Abstract
Objective
To provide nationally representative prevalence estimates of disability associated with prior head injury with loss of consciousness in the United States and to examine associations between prior head injury and disability.
Methods
This was a cross-sectional analysis of 7,390 participants ≥40 years of age in the 2011–2014 National Health and Nutrition Examination Surveys (NHANES). Head injury with loss of consciousness was assessed by self-report. Domains of disability were assessed with a standardized structured questionnaire and measured grip strength. Logistic and linear regression models adjusted for demographic, socioeconomic/behavioral, and medical comorbidity variables were used. Multiple imputation was used to account for missing covariate data.
Results
Mean age of participants was 58 years; 53% were female; 71% were non-Hispanic White; and 16% had a history of head injury with loss of consciousness. Overall, participants with a history of head injury had higher prevalence of disability in at least 1 domain of functioning compared to individuals without head injury (47.4% vs 38.6%, p < 0.001), with the highest prevalence of disability in the domains of mobility and work productivity. In fully adjusted models, head injury was significantly positively associated with disability in all domains assessed on the standardized questionnaire (all p < 0.05). Participants with head injury had greater grip strength (all p < 0.05).
Conclusions
We found that 47.4% of individuals ≥40 years of age in the United States with a history of head injury are living with disability in at least 1 domain of functioning, corresponding to 11.4 million affected individuals. This significant burden of disability suggests that efforts are needed to improve functioning among individuals with head injury.
Head injury is associated with significant morbidity and mortality in the United States, with ≈16% of adults ≥40 years of age reporting a history of head injury with loss of consciousness at some point in their lives.1 Over the past few decades, there has been increased recognition that the sequelae of head injury are long-lasting. Further, head injury with loss of consciousness has been shown to be associated with worse outcomes compared to head injury without loss of consciousness.2 Given the high burden of head injury with loss of consciousness in the United States and the association with worse outcomes, accurate, representative data on the prevalence and associations of head injury with loss of consciousness with disability are particularly important for both public health and patient-related long-term care and management planning.
Early data on head injury–associated disability were primarily extrapolated from models as opposed to primary data collected on head injury–associated disability from studies.3-7 More recently, several hospital-based and population-based studies have reported prevalence of head injury–related disability and investigated associations between head injury and disability, both within the United States8-12 and internationally.13-16 However, to the best of our knowledge, no prior study has provided nationally representative estimates of the prevalence of disability associated with prior head injury with loss of consciousness in the United States based on data collected in a nationally representative sample.
The 2011–2014 National Health and Nutrition Examination Surveys (NHANES) provide a unique opportunity to estimate the prevalence of head injury with loss of consciousness–associated disability and estimates are generalizable to the noninstitutionalized civilian population of adults ≥40 years of age in the United States. The primary objectives of this study were (1) to provide nationally representative prevalence estimates of disability associated with prior head injury with loss of consciousness in the United States and (2) to examine associations between prior head injury with loss of consciousness and disability.
Methods
Study Population
NHANES is a series of cross-sectional surveys conducted biennially since 1999 to 2000 by the National Center for Health Statistics of the Centers for Disease Control and Prevention.
NHANES uses a complex, multistage probability sampling design to select participants who are representative of the civilian noninstitutionalized population of the United States.17,18 All participants undergo a standardized in-home interview, followed by a physical examination and blood and urine collection at a mobile examination center. An adult proxy provides information for participants who are unable to answer questions themselves. For the present study, we used data from the 2011–2012 and 2013–2014 survey cycles, when head injury was assessed.
Standard Protocol Approvals, Registrations, and Patient Consents
The NHANES protocol was approved by the National Center for Health Statistics Research Ethics Review Board, and written informed consent was obtained from all participants or legally authorized representatives.19
Head Injury With Loss of Consciousness Definition
Head injury with loss of consciousness was self-reported with the question, “have you ever had loss of consciousness because of a head injury?” This definition has been reported previously.1 The self-reported question was a part of the taste and smell questionnaire administered to all participants ≥40 years of age in 2011 to 2014.
Disability Definitions
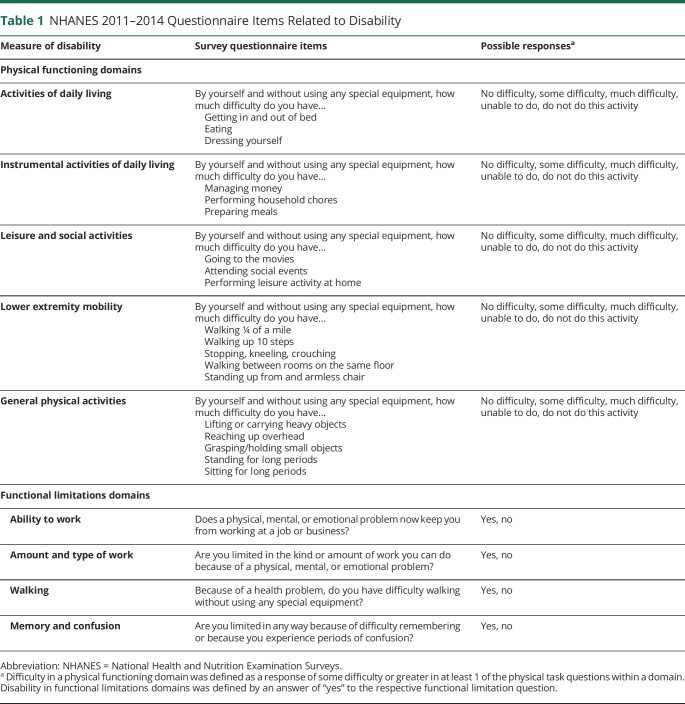
Participants were interviewed about physical functioning and functional limitations with a Computer-Assisted Personal Interviewing system.17,18 Participants were asked questions regarding difficulty performing physical functioning activities in 5 domains: activities of daily living (ADL), instrumental ADL (IADL), leisure and social activities, lower extremity mobility, and general physical activities. Disability in physical functioning domains was defined as a report of “some” or greater difficulty in at least 1 of the activities within each domain (table 1). Participants were also asked questions about functional limitations in ability to work, in type or amount of work, in walking, and due to memory and confusion. Disability in functional limitations domains was defined by an answer of “yes” to the respective functional limitation question (table 1). Domains of disability were defined in accordance with previously described methods.20,21 Because the self-reported disability domains did not assess upper extremity function, we additionally used measured grip strength to assess for upper extremity disability.22 Grip strength has previously been shown to be a meaningful measure of upper extremity function and disability.23,24 A Takei digital dynamometer (model T.K.K.5401, Niigata City, Japan) was used to record the maximum reading (kilograms) of grip strength force. Each hand was tested 3 times with a 60-second break between trials, and best values were recorded for the dominant hand, the nondominant hand, and combined hands.
