Background:
The presence of a thoracolumbar transitional vertebra (TLTV) and/or lumbosacral transitional vertebra (LSTV) may cause wrong-site surgery and problems while measuring spinopelvic parameters, including pelvic incidence and lumbar lordosis. The Castellvi classification of LSTV addresses coronal images but not sagittal or axial images. Therefore, it is unclear how LSTV differs from the normal lumbosacral anatomy. We aimed to investigate the lumbosacral anatomy and vertebral numbering in patients with TLTV and/or LSTV. We performed computed tomography (CT) to identify TLTV, to number presacral vertebrae accurately, and to analyze morphological differences in each LSTV type.
Methods:
The medical records of 880 patients who underwent spinopelvic fixation between July 2014 and March 2020 were evaluated for TLTV and LSTV. Castellvi LSTVs (above the promontory on the arcuate line of the ilium) and our newly proposed LSTV (“S6 LSTV,” with 6 sacral vertebrae and 5 foramina below the promontory) were analyzed. The anatomical location of the lowest thoracic vertebra was defined, and TLTV with dysplastic ribs was identified. Each LSTV type was examined for its morphological features on sagittal and axial CT images.
Results:
LSTV was observed in 111 (12.6%) of 880 patients. Castellvi type-III LSTV was the most common (42 [37.8%] of 111), followed by S6 LSTV (37 [33.3%] of 111). TLTV was associated with LSTV (87 [78.4%] of 111) and was commonly identified at T13 (59 [67.8%] of 87). On sagittal CT images, the lumbosacral transitional anatomy of Castellvi LSTVs resembled that of normal L5-S1, and the lumbosacral transitional anatomy of S6 LSTV resembled that of normal S1-S2. When comparing the S1 upper segments on axial CT images, most Castellvi LSTVs exhibited S2-like appearances and most S6 LSTVs exhibited L5-like appearances.
Conclusions:
Although LSTV possesses L5 and S1 features, Castellvi LSTVs have more L5 elements than S1 elements. The converse is true for S6 LSTV. At least for the Castellvi type-IIIb LSTV, the vertebra below the Castellvi type-IIIb LSTV should be recognized as S1, but clinically it is better to recognize it as S2. Overlooking TLTV may cause problems in vertebral numbering due to coexisting LSTV.
Clinical Relevance:
Three-dimensional CT images are suitable for detecting transitional vertebrae. This study reveals their morphological features on axial CT images and their lumbosacral anatomy on sagittal CT images.
The presence of a thoracolumbar transitional vertebra (TLTV) and/or lumbosacral transitional vertebra (LSTV) may lead to wrong-site surgery1-3, as well as problems while measuring the spinopelvic parameters. Wrong-site surgery in patients with transitional vertebrae may be avoided by comparing preoperative radiographs with corresponding magnetic resonance imaging (MRI) scans to identify the surgical site and compare preoperative and intraoperative radiographs4. Nevertheless, measurement problems may be complicated as there is no clear definition regarding the measurement of spinopelvic parameters when these vertebrae exist. Pelvic incidence and lumbar lordosis are essential parameters for adult spinal deformity surgery5; however, their values depend on recognizing transitional vertebrae6-8. Stated differently, these values change depending on whether LSTV is regarded as L5 or S1 when measuring the pelvic incidence and on the vertebrae included in the lumbar spine when measuring the lumbar lordosis. Therefore, there is a critical unmet need for further investigation of the morphological features of transitional vertebrae.
Castellvi et al. classified LSTV into 4 types, ranging from enlarged transverse processes of the lowest lumbar vertebra to the complete fusion of its transverse processes with the sacral alae9. This classification is based on the coronal images of LSTV but not on the sagittal or axial images. Although “sacralized L5” and “lumbarized S1” are terms that focus on the sagittal images of LSTV3,10, the Castellvi classification to which these terms apply remains unclear.
