonadism is an uncommon but potentially treatable cause of MFI. Various treatments used in this condition are gonadotropin-releasing hormone, hCG, and recombinant FSH. A few of these patients need only short-term treatment.[42]
Of men presenting for infertility evaluation, 35%–40% would have a clinical varicocele. Meticulous palpation by an experienced andrologist is important as only the varicoceles diagnosed on clinical examination are associated with infertility. Surgery for subclinical varicoceles picked up on scrotal Doppler ultrasound has no beneficial effect on fertility.[43] In selected patients, varicocele repair (VR) is a potentially cuarative and cost-effective treatment for MFI. VR leads to improved semen parameters, pregnancy rates, and live birth rates.[43] VR has potential of either eliminating the need or downgrading the ART intervention[44] and may be a permanent solution for MFI unlike ART. VR may be considered in some azoospermic and cryptozoospermic men even if there are clear-cut female factor indications for IVF.[43] Spontaneous pregnancy is also possible in some men with NOA. In NOA, men with late maturation arrest and hypospermatogenesis have a higher likelihood of success with VR.[45]
Obstructive Azoospermia
Obstructive azoospermia (OA) because of obstruction in epididymis, vas (vasectomy), and ejaculatory duct obstruction (EDO) is amenable to surgical therapy and is potentially curable. While the results of vasoepididymal anastomosis are perceived to be poor, some centers have reported success rates ranging between 40% and 80% in different subpopulations.[46] Interestingly Shah[47] reported a series of ten azoospermic men with genital tuberculosis (GTB) treated with anti-Koch's treatment (AKT). Six men had reappearance of sperms after AKT. There is potential of cure in some patients with GTB.[47]
Microsurgical vasovasostomy is a reliable and cost-effective modality in most of the men with vasal obstruction.[48] Similarly, in EDO with dilated seminal vesicles and midline prostatic cyst, transurethral resection of ejaculatory duct is the procedure of choice.[49] Of course, the surgical procedure for OA is worthwhile if the female partner has good ovarian reserve and intact genital tract. The main advantage is that the couple can plan multiple pregnancies.
Male Sexual Dysfunction
The anxiety of producing semen sample on demand may lead some men to situational ED or anejaculation. They can be offered phosphodiesterase inhibitors, vibrator, electroejaculation, or SSR through TESA/TESE.[50] Percutaneous epididymal sperm aspiration (PESA) should not be offered to these men because of the fear of causing epididymal obstruction.[50] PESA in this situation is unindicated, and a well-informed andrologist is unlikely to commit such a mistake.
Male sexual dysfunction (MSD) contributes to around a quarter of cases of unconsummated marriage. Home intravaginal insemination (IVI) is a simple and effective method of managing infertility in these patients.[51] In infertility due to MSD, IVI should be utilized before resorting to ART.[52] Men with spinal cord injury have infertility due to ED, anejaculation, and semen abnormalities. These men should be offered vibrator stimulation or electroejaculation.[53] However, these methods are not utilized because of lack of equipment or training.[54] In India, electroejaculation is not easily available, and most of the urologists are not trained at using electroejaculation device. When these two modes are either not available or have failed, TESA can be performed.[41]
Surgical Sperm Retrieval
SSR is routinely performed at IVF clinics. There are a variety of techniques for this, and it is important to choose the most appropriate technique for specific situations. In OA when operative correction is not contemplated, the sperm retrieval can be performed by PESA or microsurgical epididymal sperm aspiration. If operating microscope is not available, open fine-needle aspiration or single open testicular biopsy would suffice.[55] SSR in NOA is more challenging as there are no reliable predictors for sperm retrieval. It is possible to get sperms from a small testis with high FSH and low testosterone, while we may fail in another with normal-sized testis and normal FSH.
