Abstract
Background
To examine association between gestational weight gain (GWG) in women with gestational diabetes mellitus (GDM) and adverse pregnancy outcomes (APOs).
Methods
This retrospective cohort study enrolled women with GDM who delivered at 2010–2020 in Changzhou, Jiangsu. Total GWG, rates of GWG in second trimester and third trimesters were stratified into three categories according to IOM guidelines: within, below, and above IOM guidelines. Univariable and multivariable logistic regression analyses were used.
Results
Overall, 1606 women with GDM fulfilled inclusion criteria. Compared with within IOM guidelines and after adjusting for confounders, total GWG above IOM guidelines in pregnancy was associated with an increased odds of caesarean delivery [adjusted odds ratio (aOR) = 1.34, 95% confidence interval (CI): 1.04–1.72], hypertensive disorders of pregnancy (HDP) (aOR = 2.00, 1.28–3.12), preeclampsia (aOR = 2.06, 1.01–3.12), macrosomia (aOR = 1.55, 1.13–2.13) and large for gestational age (LGA) (aOR = 2.82, 1.94–3.23), and a decreased odds of premature rupture of membrane (PROM) (aOR = 0.46, 0.36–0.60) and preterm birth (aOR = 0.35, 0.26–0.44); total GWG below IOM guidelines in pregnancy was associated with an increased risk of preterm birth (aOR = 1.96, 1.44–2.66), small for gestational age (SGA) (aOR = 1.32, 1.11–1.50) and a decreased odds of macrosomia (aOR = 0.35, 0.23–0.53) and LGA (aOR = 0.54, 0.42–0.72). Further, in both second and third trimesters of pregnancy, rates of GWG above IOM guidelines was found to be associated with a high odds of HDP (aOR = 2.55, 1.86–3.38; aOR = 1.93, 1.08–2.98), preeclampsia (aOR = 2.28, 1.21–3.81; aOR = 2.17, 1.35–4.37), macrosomia (aOR = 1.20, 1.02–1.82; aOR = 2.02, 1.51–2.64) and LGA (aOR = 1.42, 1.24–1.97; aOR = 1.79, 1.51–2.54). Rates of GWG above IOM guidelines in third trimester of pregnancy also increased odds of caesarean delivery (aOR = 1.48, 1.16–2.34) when compared with within IOM guidelines. While rates of GWG below IOM guidelines in both second and third trimesters of pregnancy was associated with a decreased odds of macrosomia (aOR = 0.66, 95% CI: 0.52–0.78; aOR = 0.52, 0.39–0.63) and LGA(aOR = 0.71, 0.51–0.82; aOR = 0.67, 0.55–0.79). In addition, rate of GWG below IOM guidelines in third trimester of pregnancy was associated with an increased odds of preterm birth (aOR = 1.52, 1.12–2.05) and SGA (aOR = 1.21, 1.10–1.69).
Conclusion
GWG, outside IOM guidelines has increased risks of APOs among women with GDM, implying that careful surveillance for GWG during different stages of pregnancy is warranted.
Keywords: Gestational weight gain, Gestational diabetes mellitus, Institute of Medicine guidelines, Adverse pregnancy outcomes
Background
Gestational diabetes mellitus (GDM) is defined as hyperglycaemia first detected during pregnancy and not reaching non-pregnant diabetes levels; it is one of the major risk factors of adverse pregnancy outcomes (APOs) [1, 2]. Previous studies have shown that the diagnosis of GDM was highly associated with a risk of hypoglycemia, hyperbilirubinemia, preeclampsia, and cesarean section. It was also associated with a risk of fetal macrosomia, preterm birth, and large for gestational age (LGA) infants, in addition, women with GDM were shown to be at a risk of long-term obesity and diabetes [3, 4]. In China, the prevalence of GDM is approximately 10% of pregnancies [5]. However, recent studies have shown that the prevalence of GDM has increased with both obesity and gestational weight gain (GWG) among pregnant women on other areas of the world and has been correlated with APOs [6, 7].
GWG, an important antenatal factor, is reportedly associated with APOs [8–10]. According to the 2009 Institute of Medicine (IOM) guidelines, excessive GWG increases the risk of cesarean delivery, hypertensive disorders of pregnancy (HDP), GDM, and LGA infants. On the other hand, insufficient GWG increases the risk of small for gestational age (SGA) infants and preterm births [11–14]. However, studies on the association of GWG with APOs in women with GDM are conflicting [15–18]. Yasuda et al. indicated that excessive GWG in women with GDM was significantly related to increased infant birthweight [19]. Insufficient GWG reportedly increased the incidence of preterm birth in women with GDM [20]. Moreover, some studies showed that insufficient GWG in women with GDM is associated with more favorable obstetric and neonatal outcomes than adequate or excessive GWG [16, 21]. However, whether inadequate GWG is associated with adverse outcomes in GDM has not been fully elucidated. Additionally, there is limited research on the association of APOs with GDM among the adequate range of GWG at different stages (total GWG and rates of GWG in the second trimester and third trimesters).
Therefore, we conducted a retrospective cohort study of women with GDM in China which included a wide range of perinatal outcomes to investigate the associations among GWG within, below, or above the IOM guidelines with adverse perinatal outcomes. We also assessed whether inadequate GWG is associated with adverse outcomes in GDM in the second and third trimesters of pregnancy.
Methods
Study design and population
The study was conducted at a hospital in Changzhou, Jiangsu, China. We analyzed the data recorded for pregnant women diagnosed with GDM who delivered between January 2010 and December 2020, all data were extracted from the institutional medical record database. All pregnant women self-reported their pre-gestational body mass index (ppBMI) and measured their height and weight at the first trimester visit to the hospital. Their weight was then recorded in the electronic medical records during every subsequent antenatal clinical visit to the hospital. According to the following World Health Organization (WHO) classifications for body mass index (BMI), women were classified into four categories by their ppBMI (see Table 1). All pregnant women had their last weight measured at delivery within 24 h of entry into the labor room. Total GWG was calculated by deducting pre-gestational weight from maternal weight at delivery; The rates of GWG were calculated by dividing the GWG in the second ( 16 weeks) or third trimester (final number of weeks) by the corresponding number of weeks. The GWG of different stages (total GWG and rates of GWG in the second trimester and third trimesters) was stratified into three categories according to IOM guidelines: within, below, and above the IOM guidelines (see Table 1) [22].