TLTV is defined as a vertebra with dysplastic ribs that has partial features of thoracic and lumbar vertebrae at the thoracolumbar junction. Studies on TLTV have examined dysplastic ribs using computed tomographic (CT) images11-13; however, the anatomical location of the lowest thoracic vertebra and enumeration of the thoracic spine to identify TLTV have not been established to date.
We aimed to examine the rib morphology of the lowest thoracic vertebra to identify TLTV using CT images and to investigate the incidence of TLTV and LSTV. Furthermore, each LSTV type was examined to reveal its morphological features on axial CT images and its lumbosacral anatomy on sagittal CT images.
Materials and Methods
This study included patients with lumbar degenerative diseases who underwent spinopelvic fixation between July 2014 and March 2020 at our institution’s spine center. All patients underwent whole-spine radiography, CT, and MRI preoperatively. Patients with congenital spinal anomalies with scoliosis or kyphosis were excluded because of concerns that vertebral numbering could not be accurately assessed14. The medical records of 880 consecutive eligible patients were retrospectively reviewed, and imaging data of these patients were examined for the presence of transitional vertebrae and vertebral numeric variation. This study was approved by the institutional review board (number: 2-19-11-6). This observational study only used clinical information; however, we explained in advance to each patient that these data might be used for research and disclosed the outline of our research content on the home page of our hospital’s website, providing the participants with an opt-out option.
Vertebral Numbering
The number of presacral vertebrae was counted caudally from C2 using whole-spine radiographs, but the following points were noted. First, in order to not consider TLTV as L1 because of rib dysplasia, we clarified the definition of the lowest thoracic vertebra, regardless of the rib morphology. The most proximal bundle of the psoas major typically attaches to the lower margin of the T12 body, upper margin of the L1 body, and the intervertebral disc between T12 and L115. Thus, the lowest thoracic vertebra was identified according to the above definition, mainly using coronal CT images.
Second, the lowest lumbar vertebra was identified as a lumbar vertebra when it was located above the arcuate line of the ilium because normal lumbar vertebrae are located above that line. Additionally, the number of sacral vertebrae and sacral foramina was identified and enumerated when they were below the promontory on the arcuate line on 3-dimensional CT images.
The lowest normal thoracic or lumbar vertebra was designated “non-TLTV” or “non-LSTV” even if numerical variations existed. To accurately express the number of presacral vertebrae, these vertebrae were explicitly described as T13 and L4, T12 and L6, and so on.
TLTV
The rib morphology of the lowest thoracic vertebra was investigated on axial and 3-dimensional CT images. TLTV was defined as the lowest thoracic vertebra with dysplastic ribs. Dysplastic ribs were classified into the following 3 types based on previous studies16,17: type A, short ribs; type B, hypoplastic ribs; and type C, missing ribs (Fig. 1).
Fig. 1.
Schematic representation of 3 types of thoracolumbar transitional vertebrae on axial CT images. Type A: The rib head is present but is smaller than normal, less than half the length of a normal rib 1 level above, and is substantially longer than the L1 transverse process. Type B: The rib head is hypoplastic or not present at all. The costovertebral and costotransverse joints are also hypoplastic. The type-B rib may be shorter or slightly longer than the L1 transverse process. Type C: Missing ribs: Hypoplastic thoracic or lumbar-type transverse process only. Occasionally, a rudimentary rib fuses with the transverse process, appearing as a lumbar-type transverse process.
LSTV
LSTV was detected on 3-dimensional CT images and classified according to the Castellvi classification: type I, unilateral (Ia) or bilateral (Ib) dysplastic transverse process(es) >19 mm; type II, incomplete unilateral (IIa) or bilateral (IIb) osseous fusion of the transverse process(es) to the sacrum; type III, complete unilateral (IIIa) or bilateral (IIIb) osseous fusion of the transverse process(es) to the sacrum; and type IV, mixed. Distinguishing type-I LSTV from normal lumbar vertebrae was often challenging; hence, type-I LSTV was regarded as non-LSTV.
