Abstract
Societal lockdowns during the first wave of the coronavirus disease 2019 pandemic were associated with decreased admission rates for acute cardiovascular conditions worldwide. In this nationwide Danish study of the first five weeks of a second pandemic lockdown, incidence of new-onset heart failure and atrial fibrillation remained stable, but there was a significant drop in new-onset ischemic heart disease and ischemic stroke during the fourth week of lockdown, which normalized promptly. The observed drops were lower compared to the first Danish lockdown in March 2020; thus, our data suggest that declines in acute cardiovascular disease admission rates during future lockdowns are avoidable.
The first wave of the coronavirus disease 2019 (COVID-19) pandemic led to societal lockdowns and related declines in cardiovascular disease (CVD) admission rates worldwide.1., 2, 3. Evidence suggests that such declines were linked to increased out of hospital cardiovascular mortality rates, possibly due to delays in seeking treatment,4 , 5 and information campaigns were instigated to urge patients to seek timely care. Normalization of CVD admission rates following relaxation of lockdown measures were observed.2 In response to rapidly growing COVID-19 case numbers, a second nationwide lockdown was issued by the Danish government from December 17, 2020, requiring closure of schools, stores, restaurants, cultural offerings, etc., and banning public gatherings above five people. It remains unclear whether the second wave of the COVID-19 pandemic and subsequent societal lockdowns led to declines in acute CVD admissions.
Methods
To address this, we studied admission rates for new-onset (ie, first-time diagnosis) of heart failure (HF), ischemic heart disease (IHD), ischemic stroke (IS), and atrial fibrillation (AF) using Danish registries with nationwide coverage. The Danish registries have been described in detail previously.6 Methods were similar to those utilized in studies of admission rates during the first lockdown.2 , 3 Briefly, we identified all first-time admissions for HF (International Classification of Diseases, 10th revision codes [ICD-10]: I50, I110, I130, I132), IHD (ICD-10: I20-I25), IS (ICD-10: I63-64), and AF (ICD-10: I48) from February 16, 2019 through January 21, 2021. The period of interest was the first five weeks of the second Danish lockdown from December 17, 2020 through January 21, 2021 (lockdown continued beyond end of data). Using Poisson regression, we calculated weekly incidence rates (IR) and incidence rate ratios (IRR) with 95% confidence intervals (CI) per 100,000 person-years (PY), comparing them to the corresponding calendar weeks in the previous year. In a post-hoc analysis, we calculated IRRs for the total period of each of the two lockdowns compared to the previous year. Capital Region of Denmark approved the study (approval number P-2019-191). No external funding was used to support this work.
Results
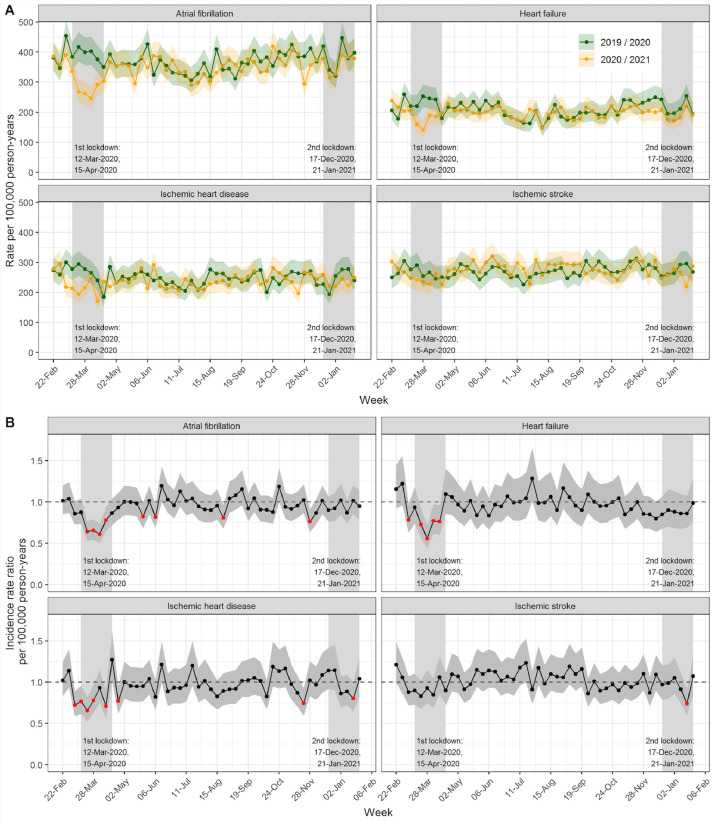