Table 1.
IOM guidelines for total GWG and rates of GWG during Pregnancy, by ppBMI
| Total GWG (kg) | Rates of GWG in second and third Trimester (kg/week) | |
|---|---|---|
| Underweight (< 18.5 kg/m2) | 12.5–18 | 0.44–0.58 |
| Normal weight (18.5–24.9 kg/m2) | 11.5–16 | 0.35–0.50 |
| Overweight (25.0–29.9 kg/m2) | 7–11.5 | 0.23–0.33 |
| Obese (≥ 30.0 kg/m2) | 5–9 | 0.17–0.27 |
IOM Institute of Medicine, GWG gestational weight gain, ppBMI pre-pregnancy Body Mass Index
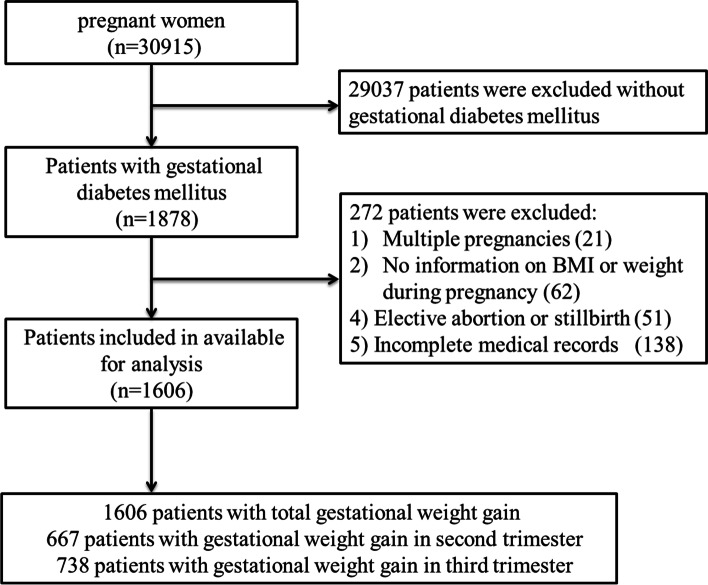
The inclusion criteria comprised of (a) aged 18 years or older without pre-GDM, pre-gestational hypertension, heart disease, hepatic disease, or renal disease; (b) diagnosed with GDM with singleton pregnancy and live birth; and (c) complete medical records of APOs. The exclusion criteria were as follows: (a) multiple pregnancies; (b) no information on ppBMI or weight during pregnancy; and (c) elective abortion or stillbirth before 22 weeks of pregnancy. A total of 30,915 pregnant women delivered at our hospital; 1878 pregnant women with GDM were included after applying the inclusion criteria. However, 272 of them were removed from the study after applying the exclusion criteria (Fig. 1). Finally, 1606 pregnant women with GDM were included for analysis. Data of general information (included maternal age, pre-pregnancy BMI, maternal education, caesarean history, parity, IVF, mode of delivery, gestational age), gestational weight, blood glucose, and APOs were obtained from the institutional medical record system. The APOs consisted of adverse maternal pregnancy outcomes and adverse neonatal outcomes. We examined the following adverse maternal pregnancy outcomes: cesarean delivery, HDP, preeclampsia, premature rupture of membranes (PROM), postpartum hemorrhage, and fetal distress. Adverse neonatal outcomes examined were preterm birth (before 37 weeks of pregnancy), macrosomia with birth weight ≥ 4000 g, SGA (birth weight below the10th percentile per gestational age and gender), and LGA (birth weight above the 90th percentile per gestational age and gender).
Fig. 1.
Flow diagram of Study cohort
Diagnosis of GDM
GDM was diagnosed when any blood glucose value was greater than fasting blood glucose at 5.1 mmol/L or blood glucose after 1 h at 10.0 mmol/L or after 2 h at 8.5 mmol/L based on a 75-g oral glucose tolerance test (75 g OGTT). This was based on the criteria of the International Association of Diabetes and Pregnancy Study Groups (IADPSG) [23].
Statistical analysis
Statistical analysis of all data was completed using SPSS version 23.0 (SPSS, Chicago, IL, USA). Mean ± standard deviation (SD) was used to describe continuous variables, and categorical data were expressed as proportions (n [%]). The ANOVA test were used to analyze the differences in continuous variables, and Pearson’s χ2 test or Fischer exact test were used to analyze categorical data. Adjusted odds ratios (aORs) with 95% confidence intervals (CIs) were calculated to express the odds ratios of the GWG above or below the IOM guidelines on APOs by multivariable logistic regression after adjusting for potential confounding variables. A p value < 0.05 (two sided) indicated statistical significance.
Results
Demographic characteristics of the cohort
Overall, 1606 women were enrolled according to the inclusion criteria (Fig. 1). The GWG of 560 women (34.9%) was within the IOM guidelines, 545 (33.9%) had GWG below IOM guidelines, and 501 (31.2%) had GWG above the IOM guidelines. The demographic and clinical data of these three groups are summarized in Table 2. The pregnant women in the GWG below IOM guidelines group were significantly older than those in the GWG within and above IOM guidelines group (mean age ± SD: 33.21 ± 4.36 vs 32.75 ± 4.83 vs 31.86 ± 4.58 years, P < 0.01). The ppBMI in the above IOM guidelines group (23.68 ± 3.41 kg/m2) was significantly higher than that in the within (22.72 ± 3.11 kg/m2) and below (22.48 ± 2.62 kg/m2) IOM guidelines groups. The proportion of overweight and obese women (25.2%) was highest in the above IOM guidelines group, and women in the below IOM guidelines group had the highest proportion (81.7%) of normal ppBMI. In addition, there were significant differences in the mode of delivery, maternal education, fasting plasma glucose (FBG), and 2 h GLU among the three groups. However, there were no significant differences in cesarean history, parity, or in-vitro fertilization in these three groups (P > 0.05) (see Table 2).
