Abstract
OBJECTIVES:
Positive end-expiratory pressure and tidal volume may have a key role for the outcome of patients with acute respiratory distress syndrome. The variety of acute respiratory distress syndrome phenotypes implies personalization of those settings. To guide personalized positive end-expiratory pressure and tidal volume, physicians need to have an in-depth understanding of the physiologic effects and bedside methods to measure the extent of these effects. In the present article, a step-by-step physiologic approach to select personalized positive end-expiratory pressure and tidal volume at the bedside is described.
DATA SOURCES:
The present review is a critical reanalysis of the traditional and latest literature on the topic.
STUDY SELECTION:
Relevant clinical and physiologic studies on positive end-expiratory pressure and tidal volume setting were reviewed.
DATA EXTRACTION:
Reappraisal of the available physiologic and clinical data.
DATA SYNTHESIS:
Positive end-expiratory pressure is aimed at stabilizing alveolar recruitment, thus reducing the risk of volutrauma and atelectrauma. Bedside assessment of the potential for lung recruitment is a preliminary step to recognize patients who benefit from higher positive end-expiratory pressure level. In patients with higher potential for lung recruitment, positive end-expiratory pressure could be selected by physiology-based methods balancing recruitment and overdistension. In patients with lower potential for lung recruitment or in shock, positive end-expiratory pressure could be maintained in the 5–8 cm H2O range. Tidal volume induces alveolar recruitment and improves gas exchange. After setting personalized positive end-expiratory pressure, tidal volume could be based on lung inflation (collapsed lung size) respecting safety thresholds of static and dynamic lung stress. Positive end-expiratory pressure and tidal volume could be kept stable for some hours in order to allow early recognition of changes in the clinical course of acute respiratory distress syndrome but also frequently reassessed to avoid crossing of safety thresholds.
CONCLUSIONS:
The setting of personalized positive end-expiratory pressure and tidal volume based on sound physiologic bedside measures may represent an effective strategy for treating acute respiratory distress syndrome patients.
Keywords: acute respiratory distress syndrome, personalized medicine, protective ventilation, recruitment, ventilator-induced lung injury
Fine-tuning of mechanical ventilation settings may be a life-saving treatment for acute respiratory distress syndrome (ARDS) (1, 2). Since the very first clinical description of ARDS, Ashbaugh et al (3) reported lower mortality in patients treated with positive end-expiratory pressure (PEEP) or sigh breaths. The role of protective ventilation combining PEEP and low tidal volume (VT) (4) to minimize the risk of ventilator-induced lung injury (VILI) (5) is now well established (6).
Subsequent studies failed to find the average PEEP and VT values that could further reduce mortality (7–11). Thus, application of evidence-based medicine in this field may be complicated; for example, patients with severe ARDS may benefit from higher PEEP, but this was demonstrated through pooled analysis of studies using very different methods to select PEEP (7–9). The selection of low VT can result in similar conflicting methods to size it (predicted body weight [PBW] vs driving pressure).
As average values from randomized controlled trials (RCTs) are currently lacking, the author reasoned that a bedside physiologic understanding of the individual patient might guide the selection of PEEP and VT. Recent studies introduced ARDS phenotypes based on radiological findings (12) or inflammation and clinical data (13) to guide personalized ventilation management. Those findings advocate for personalized titration of PEEP and VT to fully exploit their protective effects.
PERSONALIZED PEEP
Physiologic Effects of PEEP
The ARDS lungs (14) are characterized by heterogenous collapse of gravity-dependent and highly inflamed zones, which induces a reduction of the respiratory system compliance (CRS). Alveolar collapse represents one of the main triggers for the detrimental effects of ventilation. Smaller functional lung volume determining lower compliance requires higher inspiratory pressure (transpulmonary pressure: ΔPL), which induces larger parenchymal stress (barotrauma) (15). Excessive and repeated lung stress is associated with lung damage (16) and poorer prognosis (17). Lung damage is also proportional to the ratio between VT and the collapsed lung (volutrauma), and the smaller the denominator, the higher the risk of VILI. Finally, larger alveolar collapse increases the number of lung units at risk of cyclic opening and closing during tidal breathing (atelectrauma).
Increasing the size of the collapsed lung through stable alveolar recruitment may dampen these effects, thus representing a key goal of the ventilatory management of ARDS.
Once recruited by higher inspiratory pressure, PEEP keeps the lungs open (18, 19), stabilizing recruitment. PEEP provides protection against lung collapse (20) and alveolar flooding by inflammatory edema (18). The recruited lung units react to tidal ventilation, increase the collapsed lung size, and break the vicious cycle of baro-, volu- and atelectrauma, promoting lung healing (21) (Table 1). PEEP stabilizes recruitment by granting an end-expiratory pressure higher than the alveolar and/or airway closing pressures (20), which are usually higher in the dependent areas (22).
TABLE 1.
Physiologic Effects of Positive End-Expiratory Pressure and Tidal Volume
| Physiologic Effects | Positive End-Expiratory Pressure | Tidal Volume |
|---|---|---|
| Beneficial effects | Recruitment by higher inspiratory pressure | Improved Co2 clearance by dead space washout |
| Larger baby lung size | Recruitment stabilization | |
| Alveoli stabilization | Surfactant production | |
| Reduced volutrauma | ||
| Reduced atelectrauma | ||
| Adverse effects | Alveolar overdistension | Alveolar overdistension |
| Barotrauma | Volutrauma | |
| Hemodynamic impairment | Barotrauma |
When PEEP stabilizes recruitment (23), atelectrauma (24), inflammation (25) and alveolar damage (26) are reduced, and often, oxygenation improves. In ARDS, appropriate application of PEEP may also be an efficient way to reduce the ventilation-perfusion mismatch (27).
Nevertheless, PEEP carries the intrinsic risk of serious detrimental effects, amplified by the heterogeneity of ARDS lungs. When recruitability is minimal or absent, setting inadequate high PEEP may lead to hemodynamic instability (28). This adverse effect may be particularly dangerous in nonrecruitable patients with inadequate volume status (29) and risk dysfunction of the right side of the heart (30). In contrast, setting higher PEEP in recruitable patients could optimize hemodynamics (31, 32). Inappropriate high PEEP may also induce overdistension of already open lung units, with an increase in the amount of overinflated tissue in the nondependent zones (32). In extreme cases, PEEP-induced overdistension may favor barotrauma and life-threatening complications (33).
VILI is an extremely complex phenomenon, not only dependent on airway pressure but also on tissue inflammation, pulmonary blood flow, and microvascular structure as well. Furthermore, the effects of airway pressure on the lung also depend on patient position, chest wall mechanics, and the use of inspiratory muscles (5, 21). Thus, stable recruitment enabled by PEEP enhances lung protection if all other factors remain unchanged, whereas it should be reassessed if these change.