During the second Danish nationwide lockdown there were 635 vs 748 new-onset HF admissions, 780 vs 885 new-onset IHD admissions, 879 vs 984 new-onset IS admissions, and 1208 vs 1345 new-onset AF admissions compared to the corresponding period of the previous year. The weekly incidence rates during the second lockdown (Figure 1 A) were similar to the previous year for HF and AF. They were, however, lower during the fourth week of lockdown for IHD (IR per 100,000 PY: 223 [CI: 190-260] vs 278 [CI: 240-319]) and IS (IR per 100,000 PY: 219 [CI: 186-256] vs 296 [CI: 257-339]), but only the difference for IS was significant.
Figure 1.
Rates and incidence rate ratios per 100,000 person-years with 95% confidence intervals of new-onset atrial fibrillation, heart failure, ischemic heart disease, and ischemic stroke. A, Weekly rates per 100,000 person-y in 2020/2021 compared to the corresponding wk in 2019/2020. B, Weekly incidence rate ratios in 2020/2021 compared to the corresponding wk in 2019/2020.
The weekly IRRs during the second lockdown (Figure 1B) were not significantly lower compared to the previous year for HF and AF. However, there was a significant drop in admissions during the fourth week of lockdown for IHD (IRR 0.80 [CI: 0.65-0.99]) and IS (IRR 0.74 [CI: 0.60-0.91]), which normalized the following week.
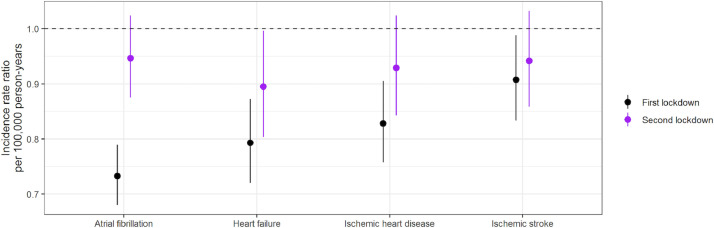
In the post-hoc analysis (Figure 2 ), the IRR for the total second lockdown period vs the corresponding period in the previous year was lower for IHD (IRR: 0.93 [CI: 0.84-1.02]), IS (IRR: 0.94 [CI: 0.86-1.03]), and AF (IRR: 0.95 [CI: 0.88-1.02]), but only significantly so for HF (IRR: 0.89 [CI: 0.80-0.99]). However, the IRRs were higher for all four conditions than throughout the first lockdown, where statistically significant drops were observed.
Figure 2.
Incidence rate ratios for the total period of the first and the second lockdown compared to the corresponding periods of the previous year.
Discussion
Overall, the observed drops in CVD admission rates appeared to be of substantially smaller magnitude compared to the first Danish lockdown. This was unexpected, as the second lockdown was of similar stringency to the first one. Our findings are in contrast to a study from the United Kingdom (UK) that reported second declines in myocardial infarction and HF admission rates of equal magnitude to the first ones in the spring of 2020.7
However, the COVID-19 pandemic in 2020 was more severe in the UK compared to Denmark, and the standard of care in the Danish healthcare system is high, which may limit generalizability to other settings. Moreover, Danish COVID-19 patients with CVD, compared to other chronic diseases, did not appear to be at increased risk of worse clinical outcomes during the first wave of the pandemic.8 , 9 These circumstances may have contributed to differences in health-seeking behavior in Denmark and the UK, which may partly explain the conflicting results. However, recent data from the United States showed no drops in acute myocardial infarction and ischemic stroke admission rates during second and third COVID-19 case count surges.10 This, in conjunction with our findings, suggests that declines in CVD admission rates may be preventable during COVID-19 case surges and subsequent societal lockdowns, and that avoidance of seeking healthcare may not be driven directly by lockdowns per se, but other factors such as fear of the virus, not wanting to further burden the healthcare system, media coverage, or lack of trust in authorities.