Table 1.
NHANES 2011–2014 Questionnaire Items Related to Disability
Covariates
Detailed information on the data collection for the 2011–2012 and 2013–2014 in-person interviews, physical examinations, and blood samples obtained in NHANES is documented elsewhere.17,18 Briefly, data on age (continuous), sex (male, female), race/ethnicity (non-Hispanic White, non-Hispanic Black, Mexican American; other), education (less than high school, high school or equivalent, some college or above), ratio of family income to poverty (ratio of the participant's self-reported annual family income to the federal poverty threshold specific for the year of the interview25; ≥350%+, 130%–349%, <130%), moderate/vigorous work or recreational activity (defined as performing ≥10 minutes of activity causing either small or large increases in breathing or heart rate; yes, no), alcohol consumption (never, former, current), smoking status (never, former, current), and military veteran status (yes, no) were self-reported. Diabetes was defined as self-reported physician-diagnosed diabetes, taking diabetes medications, or hemoglobin A1c ≥6.5. Hypertension was defined as self-reported physician-diagnosed hypertension, taking hypertension medications, systolic blood pressure ≥40 mm Hg, or diastolic blood pressure ≥90 mm Hg. History of cardiovascular disease (defined as coronary heart disease or prior myocardial infarction), history of stroke, and history of sleep disorder were self-reported. Depression was defined as a score of ≥10 on the 9-item Patient Health Questionnaire.26
Statistical Analyses
We performed all statistical analyses incorporating appropriate National Center for Health Statistics–derived survey weights to account for the complex NHANES sampling design and to make the estimates reported here nationally representative of the noninstitutionalized civilian population of adults ≥40 years of age in the United States in 2011 to 2014.27 Standard errors were obtained with the Taylor series (linearization) method in accordance with analysis recommendations from the National Center for Health Statistics.27
Unadjusted and age-adjusted prevalences (95% confidence interval [CI]) were calculated by history of head injury for each domain of disability. We applied our prevalence estimates to the 2013 American Community Survey–Public Use Microdata Sample to obtain estimates of the number of individuals ≥40 years of age with disability among individuals with and without head injury in the United States in the year 2013.28 Specifically, the prevalence of head injury was multiplied by the number of American Community Survey–Public Use Microdata Sample individuals ≥40 years of age to obtain the estimate of the number of adults with and without a history of head injury in the United States in 2013. Then, the prevalence of disability among individuals with and without head injury was multiplied by the number of individuals with and without head injury, respectively, to obtain the estimate of the number of adults ≥40 years of age with disability among individuals with and without head injury in the United States in 2013.
We used logistic regression models to estimate the associations between head injury with loss of consciousness and domains of disability. Sex-stratified linear regression models were used to estimate associations between head injury with loss of consciousness and grip strength. We present 3 statistical models to show the impact of progressive adjustment for a priori–selected confounders of the association between history of head injury and disability. Model 1 was adjusted for demographic variables (age, sex, and race/ethnicity). Model 2 included all variables in model 1 plus socioeconomic status and behavioral variables (education, ratio of family income to poverty, physical activity, alcohol consumption, smoking, and military status). Model 3 included all variables in model 2 plus medical comorbid conditions (diabetes, hypertension, history of cardiovascular disease, history of stroke, depression, and history of sleep disorder). Multiple imputation by chained equations methods with 25 sets of imputations was used to account for missing covariates in all analyses; we additionally performed a sensitivity analysis using 100 sets of imputations. The following variables contained missing data: education (n = 7), family income to poverty ratio (n = 663), moderate/vigorous work or recreational activity (n = 2), alcohol consumption (n = 961), hypertension (n = 314), history of cardiovascular disease (n = 3), history of stroke (n = 8), and depression (n = 986). We additionally performed a sensitivity analysis excluding participants with a history of stroke (unweighted n = 422). In prespecified secondary analyses, we repeated our analyses stratified by age (40–64 years vs ≥65 years) because both head injury and disability increase with age.29,30 Formal testing for multiplicative interaction by age was performed.
All reported p values were based on 2-sided tests, and values of p < 0.05 were considered statistically significant. Stata SE version 15 (StataCorp, College Station, TX) was used to perform all analyses.
Data Availability
NHANES questionnaires, datasets, and data dictionaries are publicly available at cdc.gov/nchs/nhanes/index.htm.
Results
Detailed in-person interviews were obtained from 19,931 individuals (9,338 individuals in 2011–2012 and 9,813 individuals in 2013–2014). Information on head injury was obtained from all participants ≥40 years of age. Of the 7,418 individuals ≥40 years of age, 19 were excluded due to missing head injury data, and 9 were excluded due to missing disability data, leaving a total of 7,390 participants included in the present analyses (figure 1). Grip strength data were available in a subset of this population (n = 6,308).
