Abstract
Objectives.
Few couple-focused interventions have improved psychological and relationship functioning among men diagnosed with localized prostate cancer and their spouses. This study compared the impact of intimacy-enhancing therapy (IET), a general health and wellness intervention (GHW), and usual care (UC) on the psychological and relationship functioning of localized prostate cancer patients and their partners. Relationship length, relationship satisfaction, and patient masculinity were evaluated as moderators.
Design.
This study was a randomized clinical trial with three study arms and four assessment time points.
Methods.
A total of 237 patients and partners were randomly assigned to receive IET, GHW, or UC. Participants completed measures of psychological functioning and relationship satisfaction at baseline, 5 weeks, 3 months, and 6 months post-baseline. Primary outcomes were psychological adjustment, depression, cancer-specific distress, cancer concerns, and relationship satisfaction.
Results.
Spouses in IET showed greater increases in relationship satisfaction than spouses in GHW and UC between the baseline and 5-week follow-up. Among patients in longer relationships, significant increases in psychological adjustment were found in both treatments compared to UC. Among spouses in longer relationships, psychological adjustment increased in both IET and UC but declined in GHW.
Conclusions.
Intimacy-enhancing therapy did not show an impact on general or cancer-specific distress, but did show an early impact on relationship satisfaction among spouses. IET was superior to UC for patients in longer relationships. It will be important for researchers to understand which couple-focused interventions benefits both patients and spouses and to identify characteristics of patients, partners, and couples who may not benefit from psychological treatments.
Along with the practical and emotional stressors that accompany the diagnosis of any type of cancer, the unique long-term sequelae associated with localized prostate cancer can pose a challenge to the patient, the spouse, and to their relationship. These treatment effects can include impaired erectile functioning, urinary incontinence, problematic bowel function, and erectile dysfunction (Burnett et al., 2007; Gacci et al., 2009; Penson et al., 2005). In addition, localized prostate cancer patients report lower health-related quality of life than men in the general population (Love et al., 2008; Mols, van de Poll-Franse, Vingerhoets, & Essink-Bot, 2006; van Stam et al., 2017). Between 15% and 18% of patients report elevated depressive symptoms, and between 15% and 27% report elevated anxiety (e.g., Cliff & MacDonagh, 2000; Trinchieri, Nicola, Masini, & Mangiarotti, 2005). Spouse quality of life also declines, particularly among spouses reporting greater bother from the patient’s urinary and sexual side effects (Harden, Sanda, Wei, & Northouse, 2013). Spouse depression and anxiety are also higher than the general population (e.g., Couper et al., 2006; Eton, Lepore, & Helgeson, 2005; Winters-Stone, Lyons, Bennett, & Beer, 2014)).
For these reasons, localized prostate cancer can take a toll on the marital relationship, and how couples handle this experience is important. Relationship quality declines after diagnosis, particularly among partners (Couper et al., 2006). Partners report sexual dissatisfaction (Garos, Kluck, & Aronoff, 2007) and poorer relationship communication (Manne, Badr, Zaider, Nelson, & Kissane, 2010). Constructive marital communication is associated with better patient and spouse quality of life and marital satisfaction (Badr & Taylor, 2009; Manne et al., 2010, 2015; Song et al., 2012). Despite its importance, some couples struggle to communicate (Badr & Taylor, 2009; Haun, Sklenarova, Brechtel, Herzog, & Hartmann, 2014; Manne et al., 2010, 2015). Avoiding discussion of cancer-related concerns, particularly sexuality and worries about the future, is relatively common in this population (Manne et al., 2015).
Although relationship communication clearly plays a role in couples’ adaptation, there have been relatively few empirically based couple-focused interventions targeted to men with prostate cancer. Two studies have targeted patients’ communication about sexual concerns and use of erectile aids (Canada, Neese, Sui, & Schover, 2005; Chambers et al., 2015). Despite achieving greater use of erectile aids, they did not improve relationship satisfaction or quality of life. Northouse et al. (2007) evaluated a three-session supportive, educational intervention for prostate cancer patients and spouses. They encouraged teamwork and living with uncertainty. Patients in the intervention group reported less uncertainty and more relationship communication than controls. There were no benefits on patients’ quality of life.
Based on the Relationship Intimacy Model of Cancer Adaptation (Manne & Badr, 2008), we developed and evaluated a five session intimacy-enhancing therapy (IET) for men diagnosed with prostate cancer and their spouses (Manne et al., 2011) and compared it with usual care. We designed IET to improve the quality of communication about cancer-related concerns. Although we did not show an overall effect on patient and spouse distress and relationship outcomes, IET reduced psychological distress among patients endorsing more cancer concerns or poorer relationship communication, and reduced distress among spouses endorsing greater cancer-specific distress, lower relationship satisfaction, less relationship intimacy, and poorer communication (Manne et al., 2011).
The current study extends our previous work in four ways. Most importantly, we compared IET with another couple-focused intervention to ensure that benefits were not only the result of time and attention. We developed a general health and wellness intervention (GHW), in which conjoint sessions focused on adopting and maintaining a healthy lifestyle. Content included nutrition education and goal setting, maintaining a healthy weight, engaging in regular physical activity, and relaxation. We selected this comparison because lifestyle interventions that include diet and physical activity improve quality of life outcomes among men with prostate cancer (Winters-Stone et al., 2016) (see Menichetti et al., 2016 for a review). In addition, partnered physical activity may enhance relationship intimacy (Lyons, Winters-Stone, Bennett, & Beer, 2016). Thus, GHW was a viable intervention that would both engage couples and potentially enhance psychosocial and relationship functioning.
Second, as our prior work (Manne et al., 2011) suggested that distressed patients and spouses benefitted from IET, we targeted couples in which one or both partners reported elevated cancer-specific distress. Third, we enhanced IET by focusing on cancer-related concerns that patients and spouses identified in the first session. This was added because patients endorsing more concerns benefited more from IET (Manne et al., 2011). In addition, by targeting concerns, we could better tailor IET to the issues causing distress. Third, to bolster intervention effects, a phone booster session was added 3 weeks after the last session. Fourth, we evaluated three pre-intervention factors, relationship duration, relationship satisfaction, and patient traditional masculinity, as novel moderators for IET’s intervention effects.
Our primary aim was to evaluate the impact of IET versus GHW and usual care (UC) on the primary outcomes of patient and spouse general psychological adjustment, depression, cancer-specific distress, cancer-related concerns, and relationship satisfaction. We hypothesized that couples who were randomized to IET would report higher general psychological adjustment and relationship satisfaction and lower cancer-specific distress and concerns compared with those enrolled in GHW and UC. Our secondary aim was to evaluate the moderating role of pre-intervention characteristics on treatment response to IET, specifically relationship satisfaction, relationship duration, and the patient’s endorsement of traditional masculine norms. Based on the prior literature (Halford et al., 2017; Lyons et al., 2016; Manne et al., 2011; Menichetti et al., 2016; Winters-Stone et al., 2016), we predicted that couples reporting lower pre-intervention relationship satisfaction would respond more favourably to IET. Based on marital therapy research suggesting that longer-married couples gain more from treatment, we proposed that IET would have stronger effects on couples in relationships of a longer duration (Atkins et al., 2005; Baucom, Atkins, Rowe, Doss, & Christensen, 2015). Finally, side effects of prostate cancer treatments may threaten masculine self-image (Maliski, Rivera, Connor, Lopez, & Litwin, 2008), and men who endorse traditional masculinity endorse more distress (Helgeson & Lepore, 1997; Hoyt & Stanton, 2011). Men endorsing traditional masculinity are less likely to process/understand their emotional reactions to prostate cancer (Hoyt, Stanton, Irwin, & Thomas, 2013). Therefore, we hypothesized that men with higher endorsement of traditional masculinity would respond more favourably to IET because the intervention facilitates processing their reactions.
Method
Participants
Men diagnosed with localized prostate cancer and their partners were recruited from five cancer centres in the Northeastern United States (Memorial Sloan-Kettering, Fox Chase, University of Pennsylvania, Lurie Cancer Center, and Rutgers) and three community hospital settings (Garden State Urology, Newark University Hospital, Hackensack/Meridian Health System). Eligibility criteria included (1) treatment for non-metastatic prostate cancer within the last 18 months; (2) Eastern Cooperative Oncology Group (Oken et al., 1982) performance status score of 0 or 1; (3) cohabitating for a year or more with a significant other of either gender; (4) either patient or spouse had elevated cancer-specific distress reflected by a score at recruitment ≥16 (patient) or ≥17 (spouse) on the Impact of Events Scale (IES (Horowitz, Wilner, & Alvarez, 1979); (5) ≥18 years of age (Manne et al., 2011); (6) no self-reported hearing impairment; and (7) lived within a one-hour commuting distance of the centre. The study was approved by each site’s Institutional Review Board.