Assessing Potential for Lung Recruitment
CT scan studies taught the researchers that ARDS patients present high interindividual differences in response to PEEP (34, 35). End-expiratory CT scans performed at two PEEP levels can quantify the weight of the nonaerated lung at each level. The difference between the nonaerated lung weight at lower PEEP minus the higher PEEP value represents the weight of the recruited lung. CT-based potential for lung recruitment (PLRCT) is the weight of the recruited lung as a percentage of the total lung weight (35). Identification of patients with higher PLRCT (i.e., > 10%) represents a first step to correctly assessing the potential benefit of higher PEEP (35). However, CT is not a bedside tool, and transport to the CT room may be dangerous and labor consuming; also, repeated testing for PLRCT during the course of ARDS may be cumbersome, and patients may receive an excessive amount of radiation.
An alternative principle to measure potential for lung recruitment (PLR) at the bedside relies on differentiating the predicted versus the measured effects of PEEP on lung inflation (PLR based on lung inflation [PLRINFL]). A number of bedside techniques can measure the global change in end-expiratory lung volume (ΔEELVglobal) between two PEEP levels: namely, electrical impedance tomography (EIT) (36, 37), helium dilution technique (37, 38), oxygen or nitrogen washout-washin methods (39, 40), and the difference between expired and set VT measured by the ventilator pneumotachograph when PEEP is decreased (41, 42).
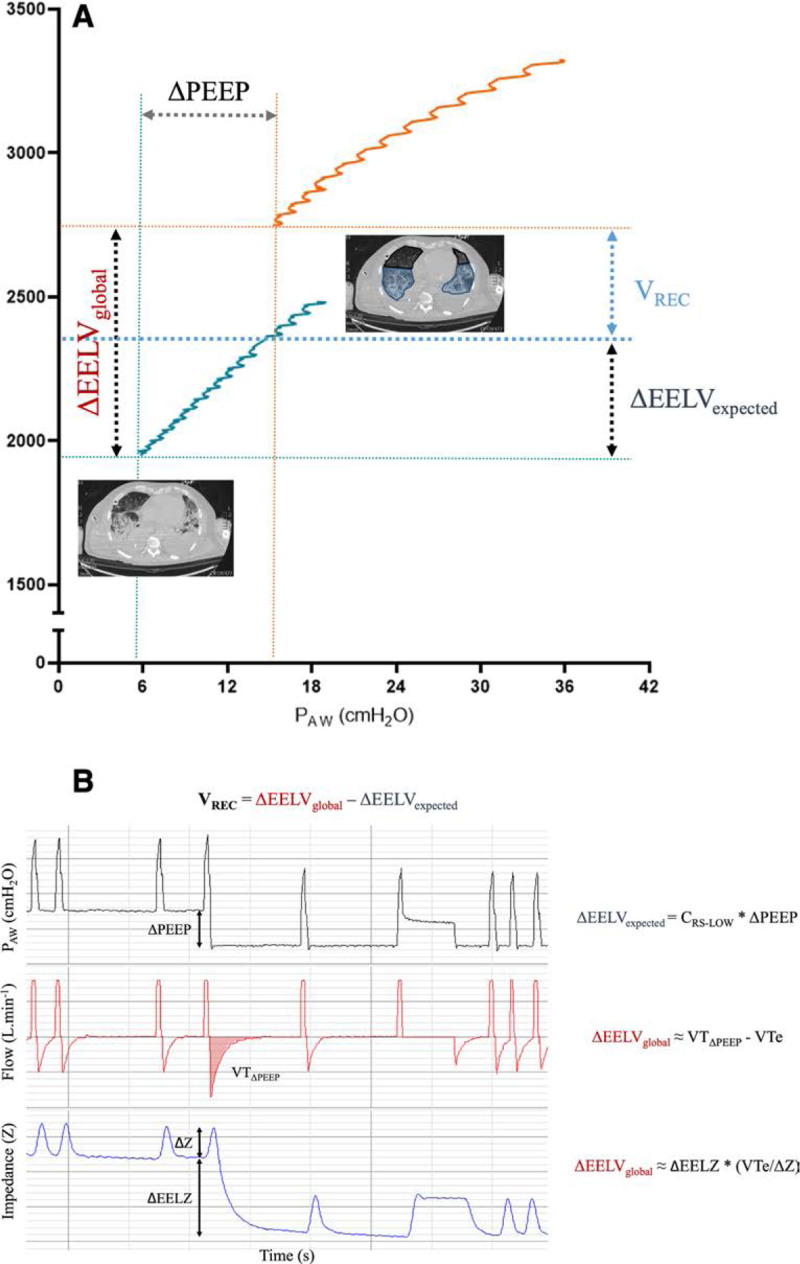
The measured ΔEELVglobal is made up of two parts (Fig. 1). First, already aerated lung regions simply inflate due to the rise in airway pressure without any recruitment, generating an expected increase in change in end-expiratory lung volume (ΔEELV) which is not associated with any change in the lung size. The increase in lung volume will equal the change in PEEP (ΔPEEP) multiplied by the CRS at a lower starting PEEP (40):
Figure 1.
Bedside assessment of the potential for lung recruitment based on lung inflation. A, Pressure-volume curves at PEEP 5 cm H2O and PEEP 15 cm H2O are built. Note the gap between the two EELVs (ΔEELVglobal) measured by the airway release method. VREC corresponds to the volume exceeding the expected increase in lung inflation from compliance at PEEP 5 cm H2O (ΔEELVexpected). CT scan results at PEEP 5 cm H2O (left panel) and 15 cm H2O (right panel) are also reported in the figure. Increased lung aeration could be related to VREC (right panel, blue areas), whereas inflation of previously aerated volume leads to higher lung volumes in the nondependent zones (right panel, black areas). B, Visual description of two methods to calculate VREC at the bedside: PAW release (top) vs electrical impedance tomography (bottom). CRS-LOW = respiratory system compliance at low positive end-expiratory pressure, EELV = end-expiratory lung volume, EELZ = end-expiratory lung impedance, PAW = airway pressure, PEEP = positive end-expiratory pressure, VREC = recruited lung volume, VTe = exhaled tidal volume, VTΔPEEP = expired tidal volume when changing from higher to lower PEEP, ΔEELVexpected = change in EELV related to lung inflation, ΔEELVglobal = global change in EELV, ΔEELZ = change in end-expiratory lung impedance, ΔPEEP = PEEP variation between the two levels, ΔZ = tidal impedance variation.
| (1) |
Second, a fraction of collapsed lung units may be recruited by the higher PEEP, resulting in an unexpected increase of ΔEELV. The larger this fraction of newly recruited units, the larger will be the improvement of the functional lung size and the reduction of the risk of VILI (38, 40). This recruited lung volume (VREC) can be measured as the part of ΔEELVglobal exceeding ΔEELVexpected (37, 40):
| (2) |
An alternative bedside method to calculate the VREC is to perform two pressure-volume curves (Fig. 1A) (40).