Figure 1. Participant Inclusion/Exclusion Diagram, NHANES 2011–2014.
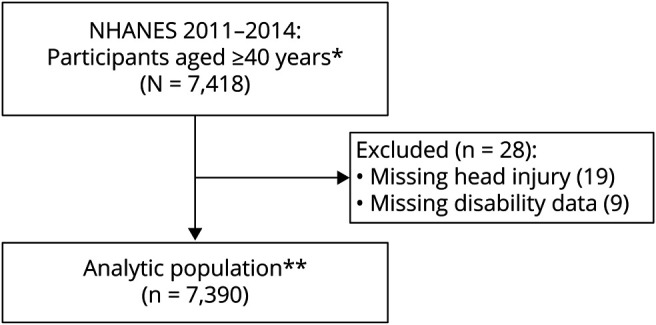
NHANES = National Health and Nutrition Examination Surveys. *Head injury with loss of consciousness question was a part of the taste and smell questionnaire, which was administered to all participants ≥40 years of age during the 2011–2012 and 2013–2014 surveys. **The following covariates contained missing data that were accounted for with multiple imputation using chained equations in all adjusted analyses: education (n = 7), family income to poverty ratio (n = 663), moderate/vigorous work or recreational activity (n = 2), alcohol consumption (n = 961), hypertension (n = 314), history of cardiovascular disease (n = 3), history of stroke (n = 8), and depression (n = 986).
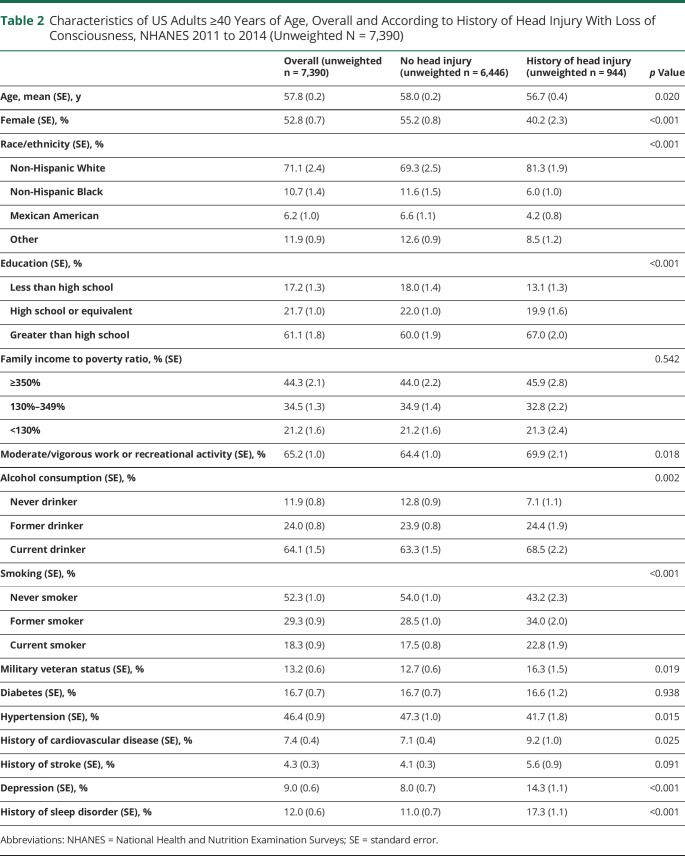
Mean age of participants was 58 years; 53% were female; 11% were non-Hispanic Black; 6% were Mexican American; and 16% had a history of head injury with loss of consciousness (table 2). Compared to individuals without head injury, individuals reporting a history of head injury with loss of consciousness were younger (57 years vs 58 years, p = 0.02) and were more likely to be male (60% vs 45%, p < 0.001) and of non-Hispanic White race (81% vs 69%, p < 0.001). Individuals with a history of head injury with loss of consciousness were also more likely than individuals without head injury to engage in moderate/vigorous work or recreational activity (70% vs 64%, p = 0.02), to be military veterans (16% vs 13%, p = 0.02), and to have depression (14% vs 8%, p < 0.001).
Table 2.
Characteristics of US Adults ≥40 Years of Age, Overall and According to History of Head Injury With Loss of Consciousness, NHANES 2011 to 2014 (Unweighted N = 7,390)
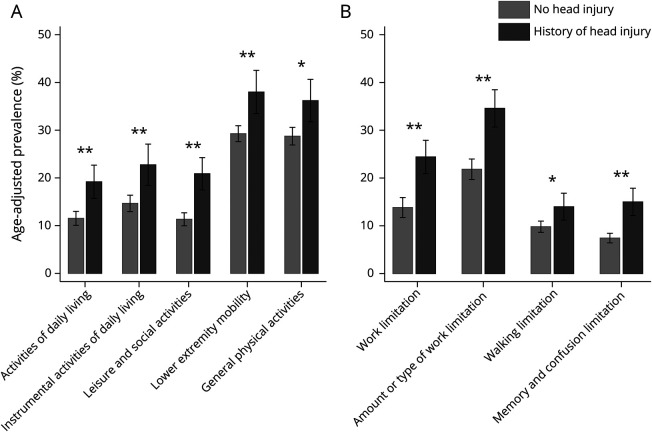
Overall, participants with a history of head injury with loss of consciousness had higher unadjusted prevalence of disability in at least 1 domain of functioning as assessed on the standardized questionnaire compared to individuals without a history of head injury (47.4% vs 38.6%, p < 0.001). This corresponds to 11.4 million (95% CI 10.3–12.3 million) individuals in the United States with a history of head injury with loss of consciousness and disability in at least 1 domain of functioning. Across all physical functioning domains (figure 2A) and functional limitations domains (figure 2B), individuals with head injury with loss of consciousness had higher age-adjusted prevalence of disability compared to individuals without head injury (all p < 0.01). Among the physical functioning domains, individuals with head injury with loss of consciousness had highest age-adjusted prevalence of disability in the lower extremity mobility domain (38.0%, 95% CI 33.5%–42.5%), which corresponds to 8.6 million (95% CI 7.5–9.7 million) affected individuals in the United States, closely followed by the general physical activities domain (36.2%, 95% CI 31.7%–40.6%), corresponding to 8.2 million (95% CI 7.1–9.3 million) affected US individuals. Within the functional limitations domains, individuals with head injury with loss of consciousness had the highest age-adjusted prevalence of disability in the amount and type of work domain (34.6%, 95% CI 30.7%–38.5%), which corresponds to 8.1 million (95% CI 7.2–9.0 million) affected individuals in the United States.