A total of 2,834 patients and/or spouses were screened (Figure 1) for cancer-specific distress using the procedures described below. Of these, 1,561 couples (55%) were eligible, of whom 1,324 refused (84.6%) and 237 (15.2%) consented and completed the baseline survey. Comparisons were made between patient participants and refusers on available data (i.e., age, site, race, stage, Gleason score, performance status, time since treatment initiation). Participants were more likely to consent at one site (Lurie Cancer Center; 30.3%) than other sites (χ2 = 15.4, p < .01), but the enrolment there was low (N = 10).
Figure 1.
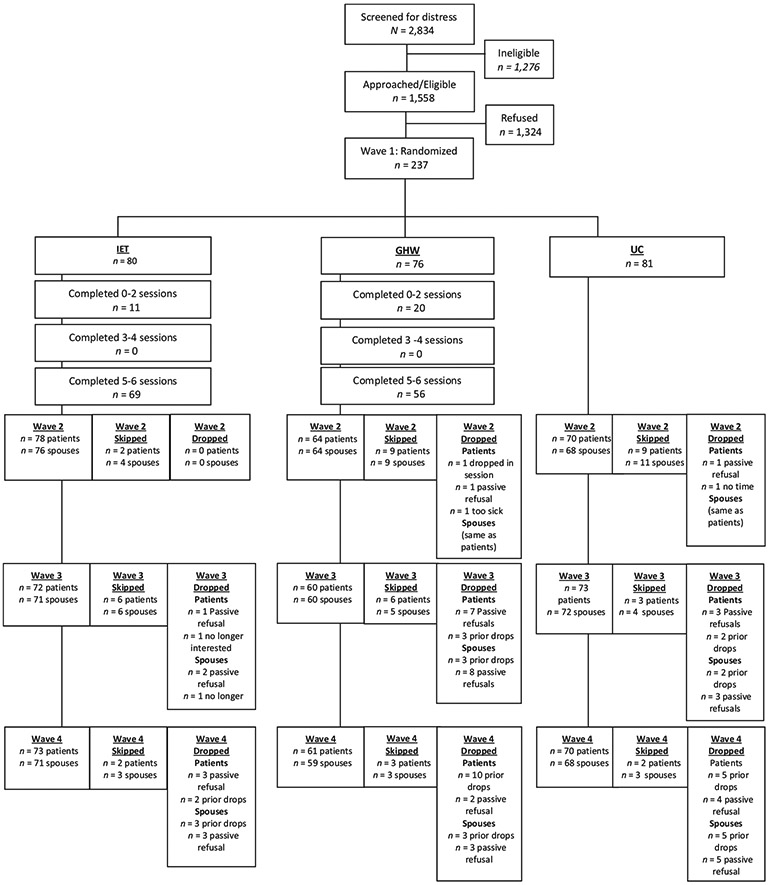
Study CONSORT.
Procedures
Participants were approached in person in clinic. Those not seen in clinic were sent letters about the study and contacted by phone. During this contact, patients were administered the IES (Horowitz et al., 1979) as a screener. If the patient met screening eligibility, the couple was invited to participate. If the patient did not meet screening eligibility, the spouse was contacted and screened, if possible. If the spouse was eligible, the couple was invited to participate. If interested, an informed consent form and the questionnaire were provided to return by mail. If the consent and survey were not returned within 2 weeks, couples were contacted. If the material was not returned after 3 months, the couple was considered a refuser. After consents and surveys were received, couples were randomly assigned to IET, GHW, or UC. Randomization was stratified on the patient’s baseline IES score. The cut-off for high distress was M > 21 (Manne et al., 2011). The study was registered with clinicaltrials.gov (NCT01982058). The four assessment time points were pre-intervention (baseline/Wave 1), 5 weeks post-baseline (Wave 2), 3 months post-baseline (Wave 3), and 6 months post-baseline (Wave 4).
Interventions
IET and GHW consisted of five 90-min audio-recorded couples’ sessions and one 30–45 min booster call. Both interventions were manualized and are available upon request. IEC content focused on improving couples’ ability to share thoughts and feelings regarding cancer, promote mutual understanding and support, facilitate constructive discussion of cancer concerns, and to enhance emotional intimacy. GHW’s focus was on a healthy lifestyle. The first three sessions focused on dietary assessment, setting goals, adopting a plant-based diet using the American Institute of Cancer Research guidelines (American Institute for Cancer Research, 2017), and relaxations. The last two in-person sessions focused on education about and increasing regular activity. A description of both interventions is in Table S1. In UC, participants received standard care, which was similar at all sites. If indicated, a referral to a psychiatrist/psychologist was provided for patient or couple at each site.
Interventionists and supervision
Intimacy-enhancing therapy interventionists were psychologists or social workers. GHW interventionists were certified nutritionists or personal trainers. Both IET and GHW interventionists underwent 6–7 hr of training in the assigned manual-based intervention. Supervision was provided after each session by one of three study investigators or a certified nutritionist. Supervisors completed fidelity checklists and provided feedback.
Outcome measures (all waves)
Higher scores indicate greater levels of the assessed construct.
General psychological adjustment
The Mental Health Inventory-38 (Veit & Ware, 1983) is a 38-item measure assessing distress and well-being. The scale has been used in prior studies of cancer patients and their spouses (Manne, Badr, & Kashy, 2012). Coefficient alpha was .96–.97 for patients and spouses across waves.
Depression
The Patient Health Questionnaire-9 (PHQ-9) is the 9-item depression module from the full PHQ (Kroenke, Spitzer, & Williams, 2001; Spitzer, Williams, Kroenke, Hornyak, & McMurray, 2000). It has been widely used to assess depressive symptoms in cancer patients (Hinz et al., 2016; Martin, Rief, Klaiberg, & Braehler, 2006) and has cut-offs for mild (0–9), moderate (10–14), and severe depression (15–27). Coefficient alpha = .80–.87 across waves.
Cancer-specific distress
Patients and spouses completed the Impact of Events Scale (Horowitz et al., 1979), a 15-item scale measuring the severity of intrusive thoughts, worries, and feelings about having (or one’s spouse having) cancer, avoidance, and numbing. Coefficient alpha across waves was .93–.94.
Cancer-related concerns
Patients and spouses rated the degree to which they were concerned about ten cancer-related problems (e.g., the couples’ sexual relationship, fear of disease progression, finances) (Manne et al., 2010). Ratings ranged from 1 = not at all concerned to 5 = extremely concerned. Items were averaged within each partner for analyses. Coefficient alpha across waves was .83–.87.
Relationship satisfaction
Patients and spouses completed the 32-item Dyadic Adjustment Scale (DAS), which is a widely used measure of relationship satisfaction (Spanier & Filsinger, 1983). Scores range from 0 to 151, and scores below 97 indicate relationship distress. Coefficient alpha across waves was .93–.95.
Moderators (Wave 1 only)
Baseline relationship satisfaction
The DAS, as described above.
Relationship duration
Both partners reported the number of years married or cohabiting. For the moderator analysis, patient report was used.
Conformity to masculine norms (patient only)
The 22-item Conformity to Masculine Norms Inventory (Burns & Mahalik, 2008; Mahalik, Good, & Englar-Carlson, 2003; Mahalik, Locke, et al., 2003) assessed the degree of conformity to actions, thoughts, and feelings in the dominant culture. Items assess the importance of winning, emotional control, risk-taking, dominance, self-reliance, power over women, and toughness. Coefficient alpha was .69.
Covariates
Demographic information
Age (in years), education (‘How far did you go in school?’, 1 = 1–4 years, 2 = 5–8 years, 3 = some high school, 4 = finished high school, 5 = 1–3 years of college, 6 = 4 years of college, 7 = trade or business school, 8 = some graduate school, 9 = graduate degree) ethnicity (White, Black, Asian, Hispanic, Native American, Other), income [‘Please estimate your annual household income (before taxes) to the nearest thousand’] and relationship length (‘How long have you and your partner been married?’) were collected.
Medical information
Time since diagnosis, receipt of psychological care (other than IEC or GHW), erectile function, and bowel function were collected. Patients completed the bowel function (IIEF-BF) and the Erectile Function Domain subscale of the International Inventory of Erectile Function (IIEF-ED) (Rosen et al., 1997). Coefficient alpha was .67 for the Bowel Function scale and .95 for the Erectile Function scale.
Treatment fidelity and evaluation
Fidelity
Three out of each couple’s five sessions were randomly selected for fidelity rating. Criteria were topics covered, exercises conducted, and whether home assignments were given.
Evaluation
A scale adapted from Borkovec and Nau (1972) was administered at Wave 3. Fourteen items assessed session helpfulness and importance. The percentage of home assignments completed was collected.
