Abstract
Objective
To describe the natural history of afferent baroreflex failure (ABF) based on systematic review of clinical and laboratory data in patients with a diagnosis of ABF at Mayo Clinic Rochester.
Methods
We performed a retrospective chart review of all patients who underwent standardized autonomic reflex testing between 2000 and 2020 and had confirmation of the diagnosis of ABF by an autonomic disorders specialist. Patients were identified using a data repository of medical records. Variables included demographic, all-cause mortality, medications, ABF manifestations, comorbidities, and laboratory (autonomic testing, blood pressure monitoring, echocardiogram, brain imaging, plasma catecholamines, serum sodium level, and kidney function tests).
Results
A total of 104 patients with ABF were identified. Head and neck radiation was the most common etiology (86.5%), followed by neck surgery (5.8%) and other causes (7.7%). The most common findings were hypertension (87.5%), fluctuating blood pressure (78.8%), orthostatic hypotension (91.3%), syncope (58.6%), headache (22.1%), and tachycardia (20.2%). Patients commonly received antihypertensives (66.3%), pressor agents (41.3%), or a combination of both (19.2%). The median latency from completion of radiation to ABF was longer compared to the latency in the surgery group (p < 0.0001). Comorbidities, including complications from neck radiation, were frequently seen and all-cause mortality was 39.4% over a 20-year period.
Conclusions
ABF should be suspected in patients with prior head and neck cancer treated by radiation or surgery who present with labile hypertension and orthostatic hypotension. Management may require both antihypertensive and pressor medications. The morbidity and mortality in ABF are high.
The arterial baroreflex is a critical buffering mechanism that prevents acute fluctuation of blood pressure (BP).1 Stretch mechanosensors in each carotid sinus and the aortic arch send information about distention of the vessel walls via glossopharyngeal and vagal nerves, respectively, to a group of specialized nuclei in the medulla (figure 1).1,2 Afferent baroreflex failure (ABF) refers to the clinical syndrome resulting from impairment of the afferent limb of the baroreflex or its central connections at the level of the medulla.3 The main previously described manifestation of ABF is fluctuating hypertension; other manifestations include orthostatic hypotension (OH), episodic tachycardia, and episodes of bradycardia.3 ABF has been described as a complication of neck radiation, neck surgery, trauma of the neck region, brainstem stroke or tumor, and afferent sensory neuropathy; however, no clear etiology can be documented in some patients.3-6
Figure 1. Baroreflex Circuit.
The arterial baroreceptors are stretch mechanoreceptors located in the carotid sinuses (innervated by the glossopharyngeal nerve, IX) and aortic arch (innervated by the vagus nerve, X) that send information about distention of the vessel walls via glossopharyngeal (IX) and vagal (X) nerves (i.e., afferent limb of the baroreflex). Baroreceptor afferents provide monosynaptic excitatory input to the nucleus of the solitary tract (NTS). Through interneurons in the caudal ventrolateral medulla (CVL), neurons in the NTS inhibit sympathetic pacemaker neurons in the rostral ventrolateral medulla inhibiting sympathetic efferent pathway to skeletal muscle and mesenteric and renal vessels. The baroreflex-cardioinhibitory pathway involves a direct input from the NTS to a group of vagal preganglionic neurons located in the nucleus ambiguus (NA). These neurons project to the cardiac ganglion neurons that elicit bradycardia. Therefore, stimulation of the afferent limb of the baroreflex has the double effect of stimulating vagal outflow and attenuating global sympathetic outflow. The baroreflex, via the NTS, also inhibits secretion of arginine vasopressin by magnocellular neurons of the supraoptic (SON) and paraventricular (PVN) nuclei of the hypothalamus, in part by inhibiting noradrenergic cells of the A1 group. The figure is republished and adapted from a review on the arterial baroreflex by Benarroch.2
The diagnosis of ABF is difficult and this condition is likely underrecognized.7 Although ABF can be suggested by a careful history and testing (autonomic testing and ambulatory BP monitoring), the differential diagnosis of ABF is extensive and includes conditions that can produce fluctuating hypertension, tachycardia, and episodic hypotension (e.g., pheochromocytoma and partial autonomic failure).
The pathophysiology, clinical presentation, natural history, and prognosis of ABF are not well understood. We aimed to study the natural history of adult patients with acquired ABF through a retrospective review of patients diagnosed and treated at a large referral center for autonomic disorders.
Methods
Standard Protocol Approvals, Registrations, and Patient Consents
This study was reviewed and approved by the Mayo Clinic institutional review board and included patients who provided consent for use of their medical records for research purposes.
