Abstract
Introduction
Pleomorphic adenoma of the minor salivary gland is not uncommon. Although malignant lesion is the most common in the minor salivary glands, benign lesion has been also reported. Many ectopic sites for minor salivary gland including the lip have been reported mainly intra-orally. But external cutaneous lesion is not that common, which will confuse the diagnosis.
Case presentation
This is a case report of a small 1.5 × 1 cm lesion in the left side of the upper lip in a healthy male. The lesion is fixed to the skin and was confused as dermal sebaceous cyst, which was excised with 2 mm safe margin under local anesthesia in an academic setting and closed primarily. Wound healed completely with no local complication and no evidence of recurrence in 1 year.
Discussion
Minor salivary glands are numerous in numbers specially in the oral cavity mainly in the hard and soft palate. Ectopic site in the head and neck area is well documented including the upper lip. But cutaneous presentation in the skin of the upper lip is not very common and can be easily missed especially if the specimen is not sent to permanent pathology. Pleomorphic adenoma has a unified histopathological feature that can be diagnosed by expert histopathologist.
Conclusion
Even for benign looking skin lesions excision with safe margin and histopathology should be the standard of care. By executing this we ensure a serious malignancy will not be missed, were additional surgical or non-surgical management might be considered necessary.
Keywords: Skin lesion, Pleomorphic adenoma, Histopathological examination
Highlights
-
•
Pleomorphic adenoma is the most common salivary gland benign tumor.
-
•
Ectopic site is well known in the literature.
-
•
Cutaneous presentation of pleomorphic adenoma is extremely rare.
-
•
Histopathology examination for any excised lesion is extremely crucial even when benign looking.
-
•
Occasionally further surgical or non surgical treatment might be necessary.
1. Introduction
Small or minor salivary glands are separate entity of salivary cells, and they exist in hefty numbers in the intraoral cavity most commonly in the hard and soft palate. They generate around 10% of the total salivary secretion of the oral cavity per day. Most of minor salivary gland lesions are malignant but still benign lesion could appear. Although pleomorphic adenoma is the most common benign salivary gland neoplasm affecting the parotid gland, it still could present in the submandibular, sublingual, and minor salivary glands. It was first described by Willis as it has a unique histopathological feature of mixed epithelial cell tumor that is fully capsulated by fibrosis of the outer parenchymal cells [1], [2], [3], [4], [5].
Minor salivary glands rarely present in unusual location like the floor of the moth, tongue, upper gingival sulcus, upper and lower lips. Because of that fact the presence of pleomorphic adenoma lesion in the upper lip is extremely rare despite it has been reported in the literature. Lesions that lack mucosal communication and appears on the cutaneous aspect of the external lips makes the clinical diagnosis slope quit long. Histopathological evaluation and diagnosis are crucial in these cases to avoid missing a serious malignant skin or salivary gland conditions that require extra measure for treatment as well reduce the risk of recurrence or metastasis [6], [7]. The work has been reported in line with the SCARE 2020 criteria [8].
2. Case report
A 46-year-old male presented to the plastic surgery clinic at our university hospital with a 2-year history of painless, progressive left upper lip external swelling. There was no history of previous trauma, and past medical and dental history were unremarkable. The patient was not on any medication, and has no significant family medical history, or genetic disorder. The patient is married with four children and works as an engineer in a private company. On clinical examination, the patient's general exam was unremarkable. The local lesion examination revealed a firm and rubbery, well-circumscribed lesion in the left side of the external lip close to the left philtrum columns fixed to the skin with no clear central punctum measuring 1.5 × 1 cm in diameter. No evidence of extension to the intra-oral mucosa. It appears to be superficial to underlaying orbicularis oris muscle, with full mouth muscle function with no limitation or asymmetry, with negative regional lymphadenopathy [Fig. 1]. Clinical impression was a localized sebaceous cyst and patient was planned for excision under local anesthesia to be performed by the first author (A.G). A written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Fig. 1.