Table 2.
Characteristics of women with gestational diabetes mellitus stratified by GWG according to IOM guidelines
| Characteristic | Within (n = 560) (34.9%) |
Below (n = 545) (33.9%) |
Above (n = 501) (31.2%) |
P value |
|---|---|---|---|---|
| Maternal age | 32.75 ± 4.83 | 33.21 ± 4.36 | 31.86 ± 4.58 | < 0.001 |
| Pre-pregnancy BMI (kg/m2) | 22.72 ± 3.11 | 22.48 ± 2.62 | 23.68 ± 3.41 | < 0.001 |
| BMI category [n (%)] | < 0.001 | |||
| Underweight (< 18.5) | 68(12.1) | 60(11.0) | 37(7.4) | |
| Normal weight (18.5–24.9) | 414(73.9) | 445(81.7) | 338(67.5) | |
| Overweight (25–29.9) | 71(12.7) | 37(6.8) | 108(21.6) | |
| Obese (≥ 30) | 7(1.3) | 3(0.6) | 18(3.6) | |
| Maternal education [n (%)]a | 0.002 | |||
| Low | 2(0.4) | 2(0.4) | 6(1.2) | |
| Medium | 100(17.9) | 76(13.9) | 112(22.4) | |
| High | 458(81.8) | 467(85.7) | 383(76.4) | |
| Caesarean history [n (%)] | 105(18.8) | 90(16.5) | 96(19.2) | 0.481 |
| Parity [n (%)] | 0.869 | |||
| Primiparous | 330(58.9) | 327(60.0) | 303(60.5) | |
| Multiparous | 230(41.1) | 218(40.0) | 198(39.5) | |
| IVF [n (%)] | 51(9.1) | 55(10.1) | 54(10.8) | 0.657 |
| Mode of delivery [n (%)] | < 0.001 | |||
| Vaginal | 325(58.0) | 346(63.5) | 254(50.7) | |
| Cesarean | 235(42.0) | 199(36.5) | 247(49.3) | |
| Gestational age (weeks, mean ± SD) | 38.16 ± 2.00 | 37.49 ± 2.46 | 38.61 ± 1.68 | < 0.001 |
| FPG on OGTT (mmol/L) | 5.03 ± 0.95 | 5.53 ± 0.78 | 5.62 ± 0.89 | < 0.001 |
| 2-h blood glucose on OGTT (mmol/L) | 8.83 ± 1.71 | 8.72 ± 1.65 | 8.49 ± 1.58 | < 0.001 |
IOM Institute of Medicine, GWG gestational weight gain, BMI Body Mass Index, IVF in-vitro fertilization, SD standard deviation, FPG fasting blood glucose, OGTT oral glucose tolerance test; a Low, primary school or less; Medium, middle and high school graduate; High, College or above
Association of total GWG with APOs among women with GDM
We analyzed the APOs according to total GWG among women with GDM. In comparison to pregnant women with GWG within the IOM guidelines, women with total GWG above the IOM guidelines had an increased odds of cesarean delivery (aOR = 1.34; 95% CI 1.04–1.72), HDP (aOR = 2.00; 95% CI 1.28–3.12), preeclampsia (aOR = 2.06; 95% CI 1.01–3.12), macrosomia (aOR = 1.55; 95% CI 1.13–2.13), and LGA (aOR = 2.82; 95% CI 1.94–3.23). Conversely, they had a decreased odds of PROM (aOR = 0.46; 95% CI 0.36–0.60) and preterm birth (aOR = 0.35; 95% CI 0.26–0.44).
Women with total GWG below the IOM guidelines had an increased odds of preterm birth (aOR = 1.96; 95% CI 1.44–2.66) and SGA (aOR = 1.32; 95% CI 1.11–1.50). However, they had a decreased odds of macrosomia (aOR = 0.35; 95% CI 0.23–0.53) and LGA (aOR = 0.54; 95% CI 0.42–0.72). There were no statistically significant differences in the odds ratios of postpartum hemorrhage, fetal distress, and placenta previa among all three groups (Table 3).
Table 3.
