Abstract
Background
While socioeconomic disparities persist both pre- and post-transplantation, the impact of payer status has not been studied at the national level. We examined the association between public insurance coverage and waitlist outcomes among candidates listed for liver transplantation (LT) in the United States.
Methods
All adults (≥18 years) listed for LT between 2002-2018 in the United Network for Organ Sharing (UNOS) database were included. The primary outcome was waitlist removal due to death or clinical deterioration. Continuous and categorical variables were compared using the Kruskal-Wallis and chi-squared tests, respectively. Fine and Gray competing-risks regression was used to estimate sub-distribution hazard ratios for risk factors associated with delisting.
Results
Of 131,839 patients listed for LT, 61.2% were covered by private insurance, 22.9% by Medicare and 15.9% by Medicaid. The one-year cumulative incidence of delisting was 9.0% (95% CI: [8.3%-9.8%]) for patients with private insurance, 10.7% [9.9%-11.6%] for Medicare and 10.7% [9.8%-11.6%] for Medicaid. In multivariable competing-risks analysis, Medicare (HR 1.20 [1.17-1.24], p<0.001) and Medicaid (HR 1.20 [1.16-1.24], p<0.001) were independently associated with an increased hazard of death or deterioration compared to private insurance. Additional predictors of delisting included Black race (HR 1.06 [1.02-1.11], p=0.01) and Hispanic ethnicity (HR 1.05 [1.02-1.09], p=0.01), while college education (HR 0.89 [0.84-0.94], p<0.001) and employment (HR 0.81 [0.78-0.84], p<0.001) were associated with a decreased hazard of delisting.
Conclusions
In this study, LT candidates with Medicare or Medicaid had 20% increased risk of delisting due to death or clinical deterioration than those with private insurance. As more patients use public insurance to cover the cost of LT, targeted waitlist management protocols may mitigate the increased risk of delisting in this population.
Keywords: public insurance, waitlist outcomes, disparities, organ allocation, UNOS
Introduction
Liver transplantation (LT) is the only definitive therapy for end-stage liver disease and considered the standard of care for suitable candidates (1). Despite an increasing caseload and broader offer acceptance criteria, LT volume remains surpassed by the number of patients added to the LT waitlist annually in the United States (2,3). Importantly, the number of patients who die or are removed from the LT waitlist has increased significantly over the past decade (4).
Prior studies have highlighted the contribution of socioeconomic disparities to poor outcomes for those awaiting LT (2,5,6). Across all causes of liver failure, Black patients and those with publicly sponsored insurance were less likely to be listed for LT upon diagnosis (7,8). Once listed, Black and Hispanic patients have been consistently reported to have lower probabilities of receiving LT or surviving on the waitlist compared to those of White race (2,7,9,10). Among patients with hepatocellular carcinoma (HCC), those who were uninsured or insured by Medicaid had more advanced tumors and were less likely to undergo LT (5,6). Since the enactment of the Affordable Care Act (ACA) Medicaid expansion policy in 2014, an increasing number of patients have used public insurance to finance LT (11,12). Therefore, characterizing the effect of public insurance coverage on LT waitlist outcomes is particularly relevant.
Although several studies have explored the relationship between payer status and LT outcomes, none have examined how the former impacts removal from the LT waitlist at the national level. In this study, we examined the potential association between payer status and waitlist outcomes across liver disease etiologies. We hypothesized that patients with Medicare or Medicaid would have an increased likelihood of waitlist removal due to death or deterioration compared to those with private insurance.
Methods
This was a retrospective study of the United Network for Organ Sharing (UNOS) database, which is a comprehensive registry of organ transplants performed in the United States. The sample included all adult patients (≥18 years) listed for liver transplantation between 2002 and 2018. Patients under the age of 18 at listing and those listed for multiple organs, missing a final waitlist status, refusing transplant, or delisted due to improvement were excluded.
Variables for patient characteristics were defined according to definitions of the UNOS registry (13). Patients were stratified based on primary payer status (private health insurance, Medicare, or Medicaid). Liver disease etiologies were divided into the following categories: alcoholic liver disease, acute liver failure, cholestatic liver disease, hepatitis B, hepatitis C, hepatocellular carcinoma (HCC), nonalcoholic steatohepatitis (NASH), and other (14).
Reasons for removal from the waitlist were classified using UNOS removal codes for transplant (2, 3, 4, 14, 15, 18, 19, and 21), delisting due to medical deterioration (5 and 13), and death on the waitlist (8). The primary outcome of this study was removal from the waitlist due to death or clinical deterioration. Secondary outcomes included the rate of delisting due to death or deterioration and differences in the proportion delisted by UNOS geographic region.