Preoperative photo of the lesion.
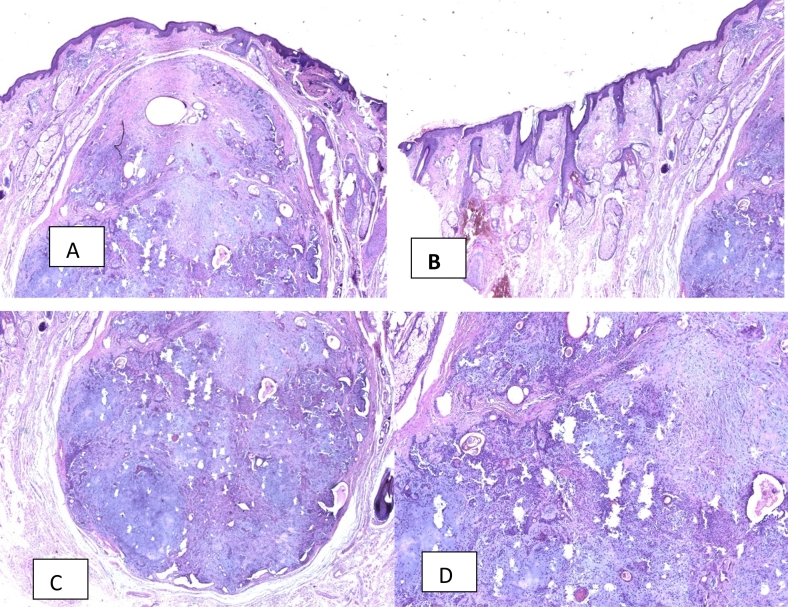
The lesion was marked then LA with 2% lignocaine with 1:100,000 adrenaline hydrochloride around 5 cc was injected in the normal skin surrounding the lesion. A wedge shape incision was made with 2 mm of safe margin down to orbicularis muscle lesion that was completely excised and sent to histopathology. After accomplishing good hemostasis, the defect was closed in vertical fashion lying on the philtrum columns, with 4/0 vicryl and 6/0 prolen [Fig. 2]. Postoperative course was unremarkable, and sutures were removed after 10 days. The excised lesion was round pinkish and encapsulated. Patient was discharged home on the same day and followed up in the clinic after 10 days to remove the surgical sutures. Permanent pathology came back as pleomorphic adenoma that is completely excised and followed up for 3 months with no signs of recurrence and referred to head and neck surgeon to ensure that nothing further is required. The patient was seen again after 1 year and no evidence of local recurrence. The histological findings showed circumscribed benign minor salivary gland neoplasm that shows epithelial (ductal) component forming the inner layer of cyst and tubules and myoepithelial cells present as the outer layer of cysts and tubules and scattered within the myxoid stroma. The diagnosis of pleomorphic adenoma was established [Fig. 3]. Patient tolerated the procedures well with no complication after the intervention. Patient was completely satisfied with the outcome and planned for yearly follow up to ensure no local recurrence.
Fig. 2.
Lesion post excision.
Fig. 3.
Histopathology of the cutaneous pleomorphic adenoma A. The lesion with surrounding skin. B.C. The edge of skin and pleomorphic adenoma. D. The pleomorphic adenoma lesion.
3. Discussion
Pleomorphic adenoma of the salivary glands in the most common benign sub type in all major salivary gland that is highly widespread in the parotid gland to around 60–70% of the cases. The involvement of the minor salivary glands has been reported in the literatures with majority of the lesions are malignant and benign cases composing around 18%. Minor salivary glands are common in the intraoral regions with hard and soft palate being the most common followed by the lip region as the second most common then cheek, floor of the mouth, retromolar trigon, gingiva. But presence of minor salivary glands with pleomorphic adenoma lesion on the external cutaneous skin of the upper lip with no mucosal involvement is extremely rare. Upper lip involvement with pleomorphic adenoma is reported in younger age group averaging the 4th decade and it has been reported in children, with upper lip involved more than the lower one 6:1 ratio [3], [4], [9], [10]. Suka et al. reviewed the literatures found upper lip involvement with pleomorphic adenoma is extremely rare only 38 cases were reported [11].