TESA or testicular FNA, although widely practiced by gynecologists, is not recommended for NOA patients.[41] PESA has no role in NOA. Needle aspiration biopsy or needle TESE gives a better sperm retrieval rate. Single seminiferous tubule (SST) mapping would give a better SSR in a normal-sized testis, with much less trauma to the testis as compared to TESE or mTESE. However, SST mapping is not satisfactory in small fibrotic or atrophic testis and also in cases with very focal spermatogenesis as it samples only the surface of the testis.[41] mTESE is the most efficient but most traumatic method of SSR in NOA. The first attempt at sperm retrieval usually is the best attempt in NOA. In most centers, SSR in the cases of NOA is scheduled on the same day of egg pickup. This exposes both the partners to a surgical procedure on the same day.[56] Availability of an andrologist for integrated single-session staged sperm retrieval is crucial in this scenario. The role of an andrologist is far more than being a sperm retrieval technician looking at the complexity of SSR in NOA.[41]
Identifying Patients who Would Need Nothing but ART
There are some conditions wherein no medical or surgical treatment would work. An andrologist has to identify these patients to avoid wastage of time and money on ineffective treatments.[57]
Globozoospermia
This is a rare type of teratozoospermia (0.1% of andrological patients) wherein the acrosome of spermatozoa is absent, hence they appear round headed. It is classified as total or partial based on how many spermatozoa are round headed. There are no identifying phenotypic characteristics. There have been few reports of paternity in globozoospermia, but they were not confirmed by a paternity test. For globozoospermia, ICSI is the treatment of choice.[58]
Female Aging
With increasing age, especially after the age of 30 years, fertility of a woman decreases. This decline is slow and steady between 30 and 35 years of age and accelerates after 35. There is no treatment strategy to make up for this age-related decline.[59] Anti-Mullerian hormone is a reliable predictor of ovarian reserve and is also a predictor of live birth after ART.[60] If the female's age is more than 40 years or if the antral follicle count (AFC) is low, any treatment for male infertility would be ineffective.[57]
Yq Microdeletions
The determinants of spermatogenesis are mapped on the long arm of Y chromosome (Yq) collectively called azoospermia factors (AZF). Genetic domains are referred to as AZFa, AZFb, and AZFc. The Yq microdeletions are not found in normospermia but are frequently associated with azoospermia and oligospermia. SSR should not be attempted in complete deletions of AZFa and AZFb. Conversely, men with AZFc deletion will have sperms in either semen or testes.[61]
Congenital Bilateral Absence of the Vas Deferens
Congenital bilateral absence of the vas deferens (CBAVD) is found in 2%–6% of infertile men and 25% of cases with OA.[62] An andrologist can clinically diagnose this condition. CBAVD is usually associated with mutations in cystic fibrosis transmembrane conductance regulator (CFTR) gene and congenital renal anomalies. It is generally believed that men with CBAVD and renal anomalies rarely have CFTR abnormalities.[63] However, Gajbhiye et al.[62] reported a series of five Indian men with CFTR mutations with CBAVD and unilateral renal agenesis. Hence, a change in policy of not offering CFTR assay in men with CBAVD and renal anomaly may be prudent looking at this report. CFTR assay is sometimes omitted because of cost constraints. If there are financial constraints, CFTR assay may be offered to the wife if husband has CBAVD without renal anomaly. Most of the CBAVD men would be subjected to PESA or TESE for SSR. Andrologists have a significant role in selecting appropriate patients for ART as CBAVD with CFTR gene mutations is transmitted as an autosomal recessive trait.
Is There a Role for Andrologists in Future?
Current infertility practices put a lot of burden on women. Comparatively, the male evaluation is simple, less elaborate, and less invasive. It is possible that MFI evaluation and treatment may downgrade the ART procedure from ICSI to IUI or may completely eliminate it.[64] An issue of concern is the poorer ovarian reserve in Indian women.[65] AFC of Indian women is comparable to AFC of a 6.3-year-older Spanish woman.[66] This suggests premature ovarian aging in Indian women. Another concern is the declining sperm counts. A meta-analysis[67] has reported a 50% decline in sperm counts between 1973 and 2011. Coupled with the fact many women are delaying childbearing because of social, economic, and cultural reasons, we are likely to see many women needing ART at an earlier age. Evaluation and treatment of MFI by andrologists will reduce some burden of these women on ART clinics.