A normal sacrum has 5 sacral vertebrae and 4 sacral foramina. Type-IIIb LSTV (Fig. 2) appeared to have 6 sacral vertebrae on sagittal CT images and 5 sacral foramina on 3-dimensional CT images. Closer scrutiny of the position of the promontory on the arcuate line of the ilium on 3-dimensional CT images revealed that type-IIIb LSTV was positioned above the arcuate line and was identified as the lowest lumbar vertebra. We identified a different LSTV type than type-IIIb LSTV and named it “S6 LSTV” (Fig. 3). Patients with S6 LSTV had 6 sacral vertebrae and 5 sacral foramina below the arcuate line of the ilium. However, demonstrating the difference between type-IIIb LSTV and S6 LSTV based on radiographs only was difficult (Fig. 4).
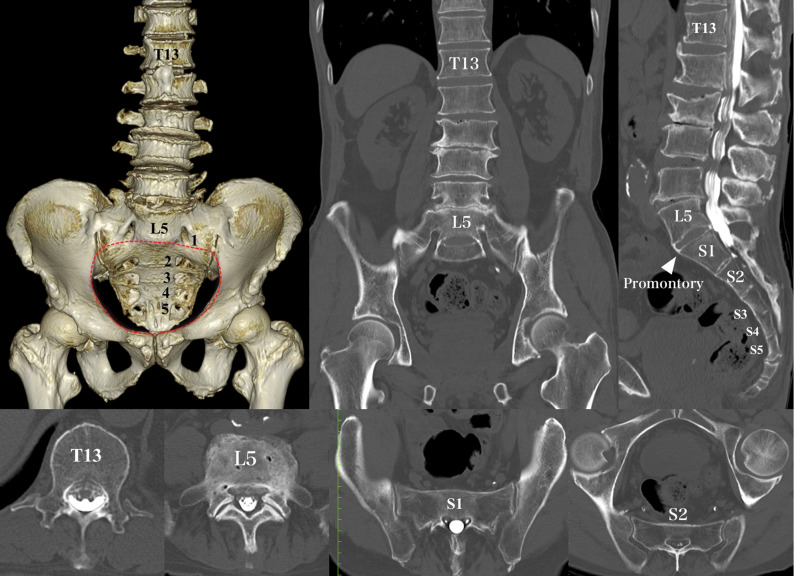
Fig. 2.
CT images demonstrating a type-IIIb LSTV case. The 3-dimensional CT image shows that bilateral L5 transverse processes fuse completely to the sacral alae, which indicates type-IIIb LSTV, and it is positioned above the arcuate line (red dotted line). In this case, the combination of presacral vertebrae is T13 and L5, bilateral dysplastic ribs of T13 are type B (hypoplastic), and the S1 upper segment has an S2-like morphology.
Fig. 3.
CT images demonstrating an S6 LSTV case. The 3-dimensional CT image and sagittal CT image show 6 sacral vertebrae and 5 sacral foramina below the promontory, indicating S6 LSTV and it is positioned below the arcuate line (red dotted line). In this case, the combination of presacral vertebrae is T13 and L4, and bilateral dysplastic ribs of T13 are type B (hypoplastic). The S1 upper segment has an L5-like morphology as the upper segment seems to have the equivalent of a transverse process and does not articulate with the ilium, whereas the S2 level appears normal.
Fig. 4.
Lateral pelvic radiographs. The left panel shows a Castellvi type-IIIb LSTV case, and the right panel shows an S6 LSTV case. The white triangle indicates each LSTV.
We investigated the morphology of the S1 upper segment of each LSTV type on axial CT images to assess any differences between them. To determine the difference between type-IIIb LSTV and S6 LSTV, we measured the anterior lumbosacral transitional angle according to the definition shown in Figure 5. If the angle is measured as a positive value due to the lordotic nature, the transitional anatomy resembles normal L5-S1. If the angle is measured as a negative value due to the kyphotic nature, the transitional anatomy resembles normal S1-S2.
Fig. 5.