Association of adverse pregnancy outcome among gestational diabetes mellitus with IOM guideline on total GWG
| Within (n = 560) | Below (n = 545) | Above (n = 501) | |||||
|---|---|---|---|---|---|---|---|
| n(%) (Reference) | n (%) | crude OR (95% CI) | Adjusted OR (95% CI) | n (%) | Crude OR (95% CI) | Adjusted OR (95% CI) | |
| Caesarean delivery | 235(42.0) | 199(36.5) | 0.80(0.62–1.01) | 0.79(0.61–1.01) | 247(49.3) | 1.35(1.06–1.71)a | 1.34(1.04–1.72)b |
| HDP | 36(6.4) | 25(4.6) | 0.70(0.41–1.18) | 0.63(0.406–1.11) | 65(13.0) | 2.17(1.15–3.32)b | 2.00(1.28–3.12)b |
| preeclampsia | 15(2.7) | 11(2.0) | 0.80(0.35–1.85) | 0.83(0.35–1.97) | 33(6.6) | 2.30(1.17–4.53)b | 2.06(1.01–4.21)b |
| PROM | 263(47.0) | 278(51.0) | 1.18(0.93–1.49) | 1.17(0.92–1.48) | 147(29.3) | 0.47(0.36–0.61)a | 0.46(0.36–0.60)b |
| Postpartum hemorrhage | 50(8.9) | 58(10.6) | 1.22(0.82–1.81) | 1.24(0.83–1.85) | 43(8.6) | 0.96(0.63–1.47) | 0.90(0.58–1.40) |
| Fetal distress | 164(29.3) | 152(27.9) | 0.93(0.72–1.21) | 0.93(0.72–1.22) | 138(27.5) | 0.92(0.71–1.20) | 0.94(0.71–1.23) |
| Preterm birth | 89(15.9) | 138(25.3) | 2.39(1.63–2.42)a | 1.96(1.44–2.38)a | 34(6.8) | 0.39(0.25–0.58)a | 0.35(0.23–0.44)a |
| Macrosomia | 90(16.1) | 33(6.1) | 0.34(0.22–0.55)a | 0.35(0.23–0.53)a | 123(24.6) | 1.70(1.25–2.30)a | 1.55(1.13–2.13)b |
| SGA | 41(7.3) | 59(10.8) | 1.43(1.23–1.69)a | 1.32(1.11–1.50)b | 21(4.2) | 0.66(0.51–0.87)b | 0.89(0.69–1.09) |
| LGA | 126(22.5) | 73(13.4) | 0.47(0.35–0.68)a | 0.54(0.42–0.72)a | 183(36.5) | 3.04(2.12–4.25)a | 2.82(1.94–3.23)a |
Multivariate analyses were adjusted for maternal age, pre-pregnancy BMI, maternal education, IVF, FPG, 2-h blood glucose. The results were presented with an adjusted odds ratio, aOR (95% CI);
IOM, Institute of Medicine; GWG, gestational weight gain; HDP, hypertensive disorders of pregnancy; PROM, premature rupture of the membranes; SGA, small for gestational age; LGA, large for gestational age; OR odds ratio; CI, Confidence interval
aP < 0.01
bP < 0.05,compared with the within IOM guideline subjects
Association of rate of GWG in the second trimester of pregnancy with APOs among women with GDM
To further evaluate the effect of rate of GWG in the second trimester of pregnancy on APOs among women with GDM, 667 women were included for this analysis. Women with rate of GWG above the IOM guidelines were associated with a higher risk of HDP (aOR = 2.55; 95% CI 1.86–3.38), preeclampsia (aOR = 2.28; 95% CI 1.21–3.81), macrosomia (aOR = 1.20; 95% CI 1.02–1.82), and LGA (aOR = 1.42; 95% CI 1.24–1.97) than those with rate of GWG within IOM guidelines.
On the other hand, GDM patients with rate of GWG below the IOM guidelines were associated with a lower risk of macrosomia (aOR = 0.66; 95% CI 0.52–0.78) and LGA (aOR = 0.71; 95% CI 0.51–0.82). There were no statistically significant differences in the odds ratios of cesarean delivery, PROM, postpartum hemorrhage, fetal distress, preterm birth, and SGA among all three groups of women with GDM (Table 4).
Table 4.
Association of adverse pregnancy outcome among gestational diabetes mellitus with IOM guideline on rate of GWG in second trimester of pregnancy
| Within (n = 243) | Below (n = 225) | Above (n = 199) | |||||
|---|---|---|---|---|---|---|---|
| n(%) (Reference) | n (%) | crude OR (95% CI) | Adjusted OR (95% CI) | n (%) | crude OR (95% CI) | Adjusted OR (95% CI) | |
| Caesarean delivery | 99(40.7) | 88(39.1) | 0.85(0.72–1.21) | 0.69(0.59–1.11) | 86(43.2) | 0.95(0.72–1.43) | 0.83(0.69–1.32) |
| HDP | 13(5.3) | 10(4.4) | 0.62(0.39–1.13) | 0.60(0.36–1.16) | 31(15.6) | 3.25(1.74–3.88)a | 2.55(1.86–3.38)a |
| preeclampsia | 6(2.4) | 4(1.8) | 0.63(0.46–1.35) | 0.74(0.41–1.45) | 15(7.5) | 2.51(1.59–3.67)a | 2.28(1.21–3.81)b |
| PROM | 103(42.4) | 102(45.3) | 1.08(0.81–1.48) | 1.06(0.74–1.38) | 81(40.7) | 0.91(0.56–1.53) | 0.82(0.47–1.41) |
| Postpartum hemorrhage | 22(9.1) | 24(10.7) | 1.15(0.76–1.89) | 1.09(0.69–1.71) | 19(9.5) | 1.08(0.45–1.77) | 1.10(0.51–1.63) |
| Fetal distress | 71(29.2) | 61(27.1) | 0.90(0.72–1.33) | 0.86(0.74–1.19) | 55(27.6) | 0.92(0.71–1.20) | 0.94(0.71–1.23) |
| Preterm birth | 39(16.0) | 43(19.1) | 1.19(0.73–1.72) | 1.11(0.64–1.65) | 29(14.6) | 0.893(0.45–1.49) | 0.78(0.40–1.28) |
| Macrosomia | 42(17.7) | 15(6.6) | 0.51(0.39–0.67)b | 0.66(0.52–0.78)b | 45(22.6) | 1.40(1.27–2.10)b | 1.20(1.02–1.82)b |
| SGA | 18(7.4) | 20(8.8) | 1.23(0.84–1.77) | 1.12(0.72–1.61) | 10(5.0) | 0.89(0.61–1.13) | 0.90(0.79–1.01) |
| LGA | 58(23.9) | 17(14.2) | 0.63(0.43–0.71)b | 0.71(0.51–0.82) b | 71(35.7) | 1.61(1.43–2.15)b | 1.42(1.24–1.97)b |
Multivariate analyses were adjusted for for maternal age, pre-pregnancy BMI, maternal education, IVF, FPG, 2-h blood glucose. The results were presented with an adjusted odds ratio, aOR (95% CI);
IOM, Institute of Medicine; GWG, gestational weight gain; HDP, hypertensive disorders of pregnancy; PROM, premature rupture of the membranes; SGA, small for gestational age; LGA, large for gestational age; OR odds ratio; CI, Confidence interval
aP < 0.01
bP < 0.05,compared with the within IOM guideline subjects
Association of rate of GWG in the third trimester of pregnancy with APOs among women with GDM
We then analyzed the association between rate of GWG in the third trimester of pregnancy and APOs; 738 women with GDM were included for analysis. Women with GDM with rate of GWG above the IOM guidelines in the third trimester of pregnancy were associated with a significantly increased risk of cesarean delivery (aOR = 1.48; 95% CI 1.16–2.34), HDP (aOR = 1.93; 95% CI 1.08–2.98), preeclampsia (aOR = 2.17; 95% CI 1.35–4.37), macrosomia (aOR = 2.02; 95% CI 1.51–2.64), and LGA (aOR = 1.79; 95% CI 1.51–2.54). This group was also associated with a significantly decreased risk of PROM (aOR = 0.51; 95% CI 0.40–0.67) and preterm birth (aOR = 0.51; 95% CI 0.37–0.72).