Once the VREC has been reached, the ratio between the size of the newly recruited lung areas divided by the size of the starting collapsed lung will be a measure of the PLRINFL (15). The size of aerated lung regions is proportional to compliance; thus, the ratio of the compliance of VREC divided by the compliance of the collapsed lung will be an estimate of PLRINFL (42, 43). A recent publication alternatively named PLRINFL as the recruitment to inflation (R/I) ratio (42):
| (3) |
A PLRINFL value greater than 0.5 is the proposed threshold for patients with higher PLRINFL. If airway opening pressure (AOP) is detected, the compliance of the recruited lung should be computed as VREC/(PEEP high−AOP) instead of VREC/ΔPEEP (42).
Another simpler and less expensive method for assessing PLR at the bedside focuses on oxygenation. The functional intrapulmonary shunt should increase with derecruitment, and researchers explored the correlation between poorer oxygenation assessed at low PEEP level with PLRCT, describing a significant association (44). Indeed, higher PEEP is beneficial when applied to patients with Pao2/Fio2 less than or equal to 200 mm Hg (45). However, the mechanisms underlying poor oxygenation vary, and in some ARDS patients, shunt may not be the most relevant, thus decreasing the specificity of this method.
More severe ARDS lung edema, which is usually associated with derecruitment and larger PLR, generates higher lung weight. When a patient is supine, the superimposed weight of the lung generates a proportional compression on the dependent region of the pleural space (46). Esophageal pressure (PES) (47) is a substitute for dependent pleural pressure (46). Thus, higher end-expiratory PES (e.g., > 10 cm H2O) is a sign of heavier ARDS lungs and higher PLR, especially in the nonobese patient. Those findings might match those recorded in a recently published study, showing a correlation between end-expiratory PES and stronger inspiratory effort, which indicates more severe respiratory failure in spontaneously breathing hypoxemic patients (48).
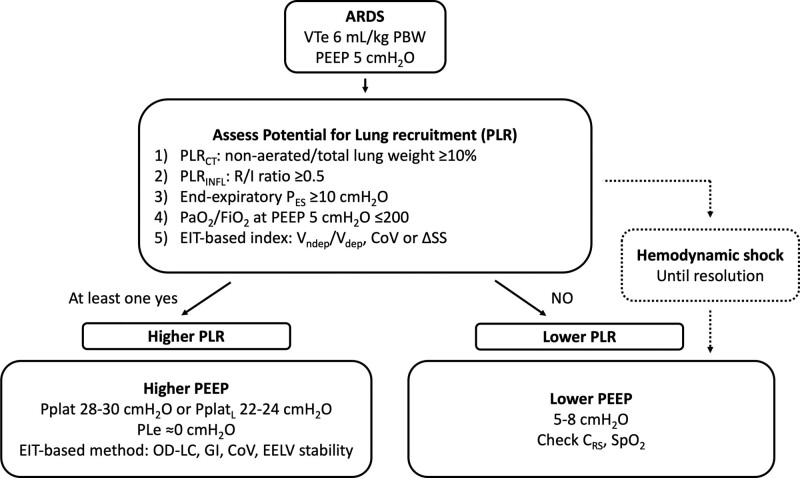
EIT is a dynamic method to assess inhomogeneity of ventilation distribution, albeit still expensive and available only in a limited number of centers. Alveolar collapse generates inhomogeneous distribution of respiratory time constants within the lungs (37, 49). Thus, larger collapse is associated with higher regional inhomogeneity indexes measured by EIT. When assessed at low PEEP levels, higher values of the following indexes may be correlated with significant PLR: 1) the ratio between gravitational nondependent and dependent VT ratios (50, 51), 2) the global inhomogeneity index, and 3) the dependent fraction of hypoventilated lung units (i.e., silent spaces) (52, 53). EIT-based lung perfusion assessment was recently introduced, and larger potential for improved ventilation-perfusion matching may become the new standard for evaluating the potential benefits of higher PEEP at the bedside (37, 54) (Fig. 2).
Figure 2.
Setting personalized positive end-expiratory pressure (PEEP) at the bedside. ARDS = acute respiratory distress syndrome, CoV = center of ventilation, CRS = respiratory system compliance, EELV = end-expiratory lung volume, EIT = electrical impedance tomography, GI = global inhomogeneity index, OD-LC = overdistension and lung collapse, PBW = predicted body weight, PES = esophageal pressure, Ple = transpulmonary expiratory pressure, PLR = potential for lung recruitment, PLRCT = CT-based PLR, PLRINFL = PLR based on lung inflation, Pplat = plateau pressure, PplatL = transpulmonary plateau pressure, R/I ratio = recruited-on-inflated lung ratio, Spo2 = peripheral oxygen saturation, SS = silent spaces, VTe = exhaled tidal volume, VDEP = dependent regions tidal volume (based on impedance tidal changes), VNDEP = nondependent regions tidal volume (based on tidal impedance changes), ΔSS = change of silent spaces at higher PEEP.
In real-life ICU care, the method for determining which patient has higher PLR may be selected based on expertise, availability of new technology, time, and staffing (Fig. 2). Smooth integration of these measures into clinical routine may be the key to improve quality, be systematic, generate clinical experience, and understand their potential.
Once PLR is assessed, despite the lack of outcome data, optimal PEEP selection in patients with higher and lower PLR might be a key clinical goal to respect lung physiology and enhance healing.
Personalized PEEP in Patients With Higher PLR
The method to set personalized PEEP in patients with higher PLR should be able to recognize the minimal (higher) PEEP able to induce recruitment without increasing the risk of overdistension.
A simple bedside method to set higher PEEP in recruitable patients is to use the higher PEEP/Fio2 table (7) as a physiologic study showed that this method selects personalized higher PEEP in recruitable lungs (55).
An end-inspiratory airway plateau pressure (Pplat) above 28–30 cm H2O increases the risk of barotrauma and is associated with poor clinical outcome (5, 56). In a large RCT, Mercat et al (9) proposed to set PEEP at the level obtaining Pplat of 28–30 cm H2O with VT 6 mL/kg PBW. The study showed that this strategy obtained a higher percentage of patients reaching unassisted breathing in moderate-to-severe ARDS. This bedside dynamic strategy represents a pragmatical compromise to set PEEP high enough to induce some recruitment while limiting the risk of overdistension. However, it also tends to assign a higher PEEP to patients with higher compliance.
PES could also help in guiding higher PEEP titration. The mechanical ventilation guided by esophageal pressure in acute lung injury study trials proposed to set PEEP based on positive ΔPL at end-expiration (11, 57): a PEEP value equal to end-expiratory PES should be the lowest one able to counteract the superimposed lung weight, thus representing the optimal balance between recruitment and minimum risk of overdistension (15, 46, 51). Another method is to set the personalized PEEP level associated with static end-inspiratory ΔPL calculated with the lung/respiratory system elastance ratio method of 22–24 cm H2O with VT 6 mL/kg PBW (58). Indeed, the static inspiratory ΔPL calculated with the elastance ratio is tightly correlated with the pressure-inducing overdistension in the nondependent ventral lung regions (58).