The anterior lumbosacral transitional angle is defined as the angle between 2 lines drawn along the anterior cortex of LSTV and that of the vertebra below. Left: type-IIIb LSTV with a positive angle. Right: S6 LSTV with a negative angle.
Statistical Analysis
Descriptive statistics are expressed as the mean and the standard deviation. A 2-tailed unpaired Student t test was used for comparisons between the 2 groups. Significance was set at p < 0.05. All statistical analyses were conducted using SPSS Statistics version 24 (IBM).
Source of Funding
This study did not receive any funding.
Results
In this study, 124 (14.1%) of 880 patients had transitional vertebrae and/or vertebral numeric variation, with a mean age (and standard deviation) of 69.7 ± 12.0 years and male patients accounting for 60.5% of these 124 patients. These 124 patients had no vertebral numerical variation in the cervical spine. The frequency distribution of TLTV and LSTV is shown in Table I. LSTV was observed in 111 (12.6%) of 880 patients, with type-III LSTV being the most frequent (42 [37.8%] of 111), followed by S6 LSTV (37 [33.3%] of 111). Of these 111 patients with LSTV, an association with TLTV was observed in 87 patients (78.4%). Of these 87 patients, 28 (32.2%) had TLTV at T12 and 59 (67.8%) had TLTV at T13. Patients with type-III LSTV did not have 23 presacral vertebrae; 29 (69.1%) of these 42 patients had 25 presacral vertebrae (increased number of presacral vertebrae). Patients with S6 LSTV did not have 25 presacral vertebrae; 30 (81.1%) of these 37 patients had 24 presacral vertebrae (the standard number of presacral vertebrae). The most frequent combinations of presacral vertebral numbers were T13 and L5 with TLTV in patients with type-III LSTV (26 [61.9%] of 42) and T13 and L4 with TLTV in patients with S6 LSTV (21 [56.8%] of 37). As for non-LSTV, the most frequent combination was T13 and L5 with TLTV (7 [53.9%] of 13). Only 2 (0.23%) of 880 patients had bilateral normal ribs at T13.
TABLE I.
Frequency Distribution of TLTV and LSTV
| No. of Patients | TLTV* (N = 96) | Non-TLTV*(N = 28) | ||||||
|---|---|---|---|---|---|---|---|---|
| No. of Presacral Vertebrae† | No. of Presacral Vertebrae‡ | |||||||
| 23 | 24 | 25 | 24 | 25 | ||||
| T12 and L4 | T12 and L5 | T13 and L4 | T13 and L5 | T12 and L5 | T12 and L6 | T13 and L5 | ||
| LSTV | 111 | 7 | 21 | 23 | 36 | 17 | 6 | 1 |
| Castellvi type II | 28 | 0 | 10 | 1 | 10 | 5 | 1 | 1 |
| Castellvi type III | 42 | 0 | 9 | 1 | 26 | 3 | 3 | 0 |
| Castellvi type IV | 4 | 0 | 2 | 0 | 0 | 0 | 2 | 0 |
| S6 | 37 | 7 | 0 | 21 | 0 | 9 | 0 | 0 |
| Non-LSTV | 13 | 0 | 1 | 1 | 7 | 0 | 3 | 1 |
| Total§ | 124 | 7 | 22 | 24 | 43 | 17 | 9 | 2 |
The values are given as the number of patients.
The number of vertebrae is counted from C2; there are 87 patients in the LSTV group and 9 patients in the non-LSTV group.
The number of vertebrae is counted from C2; there are 24 patients in the LSTV group and 4 patients in the non-LSTV group.
The numbers represent the sum of LSTVs and non-LSTVs.
The frequency distribution of dysplastic rib types at the TLTV is shown in Table II. TLTV was observed in 96 (10.9%) of 880 patients; of these 96 patients, 3 had 1 normal rib on 1 side. Patients with type-II LSTV most frequently had type A (18 [42.9%] of 42), whereas patients with type-III LSTV had types B (29 [40.3%] of 72) and C (30 [41.7%] of 72) at approximately the same frequency. Patients with S6 LSTV most frequently had type C (34 [60.7%] of 56).