Patients
All patients with a diagnosis of ABF evaluated by an autonomic disorders specialist at Mayo Clinic in Rochester, Minnesota, between January 1, 2000, and September 1, 2020, were identified through an electronic search by 2 of the authors (G.L., M.D.S.) using a search tool and data repository of Mayo Clinic medical records. Three additional patients were identified by one of the authors (G.L.) in the autonomic laboratory. Patients were included in the study if they fulfilled the following inclusion criteria: diagnosis of ABF confirmed by an autonomic disorders specialist based on the clinical presentation with fluctuating hypertension with or without OH or orthostatic tachycardia with or without episodes of bradycardia with otherwise unexplained symptoms suggestive of impaired BP or heart rate regulation; patient age 18–90 years at time of onset of symptoms; and supportive features including a history of head and neck radiation or surgery or head and neck trauma, or standardized autonomic testing with autonomic reflex screen with abnormal baroreflex tests. Patients with a diagnosis not consistent with ABF after review of the history and autonomic evaluation (e.g., alternative diagnoses such as pheochromocytoma, untreated hyperthyroidism, or carcinoid syndrome) were excluded from this study.
Patients were divided into 3 groups. The postradiation group included patients who received head and neck radiation as well as patients who received head and neck radiation and adjuvant neck surgery preceding the onset of ABF. The postsurgery group included patients with a history of neck surgery without head and neck radiation preceding ABF. The “other” group included patients without a history of head and neck radiation or surgery.
Variables
A detailed medical record review was performed by one of the authors (G.L., an autonomic disorders clinical fellow) and included demographic information, all-cause mortality, medications, characteristics of ABF manifestations (hypertension, hypertensive crisis, OH, tachycardia, bradycardia, flushing, headache), date of symptom onset, comorbidities including history of head and neck cancer, history of neck surgery or radiation, date of surgery or radiation, cumulative dose of radiation, radiation-induced complications (dysphagia, radiation-induced plexopathy, cranial neuropathy, vascular stenosis or thrombosis, stroke), and complications of hypertension (chronic heart failure, chronic kidney disease). If the diagnostic accuracy was unclear, quality check was performed by the senior author (W.S.). Hypertension was defined by sustained systolic BP >140 mm Hg or diastolic BP >90 mm Hg (stage 2 hypertension per most recent guidelines),8 that is, documentation of persistent history of hypertension in the medical record. Hypertensive crisis was defined by a sustained increase in systolic BP >180 mm Hg or diastolic BP >120 mm Hg.8 Fluctuating BP was defined as excessive diurnal fluctuation in BP according to the expert clinician (documented history of labile or fluctuating hypertension). Labile BP was confirmed by 24-hour BP monitoring if there were hypertensive surges defined by an abrupt increase in BP >30 mm Hg for more than 2 consecutive measurements or if the test report specified labile hypertension. Orthostatic hypotension was defined by a sustained drop in systolic BP >30 mm Hg during tilt table test from the supine to the standing position or documented sustained drop in systolic BP >20 mm Hg from the supine to the standing position during the office visit, not attributable to medications.9
All patients underwent standardized autonomic function testing with autonomic reflex screen (ARS), which tests postganglionic sudomotor, cardiovagal, and cardiovascular adrenergic functions. The composite autonomic scoring scale (CASS) was derived from ARS.10 CASS is a validated instrument that quantifies the severity and distribution of autonomic failure and is composed of 3 subdomains: sudomotor (score range 0–3), cardiovagal (0–3), and adrenergic (0–4). The total CASS ranges from 0 to 10, with 10 indicating severe autonomic failure. Twenty-four–hour BP monitoring was reviewed and loss of nocturnal fall in BP was defined by obvious blunted or absent nocturnal BP decline according to the clinician. Additional tests reviewed included echocardiogram and brain MRI. The Fazekas scale was calculated by one of the authors (G.L.) in an unblinded fashion and was used to quantify the amount of white matter T2 hyperintense lesions on MRI (0 = normal MRI; 1 = mild punctiform; 2 = moderate with small confluent areas of white matter T2 hyperintensity; 3 = severe with large confluent areas of white matter T2 hyperintensity). Laboratory variables included supine and orthostatic norepinephrine levels (pg/mL) performed as part of plasma catecholamine testing, the serum sodium level, and the serum creatinine and glomerular filtration rate at last follow-up visit.