In recent years, several studies proposed various EIT-derived indexes for personalized higher PEEP titration. The relative percentage of lung collapse and overdistension based on change in the pixel-level compliances allows recognition of optimal higher PEEP (59). Other EIT-based techniques select higher PEEP based on regional homogeneity (50, 51, 60). Stable end-expiratory lung volume after PEEP increase may also recognize the ability of PEEP to keep the recruited lung open (61).
Personalized PEEP in Patients With Lower PLR
Patients with lower PLR are characterized by indexes of recruitability below the suggested thresholds (e.g., PLR CT below 10% or R/I ratio below 0.5) (Fig. 2). In these patients, detrimental effects of high PEEP on barotrauma and hemodynamics may exceed the benefits (20, 62, 63). A reasonably safe approach in patients with lower PLR may be to set PEEP between 5 and 8 cm H2O, with higher values for patients presenting any physiologic improvement (e.g., improved saturation and/or improved CRS). Addition of cyclic recruitment by sigh breaths and early switch to assisted ventilation may limit the risk of dorsal atelectasis at such low PEEP levels (64) (Fig. 2).
Higher PEEP levels should be avoided in patients with unstable hemodynamics also (65, 66), and patients with shock could be considered as having lower PLR (Fig. 2).
In all these conditions benefiting from lower PEEP, extracorporeal membrane oxygenation (ECMO) could be added in the case of extremely poor oxygenation.
PERSONALIZED VT
Physiologic Effects of VT
Cyclic inflation of the respiratory system by VT is associated with multiple physiologic benefits. The main function of tidal ventilation is to grant Co2 clearance, which may be impaired in the adverse conditions of high Co2 production and increased dead space of ARDS (67). Higher VT is more effective than respiratory rate to improve Co2 washout (67, 68). VT generates the higher inspiratory pressure that can reopen collapsed alveoli, and it dynamically collaborates with PEEP in stabilizing recruitment. Finally, cyclic distension by VT activates surfactant excretion to stabilize the alveoli (69) (Table 1).
However, experimental studies showed development of VILI by ventilation with (very) high VT in healthy lungs. In ARDS, inhomogeneities in ventilation distribution (34, 35) lead to tidal hyperinflation in the nondependent zones, with an increasing risk of volutrauma (32), and to increased shear forces at the interface between open and collapsed regions (15), even in the presence of “normal” VT (Table 1). Indeed, a groundbreaking clinical trial demonstrated that a VT of 6 mL/kg PBW reduced mortality of ARDS in comparison with 12 mL/kg PBW (6).
Personalized VT
In that groundbreaking trial, a lower VT set at 6 mL/kg PBW showed a clear benefit of reducing the risk of mortality, especially when associated with a strategy of higher PEEP levels (4, 6). Interestingly, previous reports did not find any association between lower VT and a decrease in the risk of mortality (71, 72).
Since that trial (6), most of the studies and clinical protocols have focused on VT settings based on PBW. The rationale of this approach is that in healthy subjects, lung volume is linearly correlated with PBW (73, 74). Although this approach represents an initial effort of physiology-based personalization, the size of the lung in ARDS patients is poorly correlated with PBW due to the variability in the extent of alveolar collapse, and patients may receive excessively high (or low) VT.
Retrospective data suggested that lower VT could be harmful for patients with high CRS (75). This may be a consequence of the observation performed by multiple physiologic studies that the normally aerated lung size in ARDS is linearly correlated with the CRS (38), so that low VT may lead to hypoventilation and derecruitment in patients with larger normally inflated lungs. Of note, a recently published retrospective analysis of large seminal cohorts showed that a VT of 6 mL/kg PBW reduces mortality in comparison with 12 mL/kg PBW only in patients with lower compliance (76).
Ideal physiologic sizing of VT in ARDS may thus be obtained through dividing VT by CRS rather than by PBW (38). Driving pressure (respiratory system driving pressure [ΔPRS], i.e., Pplat minus total PEEP) is precisely the ratio between VT and CRS, and it may represent a more accurate bedside method to titrate personalized VT in the individual patient (17). The seminal study on VILI by Webb and Tierney demonstrated reduced injury when driving pressure was decreased, even in the presence of unchanged maximal inspiratory pressure (18). Multiple large retrospective and prospective studies showed significant correlation between driving pressure and the outcome of ARDS (17, 56, 77). Airway driving pressure has limits, too: it is a single global value with no regional information; when fibrosis is present, parenchymal stiffness may be its main determinant rather than the number of ventilated units; when the chest wall is stiff, the transpulmonary driving pressure may be overestimated. In contrast, in the presence of spontaneous breathing activity, airway driving pressure can underestimate the transpulmonary one.
As a safe compromise, after identification of personalized PEEP, VT could be set at 6 mL/kg PBW by pressure-controlled breaths less than 14 cm H2O. Any subsequent improvement of compliance will lead to higher VT (and better CO2 clearance) while keeping constant safe driving pressure. However, one should be careful as hypoventilation could result from worsening compliance during pressure-control ventilation.
Respiratory rate setting will follow VT selection, as the lowest associated with acceptable pH (e.g., ≥ 7.30) (70).
Safety Thresholds for VT
Based on the proposed approach, personalized PEEP could be set using a VT of 6 mL/kg PBW, and then personalized VT be adjusted to respect the following safety thresholds.
The first simple safety criterion available at the bedside is airway end-inspiratory Pplat. Pplat reflects the maximal pressure applied to the alveoli, thus is an acceptable substitute for global stress assessment. Airway end-inspiratory Pplat should not exceed 30 cm H2O (5, 56). This value is rather arbitrary, and more recent studies on inflammation and overdistension showed that maybe a Pplat of 27 or 28 might be regarded as safer (25, 32).
Transpulmonary inspiratory Pplat calculated with the elastance ratio method represents the maximal pressure in the nondependent regions. Selecting VT above personalized PEEP that does not cross the 22–24 cm H2O limit for this pressure could be regarded as the most accurate to avoid overdistension (58).
Other studies focused on limits for the dynamic inspiratory pressure, namely the driving pressure. In a retrospective analysis of several trials, Amato et al (17) found a correlation between higher ΔPRS greater than 14 cm H2O and increased risk of mortality (56). Interestingly, a retrospective analysis of an RCT highlighted a correlation between transpulmonary ΔPRS exceeding the 8–10 cm H2O and increased risk of mortality (77).
At the bedside, the analysis of the ventilator pressure-time curve profile allows assessment of the stress index (SI) (78). The shape of the slope of the pressure-time curve from the start of inspiration to peak pressure during volume-controlled ventilation depends on dynamic changes in CRS during inspiration (79, 80). Convexity in the pressure curve (SI > 1) is due to a progressive decrease in lung compliance at higher pressure, indicating tidal hyperinflation (79, 80), which should decrease if VT is reduced.