TABLE II.
Frequency Distribution of Dysplastic Rib Types in TLTVs (Excluding Non-TLTVs)
| No. of Patients | With Ribs or Rib Equivalents (sides) | Without Ribs(sides) | Total (sides) | |||
|---|---|---|---|---|---|---|
| Normal | Type A | Type B | Type C | |||
| LSTV | 87 | 3 | 36 | 62 | 73 | 174 |
| Castellvi type II | 21 | 1 | 18 | 14 | 9 | 42 |
| Castellvi type III | 36 | 1 | 12 | 29 | 30 | 72 |
| Castellvi type IV | 2 | 1 | 1 | 2 | 0 | 4 |
| S6 | 28 | 0 | 5 | 17 | 34 | 56 |
| Non-LSTV | 9 | 0 | 1 | 9 | 8 | 18 |
| Total* | 96 | 3 | 37 | 71 | 81 | 192 |
The numbers represent the sum of LSTVs and non-LSTVs.
The morphology of the S1 upper segment of each LSTV type, including non-LSTV, was investigated on axial CT images (Table III). Regarding morphology, L5-like appearances were most frequently observed in patients with S6 LSTV (Fig. 3), whereas S2-like appearances were most frequently observed in patients with Castellvi LSTVs and non-LSTV (Fig. 2). The clinical implications of these results are important, especially when planning S2-alar-iliac screw placement. Unlike patients with S6 LSTV, patients with type-III LSTV required S2-alar-iliac screw placement from the S1 level with S2-like appearance (Fig. 6).
Fig. 6.
CT images after S2-alar-iliac screw placement. The left panels show a Castellvi type-IIIb LSTV case with the screw inserted from the S1 level, and the right panels show an S6 LSTV case with the screw inserted from the S2 level.
TABLE III.
Morphology of the S1 Upper Segment*
| No. of Patients | Normal S1 | L5-Like† | S2-Like | |
|---|---|---|---|---|
| LSTV | 111 | 4 | 36 | 71 |
| Castellvi type II | 28 | 3 | 0 | 25 |
| Castellvi type III | 42 | 0 | 0 | 42 |
| Castellvi type IV | 4 | 0 | 0 | 4 |
| S6 | 37 | 1 | 36 | 0 |
| Non-LSTV | 13 | 4 | 0 | 9 |
| Total‡ | 124 | 8 | 36 | 80 |
The values are given as the number of patients.
L5-like may be L4 or L6, depending on the case.
The numbers represent the sum of LSTVs and non-LSTVs.
Of the 42 patients with type-III LSTV, 33 had type-IIIb LSTV. The anterior lumbosacral transitional angle (Fig. 5) in these patients with type-IIIb LSTV and 37 patients with S6 LSTV were statistically analyzed. The mean angle was 26.2° ± 8.5° in patients with type-IIIb LSTV and 2.7° ± 10.1° in patients with S6 LSTV, with a significant difference between these patients (mean difference, 23.5° [95% confidence interval, 19.0° to 28.0°]; p < 0.001).
Discussion
In this study, we investigated the incidence of TLTV and LSTV and examined their anatomical features on CT images. The most frequent LSTV type was type-III LSTV, followed by S6 LSTV. TLTV coexisted with LSTV at a high incidence, and the converse was also true.