Demographics and comorbidities of patients were analyzed by waitlist outcome. Continuous and categorical variables were compared using the Kruskal-Wallis test and chi-squared test, respectively. Non-parametric rank-based tests were used to assess temporal trends in waitlist mortality and delisting. With LT considered a competing event, cumulative incidence for death or clinical deterioration was calculated and stratified by insurance type. Fine and Gray competing-risk regressions were used to estimate univariate and multivariable sub-distribution hazard ratios (HRs) for risk factors associated with delisting and censored at time of waitlist removal. Covariates were chosen based on clinical relevance while optimization of the final multivariable model was based on receiver-operating characteristics (ROC) using Akaike’s Information Criteria. In all comparisons, p<0.05 was considered statistically significant. All statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC) and Stata IC 16 (StataCorp LP, College Station, TX). The study was deemed exempt from full review by the Institutional Review Board at the University of California, Los Angeles.
Results
Of 131,839 patients listed for LT during the study period, 80,694 (61.2%) were covered by private insurance, 30,150 (22.9%) by Medicare and 20,995 (15.9%) by Medicaid. Baseline demographics are reported in Table 1. Of the three insurance groups, Medicaid patients were the youngest (Medicaid: median 52, IQR 45-58 years; Medicare: median 62, IQR 54-67 years; private insurance: median 55, IQR 48-60 years; p<0.001) and most commonly female (Medicaid: 39.8%; Medicare: 38.6%; private insurance: 34.5%; p<0.001). Medicaid patients were also most likely to be Black (Medicaid: 11.0%; Medicare: 8.4%; private insurance: 7.4%), Hispanic (Medicaid: 25.1%; Medicare: 15.8%; private insurance: 11.5%) or Asian (Medicaid: 5.9%; Medicare: 3.5%; private insurance: 4.5%; p<0.001). Conversely, patients with private insurance were most likely to have a college education or be employed at listing (Table 1). The private insurance group also had the greatest proportion of patients who did not have either ascites or encephalopathy at listing (Table 1). Among liver disease etiologies, patients with Medicaid were more likely to have alcoholic liver disease, acute liver failure, hepatitis B and hepatitis C (Table 1). Lastly, Medicare insurance was most commonly associated with delisting due to death or clinical deterioration (Medicare: 35.0%; Medicaid: 33.2%; private insurance: 26.4%; p<0.001).
Table 1.
Patient demographics and comorbidities
| Private Insurance (N=80,694) |
Medicare (N=30,150) |