Finally, VT could be selected to obtain a safe ratio with the actual measured end-expiratory lung volume (e.g., assessed by nitrogen washout). However, this approach is limited by expensive techniques (81) and by the unclear role of the change in volume determined by PEEP and recruitment.
An overview of bedside safety thresholds is provided in Table 2.
TABLE 2.
Bedside Assessment of Safety for VT Titration
| Physiologic Variables | Mechanism | Threshold (cm H2O) |
|---|---|---|
| Plateau pressure | Maximal pressure across the respiratory system at the end of tidal breath | 28 |
| Static total mechanical stress and barotrauma | ||
| Transpulmonary plateau pressure | Maximal pressure across the lung at the end of tidal breath | 22–24 |
| Mechanical stress and barotrauma to the lung | ||
| Driving pressure | Dynamic pressure change during tidal breath applied to the respiratory system | 14 |
| Dynamic mechanical stress and strain | ||
| Driving transpulmonary pressure | Dynamic pressure change during tidal breath applied to the lung | 8–10 |
| Dynamic mechanical stress and strain to the lung | ||
| Stress index | `Worsening of respiratory system compliance during tidal breath | 1 |
| Overdistension and barotrauma |
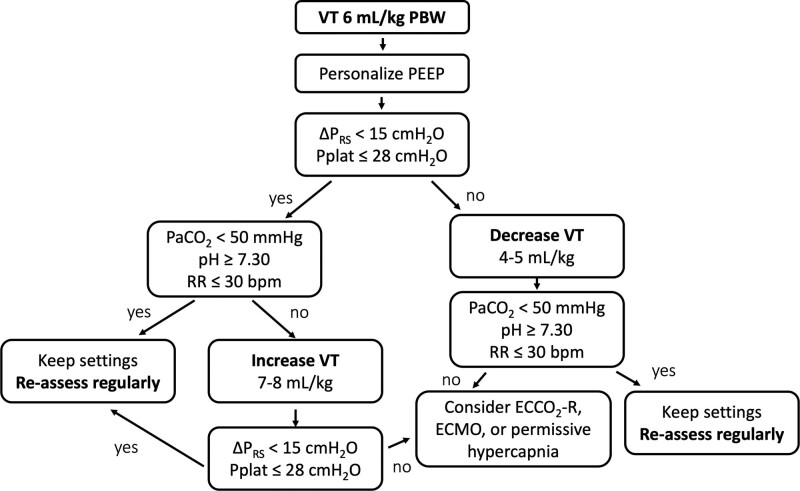
In some patients, selection of personalized PEEP and VT to stabilize recruitment while respecting safety thresholds may lead to hypercapnia and low pH (82). Addition of extracorporeal CO2 removal (ECCO2R) (83–86) or ECMO for more hypoxemic patients allows implementation of an ultraprotective strategy with high PEEP and extremely low VT (down to 2–3 mL/kg PBW). Titration of PEEP and VT during extracorporeal support could follow the same pathophysiologic approach mentioned in this article, but it also offers unique challenges due to the risk of hypoventilation (87).
After personalized PEEP and VT have been selected in the early phase of ARDS, it may be important to keep these settings for some hours to ensure early recognition of physiologic worsening or improvement. Frequent reassessment is also needed to avoid crossing of safety thresholds due to changes in the interaction between ventilation and the evolving lung injury.
CLINICAL ALGORITHMS TO SELECT PERSONALIZED PEEP AND VT
Understanding the physiology and phenotype of ARDS that most closely represents each particular patient may be the main clinical goals of the physiologic bedside measures proposed by this review. However, it is recommended that clinicians select optimal settings and evaluate the evolution of ARDS. Thus, Figures 2 and 3 summarize the proposed physiology-based path to personalize protective ventilation, incorporating some simplification to fit real-life ICU care.
Figure 3.
Setting personalized tidal volume (VT) at the bedside. ECCO2R = extracorporeal Co2 removal, ECMO = extracorporeal membrane oxygenation, PBW = predicted body weight, PEEP = positive end-expiratory pressure, Pplat = plateau pressure, RR = respiratory rate, ΔPRS = respiratory system driving pressure.
Here are the main steps: 1) assess PLR at the bedside to identify patients who will benefit from higher PEEP; 2) set higher PEEP in recruitable patients by using a physiologic bedside method and lower PEEP of 5–8 cm H2O in nonrecruiters or patients with shock; 3) size VT to the collapsed lung by reaching safe static and dynamic thresholds, 4) consider ECCO2R in hypercapnic patients; and 5) wait, reassess frequently, and ideally do not change settings for some time in order to evaluate progression of disease.
Until well-conducted large RCTs have been undertaken, safely restoring and respecting baseline physiology may represent the most reasonable goal in the treatment of ICU patients.
ACKNOWLEDGMENTS
We would like to thank Professor A. Pesenti and Drs. E. Spinelli, B. Pavlovsky, D. Grieco, I. Marongiu, and E. Scotti for their help and thoughtful reading of the article.
Footnotes
Supported, in part, by departmental funding (Ricerca corrente, Ospedale Maggiore Policlinico, Milan, Italy).
Dr. Mauri received personal fees from Drager, Fisher & Paykel Healthcare, Mindray and Bbraun, and unrestricted research grants from Drager and Fisher & Paykel Healthcare, all outside of the submitted work.