TLTV has been less well investigated than LSTV. Studies on TLTV have employed Wigh’s definition of TLTV as a vertebra with a rib length of ≤3.8 cm16. This study showed that the incidence of TLTV was 10.9%. Park et al. reported that the incidence of TLTV was 12.6%17. In contrast, Carrino et al. reported that the incidence of TLTV was 4.1%, and the rate of TLTV coexisting with LSTV was 2.7%18. If focusing solely on the rib length, the presence of TLTV may be missed. To avoid overlooking TLTV and the accompanying dysplastic ribs, we clarified the definition of the lowest thoracic vertebra and identified TLTV using CT images. Type-A dysplastic ribs (short ribs) exceed 3.8 cm in length and have been classified as normal in previous studies16-18. However, type-A TLTV had hypoplastic rib heads, unlike normal thoracic vertebrae, and was strongly associated with LSTV. Type-C TLTV (with a missing rib) was the most frequent TLTV observed in this study and had hypoplastic transverse processes, which were different from the lumbar processes. Particularly, types B and C can be thought to be L1 on radiographs, affecting vertebral numbering and the measurements of lumbar lordosis and thoracic kyphosis.
The Castellvi classification system is based on the coronal images of LSTV but not on the sagittal or axial images. As non-type-IIIb LSTVs do not completely fuse with the sacrum, they can be easily identified solely from frontal 3-dimensional CT images and are recognized as the lowest lumbar vertebra. However, distinguishing type-IIIb LSTV from our newly proposed S6 LSTV is complex. Even with 3-dimensional CT, both type-IIIb LSTV and S6 LSTV appear like S1 and may not be easily distinguishable. A review of LSTV by Konin and Walz separately introduced the terms “lumbarized S1” and “sacralized L5” from the Castellvi classification3. “Lumbarized S1” likely applies to type-IIIb LSTV, whereas “sacralized L5” may correspond to S6 LSTV; nonetheless, both terms are misleading. If S1 is lumbarized, the number of sacral vertebrae may be decreased to 4. If L5 is sacralized, the number of sacral vertebrae may be increased to 6, and the number of presacral vertebrae may be decreased. To clarify this, we counted the number of sacral vertebrae and sacral foramina based on the location of the promontory on the arcuate line of the ilium on CT images. Type-IIIb LSTV had the promontory below it; therefore, this LSTV corresponded to the lowest vertebra and the number of sacral vertebrae was not decreased. S6 LSTV had the promontory above it; therefore, this corresponded to S1 and the number of sacral vertebrae was increased (6, including itself). However, 81.1% of patients with S6 LSTV did not show a reduced number of presacral vertebrae. Therefore, the terms “lumbarized S1” and “sacralized L5” may not apply to the actual situation, and LSTV should be evaluated with a focus on the anatomical location.
A significant difference in the anterior lumbosacral transitional angle was observed between patients with type-IIIb LSTV and S6 LSTV. The angle in type-IIIb LSTV was lordotic, and its transitional anatomy resembled normal L5-S1, whereas the angle in S6 LSTV ranged from hypolordotic to kyphotic, and its transitional anatomy resembled normal S1-S2. Investigation of the S1 upper segment of each LSTV type demonstrated the difference between S6 LSTV and Castellvi LSTVs from a different perspective. On axial CT images, the S1 upper segment appeared as L5 for S6 LSTV and as S2 for Castellvi LSTVs. Nevertheless, when inserting S2-alar-iliac screws, treating S2 (the vertebra below S6 LSTV) as the true S2 in patients with S6 LSTV would be clinically less problematic (Fig. 6). Similarly, in patients with Castellvi LSTVs, particularly those with type-IIIb LSTV, considering S1 (the vertebra below type-IIIb LSTV) as the true S2 would be clinically beneficial, even if this LSTV corresponds to the lowest lumbar vertebra. In a patient series analyzed by Tatara et al., preoperative planning with navigation software required S2-alar-iliac screws to be inserted from S1 in all patients with Castellvi type-IIIb LSTV19.
Regarding vertebral numbering, TLTV was most frequently identified at T13, with the highest incidence of dysplastic rib types B and C. The most frequent combinations of presacral vertebral numbers were T13 and L5 in patients with type-III LSTV and T13 and L4 in patients with S6 LSTV. Even if the dysplastic rib types B and C of T13 caused it to be considered L1, the number of lumbar vertebrae in patients with S6 LSTV would be recognized as 5; thus, presacral vertebral enumeration problems may not have a serious clinical impact. Conversely, the number of lumbar vertebrae in patients with type-IIIb LSTV will vary depending on whether type-IIIb LSTV is considered the lowest lumbar vertebra or S1, but knowledge of how type-IIIb LSTV appears on CT images can help reduce misnumbering of lumbar vertebrae.