Statistics
Summary statistics were used to describe demographic and clinical variables including mean (SD), median (interquartile range), and frequency (percentage). Categorical variables were analyzed using χ2 test or Fisher exact test, as appropriate. Continuous variables were compared using Student t test or Wilcoxon rank-sum test, as appropriate. A p value of <0.05 defined statistical significance and 95% confidence intervals (CIs) were reported. Kaplan-Meier estimate was used to assess latency from radiation or surgery to ABF onset and from radiation to plexopathy. When the exact date or month of symptom onset could not be determined, we use the middle of the calendar year. The Pearson correlation coefficient was used to evaluate the relationship between quantitative variables.
Data Availability
Anonymized data will be shared by request from any qualified investigator.
Results
We identified 104 patients (79 men [76.0%]) with ABF (flowchart in figure 2). Patients' characteristics are shown in table 1. The most frequent etiology of ABF was prior head and neck radiation in 90 patients (radiation group). A total of 6 patients had ABF as a direct consequence of neck surgery without a prior history of neck radiation (surgery group). The surgery group included 4 patients with carotid surgeries (unilateral carotid body tumor, bilateral carotid body tumor, bilateral endarterectomy, and unilateral carotid resection following contralateral neck dissection), while 2 patients had other types of neck surgeries (thyroidectomy and parathyroidectomy). In the 3 cases of sequential bilateral surgeries, patients had clinical manifestations of ABF only after the second surgery. Eight patients had no history of neck radiation or surgery prior to the onset of ABF and were classified in the other group. The other group included patients with pure autonomic failure (n = 1), bilateral atherosclerotic carotid disease (n = 2), Takayasu arteritis (n = 1), diabetes (n = 1), neck cancer with high tumor burden without radiation or surgery (n = 1), and in 2 cases the etiology of ABF could not be determined (n = 2). The most common findings were hypertension, OH, syncope, headache, and tachycardia (table 1). Direct complication of labile hypertension was evident in 1 patient who experienced 2 separate episodes of hypertensive encephalopathy secondary to hypertensive crises. Patients commonly received antihypertensives, pressors, or a combination of both (table 1). Documented all-cause mortality in the 3 groups combined was 39.4% over a 20-year period (42% in the radiation group, 17% in the surgery group, and 25% in the other group).
Figure 2. Flowchart of the Search Results and Identification of Patients.
Table 1.
Demographics and Clinical Manifestations

There was no significant difference in age at the time of the first manifestations of ABF between groups (median age 64.0 years in the radiation group, 50.9 years in the surgery group, and 60.6 years in the other group). Patients in the radiation group frequently had significant comorbidities related to prior radiation treatment including dysphagia, hypothyroidism, brachial plexopathy, and cranial neuropathy (table 2). Other comorbidities included stroke, which was seen in all 3 groups, whereas chronic heart failure was only seen in 5 patients in the radiation group and chronic kidney disease was seen predominantly in the other group (table 2). Seven patients in the radiation group had chronic hyponatremia. Most of the patients who underwent brain MRI had mild amount of white matter T2 hyperintense lesions (median Fazekas score 1 [0–1]). History of head and neck cancer was reported in 87 patients in the radiation group; 3 patients had head and neck radiation for other reasons (acne, streptococcal infection with rheumatic fever, and metastatic non-small cell lung cancer). History of head and neck cancer was reported in 5 patients in the surgery group, whereas 1 patient had a history of bilateral endarterectomy. Patients in the radiation group frequently underwent adjuvant surgery (n = 63) or chemotherapy (n = 47) as part of the treatment of the underlying cancer (table 2). Adjuvant surgeries included right-side neck surgeries (n = 17), left-side neck surgeries (n = 17), and bilateral neck surgeries (n = 8), whereas the side of surgery could not be determined in 21 patients. The median latency from suspected baroreceptor injury (radiation or surgery) to clinical ABF varied greatly between groups, with longer latency in the radiation group compared to the surgery group (mean latencies 10.6 years and 0.3 years, respectively; mean difference 10.3 years, 95% CI 8.0–12.5; p < 0.0001; figure 3). There was no correlation between latency of ABF manifestations and age, cumulative dose of radiation, or length of radiation. Latency of ABF was not different between patients who underwent radiation alone and patients who underwent neck radiation with adjuvant neck surgery (mean latencies 12.6 years and 9.8 years, respectively; mean difference 2.8 years, 95% CI –2.7 to 8.4; p = 0.3).
Table 2.
Characteristics of the Different Subgroups

Figure 3. Probability of Freedom From Symptoms in the Radiation and Surgery Groups.