REFERENCES
- 1.Ranieri VM, Rubenfeld GD, Thompson BT, et al. ; ARDS Definition Task Force. Acute respiratory distress syndrome: The Berlin definition. JAMA 2012; 307:2526–2533 [DOI] [PubMed] [Google Scholar]
- 2.Slutsky AS. History of mechanical ventilation. From vesalius to ventilator-induced lung injury. Am J Respir Crit Care Med 2015; 191:1106–1115 [DOI] [PubMed] [Google Scholar]
- 3.Ashbaugh DG, Bigelow DB, Petty TL, et al. Acute respiratory distress in adults. Lancet 1967; 2:319–323 [DOI] [PubMed] [Google Scholar]
- 4.Amato MB, Barbas CS, Medeiros DM, et al. Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med 1998; 338:347–354 [DOI] [PubMed] [Google Scholar]
- 5.Dreyfuss D, Saumon G. Ventilator-induced lung injury: Lessons from experimental studies. Am J Respir Crit Care Med 1998; 157:294–323 [DOI] [PubMed] [Google Scholar]
- 6.Acute Respiratory Distress Syndrome Network; Brower RG, Matthay MA, Morris A, et al. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 2000; 342:1301–1308 [DOI] [PubMed] [Google Scholar]
- 7.Brower RG, Lanken PN, MacIntyre N, et al. ; National Heart, Lung, and Blood Institute ARDS Clinical Trials Network. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med 2004; 351:327–336 [DOI] [PubMed] [Google Scholar]
- 8.Meade MO, Cook DJ, Guyatt GH, et al. ; Lung Open Ventilation Study Investigators. Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome: A randomized controlled trial. JAMA 2008; 299:637–645 [DOI] [PubMed] [Google Scholar]
- 9.Mercat A, Richard JC, Vielle B, et al. ; Expiratory Pressure (Express) Study Group. Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome: A randomized controlled trial. JAMA 2008; 299:646–655 [DOI] [PubMed] [Google Scholar]
- 10.Writing Group for the Alveolar Recruitment for Acute Respiratory Distress Syndrome Trial (ART) Investigators. Effect of lung recruitment and titrated positive end-expiratory pressure (PEEP) vs. low PEEP on mortality in patients with acute respiratory distress syndrome: A randomized clinical trial. JAMA 2017; 318:1335–1345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beitler JR, Sarge T, Banner-Goodspeed VM, et al. ; EPVent-2 Study Group. Effect of titrating positive end-expiratory pressure (PEEP) with an esophageal pressure-guided strategy vs an empirical high PEEP-Fio2 strategy on death and days free from mechanical ventilation among patients with acute respiratory distress syndrome: A randomized clinical trial. JAMA 2019; 321:846–857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Constantin JM, Jabaudon M, Lefrant JY, et al. ; AZUREA Network. Personalised mechanical ventilation tailored to lung morphology versus low positive end-expiratory pressure for patients with acute respiratory distress syndrome in France (the LIVE study): A multicentre, single-blind, randomised controlled trial. Lancet Respir Med 2019; 7:870–880 [DOI] [PubMed] [Google Scholar]
- 13.Calfee CS, Delucchi K, Parsons PE, et al. ; NHLBI ARDS Network. Subphenotypes in acute respiratory distress syndrome: Latent class analysis of data from two randomised controlled trials. Lancet Respir Med 2014; 2:611–620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gattinoni L, Caironi P, Pelosi P, et al. What has computed tomography taught us about the acute respiratory distress syndrome? Am J Respir Crit Care Med 2001; 164:1701–1711 [DOI] [PubMed] [Google Scholar]
- 15.Chiumello D, Carlesso E, Cadringher P, et al. Lung stress and strain during mechanical ventilation for acute respiratory distress syndrome. Am J Respir Crit Care Med 2008; 178:346–355 [DOI] [PubMed] [Google Scholar]
- 16.Protti A, Cressoni M, Santini A, et al. Lung stress and strain during mechanical ventilation: Any safe threshold? Am J Respir Crit Care Med 2011; 183:1354–1362 [DOI] [PubMed] [Google Scholar]
- 17.Amato MB, Meade MO, Slutsky AS, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med 2015; 372:747–755 [DOI] [PubMed] [Google Scholar]
- 18.Webb HH, Tierney DF. Experimental pulmonary edema due to intermittent positive pressure ventilation with high inflation pressures. Protection by positive end-expiratory pressure. Am Rev Respir Dis 1974; 110:556–565 [DOI] [PubMed] [Google Scholar]
- 19.Richard JC, Brochard L, Vandelet P, et al. Respective effects of end-expiratory and end-inspiratory pressures on alveolar recruitment in acute lung injury. Crit Care Med 2003; 31:89–92 [DOI] [PubMed] [Google Scholar]
- 20.Crotti S, Mascheroni D, Caironi P, et al. Recruitment and derecruitment during acute respiratory failure: A clinical study. Am J Respir Crit Care Med 2001; 164:131–140 [DOI] [PubMed] [Google Scholar]
- 21.Gattinoni L, Marini JJ, Pesenti A, et al. The “baby lung” became an adult. Intensive Care Med 2016; 42:663–673 [DOI] [PubMed] [Google Scholar]
- 22.Scaramuzzo G, Spinelli E, Spadaro S, et al. Gravitational distribution of regional opening and closing pressures, hysteresis and atelectrauma in ARDS evaluated by electrical impedance tomography. Crit Care 2020; 24:622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Neumann P, Berglund JE, Fernández Mondéjar E, et al. Dynamics of lung collapse and recruitment during prolonged breathing in porcine lung injury. J Appl Physiol (1985) 1998; 85:1533–1543 [DOI] [PubMed] [Google Scholar]
- 24.Gattinoni L, Pelosi P, Crotti S, et al. Effects of positive end-expiratory pressure on regional distribution of tidal volume and recruitment in adult respiratory distress syndrome. Am J Respir Crit Care Med 1995; 151:1807–1814 [DOI] [PubMed] [Google Scholar]
- 25.Bellani G, Guerra L, Musch G, et al. Lung regional metabolic activity and gas volume changes induced by tidal ventilation in patients with acute lung injury. Am J Respir Crit Care Med 2011; 183:1193–1199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dreyfuss D, Soler P, Basset G, et al. High inflation pressure pulmonary edema. Respective effects of high airway pressure, high tidal volume, and positive end-expiratory pressure. Am Rev Respir Dis 1988; 137:1159–1164 [DOI] [PubMed] [Google Scholar]
- 27.Dueck R, Wagner PD, West JB. Effects of positive end-expiratory pressure on gas exchange in dogs with normal and edematous lungs. Anesthesiology 1977; 47:359–366 [DOI] [PubMed] [Google Scholar]
- 28.Nanas S, Magder S. Adaptations of the peripheral circulation to PEEP. Am Rev Respir Dis 1992; 146:688–693 [DOI] [PubMed] [Google Scholar]
- 29.Fougères E, Teboul JL, Richard C, et al. Hemodynamic impact of a positive end-expiratory pressure setting in acute respiratory distress syndrome: Importance of the volume status. Crit Care Med 2010; 38:802–807 [DOI] [PubMed] [Google Scholar]
- 30.Mekontso Dessap A, Boissier F, Charron C, et al. Acute cor pulmonale during protective ventilation for acute respiratory distress syndrome: Prevalence, predictors, and clinical impact. Intensive Care Med 2016; 42:862–870 [DOI] [PubMed] [Google Scholar]