Figure 2. Age-Adjusted Prevalence (95% confidence interval) of Disability by History of Head Injury With Loss of Consciousness.
(A) Physical functioning domains. (B) Functional limitations domains. *p < 0.01 comparing no head injury to history of head injury. **p < 0.001 comparing no head injury to history of head injury.
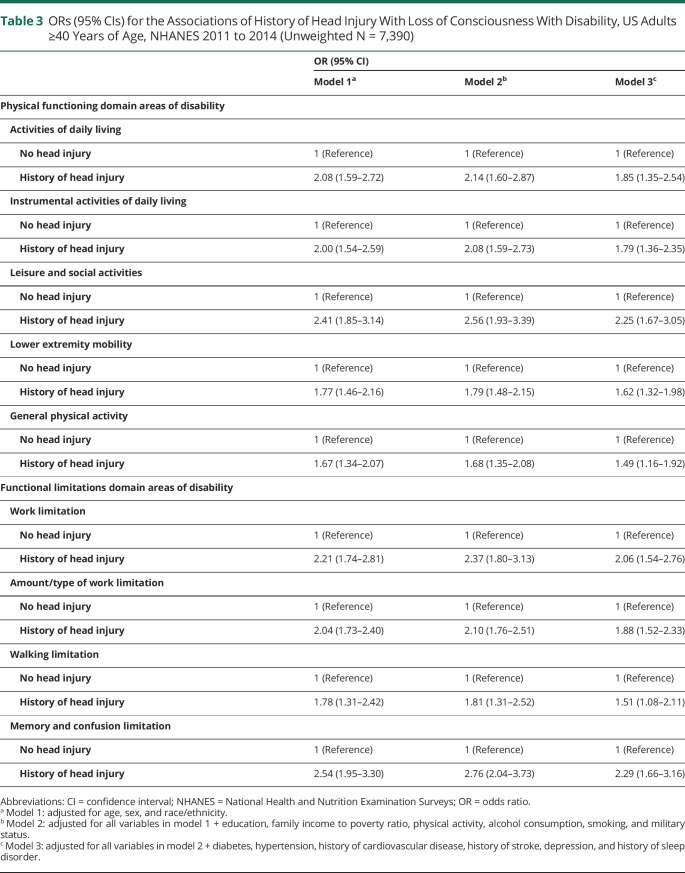
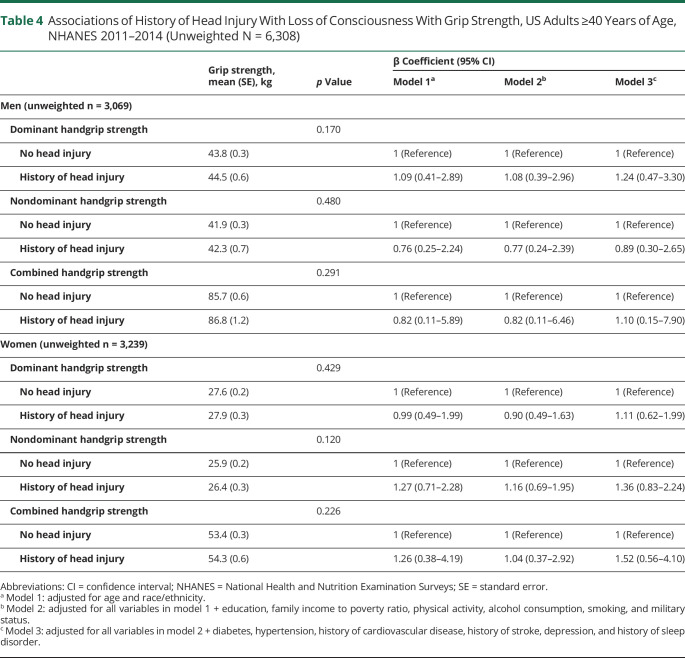
Head injury with loss of consciousness was significantly associated with disability in all domains of the standardized questionnaire after adjustment for demographics and socioeconomic status and behavioral factors (table 3, models 1 and 2). These associations were slightly attenuated but remained significant after additional adjustment for medical comorbid conditions (table 3, model 3). In fully adjusted models, within the physical functioning domains, head injury with loss of consciousness (vs no head injury) was associated with disability in domains of ADL (odds ratio [OR] 1.92, 95% CI 1.41–2.61), IADL (OR 1.84, 95% CI 1.41–2.42), leisure and social activities (OR 2.30, 95% CI 1.71–3.10), lower extremity mobility (OR 1.66, 95% CI 1.36–2.03), and general physical activity (OR 1.53, 95% CI 1.20–1.96). Within the functional limitations domains, head injury with loss of consciousness was associated with disability in domains of work limitation (OR 2.10, 95% CI 1.57–2.82), amount and type of work (OR 1.93, 95% CI 1.57–2.36), walking limitation (OR 1.57, 95% CI 1.13–2.20), and memory and confusion limitation (OR 2.36, 95% CI 1.74–3.20). Results from our sensitivity analysis with 100 sets of imputations for missing model 3 covariates and from our sensitivity analysis excluding individuals with a history of stroke were not appreciably different from our main results (etable 1; data available from Dryad: doi.org/10.5061/dryad.s1rn8pk76). In contrast, head injury was associated with greater upper extremity grip strength (all p < 0.05) (table 4).