The latency from suspected injury of the baroreceptors or afferent glossopharyngeal and vagal nerves to clinical afferent baroreflex failure (ABF) was longer in the radiation group (solid line) compared to the surgery group (dotted line) (p < 0.0001). The latency to develop symptoms of radiation-induced brachial plexopathy (dashed line) did not differ from the latency to develop radiation-induced ABF among the same patients (p = 0.5).
A total of 18 patients had both radiation-induced ABF and radiation-induced brachial plexopathy. The median latency to develop ABF was not different from the latency to develop symptoms of brachial plexopathy in this subgroup (mean latencies 7.9 years and 6.8 years, respectively; mean difference 1.1 year, 95% CI −2.1 to 4.4; p = 0.5; figure 3). There was a nonsignificant weak association between individual latencies of radiation-induced ABF and radiation-induced brachial plexopathy (R = 0.4, p = 0.14).
Standardized autonomic function testing was performed in all patients and demonstrated evidence of severe autonomic impairment with a median total CASS score of 7. The median CASS sudomotor, cardiovagal, and adrenergic scores were 0, 2, and 4, respectively, and OH was seen in 81 patients (77.9%) during head-up tilt (table 3). Twenty-four–hour BP monitoring was obtained in 89 patients and demonstrated hypertension, OH, hypertensive surge, and absence of nocturnal fall in BP in most patients (table 3). Plasma norepinephrine was elevated in the supine position and surged further upon standing (table 3).
Table 3.
Results of Imaging, Laboratory, and Autonomic Testing

Discussion
This study shows that patients with ABF frequently present with fluctuating hypertension, OH, episodic tachycardia, and headache. The most common cause of ABF is prior radiation therapy for cancers of the neck, which may damage baroreceptors or afferent baroreflex neurons. The pathophysiology remains elusive, however, with differences in symptom onset latencies suggesting different mechanisms of injury in ABF due to surgery and radiation. This study is the largest series of patients with ABF reported to date and provides important insight into morbidity and mortality associated with ABF.
In most patients, the mechanism that led to afferent baroreflex impairment is suggested by the history and the most common cause of ABF is extensive neck surgery or radiation for cancers of the neck. Other reported etiologies of acquired ABF include neck trauma, brainstem stroke or tumor, and Guillain-Barré syndrome.1 We report cases of ABF attributable to other etiologies, suggesting that ABF may be underrecognized. Impairment of baroreflex function has been demonstrated with bilateral carotid artery atherosclerosis with advanced disease and circumferential involvement of the vessel wall.11-13 The current study confirms that ABF can be seen with bilateral carotid atherosclerosis. Studies have suggested that treatment with endarterectomy or stenting does not improve baroreflex function, which in cases of endarterectomy may be due to irreversible damage or the trauma caused by the intervention itself.14-16 ABF might also reflect selective neuropathies or neurodegenerative disorders with focal pathology (e.g., Lewy bodies) in brainstem nuclei involved in central integration of the baroreceptor input.
Labile hypertension, either constant or episodic with hypertensive surges, is the hallmark of ABF and this finding is reported in the majority of patients.17,18 The degree of hypertension has been found to be different between the acute and chronic phase of ABF, with very high BP during the acute phase.5 Other commonly reported symptoms include OH, episodic tachycardia, headache, and flushing, whereas bradycardia is a rare manifestation of ABF sometimes associated with severe hypotension (malignant vagotonia).19 Previous studies have reported that OH is not seen in the majority of patients with ABF, which was hypothesized to relate to sparing of the cardiopulmonary stretch receptors or vestibulo-sympathetic responses bypassing the afferent baroreflex limb.3,5,20,21 Nevertheless, close to 80% of the patients included in the current study had sustained OH confirmed by tilt table testing, suggesting that this manifestation of ABF might be underrecognized or that most patients with ABF eventually develop OH. The presence of OH complicates the management, as it can be severe and disabling, frequently leading to syncope.5 The pathophysiology of postural hypotension in ABF is poorly understood, but conceivably is the result of inefficient baroreflex unloading, which is further supported by increased BP recovery time following the Valsalva maneuver. Hypovolemia due to pressor diuresis and presumed hypersensitivity to short-acting sympatholytic drugs commonly used to treat hypertension may be contributing factors.20
The prognosis in patients with ABF is poor, with high mortality and morbidity. The retrospective design of the current study prevents us from inferring causality between ABF and mortality; however, it has been speculated that death could occur unexpectedly at night due to sleep-disordered breathing and cardiovascular instability, similar to patients with familial dysautonomia.22 Another potential cause of mortality in these patients is aspiration-related lung disease secondary to chronic dysphagia; evidence of bronchiectasis on chest CT imaging has been reported in one study.18 The current study confirms that the majority of patients with acquired ABF experienced direct complications from prior neck surgery or radiation. There is a lack of available data on long-term complications of labile hypertension, defined as recurrent and substantial transient elevations in BP. Ischemic stroke was frequently seen and could be attributable to several risk factors such as chronic hypertension, age, diabetes, and radiation of the neck causing vasculopathy. Radiation injures the vascular endothelium and the vasa vasorum, which leads to fibrosis and accelerates the process of atherosclerosis.23 Hyponatremia secondary to inappropriate antidiuretic hormone secretion has been reported in a patient with ABF possibly from the interruption of inhibitory signal from baroreceptors required for normal antidiuretic hormone regulation.24 Chronic end organ damage to the heart and kidneys was relatively infrequent in the present study, possibly reflecting different overall cardiovascular risk compared to primary hypertension. Further prospective studies should investigate the cardiovascular complications of ABF.