Medicolegal Aspects
It is imperative that the ART center should have andrologists as a panel member, especially when ART is performed for MFI. Resorting to expensive therapies such as ICSI and IVF without proper diagnosis of MFI may have medicolegal implications. Ahypogonadal male is likely to respond to gonadotrophin therapy obviating the need of IVF. Undescended testes may present as severe oligospermia and azoospermia. These have risk of malignant transformation. Andrological evaluation can uncover the underlying problem. Utilizing ART in these couples without proper male evaluation may invite trouble for treating gynecologists.[7] PESA in ejaculatory failure should be avoided for the possibility of causing epididymal obstruction.
CONCLUSIONS
It is not the purpose of this review to underplay the role of ART in MFI, rather the authors wish to propose the role of an andrologist in this setup. Andrological evaluation of male partner in all couples presenting with infertility is necessary for proper evaluation of the couple. An andrologist can uncover associated potentially curable but life-threatening condition in some patients. The role of an andrologist goes far beyond performing SSR. They are better qualified to select the males who are best candidates for SSR and also determine the most effective SSR modality. Andrological evaluation and intervention before ART may eliminate the need for or downgrade the ART needed. Andrological interventions aid in optimizing ART outcome. The presence of andrologists in ART team adds an infinite value.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
Dr. Rupin Shah, Lilavati Hospital, Mumbai
Dr. Ranjith Ramasamy, University of Miami, USA
Dr. Arun Rathi, Siddhivinayak Test Tube Baby Centre, Akola
Dr. Deepali Shukla, Shukla Test Tube Baby Centre, Akola.
REFERENCES
- 1.Widge A. Sociocultural attitudes towards infertility and assisted reproduction in India. Curr Pract Controv Assist Reprod. 2002;60:74. [Google Scholar]
- 2.Hull MG, Glazener CM, Kelly NJ, Conway DI, Foster PA, Hinton RA, et al. Population study of causes, treatment, and outcome of infertility. Br Med J (Clin Res Ed) 1985;291:1693–7. doi: 10.1136/bmj.291.6510.1693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Petok WD. Infertility counseling (or the lack thereof) of the forgotten male partner. Fertil Steril. 2015;104:260–6. doi: 10.1016/j.fertnstert.2015.04.040. [DOI] [PubMed] [Google Scholar]
- 4.Cummins JM, Jequier AM. Treating male infertility needs more clinical andrology, not less. Hum Reprod. 1994;9:1214–9. doi: 10.1093/oxfordjournals.humrep.a138681. [DOI] [PubMed] [Google Scholar]
- 5.Sherins RJ, Thorsell LP, Dorfmann A, Dennison-Lagos L, Calvo LP, Krysa L, et al. Intracytoplasmic sperm injection facilitates fertilization even in the most severe forms of male infertility: Pregnancy outcome correlates with maternal age and number of eggs available. Fertil Steril. 1995;64:369–75. doi: 10.1016/s0015-0282(16)57737-1. [DOI] [PubMed] [Google Scholar]
- 6.Rankin TL. Andrology as the medical speciality to focus medical training on men's health? J Mens Heal Gend. 2005;2:45–8. [Google Scholar]
- 7.Jequier AM. Clinical andrology – Still a major problem in the treatment of infertility. Hum Reprod. 2004;19:1245–9. doi: 10.1093/humrep/deh269. [DOI] [PubMed] [Google Scholar]
- 8.Ketefian A, Hu J, Bartolucci AA, Schlegel PN, Azziz R. Society of Reproductive Surgeons, Inc. Fifteen-year trend in the use of male reproductive surgery: Analysis of the healthcare cost and utilization project data. BJU Int. 2011;107:1118–23. doi: 10.1111/j.1464-410X.2010.09632.x. [DOI] [PubMed] [Google Scholar]
- 9.Niemi M. Andrology as a specialty its origin. J Androl. 1987;8:201–2. doi: 10.1002/j.1939-4640.1987.tb03302.x. [DOI] [PubMed] [Google Scholar]
- 10.ICMR. National Guidelines for Accreditation, Supervision and Regulation of ART Clinics in India. 2005. 2005. [Last accessed on 2021 Apr 11]. pp. 1–33. Available from: https://main.icmr.nic.in/sites/default/files/art/ART_Pdf.pdf .