- 31.De Santis Santiago R, Teggia Droghi M, Fumagalli J, et al. High pleural pressure prevents alveolar over-distension and hemodynamic collapse in ARDS with class III obesity. Am J Respir Crit Care Med 2020; 203:575–584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Terragni PP, Rosboch G, Tealdi A, et al. Tidal hyperinflation during low tidal volume ventilation in acute respiratory distress syndrome. Am J Respir Crit Care Med 2007; 175:160–166 [DOI] [PubMed] [Google Scholar]
- 33.Boussarsar M, Thierry G, Jaber S, et al. Relationship between ventilatory settings and barotrauma in the acute respiratory distress syndrome. Intensive Care Med 2002; 28:406–413 [DOI] [PubMed] [Google Scholar]
- 34.Gattinoni L, Pesenti A, Bombino M, et al. Relationships between lung computed tomographic density, gas exchange, and PEEP in acute respiratory failure. Anesthesiology 1988; 69:824–832 [DOI] [PubMed] [Google Scholar]
- 35.Gattinoni L, Caironi P, Cressoni M, et al. Lung recruitment in patients with the acute respiratory distress syndrome. N Engl J Med 2006; 354:1775–1786 [DOI] [PubMed] [Google Scholar]
- 36.Scaramuzzo G, Spadaro S, Dalla Corte F, et al. Personalized positive end-expiratory pressure in acute respiratory distress syndrome: Comparison between optimal distribution of regional ventilation and positive transpulmonary pressure. Crit Care Med 2020; 48:1148–1156 [DOI] [PubMed] [Google Scholar]
- 37.Mauri T, Eronia N, Turrini C, et al. Bedside assessment of the effects of positive end-expiratory pressure on lung inflation and recruitment by the helium dilution technique and electrical impedance tomography. Intensive Care Med 2016; 42:1576–1587 [DOI] [PubMed] [Google Scholar]
- 38.Gattinoni L, Pesenti A, Avalli L, et al. Pressure-volume curve of total respiratory system in acute respiratory failure. Computed tomographic scan study. Am Rev Respir Dis 1987; 136:730–736 [DOI] [PubMed] [Google Scholar]
- 39.Olegård C, Söndergaard S, Houltz E, et al. Estimation of functional residual capacity at the bedside using standard monitoring equipment: A modified nitrogen washout/washin technique requiring a small change of the inspired oxygen fraction. Anesth Analg 2005; 101:206–212 [DOI] [PubMed] [Google Scholar]
- 40.Dellamonica J, Lerolle N, Sargentini C, et al. PEEP-induced changes in lung volume in acute respiratory distress syndrome. Two methods to estimate alveolar recruitment. Intensive Care Med 2011; 37:1595–1604 [DOI] [PubMed] [Google Scholar]
- 41.Chen L, Chen GQ, Shore K, et al. Implementing a bedside assessment of respiratory mechanics in patients with acute respiratory distress syndrome. Crit Care 2017; 21:84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen L, Del Sorbo L, Grieco DL, et al. Potential for lung recruitment estimated by the recruitment-to-inflation ratio in acute respiratory distress syndrome. A clinical trial. Am J Respir Crit Care Med 2020; 201:178–187 [DOI] [PubMed] [Google Scholar]
- 43.Mauri T, Spinelli E, Scotti E, et al. Potential for lung recruitment and ventilation-perfusion mismatch in patients with the acute respiratory distress syndrome from coronavirus disease 2019. Crit Care Med 2020; 48:1129–1134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Caironi P, Carlesso E, Cressoni M, et al. Lung recruitability is better estimated according to the Berlin definition of acute respiratory distress syndrome at standard 5 cm H2O rather than higher positive end-expiratory pressure: A retrospective cohort study. Crit Care Med 2015; 43:781–790 [DOI] [PubMed] [Google Scholar]
- 45.Briel M, Meade M, Mercat A, et al. Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: Systematic review and meta-analysis. JAMA 2010; 303:865–873 [DOI] [PubMed] [Google Scholar]
- 46.Yoshida T, Amato MBP, Grieco DL, et al. Esophageal manometry and regional transpulmonary pressure in lung injury. Am J Respir Crit Care Med 2018; 197:1018–1026 [DOI] [PubMed] [Google Scholar]
- 47.Mauri T, Yoshida T, Bellani G, et al. ; PLeUral pressure working Group (PLUG—Acute Respiratory Failure section of the European Society of Intensive Care Medicine). Esophageal and transpulmonary pressure in the clinical setting: Meaning, usefulness and perspectives. Intensive Care Med 2016; 42:1360–1373 [DOI] [PubMed] [Google Scholar]
- 48.Grieco DL, Menga LS, Conti G, et al. Reply to Spinelli and Mauri: Lung and diaphragm protection during noninvasive respiratory support. Am J Respir Crit Care Med 2020; 201:876–878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Victorino JA, Borges JB, Okamoto VN, et al. Imbalances in regional lung ventilation: A validation study on electrical impedance tomography. Am J Respir Crit Care Med 2004; 169:791–800 [DOI] [PubMed] [Google Scholar]
- 50.Mauri T, Bellani G, Confalonieri A, et al. Topographic distribution of tidal ventilation in acute respiratory distress syndrome: Effects of positive end-expiratory pressure and pressure support. Crit Care Med 2013; 41:1664–1673 [DOI] [PubMed] [Google Scholar]
- 51.Yoshida T, Piraino T, Lima CAS, et al. Regional ventilation displayed by electrical impedance tomography as an incentive to decrease positive end-expiratory pressure. Am J Respir Crit Care Med 2019; 200:933–937 [DOI] [PubMed] [Google Scholar]
- 52.Ukere A, März A, Wodack KH, et al. Perioperative assessment of regional ventilation during changing body positions and ventilation conditions by electrical impedance tomography. Br J Anaesth 2016; 117:228–235 [DOI] [PubMed] [Google Scholar]
- 53.Spadaro S, Mauri T, Böhm SH, et al. Variation of poorly ventilated lung units (silent spaces) measured by electrical impedance tomography to dynamically assess recruitment. Crit Care 2018; 22:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Perier F, Tuffet S, Maraffi T, et al. Effect of positive end-expiratory pressure and proning on ventilation and perfusion in COVID-19 acute respiratory distress syndrome. Am J Respir Crit Care Med 2020; 202:1713–1717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chiumello D, Cressoni M, Carlesso E, et al. Bedside selection of positive end-expiratory pressure in mild, moderate, and severe acute respiratory distress syndrome. Crit Care Med 2014; 42:252–264 [DOI] [PubMed] [Google Scholar]
- 56.Laffey JG, Bellani G, Pham T, et al. ; LUNG SAFE Investigators and the ESICM Trials Group. Potentially modifiable factors contributing to outcome from acute respiratory distress syndrome: The LUNG SAFE study. Intensive Care Med 2016; 42:1865–1876 [DOI] [PubMed] [Google Scholar]
- 57.Talmor D, Sarge T, Malhotra A, et al. Mechanical ventilation guided by esophageal pressure in acute lung injury. N Engl J Med 2008; 359:2095–2104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Grasso S, Terragni P, Birocco A, et al. ECMO criteria for influenza A (H1N1)-associated ARDS: Role of transpulmonary pressure. Intensive Care Med 2012; 38:395–403 [DOI] [PubMed] [Google Scholar]