Medicaid (N=20,995) |
p-value | |
|---|---|---|---|---|
| Age, years | 55 (48-60) | 62 (54-67) | 52 (45-58) | <0.001 |
| Female | 34,659 (34.5) | 14,503 (38.6) | 10,925 (39.8) | <0.001 |
| Race | <0.001 | |||
| White | 75,888 (75.5) | 26,696 (71.1) | 15,392 (56.1) | |
| Black | 7,481 (7.4) | 3,159 (8.4) | 3,020 (11.0) | |
| Hispanic | 11,538 (11.5) | 5,937 (15.8) | 6,877 (25.1) | |
| Asian | 4,550 (4.5) | 1,296 (3.5) | 1,605 (5.9) | |
| Other* | 1,106 (1.1) | 458 (1.2) | 561 (2.0) | |
| Education | <0.001 | |||
| Less than high school | 2,724 (2.7) | 2,603 (6.9) | 3,049 (11.1) | |
| High school diploma/GED | 34,694 (34.5) | 15,920 (42.4) | 13,552 (49.4) | |
| Attended college | 23,026 (22.9) | 7,751 (20.7) | 4,837 (17.6) | |
| Associate's/Bachelor's degree | 18,167 (18.1) | 4,706 (12.5) | 2,027 (7.4) | |
| Graduate degree | 7,939 (7.9) | 2,071 (5.5) | 471 (1.7) | |
| Unknown | 13,980 (13.9) | 4,489 (12.0) | 3,518 (12.8) | |
| Waitlist Outcome | <0.001 | |||
| Transplanted | 59,406 (73.6) | 19,587 (65.0) | 14,029 (66.8) | |
| Death or Clinical Deterioration | 21,288 (26.4) | 10,563 (35.0) | 6,966 (33.2) | |
| Employed at listing | 29,599 (33.8) | 2,391 (6.9) | 1,570 (6.4) | <0.001 |
| Diabetes mellitus | 23,387 (23.3) | 12,726 (33.9) | 6,176 (22.5) | <0.001 |
| Dialysis twice in prior week at listing | 4,123 (4.1) | 2,224 (6.0) | 1,568 (5.8) | <0.001 |
| Previous malignancy | 12,302 (12.2) | 6,723 (17.9) | 2,882 (10.5) | <0.001 |
| MELD score at listing | 15 (11-22) | 15 (11-21) | 16 (12-24) | <0.001 |
| Total days on waitlist | 173 (32-558) | 184 (42-481) | 173 (26-552) | <0.001 |
| Liver disease etiology | <0.001 | |||
| Alcoholic liver disease | 21,704 (21.6) | 7,425 (19.8) | 8,396 (30.6) | |
| Acute liver failure | 4,635 (4.6) | 921 (2.5) | 1,421 (5.2) | |
| Cholestatic liver disease | 8,657 (8.6) | 2,306 (6.1) | 1,094 (4.0) | |
| Hepatitis B | 2,296 (2.3) | 600 (1.6) | 705 (2.6) | |
| Hepatitis C | 24,755 (24.6) | 9,676 (25.8) | 7,500 (27.3) | |
| HCC | 8,373 (8.3) | 4,365 (11.6) | 2,257 (8.2) | |
| NASH | 8,824 (8.8) | 4,910 (13.1) | 1,410 (5.1) | |
| Other | 21,318 (21.2) | 7,343 (19.6) | 4,672 (17.0) | |
| Encephalopathy | <0.001 | |||
| None | 43,123 (42.3) | 14,441 (38.5) | 9.535 (34.8) | |
| Grade 1-2 | 50,135 (50.0) | 20,607 (55.0) | 15,315 (55.9) | |
| Grade 3-4 | 7,122 (7.1) | 2,455 (6.6) | 2,564 (9.4) | |
| Ascites | <0.001 | |||
| Absent | 30,144 (30.0) | 10,113 (27.0) | 6,586 (24.0) | |
| Slight | 49,998 (49.8) | 19,339 (51.6) | 14,095 (51.4) | |
| Moderate | 20,238 (20.2) | 8,051 (21.5) | 6,733 (24.6) | |
| UNOS Region | <0.001 | |||
| Region 1 | 4,493 (4.5) | 1,776 (4.7) | 1,705 (6.2) | |