Table 3.
ORs (95% CIs) for the Associations of History of Head Injury With Loss of Consciousness With Disability, US Adults ≥40 Years of Age, NHANES 2011 to 2014 (Unweighted N = 7,390)
Table 4.
Associations of History of Head Injury With Loss of Consciousness With Grip Strength, US Adults ≥40 Years of Age, NHANES 2011–2014 (Unweighted N = 6,308)
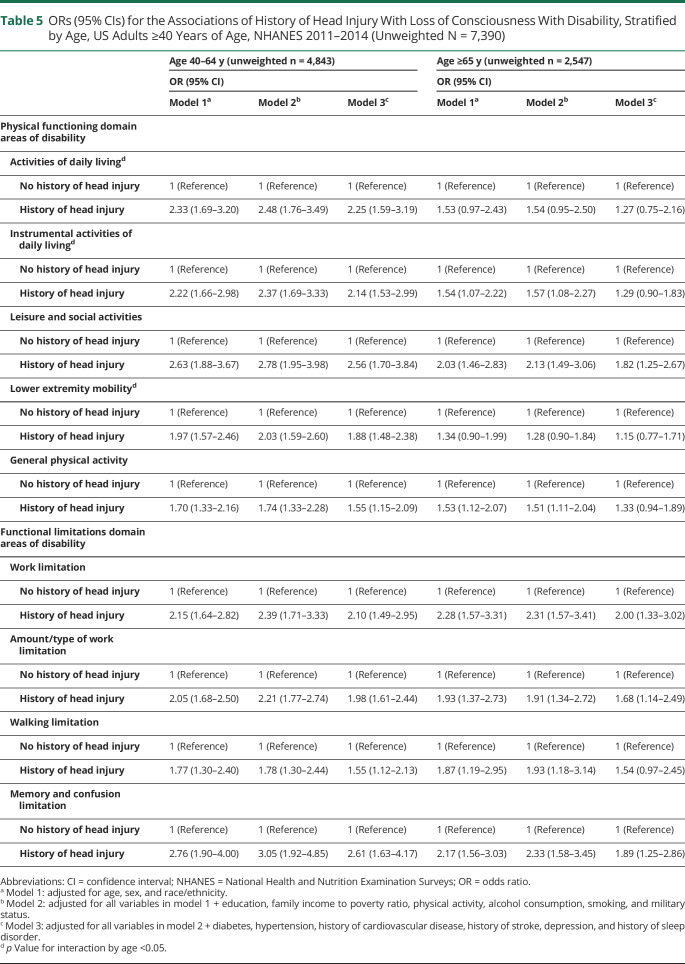
In prespecified secondary analyses stratified by age (40–64 years vs ≥65 years) (table 5), OR point estimates for the associations of head injury with loss of consciousness and physical functioning disability domains were consistently higher among younger compared to older participants. However, the p value for multiplicative interaction by age was significant only for the domains of IADL (model 3, p for interaction = 0.031) and lower extremity mobility (model 3, p for interaction = 0.026). OR point estimates were higher for younger vs older participants in the functional limitations domains of work limitation, amount/type of work limitation, and memory and confusion limitation domains, but they were similar between age groups for the walking limitation domain. However, formal tests for multiplicative interaction testing by age were nonsignificant for all functional limitations domains (all p for interaction > 0.05).
Table 5.
ORs (95% CIs) for the Associations of History of Head Injury With Loss of Consciousness With Disability, Stratified by Age, US Adults ≥40 Years of Age, NHANES 2011–2014 (Unweighted N = 7,390)
Discussion
This study provides nationally representative estimates of the prevalence of disability associated with prior head injury with loss of consciousness, showing that ≈11.4 million individuals, or 47.4% of all noninstitutionalized, civilian individuals ≥40 years of age in the United States with a history of head injury with loss of consciousness, are living with disability in at least 1 domain of functioning. Among individuals with a history of head injury with loss of consciousness, the highest age-adjusted prevalence of disability was observed in the categories of lower extremity mobility, general physical activities, and amount or type of work limitation domains, suggesting that head injury disproportionately affects functioning in mobility and work productivity. Overall, our study provides valid and reliable nationally representative estimates of disability that are important to improving the understanding of the magnitude of both the individual and societal burdens of head injury with loss of consciousness.