The onset of ABF is often abrupt soon after neck surgery due to direct injury of the baroreceptors during the surgical procedure, whereas a delayed onset is observed in patients who undergo radiation therapy of the neck. The shorter latency in the surgery group may be due to direct injury of the baroreceptors located in the carotid sinuses. Neck dissection with removal of lymph nodes was the most frequent surgery performed in the radiation group and longer latency observed in this group may be related to sparing of the baroreceptors during the adjuvant surgical procedure. The pathophysiology of radiation-induced tissue damage is a dynamic and progressive process involving oxidative stress, chronic inflammation, fibrosis, and microvascular changes with ischemia.25,26 Fibrosis of the carotid arterial walls may lead to “stiffening” of the baroreceptors and disrupt baroreflex regulation.27 Radiation-induced brachial plexopathy may provide some insights into the pathogenesis of radiation-induced ABF. Indeed, latency of radiation-induced plexopathy is usually delayed by several years and symptoms are progressive; however, the clinical presentation and latency from prior radiation vary greatly between individuals.28,29 Prior neck dissection, concurrent chemotherapy, and radiation maximum dose are reported risk factors for the development of brachial plexus symptoms after radiation.28,30 The retrospective design and limited power of the current study did not allow identification of specific risk factors for the development of radiation-induced ABF. Patients with acquired baroreflex lesions attributable to radiation also had surgery or chemotherapy that could have contributed to the damage of the baroreceptors or afferent sensory nerves. The reasons for the susceptibility of some patients to develop radiation-induced ABF are poorly understood. In our experience, ABF is a rare condition and the majority of patients who undergo neck radiation do not develop ABF. Studies including patients with radiation-induced ABF and controls who received the same dose of neck radiation would be helpful to shed light on the pathogenesis of ABF.
The diagnosis of ABF relies heavily on accurate history and autonomic testing. Classically, autonomic testing demonstrates selective involvement of the afferent limb of the baroreflex pathway, whereas the efferent pathway and chemoreflex functions are spared.31 Pharmacologic challenges with phenylephrine and sodium nitroprusside demonstrating exaggerated BP responses but lack of the appropriate reciprocal changes in heart rate and sympathetic nerve activity can confirm the diagnosis of ABF.3,20 Similarly, a lack of increase in plasma vasopressin in response to hypotension is characteristic of impaired afferent baroreflex signal and has been shown in patients with familial dysautonomia and acquired ABF.4,18 Baroreflex patients also exhibit a normal or exaggerated pressor response to physiologic (cold pressor or handgrip test) or psychological (mental arithmetic) stimuli.5 Standardized autonomic testing was available in all the patients included in the current study and the results confirm cardiovagal and adrenergic impairment while sudomotor function is most often normal. The mechanism of high supine plasma norepinephrine that surges further upon standing in the setting of ABF is poorly understood but in line with previous studies that have also reported normal to high plasma norepinephrine in these patients.3,27 High supine norepinephrine might be secondary to ABF with dysregulation and inappropriate stimulation of sympathetic postganglionic nerves. Higher orthostatic norepinephrine may reflect the effects of residual baroreflex function, central commands, and the vestibulo-sympathetic reflex with activation of sympathetic postganglionic neurons in the standing position.32
ABF is one of the most challenging autonomic disorders to manage. Patients often require antihypertensive or pressor medications, as seen in the majority of the patients in this study. For labile hypertension, it is recommended not to chase the BP and long-acting sympatholytic agents such as clonidine are the mainstay of treatment to attenuate sympathetic surge.20 Vasodilators can elicit profound hypotension and diuretics should be avoided. Because the hypertension is often driven by central inputs and stress, benzodiazepine can be useful when taken as needed to reduce BP.20 Patients should be aware that medications that modify vascular tone or sympathetic activity can have a drastic effect on the BP, precipitating hypertensive crisis or hypotension. α1 Agonists such as midodrine or norepinephrine precursors such as droxidopa should be used with caution to treat postural hypotension as they can precipitate severe hypertension. Carbidopa can reduce the BP in patients with familial dysautonomia and this approach may prove useful in treating patients with acquired ABF.33 Further research is needed to validate treatment recommendations.