This study had several limitations. Thoracolumbar CT images that included the coccyx were obtained, and the number of sacral vertebrae and sacral foramina was counted accurately. The coccyx is usually composed of 3 to 5 vertebrae, but enumeration is challenging. Further, it should be kept in mind that sacralization of the coccyx may have contributed to S6 LSTV. Anatomical studies are essential to investigate the relationship between the lumbar spine with TLTV and/or LSTV and the branching pattern of the lumbar plexus. The presence of TLTV and LSTV may noticeably impact the measurement of spinopelvic parameters; these measurements are naturally reflected in the outcomes of spinal deformity surgery. This study did not clarify the optimal approach for measuring these parameters, which should be addressed in future studies.
In conclusion, although LSTV has both L5 and S1 elements, Castellvi LSTVs have a higher proportion of L5 elements than S1 elements; it is vice versa for S6 LSTV. The S1 upper segment of Castellvi LSTVs appeared as S2 on axial CT images; therefore, particularly for type-IIIb LSTV, considering S1 as S2 is clinically less problematic. Although TLTV has both T12 and L1 elements, TLTV is likely to be considered L1 on radiographs because of its association with the rudimentary rib. However, given the high incidence of TLTV coexisting with LSTV, monitoring TLTV would aid in reducing vertebral numbering errors. The 3-dimensional CT images are suitable for detecting transitional vertebrae, and our findings may contribute to reducing the incidences of wrong-site surgery and diagnostic errors in patients with these conditions.
Acknowledgments
Note: The authors thank Editage for their English language editing.
Footnotes
Investigation performed at the Spine Center, Yokohama Minami Kyosai Hospital, Kanagawa, Japan
Disclosure: The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSOA/A289).
References
- 1.Malanga GA, Cooke PM. Segmental anomaly leading to wrong level disc surgery in cauda equina syndrome. Pain Physician. 2004. January;7(1):107-10. [PubMed] [Google Scholar]
- 2.Mody MG, Nourbakhsh A, Stahl DL, Gibbs M, Alfawareh M, Garges KJ. The prevalence of wrong level surgery among spine surgeons. Spine (Phila Pa 1976). 2008. January 15;33(2):194-8. [DOI] [PubMed] [Google Scholar]
- 3.Konin GP, Walz DM. Lumbosacral transitional vertebrae: classification, imaging findings, and clinical relevance. AJNR Am J Neuroradiol. 2010. November;31(10):1778-86. Epub 2010 Mar 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ammerman JM, Ammerman MD, Dambrosia J, Ammerman BJ. A prospective evaluation of the role for intraoperative x-ray in lumbar discectomy. Predictors of incorrect level exposure. Surg Neurol. 2006. November;66(5):470-3, discussion 473-4. [DOI] [PubMed] [Google Scholar]
- 5.Schwab FJ, Blondel B, Bess S, Hostin R, Shaffrey CI, Smith JS, Boachie-Adjei O, Burton DC, Akbarnia BA, Mundis GM, Ames CP, Kebaish K, Hart RA, Farcy JP, Lafage V; International Spine Study Group (ISSG). Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine (Phila Pa 1976). 2013. June 1;38(13):E803-12. [DOI] [PubMed] [Google Scholar]
- 6.Crawford CH, 3rd, Glassman SD, Gum JL, Carreon LY. Conflicting calculations of pelvic incidence and pelvic tilt secondary to transitional lumbosacral anatomy (lumbarization of S-1): case report. J Neurosurg Spine. 2017. January;26(1):45-9. Epub 2016 Aug 5. [DOI] [PubMed] [Google Scholar]