GDM patients with rate of GWG below the IOM guidelines were associated with a significantly increased risk of preterm birth (aOR = 1.52; 95% CI 1.12–2.05) and SGA (aOR = 1.21; 95% CI 1.10–1.69). This group was also associated with a significantly decreased risk of macrosomia (aOR = 0.52; 95% CI 0.39–0.63) and LGA (aOR = 0.71; 95% CI 0.51–0.82) (Table 5).
Table 5.
Association of adverse pregnancy outcome among gestational diabetes mellitus with IOM guideline on rate of GWG in third trimester of pregnancy
| Within (n = 258) | Below (n = 242) | Above (n = 238) | |||||
|---|---|---|---|---|---|---|---|
| n(%) (Reference) | n (%) | crude OR (95% CI) | Adjusted OR (95% CI) | n (%) | crude OR (95% CI) | Adjusted OR (95% CI) | |
| Caesarean delivery | 90(37.0) | 87(36.0) | 0.85(0.74–1.23) | 0.90(0.66–1.01) | 122(51.3) | 1.56(1.25–2.56)a | 1.48(1.16–2.34)b |
| HDP | 11(5.3) | 9(4.0) | 0.70(0.41–1.18) | 0.63(0.41–1.11) | 34(15.6) | 2.27(1.15–3.32)b | 1.93(1.08–2.98)b |
| preeclampsia | 5(1.9) | 5(2.1) | 1.15(0.69–1.47) | 1.07(0.60–1.32) | 24(10.1) | 2.30(1.47–4.53)b | 2.17(1.35–4.37)b |
| PROM | 127(49.2) | 121(50.0) | 1.08(0.87–1.39) | 1.01(0.92–1.30) | 73(30.8) | 0.57(0.41–0.79)b | 0.51(0.40–0.66)b |
| Postpartum hemorrhage | 23(8.9) | 22(9.0) | 1.15(0.67–1.79) | 1.08(0.62–1.71) | 23(9.6) | 1.35(0.75–1.77) | 1.27(0.63–1.59) |
| Fetal distress | 75(29.1) | 68(28.1) | 0.95(0.74–1.32) | 0.94(0.70–1.25) | 69(29.0) | 0.99(0.83–1.21) | 0.98(0.81–1.18) |
| Preterm birth | 40(15.5) | 78(32.2) | 1.74(1.43–2.16)a | 1.52(1.12–2.05)b | 9(4.2) | 0.42(0.33–0.64)a | 0.51(0.37–0.72)b |
| Macrosomia | 45(17.4) | 14(5.7) | 0.47(0.31–0.67)a | 0.52(0.39–0.63)a | 65(27.3) | 2.19(1.65–2.83)a | 2.02(1.51–2.64)a |
| SGA | 18(6.9) | 30(12.4) | 1.32(1.23–1.84)b | 1.21(1.10–1.69)b | 9(3.7) | 0.74(0.48–0.95)b | 0.86(0.52–1.27) |
| LGA | 62(24.0) | 31(12.8) | 0.56(0.42–0.71) | 0.67(0.55–0.79) | 100(42.0) | 1.97(1.58–2.73)a | 1.79(1.51–2.54)a |
Multivariate analyses were adjusted for for maternal age, pre-pregnancy BMI, maternal education, IVF, FPG, 2-h blood glucose. The results were presented with an adjusted odds ratio, aOR (95% CI);
IOM, Institute of Medicine; GWG, gestational weight gain; HDP, hypertensive disorders of pregnancy; PROM, premature rupture of the membranes; SGA, small for gestational age; LGA, large for gestational age; OR odds ratio; CI, Confidence interval
aP < 0.01
bP < 0.05,compared with the within IOM guideline subjects
Discussion
GDM is an abnormal glucose metabolism diagnosed and one of the common complications during pregnancy [24]. Some studies have reported the prevalence of GDM ranges from 18.1 ~ 41.4% based on IADPSG criteria [25], and the prevalence of GDM (6.1%) in this study was lower than previous studies, which may be related to the geographical differences, lifestyle changes, and lack part of 75 g OGTT. GDM and GWG have been previously reported to be associated with APOs [26, 27]. Considering the conflicting data regarding the relationship between inadequate GWG and APOs in women with GDM and the limited research on the association of the adequate range of GWG at different stages with APOs in GDM, we conducted a retrospective analysis among 1606 pregnant women with GDM. We showed the association between IOM guidelines for GWG, both in total and in the second and third trimesters of pregnancy, and APOs in women with GDM. In the present study, 33.9% of GDM women presented with a total GWG below the IOM guidelines, and 31.2% presented with a total GWG above the IOM guidelines. In a previous Chinese study, the rate of insufficient total GWG (29.6% and 12.5%) were found to be lower than our results [13, 20]. This variation may be due to rigorous lifestyle improvements, including nutritional therapy and exercise, leading to a leaner population in our study.