Our study has several limitations. The retrospective design is subject to bias with the potential for missing data and the timing of symptom onset could only be estimated based on chart review. History obtained by the clinician is also subjective to recall bias from the patient. Therefore we were unable to precisely determinate the date or month of symptom onset in the majority of patients. It should be noted, however, that a gradual onset is classically reported in ABF following radiation of the neck and further prospective studies in which investigators inquire systematically and specifically about common manifestations of baroreflex failure are needed to better define the natural history and risk factors of ABF. Due to the retrospective nature of the study, differences between acute and chronic manifestations of ABF could not be assessed properly. Pharmacologic tests or analysis of the pressor responses to different stimuli to investigate the afferent limb of the baroreflex were not performed; however, none of these tests are usually performed routinely outside of research laboratories. Finally, there is the possibility of referral bias because patients with ABF are more likely to be referred to the autonomic clinic when they experience symptoms of OH, which may have captured a more severe phenotype of ABF associated with OH.
ABF should be suspected in patients with a history of head and neck cancer treated by radiation or surgery who present with labile hypertension and OH. The management is challenging and may require the use of both antihypertensive and pressor medications. The morbidity and mortality associated with ABF are high. Further studies are needed to better understand the pathophysiology of ABF.
Glossary
- ABF
afferent baroreflex failure
- ARS
autonomic reflex screen
- BP
blood pressure
- CASS
composite autonomic scoring scale
- CI
confidence interval
- OH
orthostatic hypotension
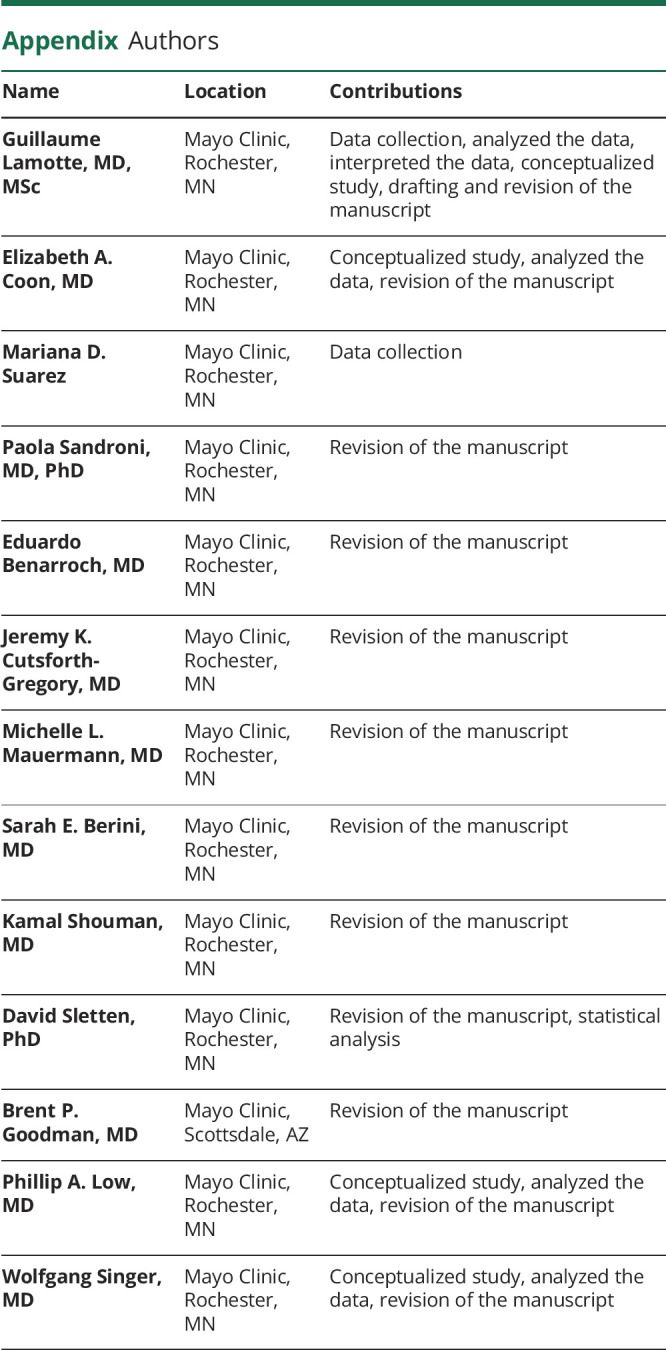
Appendix. Authors
Footnotes
CME Course: NPub.org/cmelist
Podcast: Npub.org/5AB689
Study Funding
Supported by NIH (P01NS44233, U54NS065736, K23NS075141, R01 FD004789, R01 NS092625), Cure MSA Foundation, and Mayo Funds.