- 11.AIIMS. Syllabus D M/M Ch at the AIIMS. 2005. 2005. [Last accessed on 2021 Apr 11]. pp. 1–31. Available from: https://www.aiims.edu/aiims/academic/aiims-syllabus/Syllabus-DM M Ch.pdf .
- 12.NBE. Guidelines for Competency Based Training Programme in DNB- UROLOGY. [Last acessed on 2021 Apr 11]. Available from: https://nbe.edu.in/mainpdf/curriculum/UROLOGY.pdf .
- 13.Thrasher JB. The American Board of Urology, Inc. 2021 Information for Applicants and Candidates. 2021. [Last accessed on 2021 Apr 18]. pp. 1–60. Available from: https://www.abu.org/images/pdfs/2021-Cert-Handbook.pdf .
- 14. [Last accessed on 2021 Apr 18];JSCFE. Joint Surgical Colleges Fellowship Examinations Syllabus Urology. 2014 2014:1–60. Available from: https://www.jscfe.co.uk/Utils/DocumentGenerator.aspx?Type=CMS anddocID=dcf78f8d.f0eb.4da4.b9d8.4b76773aad2c . [Google Scholar]
- 15.Nangia AK, Likosky DS, Wang D. Distribution of male infertility specialists in relation to the male population and assisted reproductive technology centers in the United States. Fertil Steril. 2010;94:599–609. doi: 10.1016/j.fertnstert.2009.02.012. [DOI] [PubMed] [Google Scholar]
- 16.ICMR. List of Enrolled ART Clinics under National Registry of ART Clinics and Banks of India. 27.January_2021. 2015. [Last accessed on 2021 Apr 11]. pp. 1–68. Available from: http://www.icmr.nic.in/icmrnews/art/New listof approved ART Clinics_30.09.2015.pdf .
- 17.USI. Urological Society of India Member Directory. 2021. [Last accessed on 2021 Apr 18]. Available from: https://www.usi.org.in/members-directory/
- 18.Leung A, Khan Z, Patil D, Mehta A. What are infertility treatment center websites telling couples about male factor infertility? Fertil Steril. 2014;102:e47. doi: 10.1016/j.urpr.2016.03.001. [DOI] [PubMed] [Google Scholar]
- 19.Canale D, Caietti L. Infertile male patients are patients, not numbers. Hum Reprod. 1996;11:2807. doi: 10.1093/oxfordjournals.humrep.a019217. [DOI] [PubMed] [Google Scholar]
- 20.Duca Y, Calogero AE, Condorelli RA, Giammusso B, La Vignera S. Collaborators (Redox Group Catania). Early male aging or poor clinical consideration for males in IVF centers? An original study. The Aging Male. 2020;23(5):882, 6. doi: 10.1080/13685538.2019.1618260. DOI: 10.1080/13685538.2019.1618260. [DOI] [PubMed] [Google Scholar]
- 21.Dunphy BC, Kay R, Barratt CL, Cooke ID. Is routine examination of the male partner of any prognostic value in the routine assessement of couples who complain of involuntary infertility? Fertil Steril. 1989;52:454–6. doi: 10.1016/s0015-0282(16)60918-4. [DOI] [PubMed] [Google Scholar]
- 22.Hargreave TB, McGowan B, Harvey J, McParland M, Elton RA. Is a male infertility clinic of any use? Br J Urol. 1986;58:188–93. doi: 10.1111/j.1464-410x.1986.tb09024.x. [DOI] [PubMed] [Google Scholar]
- 23.Kekre NS. Male infertility clinic – Is it useful? Indian J Urol. 2011;27:1. doi: 10.4103/0970-1591.78399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Honig SC, Lipshultz LI, Jarow J. Significant medical pathology uncovered by a comprehensive male infertility evaluation. Fertil Steril. 1994;62:1028–34. [PubMed] [Google Scholar]
- 25.Kolettis PN, Sabanegh ES. Significant medical pathology discovered during a male infertility evaluation. J Urol. 2001;166:178–80. [PubMed] [Google Scholar]