Analytic approach
Multilevel modelling (MLM; SPSS version 24) with REML was used to test for mean differences as a function of time, treatment (IET, GHW, or UC), and role (i.e., patient vs. spouse), and models included all main effects and interactions among these variables. Covariates included all analyses were whether the patient had surgery (1 = yes, −1 = no), ethnicity (i.e., 1 = White/not Hispanic, −1 = otherwise), the person’s age, time since most recent treatment in months, and Gleason score (all grand-mean-centred). Models included correlated random intercepts and correlated residuals for patients and spouses. In addition to being able to model the interdependence between patients and spouses, the MLM approach does not delete participants with missing data at some time points, which is a disadvantage of a more traditional ANOVA approach. Thus, this analysis utilizes all available data with the implicit assumption that missing data are missing at random.
To test whether moderators qualified the treatment effects, we simplified the analysis by treating time as a quantitative variable measured in months since the baseline and then grand-mean-centred. The models included a categorical variable to denote treatment condition as well as an effect coded variable to specify role. Two of the proposed moderator variables, relationship length and masculinity, are dyad-level variables in that each dyad has only one score. To examine these moderators, each model included the moderator, condition, role, and time in months and their interactions. The final moderator variable, baseline relationship satisfaction, was assessed for both patients and spouses, and so we used an actor–partner interdependence model (APIM) (Kenny, Kashy, & Cook, 2006) framework. That is, both the person’s own relationship satisfaction and the partner’s satisfaction were included as moderators. Thus, the moderation model included condition, role, time in months, and both actor and partner values for relationship satisfaction. All main effects and interactions between these variables were included in the models with the exception that we did not specify actor-moderator by partner–moderator interactions. Moderation analyses included the same covariates and random effects used in the primary analyses. Significant interactions were followed by simple slopes analyses at one standard deviation above and below the mean for the moderator. Because we focused on whether the variable moderated treatment effects, we discuss results only for interactions involving both the moderator and the treatment.
Results
Descriptive information
Descriptive information is presented in Table 1. The mean age of patients and spouses respectively was 61 and 57 years. Most participants were White, had completed a college degree or higher education, and were married, and the average relationship length was more than 27 years. The average time since cancer treatment was initiated was approximately 5 months, and most patients underwent surgery as their treatment. Approximately 13% had high risk disease (more likely to show cancer progression; Gleason score > 8). Eighty per cent of men reported moderate-to-severe ED on the IIEF. Fourteen per cent of patients and 15.3% of spouses were maritally distressed at Wave 1. For severity of depression, 11.8% of patients and 10.2% of spouses scored in the moderate-to-severe range. On the basis of Horowitz et al.’s (1979) and Zilberg, Weiss, and Horowitz (1982) IES categorization, 49% of patients and 52% of spouses had a significant stress response.
Table 1.
Characteristics of the Study Sample
| Variable | Full sample (N = 237) |
IET (N = 80) |
GHW (N = 76) |
UC (N = 81) |
||||
|---|---|---|---|---|---|---|---|---|
| Patient N (%) |
Spouse N (%) |
Patient N (%) |
Spouse N (%) |
Patient N (%) |
Spouse N (%) |
Patient N (%) |
Spouse N (%) |
|
| Age (years)a | 60.6 (7.3) | 57.1 (8.5) | 60.5 (6.9) | 58.1 (7.7) | 60.0 (7.4) | 55.6 (9.5) | 61.2 (7.6) | 57.5 (8.2) |
| Gender | ||||||||
| Male | 237 (100) | 2 (0.8) | 80 (100) | 1 (1.3) | 76 (100) | 0 (0) | 81 (100) | 1 (1.2) |
| Female | 0 (0) | 235 (99.2) | 0 (0) | 79 (98.7) | 0 (0) | 76 (100) | 0 (0) | 80 (98.8) |
| Race | ||||||||
| White | 179 (75.5) | 176 (74.3) | 60 (75.0) | 60 (75.0) | 57 (75) | 57 (76.0) | 62 (76.5) | 59 (72.8) |
| Black | 47 (19.8) | 46 (19.4) | 15 (18.8) | 14 (17.5) | 15 (19.7) | 15 (19.7) | 17 (21.0) | 17 (21.0) |
| Asian | 1 (0.4) | 4 (1.7) | 0 (0) | 1 (1.3) | 0 (0) | 2 (2.6) | 1 (1.2) | 1 (1.2) |
| Hispanic | 4 (1.7) | 7 (3.0) | 1 (1.3) | 4 (5.0) | 2 (2.6) | 2 (2.6) | 1 (1.2) | 1 (1.2) |
| Other | 5 (2.1) | 2 (0.8) | 3 (3.8) | 1 (1.3) | 2 (2.6) | 0 (0) | 0 (0) | 1 (1.2) |
| Missing | 1 (0.4) | 2 (0.8) | 1 (1.3) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 2 (2.5) |
| Employment | ||||||||
| On leave/not employed | 9 (3.8) | 17 (7.2) | 4 (5.1) | 7 (8.8) | 4 (5.2) | 5 (6.5) | 1 (1.2) | 5 (6.2) |
| Part-time | 18 (7.6) | 38 (16.0) | 7 (8.8) | 10 (12.5) | 7 (9.2) | 20 (26.3) | 4 (4.9) | 8 (9.9) |
| Full-time | 144 (60.8) | 108 (45.6) | 42 (52.5) | 35 (43.8) | 48 (63.2) | 31 (40.8) | 54 (66.7) | 42 (51.9) |
| Retired | 56 (23.6) | 62 (26.2) | 25 (31.3) | 26 (32.5) | 14 (18.4) | 17 (22.4) | 17 (21.0) | 19 (23.5) |
| Missing | 10 (4.2) | 12 (5.1) | 2 (2.5) | 2 (2.5) | 3 (3.9) | 3 (3.9) | 5 (6.32 | 7 (8.6) |
| Education | ||||||||
| ≤HS | 24 (10.2) | 38 (16.0) | 8 (10.0) | 14 (17.5) | 9 (11.8) | 10 (13.1) | 7 (8.8) | 14 (17.2) |
| Some college | 39 (16.5) | 49 (20.7) | 18 (22.5) | 21 (26.3) | 10 (13.2) | 16 (21.1) | 11 (13.6) | 12 (14.8) |
| College degree | 62 (26.2) | 52 (21.9) | 21 (26.3) | 12 (15.0) | 26 (34.2) | 19 (25.0) | 15 (18.5) | 21 (25.9) |
| >College | 112 (47.3) | 96 (40.5) | 33 (41.3) | 33 (41.3) | 31 (40.7) | 31 (40.8) | 48 (59.2) | 32 (39.5) |
| Missing | 0 (0) | 2 (0.9) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 2 (2.5) |
| Income ($)a | 147,000 | 147,000 | 130,000 | 147,000 | 130,000 | $120,000 | 150,000 | 150,000 |
| Rel. lengthb | 27.3 (13.3) | 27.0 (13.3) | 28.4 (12.9) | 28.3 (13.0) | 26.3 (13.8) | 26.0 (13.9) | 27.1 (13.3) | 26.7 (13.0) |
| Gleason Score | ||||||||
| 6 | 47 (19.8) | 19 (23.8) | 12 (15.8) | 16 (19.8) | ||||
| 7 | 160 (67.5) | 50 (62.5) | 54 (71.1) | 56 (69.1) | ||||
| 8 | 15 (6.3) | 8 (10.0) | 5 (6.6) | 2 (2.5) | ||||
| 9 | 15 (6.3) | 3 (3.8) | 5 (6.6) | 7 (8.6) | ||||
| Missing data | 0 (0) | 0 (0) | 0 (0) | 0 (0) | ||||
| Cancer stage | ||||||||
| 1 | 14 (5.9) | 5 (6.3) | 4 (5.3) | 5 (6.2) | ||||
| 2A | 31 (13.1) | 13 (16.3) | 7 (9.3) | 11 (13.6) | ||||
| 2B | 130 (54.9) | 44 (55.0) | 43 (56.6) | 42 (53.1) | ||||
| 3 | 62 (26.2) | 18 (22.5) | 22 (28.9) | 21 (27.2) | ||||
| Treatment | ||||||||
| Surgery only | 200 (84.4) | 66 (82.5) | 66 (86.8) | 68 (84.0) | ||||
| Radiation only | 15 (6.3) | 6 (7.5) | 2 (2.5) | 7 (8.6) | ||||
| Radiation and Hormone Rx | 10 (4.2) | 6 (7.5) | 2 (2.6) | 2 (2.5) | ||||
| Radiation, Surgery, and Hormone Rx | 2 (0.8) | 1 (1.3) | 1 (1.3) | 0 (0) | ||||
| Surgery and Hormone Rx | 8 (3.4) | 0 (0) | 4 (5.3) | 4 (4.9) | ||||
| Surgery and Radiation | 2 (0.8) | 1 (1.3) | 1 (1.3) | 0 (0) | ||||
| Time since Rx initiation (days) | 143.4 (95.3) | 136.5 (86.0) | 159.1 (110.7) | 135.6 (87.6) | ||||
| Study Site | ||||||||
| CINJ or affiliate | 46 (19.3) | 17 (21.4) | 14 (18.4) | 15 (18.4) | ||||
| FCCC | 22 (9.3) | 11 (13.8) | 3 (3.9) | 8 (9.9) | ||||
| MSKCC | 89 (37.6) | 31 (38.8) | 28 (36.8) | 30 (37.0) | ||||
| Penn | 70 (29.5) | 20 (25.0) | 27 (35.5) | 23 (28.4) | ||||
| Lurie | 10 (4.2) | 1 (1.3) | 4 (5.3) | 5 (6.2) | ||||
Notes. CINJ = Cancer Institute of New Jersey; FCCC = Fox Chase Cancer Center; GHW = general health and wellness intervention; IET = intimacy-enhancing therapy; Lurie = Lurie Comprehensive Cancer Center at Northwestern University; Penn = University of Pennsylvania Abramson Cancer Center; Rx = therapy.