We then analyzed the associations of APOs with total GWG in women with GDM during pregnancy. Our results show that total GWG above the IOM guidelines increased the risk of LGA, macrosomia, cesarean delivery, HDP, and preeclampsia. Our findings were in agreement with several previous reports [26, 28–30]. Gou et al. showed that excessive GWG increased the OR for LGA and macrosomia [20]. Komem et al. demonstrated that total GWG above the IOM guidelines is related to cesarean delivery and LGA in women with GDM [26]. Furthermore, Cheng et al. performed the largest trial to date to retrospectively analyze data among women with GDM, which showed a remarkable risk for cesarean delivery, macrosomia, and LGA among women with GWG above the IOM guidelines [31]. However, Scifres et al. reported that women with both excessive GWG and insufficient GWG had a higher risk for macrosomia, which may be due to a different grouping method [32]. In addition, Cheng et al. showed that women with GWG above the IOM guidelines had a high risk of preterm birth [31]. Huang et al. found that, in general, pregnant women with both insufficient and excessive GWG had a higher risk for preterm birth [13]. In the present study, we showed that pregnant women with total GWG above the IOM guidelines had a lower risk of preterm birth, while pregnant women with total GWG below the IOM guidelines had an increased odds of preterm birth. These findings suggest that reasonable GWG among women with GDM may shorten the incidence of preterm birth. In concordance with other reports, our results also showed that women with total GWG below the IOM guidelines had a decreased odds of macrosomia, with an increased odds of preterm birth and SGA [16, 20, 21]. In contrast, Gou et al. showed that insufficient GWG did not increase the risk for SGA [20].
Recent studies reported the influence of GWG in the second and third trimesters of pregnancy on the incidence of APOs [33, 34]. For example, Bouvier et al. found that women with GWG above the IOM guidelines had an increased odds of HDP, cesarean delivery, macrosomia, LGA, and hypoglycemia in the second and third trimesters of pregnancy [33]. Wu et al. calculated GWG ranges using receiver operating characteristic (ROC) curve analysis (ROC targets) in a retrospective cohort study of women with GDM in Shanghai, China. They showed that ROC targets that provide better GWG guidelines during the second and third trimesters could improve pregnancy outcomes [35]. However, studies on the association of GWG in the second and third trimesters in women with GDM with APOs are limited. Thus, in the present study, we further analyzed the effect of IOM guidelines for rate of GWG in the second and third trimesters of pregnancy on APOs among women with GDM. Our results showed that rate of GWG above the IOM guidelines in the second and third trimesters of pregnant women with GDM was associated with a higher risk of HDP, preeclampsia, macrosomia, and LGA. LGA has been reported to be associated with excessive weight gain in the second trimester of women with GDM in a previous Brazilian cohort study by Drehmer et al., which confirms the results of our study [36]. Drehmer et al. also found that insufficient GWG in second trimester associated with SGA. In another retrospective observational study in India, Kashyap et al. found that pregnant women who had poor rate of GWG in second trimester were at an increased risk of SGA [37]. However, in our study, there were no statistically significant differences in the odds ratios of SGA in the below or above IOM guidelines group. In addition, we found that women with rate of GWG above the IOM guidelines in the third trimester of pregnancy were associated with a significantly decreased risk of preterm birth. However, our findings showed that women with total GWG below the IOM guidelines were associated with a significantly increased risk of preterm birth, which is in contrast with a previous report [36]. A fairly large body of literature on mechanisms linking GWG to preterm birth had been reported, a lower rate of GWG during pregnancy is associated with an increased risk of preterm delivery, and that a slow rate of gain during the latter part of pregnancy may be particularly important [38]. The inconsistency may be due to the different study populations and the adjusted confounding variables. Our findings on the relationship between APOs among women with GDM and IOM guidelines for GWG in the second and third trimesters may influence clinical practitioners to pay more attention to the control of GWG.
The study has several strengths. First, this study included a relatively large sample size and we adjusted for confounding factors to ensure reliable assessments. Second, we comprehensively analyzed the associations between IOM guidelines for GWG both in total and in the second and third trimesters of pregnancy with APOs in women with GDM, which has rarely been researched previously.
Our study however had several limitations. First, this study was limited due to the retrospective design. Second, some unmeasured confounders including smoking, diet, physical activity, and other factors were not assessed; therefore, the influence of these factors on APOs could not be explored. Third, since our study did not record weight when GDM was diagnosed, we did not investigate the influence of GWG on APOs specifically after the diagnosis of GDM.
In conclusion, our research suggests that GWG above and below the IOM guidelines, both in total and in the second and third trimesters of pregnancy, is a risk indicator for adverse obstetric outcomes in women with GDM. These findings suggest that it is essential to not only maintain an adequate total GWG during pregnancy, but also in the second and third trimesters among pregnant women with GDM. We hope to encourage physicians to deal with GWG using the IOM guidelines and to trigger intervention when it is required, which should help to reduce APOs. Prospective multicenter clinical investigations will be needed to elucidate the potential role of GWG in APOs among women with GDM.
Acknowledgements
Not applicable.
Abbreviations
- IOM
Institute of Medicine
- GWG
Gestational weight gain
- BMI
Body Mass Index
- IVF
In-vitro fertilization
- SD
Standard deviation
- FPG
Fasting blood glucose
- OGTT
Oral glucose tolerance test
- HDP
Hypertensive disorders of pregnancy
- PROM
Premature rupture of the membranes
- SGA
Small for gestational age
- LGA
Large for gestational age
- OR
Odds ratio
- CI
Confidence interval
Authors’ contributions
PS developed the protocol and project, collected and analyzed the data, drafted and substantively revised the work. AL collected data, analyzed the data and helped draft the work. XY developed the protocol and project, edited the manuscript and substantively revised the work. All authors gave final approval of the submitted version to be published.
Funding
No funding was procured for this work.