Disclosure
None of the authors has conflict of interest. Go to Neurology.org/N for full disclosures.
References
- 1.Kaufmann H, Norcliffe-Kaufmann L, Palma JA. Baroreflex dysfunction. N Engl J Med. 2020;382(2):163-178. [DOI] [PubMed] [Google Scholar]
- 2.Benarroch EE. The arterial baroreflex: functional organization and involvement in neurologic disease. Neurology. 2008;71(21):1733. [DOI] [PubMed] [Google Scholar]
- 3.Robertson D, Hollister AS, Biaggioni I, Netterville JL, Mosqueda-Garcia R, Robertson RM. The diagnosis and treatment of baroreflex failure. N Engl J Med. 1993;329(20):1449-1455. [DOI] [PubMed] [Google Scholar]
- 4.Norcliffe-Kaufmann L, Axelrod F, Kaufmann H. Afferent baroreflex failure in familial dysautonomia. Neurology. 2010;75(21):1904-1911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ketch T, Biaggioni I, Robertson R, Robertson D. Four faces of baroreflex failure: hypertensive crisis, volatile hypertension, orthostatic tachycardia, and malignant vagotonia. Circulation. 2002;105(21):2518-2523. [DOI] [PubMed] [Google Scholar]
- 6.Barboi A, Pocica S. Somatic and autonomic findings in cancer-related base of the skull syndromes. Clin Auton Res. 2020;30(4):343-346. [DOI] [PubMed] [Google Scholar]
- 7.Timmers HJ, Wieling W, Karemaker JM, Lenders JW. Baroreflex failure: a neglected type of secondary hypertension. Neth J Med. 2004;62(5):151-155. [PubMed] [Google Scholar]
- 8.Whelton PK, Carey RM, Aronow WS, et al. ; 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults. Executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2018;138(17):e426-e483. [DOI] [PubMed] [Google Scholar]
- 9.Freeman R, Wieling W, Axelrod FB, et al. Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Clin Auton Res. 2011;21(2):69-72. [DOI] [PubMed] [Google Scholar]
- 10.Low PA. Composite autonomic scoring scale for laboratory quantification of generalized autonomic failure. Mayo Clin Proc. 1993;68:748-752. [DOI] [PubMed] [Google Scholar]
- 11.Nasr N, Pavy-Le Traon A, Larrue V. Baroreflex sensitivity is impaired in bilateral carotid atherosclerosis. Stroke. 2005;36(9):1891-1895. [DOI] [PubMed] [Google Scholar]
- 12.Eiken O, Nowak J, Jogestrand T, Mekjavic IB. Effects of local arteriosclerosis on carotid baroreflex sensitivity and on heart rate and arterial pressure variability in humans. Clin Physiol Funct Imaging. 2006;26(1):9-14. [DOI] [PubMed] [Google Scholar]
- 13.Gianaros PJ, Jennings JR, Olafsson GB, et al. Greater intima-media thickness in the carotid bulb is associated with reduced baroreflex sensitivity. Am J Hypertens. 2002;15(6):486-491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Timmers HJ, Buskens FG, Wieling W, Karemaker JM, Lenders JW. Long-term effects of unilateral carotid endarterectomy on arterial baroreflex function. Clin Auton Res. 2004;14(2):72-79. [DOI] [PubMed] [Google Scholar]
- 15.Dehn TC, Angell-James JE. Long-term effect of carotid endarterectomy on carotid sinus baroreceptor function and blood pressure control. Br J Surg. 1987;74(11):997–1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zar T, Peixoto AJ. Paroxysmal hypertension due to baroreflex failure. Kidney Int. 2008;74(1):126-131. [DOI] [PubMed] [Google Scholar]
- 17.Robertson D, Hollister AS, Biaggioni I, Netterville JL, Mosqueda-Garcia R, Robertson RM. The diagnosis and treatment of baroreflex failure. N Engl J Med. 1993;329(20):1449-1455. [DOI] [PubMed] [Google Scholar]