| Region 2 | 12,599 (12.5) | 4,789 (12.8) | 3,056 (11.1) | |
| Region 3 | 12,866 (12.8) | 5,661 (15.1) | 2,655 (9.7) | |
| Region 4 | 12,310 (12.2) | 5,004 (13.3) | 1,742 (6.3) | |
| Region 5 | 17,412 (17.3) | 5,178 (13.8) | 6,668 (24.3) | |
| Region 6 | 2,653 (2.6) | 783 (2.1) | 699 (2.6) | |
| Region 7 | 8,142 (8.1) | 3,036 (8.1) | 2,534 (9.2) | |
| Region 8 | 6,347 (6.3) | 2,268 (6.0) | 1,848 (6.7) | |
| Region 9 | 7,748 (7.7) | 2,743 (7.3) | 2,813 (10.3) | |
| Region 10 | 7,846 (7.8) | 2,925 (7.8) | 2,042 (7.4) | |
| Region 11 | 8,147 (8.1) | 3,383 (9.0) | 1,693 (6.2) |
Other race includes American Indian, Alaska Native, Native Hawaiian, Pacific Islander and multiracial. All continuous variables reported as median (IQR). All categorical variables reported as N (%). IQR: interquartile range; GED: general educational development; HCC: hepatocellular carcinoma
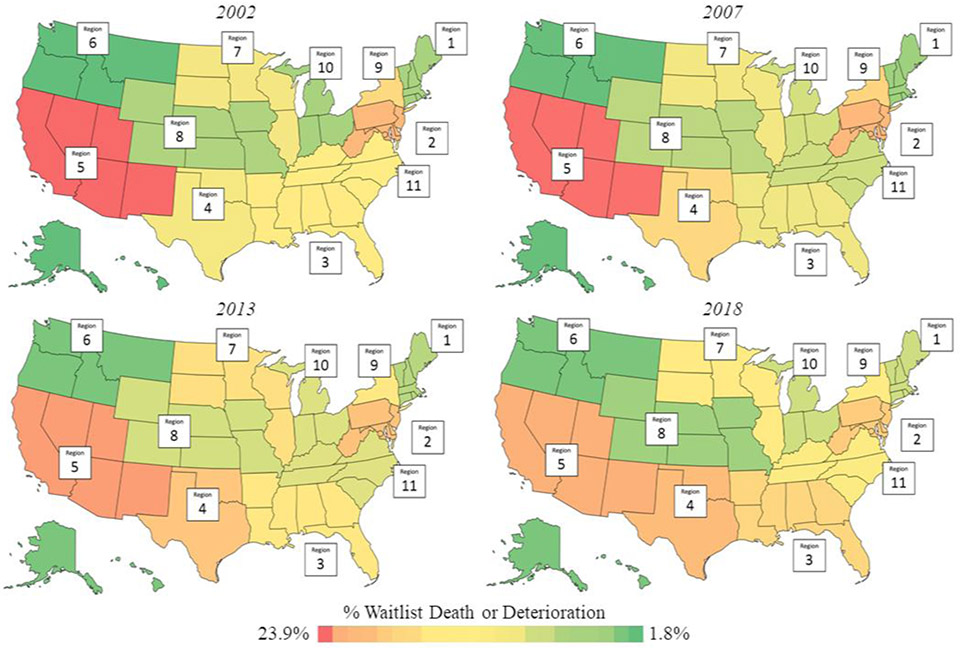
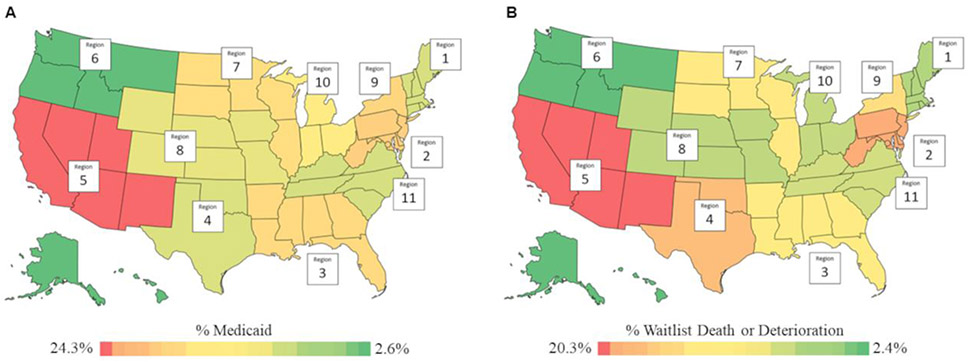
On regional analysis, the percentage of waitlist mortality and deterioration significantly increased from 2002 to 2018 in UNOS Regions 1, 3, 4, 6, 7 and 10 (p-trend<0.05) and decreased in Regions 5, 8 and 9 (p-trend<0.05). Trends observed in Regions 2 and 11 were not statistically significant. As shown in Figure 1, UNOS Region 5 had the highest percentage of waitlist mortality and deterioration throughout the study period, while Region 6 had the lowest (p<0.001). A similar pattern was observed on examination of payer type distribution, with Region 5 having the highest percentage of Medicaid coverage and Region 6 having the lowest (p<0.001, Figure 2).
Figure 1.
Regional variations in delisting due to death or clinical deterioration during study period. P-trend<0.05 for all UNOS regions except Regions 2 and 11.
Figure 2.
Regional variations in Medicaid coverage (A) and delisting due to death or clinical deterioration (B). UNOS Region 5 had the highest percentage of both Medicaid coverage and patients delisted, while Region 6 had the lowest (p<0.001).
Cumulative incidence rates were calculated with LT considered a competing event. The cumulative incidence of waitlist mortality or deterioration at one year after listing was 9.0% (95% CI 8.3%-9.8%) for patients with private insurance, 10.7% (95% CI 9.9%-11.6%) for those with Medicare and 10.7% (95% CI 9.8%-11.6%) for Medicaid. At five years following listing, the cumulative incidence of death or deterioration was 13.7% (95% CI 12.7%-14.7%) for patients with private insurance, 16.2% (95% CI 14.9%-17.7%) for Medicare and 16.2% (95% CI 15.0%-17.4%) for Medicaid (private insurance vs Medicare: p<0.001; private insurance vs Medicaid: p<0.001) (Figure 3).
Figure 3.
