Introduction
Cutaneous metastasis has a frequency of up to 10% among all metastatic cancer forms, with breast cancer being the most common, accounting for 30% of all cases.1 Thus, when a patient with a history of estrogen receptor-positive (ER+) breast cancer presents with an ER + cutaneous metastases, it is common to assume breast cancer recurrence. However, some lung adenocarcinomas can be ER +. Thus, it is important for clinicians to request further testing to determine the source of the lesion, given the poor prognosis of metastatic lung carcinomas.2,3 We present a case of cutaneous metastases from an ER + lung cancer primary in a patient with a history of ER + breast cancer.
Case report
A 70-year-old female former smoker with a history of ER+ and progesterone receptor-positive (PR+) mixed ductal/lobular breast cancer treated 10 years prior presented with intermittently pruritic lesions on the anterior aspect of the chest persisting for 10 months. Physical examination revealed indurated pink papules coalescing into a large 8-cm plaque with a few scattered indurated papules on the upper right side of the chest (Fig 1).
Fig 1.
Pruritic papules coalescing into an indurated plaque on the anterior aspect of the chest of a 70-year-old woman.
Six months prior, computed tomography was performed to investigate a sternal bony prominence, which revealed a large left lower lung mass and bony metastases, representing an ER + adenocarcinoma treated with letrozole. Biopsy of her upper right side of the chest wall plaqueshowed a metastatic carcinoma that was ER+ and a presumed recurrent metastatic breast cancer, since she was previously diagnosed in July 2009 with Stage IA (AJCC 9) 0.9-cm node negative, ER+/PR+, human epidermal growth factor receptor 2/neu-negative adenocarcinoma of the left breast with mixed ductal and lobular features. The patient was treated with lumpectomy and radiation therapy, followed by 5 years of anastazole 1 mg daily. In contrast to her PR + breast cancer, further immunohistochemistry studies revealed that the cutaneous metastasis was negative for PR, GATA-binding protein 3 (GATA3), and paired box 8, while positive for ER and thyroid transcription factor (TTF-1) These results were in contrast to the patient's prior breast cancer results—GATA-3 positive and PR/TTF-1/Cytokeratin 20 negative.
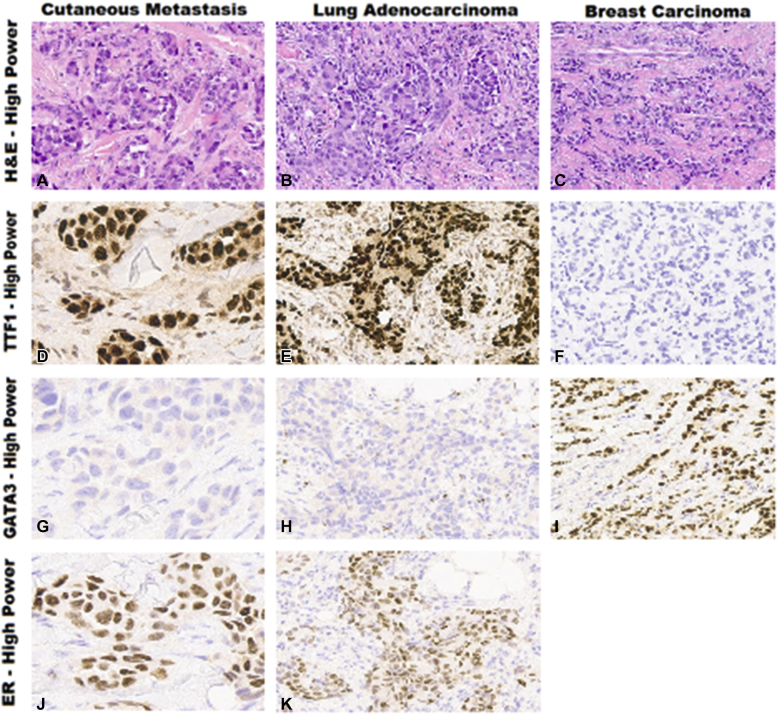
A punch biopsy from her chest showed dermal metastasis consistent with adenocarcinoma and tumor lymphovascular invasion (Fig 2, A) and immunohistochemistry-positive for ER (Fig 2, J), napsin A, TTF-1 (Fig 2, D), and Cytokeratin 7, while negative for PR, GATA-3 (Fig 2, G), and Cytokeratin 20, suggestive of metastatic lung adenocarcinoma (Fig 2, B, E, H, K) as opposed to breast carcinoma (Fig 2, C, F, I).