Availability of data and materials
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Declarations
Ethics approval and consent to participate
The study was approved by the Hospital Ethical Review Committee. Informed consent was not required from the women included in the analysis due to the retrospective design of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Spaight C, Gross J, Horsch A, Puder JJ. Gestational diabetes mellitus. Endocrine Dev. 2016;31:163–178. doi: 10.1159/000439413. [DOI] [PubMed] [Google Scholar]
- 2.Colagiuri S, Falavigna M, Agarwal MM, Boulvain M, Coetzee E, Hod M, Meltzer SJ, Metzger B, Omori Y, Rasa I, et al. Strategies for implementing the WHO diagnostic criteria and classification of hyperglycaemia first detected in pregnancy. Diabetes Res Clin Pract. 2014;103(3):364–372. doi: 10.1016/j.diabres.2014.02.012. [DOI] [PubMed] [Google Scholar]
- 3.Wendland EM, Torloni MR, Falavigna M, Trujillo J, Dode MA, Campos MA, Duncan BB, Schmidt MI. Gestational diabetes and pregnancy outcomes–a systematic review of the World Health Organization (WHO) and the International Association of Diabetes in Pregnancy Study Groups (IADPSG) diagnostic criteria. BMC Pregnancy Childbirth. 2012;12:23. doi: 10.1186/1471-2393-12-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yu W, Wu N, Li L, OuYang H, Qian M, Shen H. A review of research progress on glycemic variability and gestational diabetes. Diab Metab Syndr Obes Targets Ther. 2020;13:2729–2741. doi: 10.2147/DMSO.S261486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shang M, Lin L, Ma L, Yin L. Investigation on the suitability of the International Association of Diabetes and Pregnancy Study Group diagnostic criteria for gestational diabetes mellitus in China. J Obstetr Gynaecol. 2014;34(2):141–145. doi: 10.3109/01443615.2013.832177. [DOI] [PubMed] [Google Scholar]
- 6.Vinturache A, Moledina N, McDonald S, Slater D, Tough S. Pre-pregnancy Body Mass Index (BMI) and delivery outcomes in a Canadian population. BMC Pregnancy Childbirth. 2014;14:422. doi: 10.1186/s12884-014-0422-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aune D, Sen A, Henriksen T, Saugstad OD, Tonstad S. Physical activity and the risk of gestational diabetes mellitus: a systematic review and dose-response meta-analysis of epidemiological studies. Europ J Epidemiol. 2016;31(10):967–997. doi: 10.1007/s10654-016-0176-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Blomberg M. Maternal and neonatal outcomes among obese women with weight gain below the new Institute of Medicine recommendations. Obstetr Gynecol. 2011;117(5):1065–1070. doi: 10.1097/AOG.0b013e318214f1d1. [DOI] [PubMed] [Google Scholar]
- 9.Shin D, Song WO. Prepregnancy body mass index is an independent risk factor for gestational hypertension, gestational diabetes, preterm labor, and small- and large-for-gestational-age infants. J Matern Fetal Neonatal Med. 2015;28(14):1679–1686. doi: 10.3109/14767058.2014.964675. [DOI] [PubMed] [Google Scholar]
- 10.Mohammadi M, Maroufizadeh S. The effect of prepregnancy body mass index on birth weight, preterm birth, cesarean section, and preeclampsia in pregnant women. J Matern Fetal Neonatal Med. 2019;32(22):3818–3823. doi: 10.1080/14767058.2018.1473366. [DOI] [PubMed] [Google Scholar]
- 11.Siega-Riz AM, Viswanathan M, Moos MK, Deierlein A, Mumford S, Knaack J, Thieda P, Lux LJ, Lohr KN. A systematic review of outcomes of maternal weight gain according to the Institute of Medicine recommendations: birthweight, fetal growth, and postpartum weight retention. Am J Obstetr Gynecol. 2009;201(4):339.e331–314. doi: 10.1016/j.ajog.2009.07.002. [DOI] [PubMed] [Google Scholar]
- 12.Carreno CA, Clifton RG, Hauth JC, Myatt L, Roberts JM, Spong CY, Varner MW, Thorp JM, Jr, Mercer BM, Peaceman AM, et al. Excessive early gestational weight gain and risk of gestational diabetes mellitus in nulliparous women. Obstetr Gynecol. 2012;119(6):1227–1233. doi: 10.1097/AOG.0b013e318256cf1a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huang A, Ji Z, Zhao W, Hu H, Yang Q, Chen D. Rate of gestational weight gain and preterm birth in relation to prepregnancy body mass indices and trimester: a follow-up study in China. Reprod Health. 2016;13(1):93. doi: 10.1186/s12978-016-0204-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu L, Hong Z, Zhang L. Associations of prepregnancy body mass index and gestational weight gain with pregnancy outcomes in nulliparous women delivering single live babies. Scientific Rep. 2015;5:12863. doi: 10.1038/srep12863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Berggren EK, Stuebe AM, Boggess KA. Excess maternal weight gain and large for gestational age risk among women with gestational diabetes. Am J Perinatol. 2015;32(3):251–256. doi: 10.1055/s-0034-1383848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gante I, Amaral N, Dores J, Almeida MC. Impact of gestational weight gain on obstetric and neonatal outcomes in obese diabetic women. BMC Pregnancy Childbirth. 2015;15:249. doi: 10.1186/s12884-015-0692-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kase BA, Cormier CM, Costantine MM, Hutchinson M, Ramin SM, Saade GR, Monga M, Blackwell SC. Excessive gestational weight gain in women with gestational and pregestational diabetes. Am J Perinatol. 2011;28(10):761–766. doi: 10.1055/s-0031-1280857. [DOI] [PubMed] [Google Scholar]
- 18.Park JE, Park S, Daily JW, Kim SH. Low gestational weight gain improves infant and maternal pregnancy outcomes in overweight and obese Korean women with gestational diabetes mellitus. Gynecol Endocrinol. 2011;27(10):775–781. doi: 10.3109/09513590.2010.540597. [DOI] [PubMed] [Google Scholar]