Majority of lip tumors usually appears intraorally in the lip mucosa as solitary bump or nodule and has some relation to increase in size with eating, but our case presents as well-defined pink nodule in the external skin with small punctum resembling a sebaceous cyst or any other benign adnexal tumors [12]. No clear etiological factor has been found studies attributed minor trauma or irritation of the mucosa might be related [13], [14].
Generally diagnosing an external pink skin lesion that is asymptomatic presents a challenge with wide range of benign or malignant list is available that original from the skin like (Benign: clear acanthoma, keratoacanthoma), (Malignant: Bowen's disease basal cell carcinoma, squamous cell carcinoma), or originate from the skin appendages (Benign: sebaceous cyst, molluscum contagiosum, dermatofibroma, syringoma, cylindroma, tubular adenoma), (Malignant: tubular carcinoma, adenoid cystic carcinoma).
Although majority of small skin external lesion can be diagnosed by history and physical examination, it is still very crucial to send any excised skin lesion even benign looking lesion a must be sent for histopathological examination by an expert dermatological dermatologist to ensure any malignant lesion or even ectopic uncommon condition not been unexploited [15], [16], [17].
Rakesh et al. reviewed 112 cases of benign looking lesions all sent to histopathology found cases of skin malignancy in form Bowen's disease and basal cell carcinoma, which will be missed if it was not sent to histopathological examination [18].
Histologically Pleomorphic Adenoma has a distinct feature being well circumscribed with of epithelial and myoepithelial cells surrounded by false capsule resulted from fibrosis of salivary parenchyma, usually treatment is wide surgical excision failure to resect the entire capsule well result in increased chance of local recurrence of around 2%, and require long term of follow-up [1], [3], [5].
4. Conclusion
In summary, pleomorphic adenoma of the lips are rare, and lesions that present as external cutaneous lesion is even more rare and can confuse practitioners with a long list of skin and its appendages differential diagnosis and must have a high index of suspicion for the correct diagnosis. The excised lesion must be sent for histopathological examination to obtain the correct diagnosis, and not to forego a serious ectopic malignant condition like the ectopic salivary gland malignant tumor. The best treatment modality is complete wide surgical excision. However, practitioners should note that pleomorphic adenoma can recur even several years after the surgical excision. In addition, the transformation to the malignant state is possible, and thus long-term follow-up is essential.
Source of funding
None.
Ethical approval
Approved by the IRB committee at King Khalid University Hospital research center King Saud University.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Research registration
Not indicated this is not a new invented technique it's just modification of an existing one.
Guarantor
Dr. Adnan G Gelidan.
Provenance and peer review
Not commissioned, externally peer-reviewed.
CRediT authorship contribution statement
Author research idea, performed the surgical procedure, wrote the manuscript of the case report data collection and literature review.
Declaration of competing interest
None.
Acknowledgment
This work is supported by the college of medicine research center deanship of scientific research in King Saud University Riyadh Saudi Arabia.