Several prior studies have investigated the prevalence of head injury–related disability and associations of head injury and disability within different regions in the United States,8-12 but none to the best of our knowledge have reported nationally representative estimates using data collected in a nationally representative sample. The definitions of head injury varied between prior studies, as did the time between head injury and ascertainment of disability. Several early studies extrapolated disability prevalence from models based on head injury prevalence data, obtaining prevalence estimates ranging from 3.3 to 5.3 million individuals with prior head injury living with disability.3-7 In studies from individual states (Ohio [participants ≥18 years of age] and Colorado [participants ≥16 years of age]), the prevalence of disability ranged from 18% to 100%, depending on number of prior head injuries and injury severity.9,10,12 These studies defined head injury using the Ohio State University TBI Identification Method survey (with loss of consciousness)9,12 and using ICD-9 codes (with and without loss of consciousness).10 In a subset of patients with mild traumatic brain injury (85% with loss of consciousness) from the trauma center–based Transforming Research and Clinical Knowledge in Traumatic Brain Injury (TRACK-TBI) study (mean age of participants 41 years), the prevalence of disability decreased over the first year after injury, but a significant proportion of individuals still had disability in work functioning (24%), social/leisure functioning (27%), and ADL/IADL (4%) at 1 year after injury.8 Several international studies also have reported associations of head injury with disability.13-16 A population-based cohort study in Sweden (participants 18–64 years of age) defining head injury (with or without loss of consciousness) from hospital registers reported that ≈44% of individuals with a history of head injury had at least 1 disability 3 years after injury,16 and other studies from France15 (median age 50 years), Ontario, Canada (participants ≥18 years of age),14 and Singapore13 (participants ≥60 years of age) also reported increased disability among individuals with a history of head injury (head injury defined by self-report of injury-related harm or permanent sequelae due to a traumatic brain injury15 and by self-reported questions about head injury with loss of consciousness13,14) compared to those without a history of head injury. Similar to our study, the majority of prior studies that used a self-reported head injury definition did not have the information to report time between head injury and disability ascertainment,9,12-14 while studies using hospitalization records typically did report time between head injury and disability ascertainment.8,10,16
Our results extend the existing literature by providing nationally representative prevalence estimates from the United States. The prevalence estimates from our study are higher than much of what has been reported from extrapolated modeling data (in which disability data were not primarily collected)3-7 and from many state-representative or US hospital/clinic-based studies9,10,12 but are similar to prevalence estimates from Sweden16 and from the TRACK-TBI Study (for domains of work limitation and social and leisure activities).8 Differences in the observed prevalence estimates of head injury–associated disability likely reflect observed differences in study methods used to define head injury and differences in study populations (e.g., age of participants), head injury severity, and length of time between head injury and disability ascertainment. In addition, the definition of disability is heterogeneous in the literature, and the distinction between disability and functional limitations is often blurred. Overall, taking into account the impact of age on disability, our estimates of disability are consistent both with prior NHANES publications using the same disability definitions20,21 and with other studies using data representative of the US population.31,32 What is consistent across all studies on head injury and disability is that head injury is associated with a significant burden of disability,8-11,13-16 and the results of our study provide nationally representative estimates for the entire US population.
In our study, we observed the highest age-adjusted prevalence of disability among individuals with a history of head injury with loss of consciousness in the categories of lower extremity mobility, general physical activities, and amount or type of work limitation domains, suggesting that mobility and work/job–related functions are the most affected domains among individuals with a history of head injury. In contrast to lower extremity disability, upper extremity function, as assessed by measured grip strength,23 was stronger among individuals with head injury, which may be explained by the presence of other chronic traumatic brain injury–related symptoms such as impaired balance and vestibular dysfunction/dizziness, which affect lower extremity mobility more than upper extremity function.33
In prespecified secondary analyses, we also examined associations between a history of head injury and disability stratified by age (40–64 years vs ≥65 years) and found higher point estimates in most physical functioning and functional limitations domains among younger compared to older participants, although there was statistically significant evidence for multiplicative interaction by age only in the associations of head injury with disability in the IADL and lower extremity mobility domains. Few studies on the relationship of head injury with disability investigated differences in the association by age, and those that did used different measures to assess both head injury and disability/functioning, making comparison across studies difficult. One study of participants with an age distribution similar to that in the present study found that younger individuals (≤65 years of age) had greater functional improvement (as assessed by the Glasgow Outcome Scale–Extended) over the first year after injury compared to older individuals (>65 years of age) after severe traumatic brain injury.34 Other studies found no differences in point estimates and no significant interaction by age in the association of head injury with disability prevalence9 or functional outcome (as assessed by the Glasgow Outcome Scale–Extended).35
The use of a single self-reported question to ascertain head injury with loss of consciousness is an important consideration in the interpretation of the results of this study. This specific head injury with loss of consciousness definition has not been validated, but it has been reported previously,1,36 and other self-reported definitions have been shown to be reliable in assessing a history of head injury, even among individuals with cognitive impairment.37 However, other studies have shown that self-report of head injury may result in an underreporting of head injury events (highly specific definition with lower sensitivity), which can lead to misclassification and underestimation of associations.38,39 Self-reported definitions of head injury are valuable in large population-based epidemiologic studies in which it may not be feasible to perform a more detailed assessment. However, the use of this definition is limited by the lack of detailed information on the clinical presentation, severity, associated polytrauma, number of head injuries, timing of head injury events, or the time between head injury and disability assessment. Time between head injury and participation in NHANES may influence the recall of head injury events, whereby there may be selective underascertainment of head injury among participants with greater time between head injury and NHANES participation, which is particularly relevant among older participants who may have had more time between head injury and NHANES participation than younger participants. Indeed, prior studies have found that an increased time from head injury was associated with reduced recall.38 Other factors associated with decreased recall of a prior head injury event include injury occurring very early in childhood (i.e., during the time period of childhood amnesia whereby adults are unable to retrieve episodic memories occurring before the age of 2–4 years) and milder injury severity.38 NHANES asked participants about head injury with loss of consciousness, which represents a more severe category of head injury than head injury without loss of consciousness. It is plausible that recall for head injury with loss of consciousness may be better than for head injury without loss of consciousness due to the higher severity of injury, although no comparative validation studies have been performed. Furthermore, function and disability after head injury also vary with time since head injury, whereby a higher proportion of individuals with head injury have disability in the first few months after injury compared to later time points.8 Because NHANES does not include institutionalized persons (e.g., those in rehabilitation centers in the weeks/months immediately after a head injury), the estimates obtained in the present study may underestimate the full burden of head injury–associated disability at any given time point.