- 7.Khalsa AS, Mundis GM, Jr, Yagi M, Fessler RG, Bess S, Hosogane N, Park P, Than KD, Daniels A, Iorio J, Ledesma JB, Tran S, Eastlack RK; International Spine Study Group. Variability in assessing spinopelvic parameters with lumbosacral transitional vertebrae: inter- and intraobserver reliability among spine surgeons. Spine (Phila Pa 1976). 2018. June 15;43(12):813-6. [DOI] [PubMed] [Google Scholar]
- 8.Zhou PL, Moon JY, Tishelman JC, Errico TJ, Protopsaltis TS, Passias PG, Buckland AJ. Interpretation of spinal radiographic parameters in patients with transitional lumbosacral vertebrae. Spine Deform. 2018. Sep-Oct;6(5):587-92. [DOI] [PubMed] [Google Scholar]
- 9.Castellvi AE, Goldstein LA, Chan DP. Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects. Spine (Phila Pa 1976). 1984. Jul-Aug;9(5):493-5. [DOI] [PubMed] [Google Scholar]
- 10.Lian J, Levine N, Cho W. A review of lumbosacral transitional vertebrae and associated vertebral numeration. Eur Spine J. 2018. May;27(5):995-1004. Epub 2018 Mar 21. [DOI] [PubMed] [Google Scholar]
- 11.Paik NC, Lim CS, Jang HS. Numeric and morphological verification of lumbosacral segments in 8280 consecutive patients. Spine (Phila Pa 1976). 2013. May 1;38(10):E573-8. [DOI] [PubMed] [Google Scholar]
- 12.Nakajima A, Usui A, Hosokai Y, Kawasumi Y, Abiko K, Funayama M, Saito H. The prevalence of morphological changes in the thoracolumbar spine on whole-spine computed tomographic images. Insights Imaging. 2014. February;5(1):77-83. Epub 2013 Sep 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ropars F, Mesrar J, Ognard J, Querellou S, Rousset J, Garetier M. Psoas proximal insertion as a simple and reliable landmark for numbering lumbar vertebrae on MRI of the lumbar spine. Eur Radiol. 2019. May;29(5):2608-15. Epub 2018 Nov 9. [DOI] [PubMed] [Google Scholar]
- 14.Kawakami N, Tsuji T, Imagama S, Lenke LG, Puno RM, Kuklo TR; Spinal Deformity Study Group. Classification of congenital scoliosis and kyphosis: a new approach to the three-dimensional classification for progressive vertebral anomalies requiring operative treatment. Spine (Phila Pa 1976). 2009. August 1;34(17):1756-65. [DOI] [PubMed] [Google Scholar]
- 15.Neil RB, Jeremiah CH. Posterior abdominal wall and retroperitoneum. In: Susan S, editor. Gray’s anatomy. 39th ed. London: Elsevier; 2005. p 1114-6. [Google Scholar]
- 16.Wigh RE. The thoracolumbar and lumbosacral transitional junctions. Spine (Phila Pa 1976). 1980. May-Jun;5(3):215-22. [DOI] [PubMed] [Google Scholar]
- 17.Park SK, Park JG, Kim BS, Huh JD, Kang H. Thoracolumbar junction: morphologic characteristics, various variants and significance. Br J Radiol. 2016. August;89(1064):20150784. Epub 2016 Jan 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carrino JA, Campbell PD, Jr, Lin DC, Morrison WB, Schweitzer ME, Flanders AE, Eng J, Vaccaro AR. Effect of spinal segment variants on numbering vertebral levels at lumbar MR imaging. Radiology. 2011. April;259(1):196-202. [DOI] [PubMed] [Google Scholar]
- 19.Tatara Y, Niimura T, Sekiya T, Mihara H. Extra-articular portion of the sacroiliac joint-between the sacral and pelvic tuberosities: an anatomical guide for the S2-alar-iliac screw trajectory. Global Spine J. 2021. April;11(3):305-11. Epub 2020 Feb 3. [DOI] [PMC free article] [PubMed] [Google Scholar]