References
- 1.Taiwo A.O., Akinshipo A., Braimah R.O., Ibikunle A.A. Pleomorphic adenoma of the upper lip: a case report. Saudi J. Med. Med. Sci. January-April 2018;6(1) doi: 10.4103/sjmms.sjmms_109_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Debnath S.C., Adhyapok A.K. Pleomorphic adenoma (benign mixed tumour) of the minor salivary glands of the upper lip. J. Maxillofac. Oral Surg. 2010;9:205–208. doi: 10.1007/s12663-010-0052-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Buchner A., Merrell P.W., Carpenter W.M. Relative frequency of intra-oral minor salivary gland tumors: a study of 380 cases from Northern California and comparison to reports from other parts of the world. J. Oral. Pathol. Med. 2007;36:207–214. doi: 10.1111/j.1600-0714.2007.00522.x. [DOI] [PubMed] [Google Scholar]
- 4.Bhatia J.S.S. Pleomorphic adenoma of upper lip: a rare case presentation. Indian J. Otolaryngol. Head Neck Surg. 2019;71:755–758. doi: 10.1007/s12070-018-1537-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eveson J.W., Nagao T. Diseases of the salivary glands. In: Barnes L., editor. Surgical Pathology of the Head and Neck. Informa; New York: 2009. pp. 475–648. [Google Scholar]
- 6.Nagura I., Miyata M., Okabe K., Suzuki T., Takagi J., Katayanagi K., Kurumaya H., Sakashita H. Pleomorphic adenoma of the upper lip : report of two cases. Jpn. J. Oral Diagn. 2005;18:352–355. [Google Scholar]
- 7.Shrestha A., Reddy N.S., Ganguly S.N. Pleomorphic adenoma of the upper lip: a case report. J. Coll. Med. Sci. Nepal. 2010;6(1):51–53. [Google Scholar]
- 8.for the SCARE Group. Agha R.A., Franchi T., Sohrabi C., Mathew G. The SCARE 2020 guideline: updating consensus Surgical Case Report (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 9.Lotufo M.A., Junior C.A.L., de Mattos J.P., Franca C.M. Pleomorphic adenoma of the upper lip in a child. J. Oral Sci. 2008;50(2):225–228. doi: 10.2334/josnusd.50.225. [DOI] [PubMed] [Google Scholar]
- 10.Kataria S.P., Tanwar P., Sethi D., Garg M. Pleomorphic adenoma of the upper lip. J Cutan Aesthet Surg. 2011 Sep-Dec;4(3):217–219. doi: 10.4103/0974-2077.91260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Suka N., Magoshi S., Ogasawara Y. Pleomorphic adenoma in the upper lip: a case report and literature review. J. Meikai Dent. Med. 2021;50(1):59–65. [Google Scholar]
- 12.Debnath S.C., Adhyapok A.K. Pleomorphic adenoma (benign mixed tumour) of the minor salivary glands of the upperLip. J. Maxillofac. Oral Surg. 2010;9:205–208. doi: 10.1007/s12663-010-0052-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Piemonte E., Lazos J., Belardinelli P., Secchi D., Brunotto M., Lanfranchi-Tizeira H. Oral cancer associated with chronic mechanical irritation of the oral mucosa. Med. Oral Patol. Oral Cir Bucal. Med. Oral S.L. 2018;23 doi: 10.4317/medoral.22017. 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Singhvi H.R., Malik A., Chaturvedi P. The role of chronic mucosal trauma in oral cancer: a review of literature. Indian J. Med. Paediatr. Oncol. 2017:44–50. doi: 10.4103/0971-5851.203510. Medknow Publications. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.M.C.R.F. Van dijk , K.K.H. Aben F. Van hees , A. Klaasen W.A.M. Blokx L.A. Kiemeney D.J. Ruiter Expert review remains important in the histopathological diagnosis of cutaneous melanocytic lesions. Histopathology Volume 52, Issue 2 p. 139-146. [DOI] [PubMed]
- 16.P. Salmon N Mortimer M. Rademaker L Adams A Stanway S. Hill Surgical excision of skin cancer: the importance of training Br. J. Dermatol. Volume 162, Issue 1 p. 117-122. [DOI] [PubMed]
- 17.Saha A., Das N.K., Gharami R.C. A Clinico-histopathological study of appendageal skin tumors, affecting head and neck region in patients attending the dermatology OPD of a tertiary care centre in eastern India. Indian J. Dermatol. 2011;56:33–36. doi: 10.4103/0019-5154.77548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rakesh M., Ravi J., Kulkarni C.V., Narang S., Mittal M., Patidar H. Histopathological study of dermatological lesions – a retrospective approach. Int. J. Med. Sci. Public Health. 2014;3(9) [Google Scholar]