This study has several limitations that should be taken into consideration in the interpretation of the results. First, the cross-sectional study design of NHANES does not allow us to draw conclusions regarding directionality or causality of the observed associations. Second, head injury status was asked only of participants ≥40 years of age; therefore, our estimates are not representative of younger persons. Furthermore, our study may underestimate the total head injury–associated disability in the United States because certain groups who may have a higher burden of head injury and disability, including active-duty military, nursing facility residents, homeless individuals, and prisoners, were not included in the survey. The use of proxies to answer self-report questions allowed the inclusion of participants with a history of more severe head injury or with disability from other causes who are living at home semi-independently but are not able to complete a self-assessment without assistance. Strengths of our study include the large sample size and the comprehensive data collection by trained study personal. In addition, NHANES data provide nationally representative estimates for the noninstitutionalized, civilian US population.
We found that ≈11.4 million individuals, or 47.4% of all noninstitutionalized, civilian individuals ≥40 years of age in the United States, with a history of head injury are living with disability in at least 1 domain of functioning. Although individuals with a history of head injury had greater disability across multiple domains of physical functioning and functional limitations compared to individuals without head injury, individuals with a history of head injury had the highest prevalence in domains of mobility and work functioning. The significant burden of disability among individuals with a history of head injury in the United States suggests that research into the long-term care and management of the sequelae of head injury should be both a public health– and patient care–related priority to improve outcomes and functioning among individuals with head injury.
Glossary
- ADL
activities of daily living
- CI
confidence interval
- IADL
instrumental activities of daily living
- ICD-9
International Classification of Diseases, 9th revision
- NHANES
National Health and Nutrition Examination Surveys
- OR
odds ratio
- TRACK-TBI
Transforming Research and Clinical Knowledge in Traumatic Brain Injury
Appendix. Authors
Study Funding
The authors report no targeted funding.
Disclosure
A.L.C. Schneider, D. Wang, R.F. Gottesman, and E. Selvin report no disclosures relevant to the manuscript. Go to Neurology.org/N for full disclosures.
References
- 1.Schneider ALC, Wang D, Ling G, Gottesman RF, Selvin E. Prevalence of self-reported head injury in the United States. N Engl J Med. 2018;379(12):1176-1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roy D, Peters ME, Everett AD, et al. Loss of consciousness and altered mental state as predictors of functional recovery within 6 months following mild traumatic brain injury. J Neuropsychiatry Clin Neurosci. 2020;32(2):132-138. [DOI] [PubMed] [Google Scholar]
- 3.Thurman DJ, Alverson C, Dunn KA, Guerrero J, Sniezek JE. Traumatic brain injury in the United States: a public health perspective. J Head Trauma Rehabil. 1999;14(6):602-615. [DOI] [PubMed] [Google Scholar]
- 4.Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil. 2006;21(5):375-378. [DOI] [PubMed] [Google Scholar]
- 5.Selassie AW, Zaloshnja E, Langlois JA, Miller T, Jones P, Steiner C. Incidence of long-term disability following traumatic brain injury hospitalization, United States, 2003. J Head Trauma Rehabil. 2008;23(2):123-131. [DOI] [PubMed] [Google Scholar]
- 6.Ma VY, Chan L, Carruthers KJ. Incidence, prevalence, costs, and impact on disability of common conditions requiring rehabilitation in the United States: stroke, spinal cord injury, traumatic brain injury, multiple sclerosis, osteoarthritis, rheumatoid arthritis, limb loss, and back pain. Arch Phys Med Rehabil. 2014;95(5):986-995.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zaloshnja E, Miller T, Langlois JA, Selassie AW. Prevalence of long-term disability from traumatic brain injury in the civilian population of the United States, 2005. J Head Trauma Rehabil. 2008;23(6):394-400. [DOI] [PubMed] [Google Scholar]
- 8.Nelson LD, Temkin NR, Dikmen S, et al. Recovery after mild traumatic brain injury in patients presenting to US level I trauma centers: a transforming research and clinical knowledge in traumatic brain injury (TRACK-TBI) study. JAMA Neurol. 2019;76(9):1049-1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yi H, Corrigan JD, Singichetti B, et al. Lifetime history of traumatic brain injury and current disability among Ohio adults. J Head Trauma Rehabil. 2018;33(4):E24-E32. [DOI] [PubMed] [Google Scholar]
- 10.Whiteneck G, Brooks CA, Mellick D, Harrison-Felix C, Terrill MS, Noble K. Population-based estimates of outcomes after hospitalization for traumatic brain injury in Colorado. Arch Phys Med Rehabil. 2004;85(4 suppl 2):S73-S81. [DOI] [PubMed] [Google Scholar]
- 11.Saunders LL, Selassie AW, Hill EG, et al. A population-based study of repetitive traumatic brain injury among persons with traumatic brain injury. Brain Inj. 2009;23(11):866-872. [DOI] [PubMed] [Google Scholar]
- 12.Whiteneck GG, Cuthbert JP, Corrigan JD, Bogner JA. Prevalence of self-reported lifetime history of traumatic brain injury and associated disability: a statewide population-based survey. J Head Trauma Rehabil. 2016;31(1):E55-E62. [DOI] [PubMed] [Google Scholar]
- 13.Cetty L, Abdin E, Vaingankar JA, et al. Prevalence and correlates of traumatic brain injury (TBI) in older adults: results from the Well-being of the Singapore Elderly (WiSE) study. Int Psychogeriatr. 2017;29(11):1899-1907. [DOI] [PubMed] [Google Scholar]
- 14.Ilie G, Adlaf EM, Mann RE, et al. Associations between self-reported lifetime history of traumatic brain injuries and current disability assessment in a population sample of Canadian adults. PLoS One. 2018;13(1):e0188908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jourdan C, Azouvi P, Genet F, Selly N, Josseran L, Schnitzler A. Disability and health consequences of traumatic brain injury: national prevalence. Am J Phys Med Rehabil. 2018;97(5):323-331. [DOI] [PubMed] [Google Scholar]
- 16.Styrke J, Sojka P, Bjornstig U, Bylund PO, Stalnacke BM. Sex-differences in symptoms, disability, and life satisfaction three years after mild traumatic brain injury: a population-based cohort study. J Rehabil Med. 2013;45(8):749-757. [DOI] [PubMed] [Google Scholar]
- 17.National Center for Health Statistics. National Health and Nutrition Examination Survey, 2011-2012 [online]. Accessed August 6, 2020. : wwwn.cdc.gov/nchs/nhanes/continuousnhanes/default.aspx?BeginYear=2011.