In conclusion, the present data suggest that declines in acute CVD admission rates during societal pandemic lockdowns are avoidable. This may inform public health efforts to ameliorate the collateral damage of future waves of the COVID-19 pandemic and related societal lockdown measures.
Disclosures
Dr. Køber reported speaker's honoraria from Novo, Novartis, AstraZeneca and Boehringer, unrelated to the present study. All other authors had nothing to disclose. The authors are solely responsible for the conduct of this study, including all analyses, the drafting and editing of the paper and its final contents.
References
- 1.Solomon MD, McNulty EJ, Rana JS, et al. The Covid-19 pandemic and the incidence of acute myocardial infarction. New Engl J Med. 2020;383(7):691–693. doi: 10.1056/NEJMc2015630. [DOI] [PubMed] [Google Scholar]
- 2.Butt JH, Ostergaard L, Gerds TA, et al. The Association between cardiovascular disease admission rates and the coronavirus disease 2019 lockdown and reopening of a nation: a danish nationwide cohort study. Eur Heart J Qual Care Clin Outcomes. 2021 doi: 10.1093/ehjqcco/qcab021. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ostergaard L, Butt JH, Kragholm K, et al. Incidence of acute coronary syndrome during national lock-down: insights from nationwide data during the coronavirus disease 2019 (COVID-19) pandemic. Am Heart J. 2021;232:146–153. doi: 10.1016/j.ahj.2020.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Butt JH, Fosbol EL, Gerds TA, et al. All-cause mortality and location of death in patients with established cardiovascular disease before, during, and after the COVID-19 lockdown: a Danish Nationwide Cohort Study. Eur Heart J. 2021;42:1516–1523. doi: 10.1093/eurheartj/ehab028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Banerjee A, Chen S, Pasea L, et al. Excess deaths in people with cardiovascular diseases during the COVID-19 pandemic. Eur J Prev Cardiol. 2021 doi: 10.1093/eurjpc/zwaa155. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Christensen DM, Rajan S, Kragholm K, et al. Bystander cardiopulmonary resuscitation and survival in patients with out-of-hospital cardiac arrest of non-cardiac origin. Resuscitation. 2019;140:98–105. doi: 10.1016/j.resuscitation.2019.05.014. [DOI] [PubMed] [Google Scholar]
- 7.Wu J, Mamas MA, de Belder MA, et al. Second decline in admissions with heart failure and myocardial infarction during the COVID-19 pandemic. J Am Coll Cardiol. 2021;77:1141–1143. doi: 10.1016/j.jacc.2020.12.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Phelps M, Christensen DM, Gerds T, et al. Cardiovascular comorbidities as predictors for severe COVID-19 infection or death. Eur Heart J Qual Care Clin Outcomes. 2021;7:172–180. doi: 10.1093/ehjqcco/qcaa081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Christensen DM, Strange JE, Gislason G, et al. Charlson comorbidity index score and risk of severe outcome and death in danish COVID-19 patients. J Gen Intern Med. 2020;35:2801–2803. doi: 10.1007/s11606-020-05991-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Solomon MD, Nguyen-Huynh M, Leong TK, et al. Changes in patterns of hospital visits for acute myocardial infarction or ischemic stroke during COVID-19 surges. JAMA. 2021;326(1):82–84. doi: 10.1001/jama.2021.8414. [DOI] [PMC free article] [PubMed] [Google Scholar]