- 26.Simon SD, Lee RD, Mulhall JP. Should all infertile males undergo urologic evaluation before assisted reproductive technologies? Two cases of testicular cancer presenting with infertility. Fertil Steril. 2001;75:1226–7. doi: 10.1016/s0015-0282(01)01773-3. [DOI] [PubMed] [Google Scholar]
- 27.Bieniek JM, Juvet T, Margolis M, Grober ED, Lo KC, Jarvi KA. Prevalence and management of incidental small testicular masses discovered on ultrasonographic evaluation of male infertility. J Urol. 2018;199:481–6. doi: 10.1016/j.juro.2017.08.004. [DOI] [PubMed] [Google Scholar]
- 28.Eisenberg ML, Li S, Behr B, Cullen MR, Galusha D, Lamb DJ, et al. Semen quality, infertility and mortality in the USA. Hum Reprod. 2014;29:1567–74. doi: 10.1093/humrep/deu106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eisenberg ML, Li S, Behr B, Pera RR, Cullen MR. Relationship between semen production and medical comorbidity. Fertil Steril. 2015;103:66–71. doi: 10.1016/j.fertnstert.2014.10.017. [DOI] [PubMed] [Google Scholar]
- 30.Walsh TJ, Schembri M, Turek PJ, Chan JM, Carroll PR, Smith JF, et al. Increased risk of high-grade prostate cancer among infertile men. Cancer. 2010;116:2140–7. doi: 10.1002/cncr.25075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Walsh TJ, Croughan MS, Schembri M, Chan JM, Turek PJ. Increased risk of testicular germ cell cancer among infertile men. Arch Intern Med. 2009;169:351–6. doi: 10.1001/archinternmed.2008.562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.O'Donnell E. Making room for men in infertility counseling. J Fam Pr. 2007;5:28–32. [Google Scholar]
- 33.Akbal C, Mangir N, Tavukçu HH, Özgür Ö, Şimşek F. Effect of testicular sperm extraction outcome on sexual function in patients with male factor infertility. Urology. 2010;75:598–601. doi: 10.1016/j.urology.2009.07.1330. [DOI] [PubMed] [Google Scholar]
- 34.Wischmann T. 'Your count is zero' – Counselling the infertile man. Hum Fertil (Camb) 2013;16:35–9. doi: 10.3109/14647273.2013.776179. [DOI] [PubMed] [Google Scholar]
- 35.Glover L, Gannon K, Sherr L, Abel PD. Psychological distress before and immediately after attendance at a male sub-fertility clinic. J R Soc Med. 1994;87:448–9. doi: 10.1177/014107689408700806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Niederberger C. Re: Infertility counseling (or the Lack Thereof) of the forgotten male partner. J Urol. 2016;195:1077. doi: 10.1016/j.juro.2016.01.032. [DOI] [PubMed] [Google Scholar]
- 37.Hussein A, Ozgok Y, Ross L, Niederberger C. Clomiphene administration for cases of nonobstructive azoospermia: A multicenter study. J Androl. 2005;26:787–91. doi: 10.2164/jandrol.04180. [DOI] [PubMed] [Google Scholar]
- 38.Hussein A, Ozgok Y, Ross L, Rao P, Niederberger C. Optimization of spermatogenesis-regulating hormones in patients with non-obstructive azoospermia and its impact on sperm retrieval: A multicentre study. BJU Int. 2013;111:1–5. doi: 10.1111/j.1464-410X.2012.11485.x. [DOI] [PubMed] [Google Scholar]
- 39.Shiraishi K, Ohmi C, Shimabukuro T, Matsuyama H. Human chorionic gonadotrophin treatment prior to microdissection testicular sperm extraction in non-obstructive azoospermia. Hum Reprod. 2012;27:331–9. doi: 10.1093/humrep/der404. [DOI] [PubMed] [Google Scholar]