- 19.Yasuda S, Iuchi T, Goto A, Katanoda K. Weight control before and during pregnancy for patients with gestational diabetes mellitus. J Diabetes Investig. 2019;10(4):1075–1082. doi: 10.1111/jdi.12989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gou BH, Guan HM, Bi YX, Ding BJ. Gestational diabetes: weight gain during pregnancy and its relationship to pregnancy outcomes. Chin Med J. 2019;132(2):154–160. doi: 10.1097/CM9.0000000000000036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miao M, Dai M, Zhang Y, Sun F, Guo X, Sun G. Influence of maternal overweight, obesity and gestational weight gain on the perinatal outcomes in women with gestational diabetes mellitus. Scientific Rep. 2017;7(1):305. doi: 10.1038/s41598-017-00441-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guidelines IOMU . Weight Gain During Pregnancy: Reexamining the Guidelines. Washington (DC): National Academy of Sciences. National Academies Press (US); 2009. [PubMed] [Google Scholar]
- 23.Metzger BE, Gabbe SG, Persson B, Buchanan TA, Catalano PA, Damm P, Dyer AR, Leiva A, Hod M, Kitzmiler JL, et al. International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes care. 2010;33(3):676–682. doi: 10.2337/dc09-1848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Standards of Medical Care in Diabetes-20212 Classification and diagnosis of diabetes. Diabetes Care. 2021;44:S15–S33. doi: 10.2337/dc21-S002. [DOI] [PubMed] [Google Scholar]
- 25.Saeedi M, Cao Y, Fadl H, Gustafson H, Simmons D. Increasing prevalence of gestational diabetes mellitus when implementing the IADPSG criteria: a systematic review and meta-analysis. Diabetes Res Clin Pract. 2021;172:108642. doi: 10.1016/j.diabres.2020.108642. [DOI] [PubMed] [Google Scholar]
- 26.Komem D, Salman L, Krispin E, Arbib N, Bardin R, Wiznitzer A, Hadar E. Gestational weight gain and weight loss among women with gestational diabetes mellitus. Diab Res Clin Pract. 2018;141:88–97. doi: 10.1016/j.diabres.2018.04.034. [DOI] [PubMed] [Google Scholar]
- 27.Viecceli C, Remonti LR, Hirakata VN, Mastella LS, Gnielka V, Oppermann ML, Silveiro SP, Reichelt AJ. Weight gain adequacy and pregnancy outcomes in gestational diabetes: a meta-analysis. Obes Rev. 2017;18(5):567–580. doi: 10.1111/obr.12521. [DOI] [PubMed] [Google Scholar]
- 28.Shmueli A, Borovich A, Bergel R, Ovadia T, Hiersch L, Ashwal E, Yogev Y, Aviram A. Gestational weight gain among nutritionally treated GDM patients. J Matern Fetal Neonatal Med. 2018;31(9):1177–1181. doi: 10.1080/14767058.2017.1311316. [DOI] [PubMed] [Google Scholar]
- 29.Restall A, Taylor RS, Thompson JM, Flower D, Dekker GA, Kenny LC, Poston L, McCowan LM. Risk factors for excessive gestational weight gain in a healthy, nulliparous cohort. J Obes. 2014;2014:148391. doi: 10.1155/2014/148391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Egan AM, Dennedy MC, Al-Ramli W, Heerey A, Avalos G, Dunne F. ATLANTIC-DIP: excessive gestational weight gain and pregnancy outcomes in women with gestational or pregestational diabetes mellitus. J Clin Endocrinol Metab. 2014;99(1):212–219. doi: 10.1210/jc.2013-2684. [DOI] [PubMed] [Google Scholar]
- 31.Cheng YW, Chung JH, Kurbisch-Block I, Inturrisi M, Shafer S, Caughey AB. Gestational weight gain and gestational diabetes mellitus: perinatal outcomes. Obstetr Gynecol. 2008;112(5):1015–1022. doi: 10.1097/AOG.0b013e31818b5dd9. [DOI] [PubMed] [Google Scholar]
- 32.Scifres C, Feghali M, Althouse AD, Caritis S, Catov J. Adverse outcomes and potential targets for intervention in gestational diabetes and obesity. Obstetr Gynecol. 2015;126(2):316–325. doi: 10.1097/AOG.0000000000000928. [DOI] [PubMed] [Google Scholar]
- 33.Bouvier D, Forest JC, Dion-Buteau E, Bernard N, Bujold E, Pereira B. Association of maternal weight and gestational weight gain with maternal and neonate outcomes: a prospective cohort study. J Clin Med. 2019;8(12):2074. [DOI] [PMC free article] [PubMed]
- 34.Kominiarek MA, Saade G, Mele L, Bailit J, Reddy UM, Wapner RJ, Varner MW, Thorp JM, Jr, Caritis SN, Prasad M, et al. Association between gestational weight gain and perinatal outcomes. Obstetr Gynecol. 2018;132(4):875–881. doi: 10.1097/AOG.0000000000002854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wu JN, Gu WR, Xiao XR, Zhang Y, Li XT, Yin CM. Gestational weight gain targets during the second and third trimesters of pregnancy for women with gestational diabetes mellitus in China. Eur J Clin Nutr. 2019;73(8):1155–1163. doi: 10.1038/s41430-018-0358-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Drehmer M, Duncan BB, Kac G, Schmidt MI. Association of second and third trimester weight gain in pregnancy with maternal and fetal outcomes. PloS one. 2013;8(1):e54704. doi: 10.1371/journal.pone.0054704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kashyap H, Sharma D, Gala A, Pratap OT, Murki S. Effect of second trimester and third trimester weight gain on immediate outcomes in neonates born to mothers with gestational diabetes: a retrospective observational study from India. J Matern Fetal Neonatal Med. 2019;32(24):4133–4138. doi: 10.1080/14767058.2018.1482270. [DOI] [PubMed] [Google Scholar]
- 38.Carmichael S, Abrams B. A critical review of the relationship between gestational weight gain and preterm delivery. Obstetrics and gynecology. 1997;89:865–873. doi: 10.1016/S0029-7844(97)00047-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.