Mean and standard deviation are reported.
Median is reported.
Treatment attendance, fidelity, and evaluation
Eighty-six per cent of IET couples attended five or six sessions, and the average fidelity across sessions was 89.9%. For GHW, 73.6% of couples attended five or six sessions, and average fidelity across sessions was 93.3%. The average patient evaluation of IET was 3.44 (SD = .70) (5 = most favourable rating), and the average spouse rating was 3.77 (SD = .52) (5 = most favourable rating). The average patient rating of GHW was 3.49 (SD = .68), and the average spouse rating was 3.44 (SD = .63). IET and GHW ratings did not differ significantly for patients (d = 0.07) but IET was evaluated more positively than GHW by spouses, t(101) = 2.95, p < .01, d = 0.57. Self-reported average homework completion was high in both conditions (89%–92% for patients and 89%–91% for spouses).
Power calculations
An initial power analysis was conducted using pilot data contrasting IET with UC on a sample of 71 couples to estimate effect sizes (S. L. Manne, Unpublished pilot data). The effect sizes for the primary hypotheses based on the pilot study ranged from d = 0.6 to d = 1.1. Power analyses indicated that the study would have power of .99 with the originally proposed sample size of 469 couples. However, because the number of eligible couples presenting at each site over the study period was lower than expected, the actual sample size included 237 couples. In spite of the lower-than-expected sample size, using an effect size of d = 0.6, power to test the key predictions was above .98. Using a sensitivity analysis, our sample of 237 couples would have 80% power to detect even small effects (e.g., d = 0.20).
Preliminary analyses: baseline differences and covariates
Preliminary MLM analyses were conducted to test whether there were systematic differences in the baseline scores for the outcomes as a function of treatment group, and showed no evidence of significant mean differences as a function of treatment condition (all ps > .15) or the interaction between role and condition (all ps > .058).
Results from models predicting the outcomes as a function of only the covariates are presented in Table S2. This table also includes the dyadic correlations between the patient and caregiver intercepts, which measure similarity in the two partners’ average values, as well as the dyadic correlations between the residuals, which measure unique similarity at the particular measurement occasion. Age was consistently associated with outcomes such that older individuals reported higher psychological adjustment and relationship satisfaction and lower depression, cancer-specific distress, and cancer concerns. The only other covariate that was associated with the outcomes was ethnicity. White, non-Hispanic patients were lower in cancer distress and cancer concerns, and they were higher in relationship satisfaction. The dyadic correlations show small-to-moderate associations between both the intercepts and residuals across partners. The intercept correlations indicate that if one partner is relatively high in average distress or well-being across the study period, the other partner is, as well. The one large intercept correlation is for relationship satisfaction, indicating a strong correspondence between partners’ satisfaction. The residual correlations assess similarity in the time-specific measurements after the intercepts and the effects of the covariates have been removed. As with the intercept correlations, these associations show that if one person is uniquely high in distress (or well-being) at a particular measurement occasion, the other person tends to be higher in distress (or well-being) at that occasion, as well.
Intervention effects
Table 2 presents the estimated marginal means and standard errors for the outcomes as a function of treatment condition (IET, GHW, UC), individual role (patient, spouse), and wave of data collection. Results for general psychological adjustment only showed a significant main effect of time, F(3, 592) = 39.62, p < .001. Post hoc Bonferroni comparisons indicated that psychological adjustment increased significantly from baseline (M = 177.24, SE = 1.26) to Wave 2 (M = 181.15, SE = 1.29, d = −0.25) to Wave 3 (M = 185.25, SE = 1.29, for Wave 2 to Wave 3 d = −0.26), but the difference between Waves 3 and 4 (M = 184.72, SE = 1.30, d = 0.03) was not significant. No other main effects or interactions were statistically significant.
Table 2.
Means and standard errors for general psychological adjustment, depression, cancer-specific distress, cancer concerns, and relationship satisfaction as a function of treatment condition, role, and time
| Outcome | Cond. | Role | Wave 1 M (SE) |
Wave 2 M (SE) |
Wave 3 M (SE) |
Wave 4 M (SE) |
|---|---|---|---|---|---|---|
| Global | IET | Patient | 182.20 (2.70) | 186.06 (2.71) | 190.70 (2.74) | 190.23 (2.73) |
| Spouse | 175.03 (2.76) | 182.94 (2.79) | 186.22 (2.82) | 184.84 (2.83) | ||
| Psychological adjustment | GHW | Patient | 175.72 (2.77) | 177.78 (2.86) | 181.15 (2.88) | 180.43 (2.88) |
| Spouse | 174.82 (2.88) | 179.45 (2.98) | 182.85 (3.00) | 180.77 (3.01) | ||
| UC | Patient | 179.71 (2.69) | 181.22 (2.75) | 184.83 (2.73) | 185.49 (2.75) | |
| Spouse | 175.98 (2.73) | 179.45 (2.81) | 185.74 (2.79) | 186.58 (2.82) | ||
| Depression | IET | Patient | 3.98 (0.44) | 3.14 (0.44) | 3.26 (0.45) | 2.86 (0.45) |
| Spouse | 3.73 (0.44) | 2.86 (0.44) | 2.59 (0.45) | 2.57 (0.45) | ||
| GHW | Patient | 5.35 (0.45) | 4.84 (0.48) | 4.60 (0.48) | 4.43 (0.48) | |
| Spouse | 3.87 (0.46) | 3.20 (0.47) | 3.14 (0.48) | 3.58 (0.48) | ||
| UC | Patient | 4.28 (0.44) | 3.82 (0.45) | 3.68 (0.45) | 3.31 (0.45) | |
| Spouse | 4.06 (0.43) | 3.49 (0.45) | 3.30 (0.44) | 2.94 (0.45) | ||
| Cancer-specific distress | IET | Patient | 23.61 (1.93) | 22.31 (1.94) | 14.39 (1.97) | 14.44 (1.96) |
| Spouse | 25.48 (2.05) | 15.84 (2.07) | 11.50 (2.11) | 11.47 (2.11) | ||
| GHW | Patient | 25.80 (1.98) | 22.61 (2.06) | 16.33 (2.09) | 16.77 (2.08) | |
| Spouse | 25.95 (2.13) | 16.99 (2.22) | 13.36 (2.25) | 14.47 (2.26) | ||
| UC | Patient | 24.40 (1.92) | 19.92 (1.98) | 15.53 (1.96) | 13.11 (1.98) | |
| Spouse | 24.08 (2.01) | 17.21 (2.12) | 13.65 (2.08) | 13.96 (2.12) | ||
| Cancer concerns | IET | Patient | 2.50 (0.09) | 2.28 (0.09) | 2.06 (0.09) | 2.02 (0.09) |
| Spouse | 2.65 (0.09) | 2.33 (0.09) | 2.16 (0.09) | 2.27 (0.09) | ||
| GHW | Patient | 2.61 (0.09) | 2.44 (0.09) | 2.26 (0.09) | 2.24 (0.09) | |
| Spouse | 2.65 (0.09) | 2.51 (0.10) | 2.37 (0.10) | 2.46 (0.10) | ||
| UC | Patient | 2.45 (0.09) | 2.28 (0.09) | 2.12 (0.09) | 2.14 (0.09) | |
| Spouse | 2.52 (0.09) | 2.45 (0.09) | 2.31 (0.09) | 2.22 (0.09) | ||
| Relationship satisfaction | IET | Patient | 117.37 (1.82) | 117.50 (1.83) | 116.52 (1.85) | 116.80 (1.85) |
| Spouse | 112.57 (2.07) | 117.16 (2.08) | 116.94 (2.10) | 115.64 (2.10) | ||
| GHW | Patient | 114.59 (1.88) | 117.00 (1.94) | 116.51 (1.96) | 117.21 (1.95) | |
| Spouse | 115.60 (2.15) | 116.38 (2.21) | 119.10 (2.22) | 116.41 (2.23) | ||
| UC | Patient | 116.70 (1.81) | 116.82 (1.86) | 119.04 (1.85) | 117.77 (1.86) | |
| Spouse | 118.12 (2.04) | 118.83 (2.10) | 118.41 (2.08) | 117.76 (2.10) |
Notes. GHW = general health and wellness intervention; IET = intimacy-enhancing therapy; UC = usual care.