- 40.Reifsnyder JE, Ramasamy R, Husseini J, Schlegel PN. Role of optimizing testosterone before microdissection testicular sperm extraction in men with nonobstructive azoospermia. J Urol. 2012;188:532–7. doi: 10.1016/j.juro.2012.04.002. [DOI] [PubMed] [Google Scholar]
- 41.Shah R, Gupta C. Advances in sperm retrieval techniques in azoospermic men: A systematic review. Arab J Urol. 2018;16:125–31. doi: 10.1016/j.aju.2017.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dabaja AA, Schlegel PN. Medical treatment of male infertility. Transl Androl Urol. 2014;3:9–16. doi: 10.3978/j.issn.2223-4683.2014.01.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Masson P, Brannigan RE. The varicocele. Urol Clin North Am. 2014;41:129–44. doi: 10.1016/j.ucl.2013.08.001. [DOI] [PubMed] [Google Scholar]
- 44.Sönmez MG, Haliloğlu AH. Role of varicocele treatment in assisted reproductive technologies. Arab J Urol. 2018;16:188–96. doi: 10.1016/j.aju.2018.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Weedin JW, Khera M, Lipshultz LI. Varicocele repair in patients with nonobstructive azoospermia: A meta-analysis. J Urol. 2010;183:2309–15. doi: 10.1016/j.juro.2010.02.012. [DOI] [PubMed] [Google Scholar]
- 46.Kumar R. Surgery for azoospermia in the Indian patient: Why is it different? Indian J Urol. 2011;27:98–101. doi: 10.4103/0970-1591.78441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shah RS. 1600: Obstructive azoospermia following genital tuberculosis may be reversible with medical therapy. J Urol. 2004;171:422. [Google Scholar]
- 48.Shridharani A, Sandlow JI. Vasectomy reversal versus IVF with sperm retrieval: Which is better? Curr Opin Urol. 2010;20:503–9. doi: 10.1097/MOU.0b013e32833f1b35. [DOI] [PubMed] [Google Scholar]
- 49.Wosnitzer MS, Goldstein M. Obstructive azoospermia. Urol Clin North Am. 2014;41:83–95. doi: 10.1016/j.ucl.2013.08.013. [DOI] [PubMed] [Google Scholar]
- 50.Arafa M, Elbardisi H, Majzoub A. The Complete Guide to Male Fertility Preservation. Cham: Springer; 2018. Sperm retrieval in ejaculatory dysfunction; pp. 43–56. [Google Scholar]
- 51.Banerjee K, Singla B. Pregnancy outcome of home intravaginal insemination in couples with unconsummated marriage. J Hum Reprod Sci. 2017;10:293–6. doi: 10.4103/jhrs.JHRS_5_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kaseki H, Kaseki S, Shimizu M, Hayashi A, Suganuma N. Indication of intravaginal insemination for infertility treatment in couples with sexual dysfunction. Reprod Med Biol. 2021;20:241–5. doi: 10.1002/rmb2.12376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ibrahim E, Lynne CM, Brackett NL. Male fertility following spinal cord injury: An update. Andrology. 2016;4:13–26. doi: 10.1111/andr.12119. [DOI] [PubMed] [Google Scholar]
- 54.Kafetsoulis A, Brackett NL, Ibrahim E, Attia GR, Lynne CM. Current trends in the treatment of infertility in men with spinal cord injury. Fertil Steril. 2006;86:781–9. doi: 10.1016/j.fertnstert.2006.01.060. [DOI] [PubMed] [Google Scholar]