- 18.National Center for Health Statistics. National Health and Nutrition Examination Survey, 2013-2014 [online]. Accessed August 6, 2020, wwwn.cdc.gov/nchs/nhanes/continuousnhanes/default.aspx?BeginYear=2013.
- 19.National Center for Health Statistics. National Health and Nutrition Examination Survey research Ethics Review Board approval [online]. Accessed August 6, 2020, cdc.gov/nchs/nhanes/irba98.htm.
- 20.Chen DS, Genther DJ, Betz J, Lin FR. Association between hearing impairment and self-reported difficulty in physical functioning. J Am Geriatr Soc. 2014;62(5):850-856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Plantinga LC, Johansen K, Crews DC, et al. Association of CKD with disability in the United States. Am J Kidney Dis. 2011;57(2):212-227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang YC, Bohannon RW, Li X, Yen SC, Sindhu B, Kapellusch J. Summary of grip strength measurements obtained in the 2011-2012 and 2013-2014 National Health and Nutrition Examination Surveys. J Hand Ther. 2019;32(4):489-496. [DOI] [PubMed] [Google Scholar]
- 23.Ekstrand E, Lexell J, Brogardh C. Grip strength is a representative measure of muscle weakness in the upper extremity after stroke. Top Stroke Rehabil. 2016;23(6):400-405. [DOI] [PubMed] [Google Scholar]
- 24.Lee MC, Hsu CC, Tsai YF, Chen CY, Lin CC, Wang CY. Criterion-referenced values of grip strength and usual gait speed using instrumental activities of daily living disability as the criterion. J Geriatr Phys Ther. 2018;41(1):14-19. [DOI] [PubMed] [Google Scholar]
- 25.Gutierrez OM, Isakova T, Enfield G, Wolf M. Impact of poverty on serum phosphate concentrations in the third National Health and Nutrition Examination Survey. J Ren Nutr. 2011;21(2):140-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Levis B, Benedetti A, Thombs BD; DEPRESsion Screening Data Collaboration. Accuracy of Patient Health Questionnaire-9 (PHQ-9) for screening to detect major depression: individual participant data meta-analysis. BMJ. 2019;365:l1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.National Center for Health Statistics. National Health and Nutrition Examination Survey methods and analytic guidelines [online]. Accessed August 6, 2020, wwwn.cdc.gov/nchs/nhanes/analyticguidelines.aspx.
- 28.National Center for Health Statistics. National Health and Nutrition Examination Survey response rates and population totals [online]. Accessed August 6, 2020, wwwn.cdc.gov/nchs/nhanes/ResponseRates.aspx.
- 29.Centers for Disease Control. TBI data and statistics [online]. Accessed August 17, 2020, cdc.gov/traumaticbraininjury/data/index.html.
- 30.Seeman TE, Merkin SS, Crimmins EM, Karlamangla AS. Disability trends among older Americans: National Health and Nutrition Examination Surveys, 1988-1994 and 1999-2004. Am J Public Health. 2010;100(1):100-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Courtney-Long EA, Carroll DD, Zhang QC, et al. Prevalence of disability and disability type among adults–United States, 2013. MMWR Morb Mortal Wkly Rep. 2015;64(29):777-783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zajacova A, Montez JK. Explaining the increasing disability prevalence among mid-life US adults, 2002 to 2016. Soc Sci Med. 2018;211:1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kleffelgaard I, Soberg HL, Tamber AL, et al. The effects of vestibular rehabilitation on dizziness and balance problems in patients after traumatic brain injury: a randomized controlled trial. Clin Rehabil. 2019;33(1):74-84. [DOI] [PubMed] [Google Scholar]
- 34.Haller CS, Delhumeau C, De Pretto M, et al. Trajectory of disability and quality-of-life in non-geriatric and geriatric survivors after severe traumatic brain injury. Brain Inj. 2017;31(3):319-328. [DOI] [PubMed] [Google Scholar]
- 35.Yue JK, Levin HS, Suen CG, et al. Age and sex-mediated differences in six-month outcomes after mild traumatic brain injury in young adults: a TRACK-TBI study. Neurol Res. 2019;41(7):609-623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Grasset L, Glymour MM, Yaffe K, et al. Association of traumatic brain injury with dementia and memory decline in older adults in the United States. Alzheimers Dement. 2020;16(6):853-861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wilmoth K, LoBue C, Clem MA, et al. Consistency of traumatic brain injury reporting in older adults with and without cognitive impairment. Clin Neuropsychol. 2017(3):1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McKinlay A, Horwood LJ, Fergusson DM. Accuracy of self-report as a method of screening for lifetime occurrence of traumatic brain injury events that resulted in hospitalization. J Int Neuropsychol Soc. 2016;22(7):717-723. [DOI] [PubMed] [Google Scholar]
- 39.Corrigan JD, Selassie AW, Orman JA. The epidemiology of traumatic brain injury. J Head Trauma Rehabil. 2010;25(2):72-80. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
NHANES questionnaires, datasets, and data dictionaries are publicly available at cdc.gov/nchs/nhanes/index.htm.