Means and standard errors are computed at the means for the following covariates: surgery, ethnicity/race, age, time since most recent treatment, and Gleason score.
Results for depression showed a significant main effect of time, F(3, 591) = 15.09, p < .001. Post hoc comparisons showed that depression scores dropped significantly from Wave 1 (M = 4.32, SE = 0.20) to the other time points (e.g., Wave 1 vs. Wave 2 d = 0.303), but Wave 2 (M = 3.56, SE = 0.20), Wave 3 (M = 3.43, SE = 0.21), and Wave 4 (M = 3.28, SE = 0.21) did not differ from one another. There was also a role effect for depression severity, F(1, 262) = 5.59, p = .019, d = 0.33, such that patients (M = 3.96, SE = 0.23) had significantly higher depression than spouses (M = 3.28, SE = 0.23).
For cancer distress, there was a main effect of time, F(3, 612) = 97.97, p < .001, and a time by role interaction, F(3, 605) = 5.99, p < .001. The main effect for time indicated that cancer distress dropped from Wave 1 (M = 24.88, SE = 0.87) to Wave 2 (M = 19.15, SE = 0.90, d = 51) to Wave 3 (M = 14.13, SE = 0.90, for Waves 2 to 3 d = 0.45). For Wave 4 (M = 14.04, SE = 0.91), cancer distress did not differ from that for Wave 3, d = 0.01. The time by role interaction reflected the fact that at Wave 2, patients (M = 21.61, SE = 1.16) were significantly more distressed than their spouses (M = 16.68, SE = 1.24), F(1, 451) = 9.64, p = .002, d = 0.29. The differences between patients and partners were not significant at the other three time points (all ps > .10).
Cancer concerns showed significant main effects of time, F(3, 624) = 55.49, p < .001, and role, F(1, 259) = 5.17. Concerns dropped across Waves 1 through 3 (Wave 1 to 2 d = 0.36, Wave 2 to 3 d = 0.34), but did not change from Waves 3 to 4, d = 0.00 (Wave 1: M = 2.56, SE = 0.04, Wave 2: M = 2.38, SE = 0.04, Wave 3: M = 2.21, SE = 0.04, Wave 4:M = 2.21, SE = 0.04). In addition, the role main effect showed that spouses (M = 2.40, SE = 0.04) reported significantly higher levels of concerns than patients (M = 2.28, SE = 0.04, d = 0.36).
Relationship satisfaction revealed a significant main effect of time, F(3, 616) = 4.09, p = .007. Relationship satisfaction was significantly higher at Wave 3 (M = 117.73, SE = 1.02) than it was at Baseline (M = 115.82, SE = 1.00, d = 0.15), but did not differ from Wave 2 (M = 117.28, SE = 1.02, d = 0.04) and Wave 4 (M = 116.93, SE = 1.02, d = 0.06). There was also a significant three-way interaction between time, role, and condition (see Figure 2; F(6, 614) = 2.66, p = .015). The time by role interaction was decomposed into simple main effects for time separately for patients and spouses in each of the three treatment groups. This analysis showed that relationship satisfaction changed over time only for spouses in IET, F(3, 597) = 5.04, p = .002; all other simple main effects ps > .08). A post hoc Bonferroni test indicated that, in IET, spouses’ relationship satisfaction increased significantly from Wave 1 (M = 12.26, SE = 2.38) to Wave 2 (M = 16.88, SE = 2.39, d = 0.22), but did not differ from Waves 2 through 4.
Figure 2.
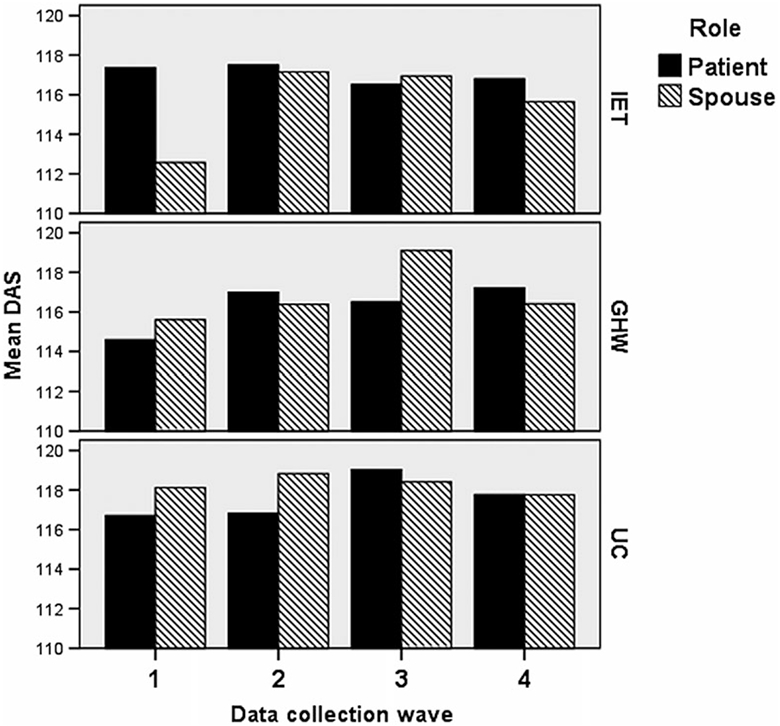
Patient and spouse relationship satisfaction over the four waves of data collection as a function of treatment condition. GHW = general health and wellness intervention; IET = intimacy-enhancing therapy; UC = usual care.
Moderation of intervention effects
As noted in the analysis section, we limit the discussion of moderation to interactions involving both the treatment and the moderator. Moreover, because we conducted analyses for five outcomes combined with three moderators, we report only interactions for which the statistical significance level was below.01. Using that more conservative criterion, two significant interactions involving treatment condition and the moderator emerged.
Interaction involving relationship length and psychological adjustment
There was a significant four-way interaction predicting general psychological adjustment that involved relationship length, F(2, 626) = 7.74, p < .001 (see Figure 3). The three-way interactions between condition, time, and role at low relationship length, F(2, 632) = 3.45, p = .032, and high relationship length, F(2, 612) = 5.22, p = .006, were both statistically significant. Looking at the simple slopes for time separately for patients and spouses in the three conditions, there was an overall pattern of increasing adjustment over time. However, among couples in shorter relationships, this increase was statistically significant for patients in IET, b = 1.26, t(617) = 3.80, p < .001, d = 0.31, and UC, b = 1.34, t(621) = 3.80, p < .001, d = 0.30, but not for patients in GHW, b = 0.40, t(640) = 1.26, p = .206, d = 0.10. Spouses showed significant increases in all three conditions, but the increases in IET, b = 0.93, t(594) = 2.39, p = .017, d = 0.20, were smaller than those in GHW, b = 1.66, t(614) = 5.23, p < .001, d = 0.42, or UC, b = 1.71, t(597) = 4.26, p < .001, d = 0.35.
Figure 3.
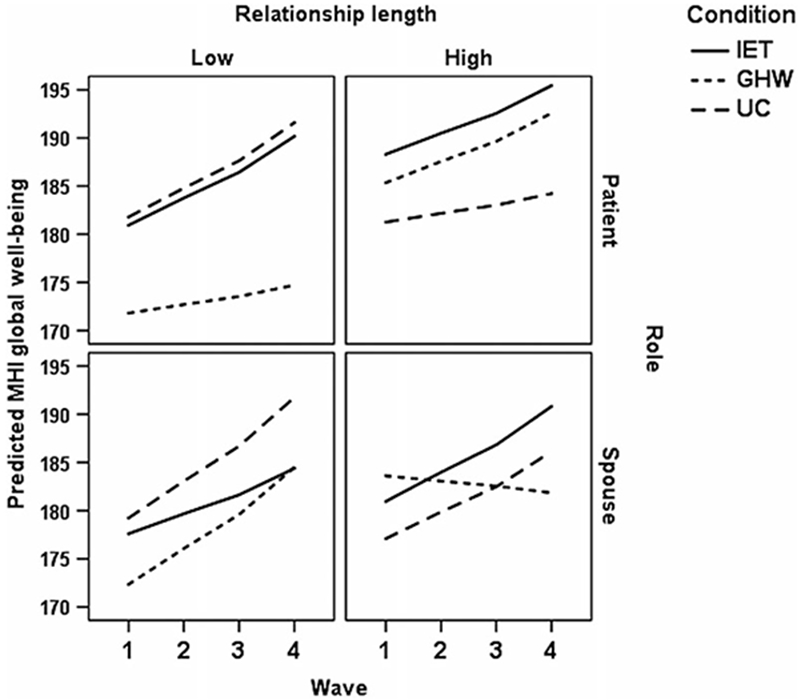
Change in general psychological adjustment over time as a function of relationship length, role, and treatment condition. GHW = general health and wellness intervention; IET = intimacy-enhancing therapy; UC = usual care.