Fig 2.
Comparison of both cutaneous metastasis and lung adenocarcinoma stained using hematoxylin-eosin (A, B), TTF1 (D, E), GATA3 (G, H), and ER (J, K) with previous breast carcinoma stained using hematoxylin-eosin (C), TTF1 (F), and GATA3 (I). The cutaneous metastasis, similarly to the lung adenocarcinoma, was negative for GATA3, while positive for ER+ and TTF-1. These results were in stark contrast to the patient's prior breast cancer, which was GATA-3 positive and TTF-1 negative. ER, Estrogen receptor; GATA3, GATA-binding protein 3; TTF1, thyroid transcription factor-1.
A computed tomography scan performed in early October 2020 showed skull-based bony lesions consistent with metastatic disease, and the patient died shortly after from complications of her metastatic cancer.
Discussion
This is a rare case of a chest lesion from metastatic lung adenocarcinoma presenting as suspected recurrent ER + breast cancer. Lung adenocarcinoma is the second-most common malignancy in the United States and often presents with distant metastasis in the liver, adrenal glands, brain, and bone.4 The proportion of patients displaying cutaneous metastases ranges between 1% and 12%.5 Although these cutaneous lesions usually lack a particular clinical appearance, they tend to present as a solitary and painless mass.4,5
In approximately 20% to 60% of cases, cutaneous metastasis presents before the diagnosis of the primary malignancy and increases the risk of misdiagnosis.6 A small subset of lung adenocarcinomas are ER+, making them difficult to distinguish from primary breast carcinoma.2 Cutaneous metastases are further difficult to diagnose without concurrent respiratory symptoms, requiring immunohistochemical studies to confirm the origin of a lesion.7
Although cutaneous metastasis stemming from lung adenocarcinoma is a rare entity, it is often terminal.5 The appearance of cutaneous metastasis indicates advanced disease, with a median patient survival time of 2.9 months.5,8 In contrast, cutaneous metastasis from a breast carcinoma has a better prognosis, with a 13.8-month median survival time.8 Therefore, clinicians should thoroughly investigate clinical pathologic correlation, such as time lapse since previous incidences of cancers, and consider the use of molecular markers to determine the origin of cutaneous metastatic tumors more accurately and quickly, given the vastly different prognosis and therapeutic approach of lung versus breast metastasis.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
IRB approval status: Not applicable.
References
- 1.Araújo E., Barbosa M., Costa R., Sousa B., Costa V. A first sign not to be missed: cutaneous metastasis from breast cancer. Eur J Case Rep Intern Med. 2020;7(1):001356. doi: 10.12890/2020_001356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rodriguez-Lara V., Hernandez-Martinez J.M., Arrieta O. Influence of estrogen in non-small cell lung cancer and its clinical implications. J Thorac Dis. 2018;10(1):482–497. doi: 10.21037/jtd.2017.12.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Davis D.G., Siddiqui M.T., Oprea-Ilies G. GATA-3 and FOXA1 expression is useful to differentiate breast carcinoma from other carcinomas. Hum Pathol. 2016;47(1):26–31. doi: 10.1016/j.humpath.2015.09.015. [DOI] [PubMed] [Google Scholar]
- 4.Hussain J., Westerveld D., Sattari M. Cutaneous metastasis: a rare herald of a silent cancer. BMJ Case Rep. 2016;2016 doi: 10.1136/bcr-2015-213734. bcr2015213734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liao Y., Zhou L., Li M., Yu S., Zhou Y., Xie L. Cutaneous metastasis from lung adenocarcinoma presenting before discovery of the primary malignancy: a case report. Int J Clin Exp Pathol. 2019;12(2):657–663. [PMC free article] [PubMed] [Google Scholar]
- 6.Mollet T.W., Garcia C.A., Koester G. Skin metastases from lung cancer. Dermatol Online J. 2009;15(5):1. [PubMed] [Google Scholar]
- 7.Yeh C.N., Lin C.H., Chen M.F. Clinical and ultrasonographic characteristics of breast metastases from extramammary malignancies. Am Surg. 2004;70(4):287–290. [PubMed] [Google Scholar]
- 8.Schoenlaub P., Sarraux A., Grosshans E., Heid E., Cribier B. Survival after cutaneous metastasis: a study of 200 cases. Article in French. Ann Dermatol Venereol. 2001;128(12):1310–1315. [PubMed] [Google Scholar]