- 55.Shah R. Surgical sperm retrieval: Techniques and their indications. Indian J Urol. 2011;27:102–9. doi: 10.4103/0970-1591.78439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sandlow J. Clomiphene administration for cases of nonobstructive azoospermia: A multicenter study: Editorial commentary. J Androl. 2005;26:792–3. doi: 10.2164/jandrol.04180. [DOI] [PubMed] [Google Scholar]
- 57.Cavallini G, Beretta G. The role of the andrologist in assisted reproduction. In: Cavallini G, Beretta G, editors. Clinical Management of Male Infertility. Springer Cham Heidelberg New York Dordrecht London: 2015. pp. 173–7. DOI: 10.1007/978-3-319-08503-6. [Google Scholar]
- 58.Dam AH, Feenstra I, Westphal JR, Ramos L, van Golde RJ, Kremer JA. Globozoospermia revisited. Hum Reprod Update. 2007;13:63–75. doi: 10.1093/humupd/dml047. [DOI] [PubMed] [Google Scholar]
- 59.Alviggi C, Humaidan P, Howles CM, Tredway D, Hillier SG. Biological versus chronological ovarian age: Implications for assisted reproductive technology. Reprod Biol Endocrinol. 2009;7:101. doi: 10.1186/1477-7827-7-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wang S, Zhang Y, Mensah V, Iii WJ, Huang Y, Alvero R. Discordant anti-müllerian hormone (AMH) and follicle stimulating hormone (FSH) among women undergoing in vitro fertilization (IVF): Which one is the better predictor for live birth? J Ovarian Res. 2018;11:1–8. doi: 10.1186/s13048-018-0430-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hopps CV, Mielnik A, Goldstein M, Palermo GD, Rosenwaks Z, Schlegel PN. Detection of sperm in men with Y chromosome microdeletions of the AZFa, AZFb and AZFc regions. Hum Reprod. 2003;18:1660–5. doi: 10.1093/humrep/deg348. [DOI] [PubMed] [Google Scholar]
- 62.Gajbhiye R, Kadam K, Khole A, Gaikwad A, Kadam S, Shah R, et al. Cystic fibrosis transmembrane conductance regulator (CFTR) gene abnormalities in Indian males with congenital bilateral absence of vas deferens and renal anomalies. Indian J Med Res. 2016;143:616–23. doi: 10.4103/0971-5916.187110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Schlegel PN, Shin D, Goldstein M. Urogenital anomalies in men with congenital absence of the vas deferens. J Urol. 1996;155:1644–8. [PubMed] [Google Scholar]
- 64.Turner KA, Rambhatla A, Schon S, Agarwal A, Krawetz SA, Dupree JM, et al. Male infertility is a women's health issue-research and clinical evaluation of male infertility is needed. Cells. 2020;9:1–4. doi: 10.3390/cells9040990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Palgamkar J, Agarwal S, Shah NJ, Sanghavi DR, Almeida FD, Mehta T, et al. Declining trend of AMH levels in Indian women of reproductive age group: The Jaslok experience. Fertil Steril. 2019;112:e386. [Google Scholar]
- 66.Iglesias C, Banker M, Mahajan N, Herrero L, Meseguer M, Garcia-Velasco JA. Ethnicity as a determinant of ovarian reserve: Differences in ovarian aging between Spanish and Indian women. Fertil Steril. 2014;102:244–9. doi: 10.1016/j.fertnstert.2014.03.050. [DOI] [PubMed] [Google Scholar]
- 67.Levine H, Jørgensen N, Martino-Andrade A, Mendiola J, Weksler-Derri D, Mindlis I, et al. Temporal trends in sperm count: A systematic review and meta-regression analysis. Hum Reprod Update. 2017;23:646–59. doi: 10.1093/humupd/dmx022. [DOI] [PMC free article] [PubMed] [Google Scholar]