Among couples in longer relationships, patient’s psychological adjustment increased significantly in IET, b = 0.97, t(614) = 3.20, p = .001, d = 0.26, and GHW, b = 0.99, t(630) = 2.62, p = .009, d = 0.21, but not UC, b = 0.40, t(622) = 1.30, p = .195, d = 0.10. For spouses, the increase in psychological adjustment was significant for IET, b = 1.35, t(589) = 3.81, p < .001, d = 0.31, and UC, b = 1.24, t(594) = 3.54, p < .001, d = 0.29. In contrast, although it is not significant, Figure 3 illustrates that spouses enrolled in GHW who were in longer relationships showed slight declines in psychological adjustment over time, b = −.24, t(594) = 0.59, p = .553, d = −0.05.
Interaction involving masculinity and depression
There was one significant interaction involving patient masculinity as the moderator. This interaction between condition, role, and masculinity predicted depression severity, F(2, 225) = 4.83, p = .009 (see Figure 4). When patient masculinity was low, the condition by role interaction was statistically significant, F(2, 227) = 5.52, p = .005. When patient masculinity was high, there was no evidence of a condition by role interaction, F(2, 226) = .65, p = .525. Among patients endorsing lower masculinity, there were significant condition differences for patients, F(2, 221) = 3.47, p = .003, but not for spouses, F(2, 218) = 0.91, p = .403. Patients endorsing low masculinity who were enrolled in GHW reported higher average depression (M = 4.65, SE = 0.68) than patients enrolled in IET (M = 2.65, SE = 0.55, d = 0.36) or UC (M = 2.75, SE = 0.59, d = 0.34).
Figure 4.
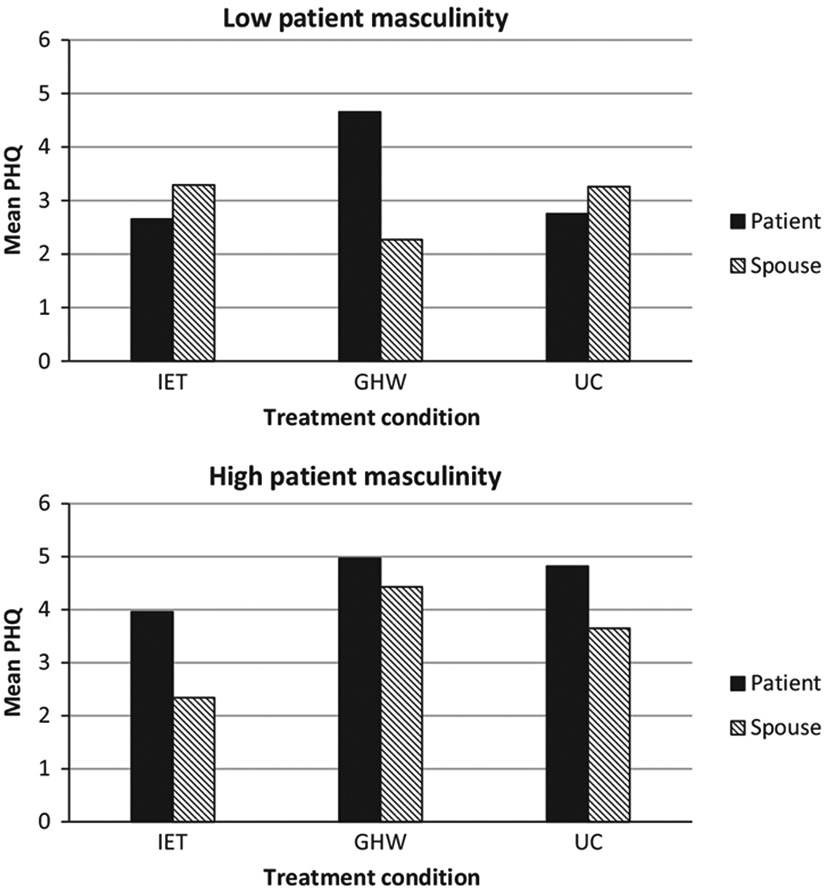
Interaction between patient masculinity, treatment condition, and role predicting depression. GHW = general health and wellness intervention; IET = intimacy-enhancing therapy; UC = usual care.
Discussion
Our study advanced couple-focused intervention research for men with prostate cancer in evaluating two different couple-focused interventions, by examining effects on both partners, by targeting couples where one or both partners evidenced elevated cancer-specific distress at recruitment, and by evaluating novel moderators of treatment effects. Our results provided limited support for the hypothesis that IET would have a stronger impact than UC and GHW across psychological and relationship outcomes. Only one finding was consistent with this prediction: Spouses enrolled in IET showed greater increases in relationship satisfaction, which occurred early in the IET treatment. This finding was, however, primarily due to the fact that spouses enrolled in IET started with lower relationship satisfaction that increased over time, and relationship satisfaction among spouses enrolled in GHW and UC did not change. There were no intervention main effects for either IET or GHW on patients’ relationship satisfaction and no treatment effects on patients’ or spouses’ general psychological adjustment, depression severity, cancer-specific distress, or cancer concerns. Taken together, these findings suggest that IET had limited effects on couples’ distress. Our findings are consistent with other studies evaluating couple-focused interventions for men with prostate cancer, which have either not had a significant main effects for treatment (Canada et al., 2005; Chambers et al., 2015) or reported intervention effects only among spouses (Lyons et al., 2016).
As in our prior work (Manne et al., 2011), treatment response was moderated by pre-intervention factors, and these moderator effects differed for patients and spouses. The findings were complex. Results suggest that for couples in shorter relationships, patients in IET reported an increase in psychological adjustment, whereas patients in GHW did not. However, patients in UC also reported increases in their psychological adjustment over time. For spouses, both GHW and UC were superior to IET. Among couples in longer relationships, patients in IET reported greater increases in psychological adjustment than patients in UC, while patients in GHW reported similar gains. For spouses, psychological adjustment actually declined in GHW, while there were increases in adjustment for IET and UC. In sum, IET was superior to UC only for patients in longer relationships, and GHW was inferior to both IET and UC for spouses.
We hypothesized that IET would be superior to GHW and UC among men endorsing more conformity to masculine norms. Our findings were surprising: Men endorsing low traditional masculine norms enrolled in GHW reported higher average depression than patients enrolled in IET or UC. It is not clear whether this suggests an adverse effect of GHW. One possible explanation is that patients who had high cancer distress were also experiencing ED. Men endorsing lower traditional masculinity may have gained by openly exploring their emotional reactions to ED and changes to their role, body image, and identity (Burns & Mahalik, 2008; Hoyt & Stanton, 2011; Walls, Parahoo, Fleming, & McCaughan, 2010). Since these topics were not discussed in GHW and the majority of patients were distressed and had ED, this treatment may have not have met their needs.
Taken together, our findings indicate that IET was not superior to no treatment or a comparison treatment for the broad range of outcomes evaluated. However, IET was more beneficial than no intervention for patients in longer relationships. Patients in long relationships may be the one setting where the promotion of emotional intimacy has some benefit to offer. Unfortunately, IET was not superior to no treatment for spouses, no matter how long they were in their relationship. GHW was not beneficial for men in shorter relationships and for men who did not endorse traditional masculine norms, and it was associated with declines in adjustment for spouses in longer relationships.
These findings point to the challenge of identifying beneficial couple-focused interventions for prostate cancer patients and their spouses. As has been noted by Nelson and Kenowitz (2013), some aspects of psychological interventions may be helpful for the patient and other aspects may be helpful for the spouse. It is interesting to note that spouses rated IET more positively than GHW, while patients evaluated both treatments equally. Although we targeted our study to patients and/or spouses who were distressed because our prior work indicated that these couples may benefit from IET, distress screening did not contribute to a stronger impact for IET. Given how complex the effects appear to be for couple-focused treatments, it will be important for research to identify what aspects of which interventions result in benefit for both patients and spouses. It will be even more important to identify possible patients and partners who may not benefit from couple-focused psychological treatment.
Further, our results underscore the complexity of intervening with couples coping with prostate cancer. Couples manage the threat of cancer to their relationship, cope with the unique challenges to sexual function and intimacy posed by this disease, process their emotional reactions to cancer, and manage disruptions to personal and relationship plans resulting from prostate cancer. Session audiotapes suggested that couples may have found it challenging and/or uncomfortable to discuss their differing perspectives on the importance of sexual dysfunction (e.g., partners felt it was better to survive and accept ED than focus on its impact, but patients felt ED compromised intimacy).
