Abstract
We observed a higher rate of blood-culture contamination during the COVID-19 pandemic at our institution compared to a prepandemic period. Given the potential implications of blood contamination in antibiotic and diagnostic test utilization as well as added cost, it is imperative to continue efforts to minimize these episodes during the pandemic.
During the initial wave of coronavirus disease 2019 (COVID-19), the delivery of healthcare services had to be rapidly adjusted to mitigate the effects of the surge in demand. This readjustment included reassignment of healthcare personnel to different services and modification of hospital infection control practices. Despite extensive efforts to maintain high-quality care, unintended lapses in healthcare delivery such as the overuse of microbiologic diagnostic tests and broad-spectrum antimicrobials have been reported.1
An earlier study conducted in patients with COVID-19 showed a significant increase in blood-culture testing despite low rates of concomitant bacteremia in these patients, overwhelming the laboratory system capacity and resources.2 Furthermore, an inadvertent upsurge in blood-culture testing in low-prevalence populations along with inadequate specimen collection could result in high rates of blood culture contamination, leading to unnecessary antibiotic treatment, diagnostic testing utilization, and added cost.3
At our institution, blood samples for culture are usually collected by dedicated phlebotomists because this practice is associated with lower rates of contamination.4 However, after the first cases of COVID-19 were reported at our institution, to preserve personal protective equipment (PPE) and limit patient interactions with healthcare workers, the phlebotomy staff dedicated to blood culture collections were temporarily disbanded, and blood culture collection was performed by nonphlebotomist staff (nurses). In addition, a prepandemic multidisciplinary team consisting of microbiologists, infectious diseases pharmacists, and a blood-culture contamination surveillance team composed of physicians designated to routinely audit the rates of blood-culture contamination, was reassigned to clinical services to meet the demands of the COVID-19 crisis. In this study, we compared blood-culture contamination rates prior to and during the COVID-19 pandemic to evaluate the impact of the aforementioned changes.
Methods
We retrospectively reviewed all blood culture results from adult patients aged ≥18 years at the University of Mississippi Medical Center, a tertiary-care center with >722 beds in Jackson, Mississippi, between September 1, 2019, and August 30, 2020, to identify cases of blood culture contamination. We divided the study period into pre–COVID-19 pandemic (between September 1, 2019, and February 29, 2020) and the COVID-19 pandemic period (between March 1, 2020, and August 30, 2020), based on the identification of initial cases of COVID-19 infection and after the reassignment of the phlebotomists and the blood-culture contamination surveillance team in the second week of March. Blood-culture contamination was defined in accordance with the criteria proposed by Bekeris et al.5
Our primary outcome of interest was the rate of blood-culture contamination before and after the onset of the COVID-19 pandemic. We used the χ2 test to compare categorical variables and the Wilcoxon rank-sum test to analyze continuous variables between study periods.
Results
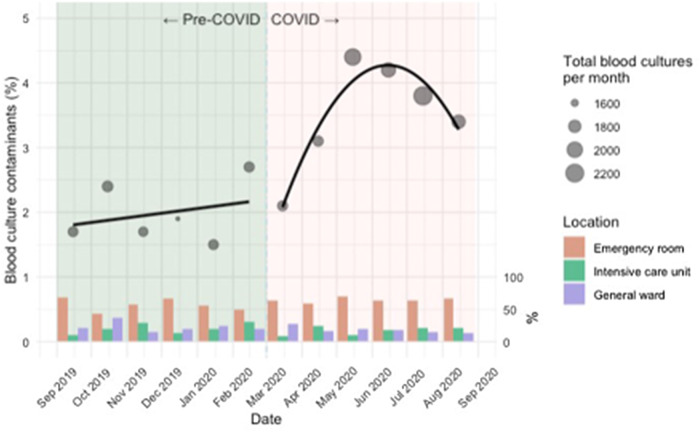
In total, 21,451 blood cultures were obtained during the study period, of which 10,001 were collected before the COVID-19 pandemic and 11,450 after the onset of the COVID-19 pandemic. Overall, 605 of 21,451 (2.8%) of all blood culture tests were deemed contaminated according to our study criteria; however, blood-culture contamination rates were significantly higher during the COVID-19 pandemic: 197 of 10,001 (1.9%) versus 408 of 11,450 (3.5%) (P = .01) (Fig. 1).
Fig. 1.
Blood cultures collected and contaminant rates before and during the COVID-19 pandemic.
Coagulase-negative staphylococci (CoNS) accounted for most blood-culture contamination cases during the entire study period (447 of 605, 73.8%). Other commonly reported contaminants included diphtheroids (41 of 605, 6.7%), Bacillus spp not anthracis (36 of 605, 5.9%), and Micrococcus luteus (29 of 605, 4.7%). The remaining cases (51 of 605, 8.4%) were caused by other gram-positive bacteria (Supplementary Table 1 online).
Regardless of the period analyzed, most cases of blood culture contamination were reported in the emergency department (109 of 197, 55.3% vs 264 of 408, 64.7% before and during COVID-19, respectively) (Fig. 1).
Most blood samples that grew contaminants during both periods were collected by nonphlebotomist healthcare workers: 176 of 197 (89.3%) before the pandemic and 338 of 408 (82.8%) during the pandemic, respectively. The percentage of contaminated samples collected by phlebotomist during the COVID-19 pandemic also increased compared to the prepandemic period: 21 of 197 (10.7%) versus 70 of 408 (17.2%) (P < .001). These results suggest that additional factors may have contributed to the increased rates of contamination.