- 18.Norcliffe-Kaufmann L, Millar Vernetti P, Palma JA, Balgobin BJ, Kaufmann H. Afferent baroreflex dysfunction: decreased or excessive signaling results in distinct phenotypes. Semin Neurol. 2020;40(5):540-549. [DOI] [PubMed] [Google Scholar]
- 19.Jordan J, Shannon JR, Black BK, et al. Malignant vagotonia due to selective baroreflex failure. Hypertension. 1997;30(5):1072-1077. [DOI] [PubMed] [Google Scholar]
- 20.Biaggioni I, Shibao CA, Diedrich A, Muldowney JAS III, Laffer CL, Jordan J. Blood pressure management in afferent baroreflex failure: JACC review topic of the week. J Am Coll Cardiol. 2019;74(23):2939-2947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yates BJ, Bolton PS, Macefield VG. Vestibulo-sympathetic responses. Compr Physiol. 2014;4(2):851-887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Palma JA, Norcliffe-Kaufmann L, Perez MA, Spalink CL, Kaufmann H. Sudden unexpected death during sleep in familial dysautonomia: a case-control study. Sleep. 2017;40(8):zsx083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Adams HP Jr. Cancer and cerebrovascular disease. Curr Neurol Neurosci Rep. 2019;19(10):73. [DOI] [PubMed] [Google Scholar]
- 24.Sarafidis PA, Theodorakopoulou M, Dipla K, et al. Hyponatremia accompanying volatile hypertension caused by baroreflex failure after neck surgery: case report and literature review. J Hypertens. 2020;38(8):1617-1624. [DOI] [PubMed] [Google Scholar]
- 25.Zhao W, Robbins ME. Inflammation and chronic oxidative stress in radiation-induced late normal tissue injury: therapeutic implications. Curr Med Chem. 2009;16(2):130-143. [DOI] [PubMed] [Google Scholar]
- 26.Xu J, Cao Y. Radiation-induced carotid artery stenosis: a comprehensive review of the literature. Interv Neurol. 2014;2(4):183-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sharabi Y, Dendi R, Holmes C, Goldstein DS. Baroreflex failure as a late sequela of neck irradiation. Hypertension. 2003;42(:110-116. [DOI] [PubMed] [Google Scholar]
- 28.Chen AM, Hall WH, Li J, et al. Brachial plexus-associated neuropathy after high-dose radiation therapy for head-and-neck cancer. Int J Radiat Oncol Biol Phys. 2012;84(1):165-169. [DOI] [PubMed] [Google Scholar]
- 29.Killer HE, Hess K. Natural history of radiation-induced brachial plexopathy compared with surgically treated patients. J Neurol. 1990;237(4):247-250. [DOI] [PubMed] [Google Scholar]
- 30.Olsen NK, Pfeiffer P, Mondrup K, Rose C. Radiation-induced brachial plexus neuropathy in breast cancer patients. Acta Oncol. 1990;29(7):885-890. [DOI] [PubMed] [Google Scholar]
- 31.Timmers HJ, Karemaker JM, Wieling W, et al. Arterial baroreflex and peripheral chemoreflex function after radiotherapy for laryngeal or pharyngeal cancer. Int J Radiat Oncol Biol Phys. 2002;53(5):1203-1210. [DOI] [PubMed] [Google Scholar]
- 32.Kaufmann H, Biaggioni I, Voustianiouk A, et al. Vestibular control of sympathetic activity: an otolith-sympathetic reflex in humans. Exp Brain Res. 2002;143(4):463-469. [DOI] [PubMed] [Google Scholar]
- 33.Norcliffe-Kaufmann L, Palma JA, Martinez J, Kaufmann H. Carbidopa for afferent baroreflex failure in familial dysautonomia: a double-blind randomized crossover clinical trial. Hypertension. 2020;76(3):724-731. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Anonymized data will be shared by request from any qualified investigator.