Strengths and limitations
This study had strong attention to treatment fidelity to ensure that treatments were delivered as intended. Adherence to home assignments was high. Both interventions were evaluated positively by couples. Statistical approaches were sophisticated. The inclusion of a comparison condition was a strength. One weakness was the high study refusal, which raises concerns about the acceptability of a couple-focused intervention in this patient population. Embarrassment or shame about the consequences of prostate cancer may have contributed to the refusal rate. Recruitment into cancer-focused couples’ interventions is a widely recognized challenge (Fredman et al., 2009; Regan, Lambert, & Kelly, 2013). Our sample was comprised primarily of men in heterosexual relationships, relatively well-educated White couples, and patients who underwent surgical treatment. Both interventions may have had a different impact among less educated, non-White couples, and men who underwent radiation therapy. Our screening schema for patients, spouses, and/or couples endorsing high cancer distress may have biased our results. Because couples began the interventions more distressed, the large decline in distress over the first several months seen across groups may have made it more difficult to find a treatment effect. Finally, because of the small sample sizes at some of our study sites, we were not able to evaluate site differences.
Conclusions and implications
Intimacy-enhancing therapy did not result in reductions across a variety of psychological and relationship outcomes, but did show an early impact on relationship satisfaction for spouses. IET was superior to no treatment for men in longer-term relationships. Despite the clear impact of prostate cancer on the marital relationship, before concluding that couple-focused interventions are effective, it will be important to understand what aspects of which couple-focused interventions result in benefit for both patients and spouses, and identify characteristics of patients, partners, and couples who may not benefit from psychological treatments.
Supplementary Material
Table S1. Description of interventions.
Table S2. Multilevel modeling regression coefficients and effect sizes for each of the seven outcomes as a function of the covariates, along with dyadic correlations between the intercepts and dyadic correlations between the residuals.
Statement of contribution.
What is already known on this subject?
Men diagnosed with localized prostate cancer report lower health-related quality of life and both patients and spouses report elevated distress.
Relationship communication plays a role in couples’ psychological adaptation to prostate cancer.
Couple-focused interventions have illustrated an impact on relationship communication.
There are no studies comparing different couple-focused interventions.
What does this study add?
Intimacy-enhancing therapy was not superior to no treatment or a comparison treatment for the broad range of psychological and relationship outcomes.
Intimacy-enhancing therapy was superior to no treatment for patients in longer-term relationship.
The general health and wellness intervention was not beneficial for men in shorter relationships and for men who did not endorse traditional masculine norms.
Footnotes
Conflict of interest
All authors declare no conflict of interest.
Supporting Information
The following supporting information may be found in the online edition of the article:
References
- American Institute for Cancer Research. (2017). Retrieved from http://www.aicr.org. Accessed July 28, 2017.
- Atkins DC, Berns SB, George WH, Doss BD, Gattis K, & Christensen A (2005). Prediction of response to treatment in a randomized clinical trial of marital therapy. Journal of Consulting and Clinical Psychology, 73, 893–903. 10.1037/0022-006X.73.5.893 [DOI] [PubMed] [Google Scholar]
- Badr H, & Taylor CL (2009). Sexual dysfunction and spousal communication in couples coping with prostate cancer. Psycho-Oncology, 18, 735–746. 10.1002/pon.1449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baucom BR, Atkins DC, Rowe LS, Doss BD, & Christensen A (2015). Prediction of treatment response at 5-year follow-up in a randomized clinical trial of behaviorally based couple therapies. Journal of Consulting and Clinical Psychology, 83, 103–114. 10.1037/a0038005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borkovec TD, & Nau SD (1972). Credibility of analogue therapy rationales. Journal of Behavioral Therapy and Experimental Psychiatry, 3, 117–126. 10.1016/0005-7916(72)90045-6 [DOI] [Google Scholar]
- Burnett AL, Aus G, Canby-Hagino ED, Cookson MS, D’ Amico AV, Dmochowski RR, … American Urological Association Prostate Cancer Guideline Update Panel. (2007). Erectile function outcome reporting after clinically localized prostate cancer treatment. Journal of Urology, 78, 597–601. 10.1016/j.juro.2007.03.140 [DOI] [PubMed] [Google Scholar]
- Burns SM, & Mahalik JR (2008). Sexual functioning as a moderator of the relationship between masculinity and men’s adjustment following treatment for prostate cancer. American Journal of Men’s Health, 2(1), 6–16. 10.1177/1557988307304325 [DOI] [PubMed] [Google Scholar]
- Canada A, Neese L, Sui D, & Schover L (2005). Pilot intervention to enhance sexual rehabilitation for couples after treatment for localized prostate carcinoma. Cancer, 104, 2689–2700. 10.1002/cncr.21537 [DOI] [PubMed] [Google Scholar]
- Chambers SK, Occhipinti S, Schover L, Nielsen L, Zajdlewicz L, Clutton S, … Dunn J (2015). A randomised controlled trial of a couples-based sexuality intervention for men with localised prostate cancer and their female partners. Psycho-Oncology, 24, 748–756. 10.1002/pon.3726 [DOI] [PubMed] [Google Scholar]
- Cliff AM, & MacDonagh RP (2000). Psychosocial morbidity in prostate cancer: II. A comparison of patients and partners. BJU International, 86, 834–839. 10.1046/j.1464-410x.2000.00914.x [DOI] [PubMed] [Google Scholar]
- Couper J, Bloch S, Love A, Macvean M, Duchesne GM, & Kissane D (2006). Psychosocial adjustment of female partners of men with prostate cancer: A review of the literature. Psychology-Oncology, 15, 937–953. 10.1002/pon.1031 [DOI] [PubMed] [Google Scholar]
- Eton DT, Lepore SJ, & Helgeson VS (2005). Psychological distress in spouses of men treated for early-stage prostate carcinoma. Cancer, 103, 2412–2418. 10.1002/cncr.21092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredman SJ, Baucom DH, Gremore TM, Castellani AM, Kallman TA, Porter LS, … Carey LA (2009). Quantifying the recruitment challenges with couple-based interventions for cancer: Applications to early-stage breast cancer. Psycho-Oncology, 18, 667–673. 10.1002/pon.1477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gacci M, Simonato A, Masieri L, Gore JL, Lanciotti M, Mantella A, … Carini M (2009). Urinary and sexual outcomes in long-term prostate cancer disease free survivors after radical prostatectomy. Health Quality Life Outcomes, 7, 94. 10.1186/1477-7525-7-94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garos S, Kluck A, & Aronoff D (2007). Prostate cancer patients and their partners: Differences in satisfaction indices and psychological variables. Journal of Sexual Medicine, 4, 1394–1403. 10.1111/j.1743-6109.2007.00545.x [DOI] [PubMed] [Google Scholar]
- Halford W, Rahimullah R, Wilson K, Occhipinti S, Busby D, & Larson J (2017). Four year effects of couple relationship education on low and high satisfaction couples. Journal of Consulting and Clinical Psychology, 85, 495–507. 10.1037/ccp0000181 [DOI] [PubMed] [Google Scholar]
- Harden J, Sanda MG, Wei JT, & Northouse L (2013). Survivorship after prostate cancer treatment: Spouses’ quality of life at 36 months. Oncology Nursing Forum, 40, 567–573. 10.1188/13.ONF.567-573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haun MW, Sklenarova H, Brechtel A, Herzog W, & Hartmann M (2014). Distress in cancer patients and their caregivers and association with the caregivers’ perception of dyadic communication. Oncology Research Treatment, 37, 384–388. 10.1159/000364885 [DOI] [PubMed] [Google Scholar]
- Helgeson VS, & Lepore SJ (1997). Men’s adjustment to prostate cancer: The role of agency and unmitigated agency. Sex Roles, 37, 251–267. 10.1023/A:1025651912128 [DOI] [Google Scholar]
- Hinz A, Mehnert A, Kocalevent RD, Brähler E, Forkmann T, Singer S, & Schulte T (2016). Assessment of depression severity with the PHQ-9 in cancer patients and in the general population. BMC Psychiatry, 16, 22. 10.1186/s12888-016-0728-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz M, Wilner N, & Alvarez W (1979). Impact of event scale: A measure of subjective stress. Psychosomatic Medicine, 41, 209–218. 10.1097/00006842-197905000-00004 [DOI] [PubMed] [Google Scholar]