- 59.Costa EL, Borges JB, Melo A, et al. Bedside estimation of recruitable alveolar collapse and hyperdistension by electrical impedance tomography. Intensive Care Med 2009; 35:1132–1137 [DOI] [PubMed] [Google Scholar]
- 60.Zhao Z, Möller K, Steinmann D, et al. Evaluation of an electrical impedance tomography-based Global Inhomogeneity Index for pulmonary ventilation distribution. Intensive Care Med 2009; 35:1900–1906 [DOI] [PubMed] [Google Scholar]
- 61.Eronia N, Mauri T, Maffezzini E, et al. Bedside selection of positive end-expiratory pressure by electrical impedance tomography in hypoxemic patients: A feasibility study. Ann Intensive Care 2017; 7:76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pelosi P, Goldner M, McKibben A, et al. Recruitment and derecruitment during acute respiratory failure: An experimental study. Am J Respir Crit Care Med 2001; 164:122–130 [DOI] [PubMed] [Google Scholar]
- 63.Writing Committee and Steering Committee for the RELAx Collaborative Group. Algera AG, Pisani L, Neto AS, et al. Effect of a lower vs. higher positive end-expiratory pressure strategy on ventilator-free days in ICU patients without ARDS: A randomized clinical trial. JAMA 2020; 324:2509–2520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mauri T, Foti G, Fornari C, et al. ; PROTECTION Trial Collaborators. Sigh in patients with acute hypoxemic respiratory failure and acute respiratory distress syndrome: The PROTECTION pilot randomized clinical trial. Chest 2021; 159:1426–1436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Vignon P, Evrard B, Asfar P, et al. Fluid administration and monitoring in ARDS: Which management? Intensive Care Med 2020; 46:2252–2264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rhodes A, Evans LE, Alhazzani W, et al. Surviving sepsis campaign: International guidelines for management of sepsis and septic shock: 2016. Intensive Care Med 2017; 43:304–377 [DOI] [PubMed] [Google Scholar]
- 67.Kiiski R, Takala J, Kari A, et al. Effect of tidal volume on gas exchange and oxygen transport in the adult respiratory distress syndrome. Am Rev Respir Dis 1992; 146:1131–1135 [DOI] [PubMed] [Google Scholar]
- 68.Kiiski R, Kaitainen S, Karppi R, et al. Physiological effects of reduced tidal volume at constant minute ventilation and inspiratory flow rate in acute respiratory distress syndrome. Intensive Care Med 1996; 22:192–198 [DOI] [PubMed] [Google Scholar]
- 69.Chander A, Fisher AB. Regulation of lung surfactant secretion. Am J Physiol 1990; 258:L241–L253 [DOI] [PubMed] [Google Scholar]
- 70.Nin N, Muriel A, Peñuelas O, et al. ; VENTILA Group. Severe hypercapnia and outcome of mechanically ventilated patients with moderate or severe acute respiratory distress syndrome. Intensive Care Med 2017; 43:200–208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Brochard L, Roudot-Thoraval F, Roupie E, et al. Tidal volume reduction for prevention of ventilator-induced lung injury in acute respiratory distress syndrome. The multicenter trail group on tidal volume reduction in ARDS. Am J Respir Crit Care Med 1998; 158:1831–1838 [DOI] [PubMed] [Google Scholar]
- 72.Brower RG, Shanholtz CB, Fessler HE, et al. Prospective, randomized, controlled clinical trial comparing traditional versus reduced tidal volume ventilation in acute respiratory distress syndrome patients. Crit Care Med 1999; 27:1492–1498 [DOI] [PubMed] [Google Scholar]
- 73.Crapo RO, Morris AH, Gardner RM. Reference spirometric values using techniques and equipment that meet ATS recommendations. Am Rev Respir Dis 1981; 123:659–664 [DOI] [PubMed] [Google Scholar]
- 74.Ibañez J, Raurich JM. Normal values of functional residual capacity in the sitting and supine positions. Intensive Care Med 1982; 8:173–177 [DOI] [PubMed] [Google Scholar]
- 75.Deans KJ, Minneci PC, Cui X, et al. Mechanical ventilation in ARDS: One size does not fit all. Crit Care Med 2005; 33:1141–1143 [DOI] [PubMed] [Google Scholar]
- 76.Goligher EC, Costa ELV, Yarnell CJ, et al. Effect of lowering tidal volume on mortality in ARDS varies with respiratory system elastance. Am J Respir Crit Care Med 2021; 203:1378–1385 [DOI] [PubMed] [Google Scholar]
- 77.Baedorf Kassis E, Loring SH, Talmor D. Mortality and pulmonary mechanics in relation to respiratory system and transpulmonary driving pressures in ARDS. Intensive Care Med 2016; 42:1206–1213 [DOI] [PubMed] [Google Scholar]
- 78.Ranieri VM, Zhang H, Mascia L, et al. Pressure-time curve predicts minimally injurious ventilatory strategy in an isolated rat lung model. Anesthesiology 2000; 93:1320–1328 [DOI] [PubMed] [Google Scholar]
- 79.Grasso S, Terragni P, Mascia L, et al. Airway pressure-time curve profile (stress index) detects tidal recruitment/hyperinflation in experimental acute lung injury. Crit Care Med 2004; 32:1018–1027 [DOI] [PubMed] [Google Scholar]
- 80.Grasso S, Stripoli T, De Michele M, et al. ARDSnet ventilatory protocol and alveolar hyperinflation: Role of positive end-expiratory pressure. Am J Respir Crit Care Med 2007; 176:761–767 [DOI] [PubMed] [Google Scholar]
- 81.Chen L, Brochard L. Lung volume assessment in acute respiratory distress syndrome. Curr Opin Crit Care 2015; 21:259–264 [DOI] [PubMed] [Google Scholar]
- 82.Richard JC, Marque S, Gros A, et al. ; REVA research network. Feasibility and safety of ultra-low tidal volume ventilation without extracorporeal circulation in moderately severe and severe ARDS patients. Intensive Care Med 2019; 45:1590–1598 [DOI] [PubMed] [Google Scholar]
- 83.Gattinoni L, Pesenti A, Mascheroni D, et al. Low-frequency positive-pressure ventilation with extracorporeal CO2 removal in severe acute respiratory failure. JAMA 1986; 256:881–886 [PubMed] [Google Scholar]
- 84.Terragni PP, Del Sorbo L, Mascia L, et al. Tidal volume lower than 6 ml/kg enhances lung protection: Role of extracorporeal carbon dioxide removal. Anesthesiology 2009; 111:826–835 [DOI] [PubMed] [Google Scholar]
- 85.Combes A, Fanelli V, Pham T, et al. ; European Society of Intensive Care Medicine Trials Group and the “Strategy of Ultra-Protective lung ventilation with Extracorporeal CO2 Removal for New-Onset moderate to severe ARDS” (SUPERNOVA) investigators. Feasibility and safety of extracorporeal CO2 removal to enhance protective ventilation in acute respiratory distress syndrome: The SUPERNOVA study. Intensive Care Med 2019; 45:592–600 [DOI] [PubMed] [Google Scholar]
- 86.Bein T, Weber-Carstens S, Goldmann A, et al. Lower tidal volume strategy (≈3 ml/kg) combined with extra-corporeal CO2 removal versus “conventional” protective ventilation (6 ml/kg) in severe ARDS: The prospective randomized Xtravent-study. Intensive Care Med 2013; 39:84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Spinelli E, Colussi G, Dal Santo G, et al. Atelectasis, shunt, and worsening oxygenation following reduction of respiratory rate in healthy pigs undergoing ECMO: An experimental lung imaging study. Front Physiol 2021; 12:663313. [DOI] [PMC free article] [PubMed] [Google Scholar]