Discussion
Despite similar numbers of blood-culture collections before and during the COVID-19 pandemic, contamination rates were significantly higher during the COVID-19 pandemic. Higher rates of blood culture contamination observed during this period may have been related to the temporary suspension of a dedicated phlebotomist team. Most contaminated blood cultures were collected by nonphlebotomists during both periods; however, the percentage of contaminated blood cultures collected by phlebotomists increased during the COVID-19 pandemic, suggesting that other factors may have contributed to the increase blood-culture contamination rates. We hypothesize that adherence to optimal phlebotomy technique was lower during the pandemic due to increase in workload and staffing shortages, which placed additional the stress on frontline staff, as well as the frequent need for use of COVID-19 PPE by collectors and reduced contact time with patients due to exposure risk.
Additionally, before the widespread use of video conferencing education, training on appropriate blood-culture collection technique for operating staff was significantly reduced during the COVID-19 pandemic for safety reasons. Moreover, as previously discussed, monthly surveillance of blood-culture contamination was interrupted during the COVID-19 pandemic, which may have prevented timely assessment of increase rate in blood-culture contamination at our institution. Indeed, the Centers for Medicare and Medicaid Services waived reporting requirements through June 2020 to allow flexibility to healthcare providers responding to the present crisis.6
Notably, regardless of the study period, most of the blood-culture contamination occurred in the emergency department, indicating that this area requires special attention. This trend has been previously studied and attributed to the workload, rapid staff turnover, and suboptimal training in this area, all factors that were likely exacerbated by the pandemic.7,8
A retrospective study from a hospital network in Sweden described a low prevalence of bloodstream infection in patients with COVID-19 and a higher rate of blood culture contamination compared to a historical control group.9
Another retrospective study conducted early during the pandemic in a large hospital network in New York City reported an increase in blood culture collection by 35%, with a rate of bacteremia of 1.6%2 and blood culture contamination rate of 2.2% in COVID-19 patients. The rate of bacteremia was lower in COVID-19 patients than in COVID-19-negative patients.
Other institutions in the United States may encounter the same phenomenon. Efforts to re-establish evidence-based strategies to minimize blood-culture contamination, including collection by dedicated phlebotomist teams, close surveillance of blood-culture contamination rates, education and training on adequate aseptic technique, should be sought based on available resources.10
Our study has several limitations. The retrospective nature of the study prevented us from accurately reviewing the blood volume submitted for each blood-culture bottle and confirming that it was appropriate. We were also unable to adjust for patient risk factors such as medical comorbidities, triage level and isolation precautions at the time of blood culture collection, as well as hand hygiene practices at the time of collection.
In conclusion, despite similar numbers of blood-culture samples collected before the emergence of and during the COVID-19 pandemic, contamination rates were significantly higher during the COVID-19 pandemic. Given the potential implications of blood-culture contamination in antibiotic and diagnostic test utilization and subsequent added cost, efforts to re-establish evidence-based strategies to minimize blood-culture contamination should be sought based on available resources.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/ice.2021.292.
click here to view supplementary material
References
- 1. Mazdeyasna H, Nori P, Patel P, et al. Antimicrobial stewardship at the core of COVID-19 response efforts: implications for sustaining and building programs. Curr Infect Dis Rep 2020;22. [DOI] [PMC free article] [PubMed]
- 2. Sepulveda J, Westblade LF, Whittier S, et al. Bacteremia and blood culture utilization during COVID-19 surge in New York City. J Clin Microbiol 2020;58(8):e00875–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Dargere S, Cormier H, Verdon R. Contaminants in blood cultures: importance, implications, interpretation and prevention. Clin Microbiol Infect 2018;24:964–969. [DOI] [PubMed] [Google Scholar]
- 4. Norberg A, Christopher NC, Ramundo ML, Bower JR, Berman SA. Contamination rates of blood cultures obtained by dedicated phlebotomy vs intravenous catheter. JAMA 2003;289:726–729. [DOI] [PubMed] [Google Scholar]
- 5. Bekeris LG, Tworek JA, Walsh MK, Valenstein PN. Trends in blood culture contamination: a College of American Pathologists Q-Tracks study of 356 institutions. Arch Pathol Lab Med 2005;129:1222–1225. [DOI] [PubMed] [Google Scholar]
- 6. McMullen KM, Smith BA, Rebmann T. Impact of SARS-CoV-2 on hospital-acquired infection rates in the United States: predictions and early results. Am J Infect Control 2020;48:1409–1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Halverson S, Malani PN, Newton DW, Habicht A, Vander Have K, Younger JG. Impact of hourly emergency department patient volume on blood culture contamination and diagnostic yield. J Clin Microbiol 2013;51:1721–1726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lee CC, Lee NY, Chuang MC, Chen PL, Chang CM, Ko WC. The impact of overcrowding on the bacterial contamination of blood cultures in the ED. Am J Emerg Med 2012;30:839–845. [DOI] [PubMed] [Google Scholar]
- 9. Yu D, Ininbergs K, Hedman K, Giske CG, Stralin K, Ozenci V. Low prevalence of bloodstream infection and high blood-culture contamination rates in patients with COVID-19. PLoS One 2020;15:e0242533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wang P, Hu B. Strategies on reducing blood culture contamination. Rev Med Microbiol 2012;23:63–66. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/ice.2021.292.
click here to view supplementary material