- Hoyt MA, & Stanton AL (2011). Unmitigated agency, social support, and psychological adjustment in men with cancer. Journal of Personality, 79, 259–276. 10.1111/j.1467-6494.2010.00675.x [DOI] [PubMed] [Google Scholar]
- Hoyt MA, Stanton AL, Irwin MR, & Thomas KS (2013). Cancer-related masculine threat, emotional approach coping, and physical functioning following treatment for prostate cancer. Health Psychology, 32, 66–74. 10.1037/a0030020 [DOI] [PubMed] [Google Scholar]
- Kenny DA, Kashy DA, & Cook WL (2006). Dyadic data analysis. New York, NY: Guilford Press. [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JB (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16, 606–613. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Love AW, Scealy M, Bloch S, Duchesne G, Couper J, Macvean M, … Kissane DW (2008). Psychosocial adjustment in newly diagnosed prostate cancer. Australian and New Zealand Journal of Psychiatry, 42, 423–429. 10.1080/00048670801961081 [DOI] [PubMed] [Google Scholar]
- Lyons KS, Winters-Stone KM, Bennett JA, & Beer TM (2016). The effects of partnered exercise on physical intimacy in couples coping with prostate cancer. Health Psychology, 35, 509–513. 10.1037/hea0000287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahalik JR, Good GE, & Englar-Carlson M (2003). Masculinity scripts, presenting concerns, and help seeking: Implications for practice and training. Professional Psychology: Research and Practice, 34, 123. 10.1037/0735-7028.34.2.123 [DOI] [Google Scholar]
- Mahalik JR, Locke BD, Ludlow LH, Diemer MA, Scott RPJ, Gottfried M, & Freitas G (2003). Development of the conformity to masculine norms inventory. Psychology of Men & Masculinity, 4(1), 3–25. 10.1037/1524-9220.4.1.3 [DOI] [Google Scholar]
- Maliski SL, Rivera S, Connor S, Lopez G, & Litwin MS (2008). Renegotiating masculine identity after prostate cancer treatment. Qualitative Health Research, 18(12), 1609–1620. 10.1177/1049732308326813 [DOI] [PubMed] [Google Scholar]
- Manne S, & Badr H (2008). Intimacy and relationship processes in couples’ psychosocial adaptation to cancer. Cancer, 112, 2541–2555. 10.1002/cncr.23450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manne S, Badr H, & Kashy DA (2012). A longitudinal analysis of intimacy processes and psychological distress among couples coping with head and neck or lung cancers. Journal of Behavioral Medicine, 35, 334–346. 10.1007/s10865-011-9349-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manne S, Badr H, Zaider T, Nelson C, & Kissane D (2010). Cancer-related communication, relationship intimacy, and psychological distress among couples coping with localized prostate cancer. Journal of Cancer Survivorship, 4, 74–85. 10.1007/s11764-009-0109-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manne SL, Kissane DW, Nelson CJ, Mulhall JP, Winkel G, & Zaider T (2011). Intimacy-enhancing psychological intervention for men diagnosed with prostate cancer and their partners: A pilot study. Journal of Sexual Medicine, 8, 1197–1209. 10.1111/j.1743-6109.2010.02163.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manne SL, Kissane D, Zaider T, Kashy D, Lee D, Heckman C, & Virtue SM (2015). Holding back, intimacy, and psychological and relationship outcomes among couples coping with prostate cancer. Journal of Family Psychology, 29, 708–719. 10.1037/fam0000096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin A, Rief W, Klaiberg A, & Braehler E (2006). Validity of the brief patient health questionnaire mood scale in the general population. General Hospital Psychiatry, 28, 71–77. 10.1016/j.genhosppsych.2005.07.003 [DOI] [PubMed] [Google Scholar]
- Menichetti J, Villa S, Magnani T, Avuzzi B, Bosetti D, Marenghi C, … Bellardita L (2016). Lifestyle interventions to improve the quality of life of men with prostate cancer: A systematic review of randomized controlled trials. Critical Reviews in Oncology Hematology, 108, 13–22. 10.1016/j.critrevonc.2016.10.007 [DOI] [PubMed] [Google Scholar]
- Mols F, van de Poll-Franse LV, Vingerhoets AJ, & Essink-Bot ML (2006). Long-term quality of life among Dutch prostate cancer survivors: Results of a population-based study. Cancer, 107, 2186–2196. 10.1002/cncr.22231 [DOI] [PubMed] [Google Scholar]
- Nelson CJ, & Kenowitz J (2013). Communication and intimacy-enhancing interventions for men diagnosed with prostate cancer and their partners. Journal of Sexual Medicine, 10(Suppl 1), 127–132. 10.1111/jsm.12049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Northouse LL, Mood DW, Schafenacker A, Montie JE, Sandler HM, Forman JD, … Kershaw T (2007). Randomized clinical trial of a family intervention for prostate cancer patients and their spouses. Cancer, 110, 2809–2818. 10.1002/cncr.23114 [DOI] [PubMed] [Google Scholar]
- Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, & Carbone PP (1982). Toxicity and response criteria of the Eastern Cooperative Oncology Group. American Journal of Clinical Oncology, 5, 649–655. PMID: 7165009. 10.1097/00000421-198212000-00014 [DOI] [PubMed] [Google Scholar]
- Penson DF, McLerran D, Feng Z, Li L, Albertsen PC, Gilliland FD, … Stanford JL (2005). 5-year urinary and sexual outcomes after radical prostatectomy: Results from the prostate cancer outcomes study. Journal of Urology, 173, 1701–1705. 10.1097/01.ju.0000154637.38262.3a [DOI] [PubMed] [Google Scholar]
- Regan T, Lambert SD, & Kelly B (2013). Uptake and attrition in couple-based interventions for cancer: Perspectives from the literature. Psycho-Oncology, 22, 2639–2647. 10.1002/pon.3342 [DOI] [PubMed] [Google Scholar]
- Rosen R, Riley A, Wagner G, Osterloh I, Kirkpatrick J, & Mishra A (1997). The international index of erectile function (IIEF): A multidimensional scale for assessment of erectile dysfunction. Urology, 49, 822–830. 10.1016/S0090-4295(97)00238-0 [DOI] [PubMed] [Google Scholar]
- Song L, Northouse LL, Zhang L, Braun TM, Cimprich B, Ronis DL, &Mood DW (2012). Study of dyadic communication in couples managing prostate cancer: A longitudinal perspective. Psycho-Oncology, 21, 72–81. 10.1002/pon.1861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spanier GB, & Filsinger EE (1983). Clinical use of the Dyadic Adjustment Scale. In Filsinger EE (Ed.), A sourcebook of marriage and family assessment (pp. 155–168). Beverly Hills, CA: Sage. [Google Scholar]
- Spitzer RL, Williams JB, Kroenke K, Hornyak R, & McMurray J (2000). Validity and utility of the PRIME-MD patient health questionnaire in assessment of 3000 obstetric-gynecologic Patients. American Journal of Obstetrics and Gynecology, 183, 759–769. 10.1067/mob.2000.106580 [DOI] [PubMed] [Google Scholar]
- Trinchieri A, Nicola M, Masini F, & Mangiarotti B (2005). Prospective comprehensive assessment of sexual function after retropubic non nerve sparing radical prostatectomy for localized prostate cancer. Archivio Italiano di Urologia, 77, 219–223. [PubMed] [Google Scholar]
- van Stam MA, van der Poel HG, Bosch JLHR, Tillier CN, Horenblas S, Mols F, & Aaronson NK (2017). Prevalence and correlates of mental health problems in prostate cancer survivors. Urologic Oncology, 35, 531.e1–531.e7. 10.1016/j.urolonc.2017.03.028 [DOI] [PubMed] [Google Scholar]
- Veit CT, & Ware JE Jr (1983). The structure of psychological distress and well-being in general populations. Journal of Consulting and Clinical Psychology, 51, 730–742. 10.1037/0022-006X.51.5.730 [DOI] [PubMed] [Google Scholar]
- Walls P, Parahoo K, Fleming P, & McCaughan E (2010). Issues and considerations when researching sensitive issues with men. Nurse Researcher, 18, 26–34. 10.7748/nr2010.10.18.1.26.c8045 [DOI] [PubMed] [Google Scholar]
- Winters-Stone K, Lyons K, Bennett J, & Beer T (2014). Patterns and predictors of symptom incongruence in couples coping with prostate cancer. Supportive Care in Cancer, 22, 1341–1348. 10.1007/s00520-013-2092-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winters-Stone KM, Lyons KS, Dobek J, Dieckmann NF, Bennett JA, Nail L, & Beer TM (2016). Benefits of partnered strength training for prostate cancer survivors and spouses. Journal of Cancer Survivorship, 10, 633–644. 10.1007/s11764-015-0509-0 [DOI] [PubMed] [Google Scholar]
- Zilberg N, Weiss D, & Horowitz M (1982). Impact of Event Scale: A cross-validation study and empirical evidence supporting a conceptual model of stress response syndromes. Journal of Consulting and Clinical Psychology, 50, 407–414. 10.1192/bjp.180.3.205 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Description of interventions.
Table S2. Multilevel modeling regression coefficients and effect sizes for each of the seven outcomes as a function of the covariates, along with dyadic correlations between the intercepts and dyadic correlations between the residuals.