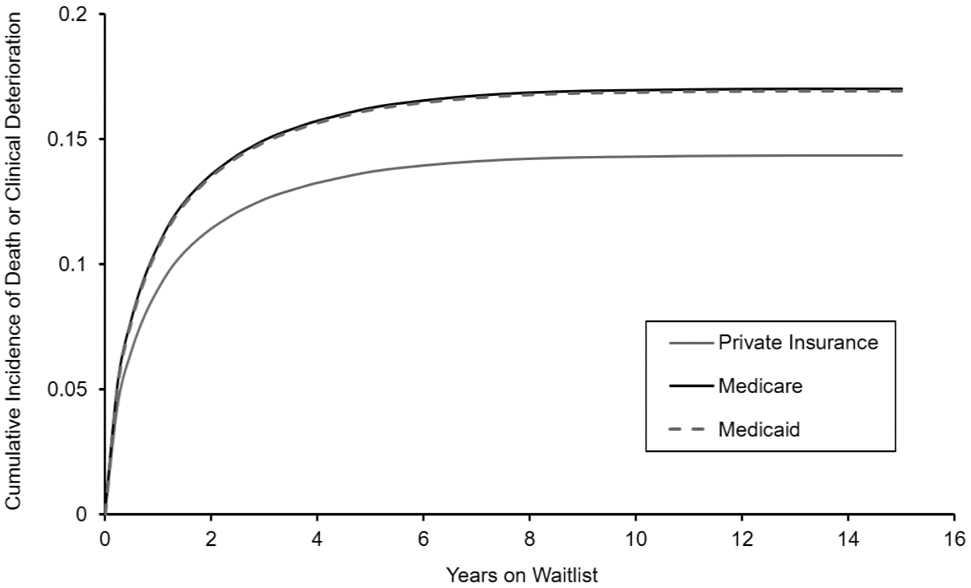
Cumulative incidence of delisting due to death or clinical deterioration stratified by insurance status, with liver transplantation considered a competing event. Patients with Medicare or Medicaid were delisted due to at a more rapid rate compared to those with private insurance. At every time point following listing, a higher incidence of delisting was observed among publicly insured patients.
On univariate competing risks regression, Medicare (Hazard Ratio [HR] 1.42, 95% CI 1.39-1.45) and Medicaid coverage (HR 1.27, 95% CI 1.24-1.31) were both associated with increasing hazard of death or clinical deterioration. Additional factors associated with delisting included increasing age (HR 1.02, 95% CI 1.02-1.02, p<0.001) and MELD score at listing (HR 1.02, 95% CI 1.02-1.02, p<0.001). Patients who were Black (HR 1.07, 95% CI 1.04+1.11, p<0.001) or Hispanic (HR 1.22, 95% CI 1.19-1.25, p<0.001) had increased hazard of death or deterioration compared to those who were White. Conversely, male sex (HR 0.85, 95% CI 0.83-0.86, p<0.001) and employment at listing (HR 0.61, 95% CI 0.59-0.63, p<0.001) were associated with decreased hazard of death or deterioration. Furthermore, hazard of delisting decreased with increasing education levels (Table 2).
Table 2.
Univariate analysis of delisting due to death or clinical deterioration
| Risk Factor | Hazard Ratio [95% CI] | p-value |
|---|---|---|
| Age, per year | 1.02 [1.02-1.02] | <0.001 |
| Male | 0.85 [0.83-0.86] | <0.001 |
| Race | ||
| White | Reference | |
| Black | 1.07 [1.04-1.11] | <0.001 |
| Hispanic | 1.22 [1.19-1.25] | <0.001 |
| Asian | 0.92 [0.87-0.97] | 0.001 |
| Other* | 1.12 [1.03-1.22] | 0.01 |
| Education level | ||
| Less than high school | Reference | |
| High school diploma/GED | 0.82 [0.78-0.85] | <0.001 |
| Attended college | 0.73 [0.70-0.76] | <0.001 |
| Associate's/Bachelor's degree | 0.66 [0.63-0.69] | <0.001 |
| Graduate degree | 0.62 [0.59-0.66] | <0.001 |
| Insurance type | ||
| Private | Reference | |
| Medicare | 1.42 [1.39-1.45] | <0.001 |
| Medicaid | 1.27 [1.24-1.31] | <0.001 |
| Employed at listing | 0.61 [0.59-0.63] | <0.001 |
| Dialysis twice in prior week at listing | 2.55 [2.45-2.65] | <0.001 |
| MELD score at listing, per point | 1.02 [1.02-1.02] | <0.001 |
| Liver disease etiology | ||
| Alcoholic liver disease | Reference | |
| Acute liver failure | 1.07 [1.01-1.13] | 0.017 |
| Cholestatic liver disease | 0.80 [0.77-0.84] | <0.001 |
| Hepatitis B | 0.83 [0.77-0.89] | <0.001 |
| Hepatitis C | 1.03 [1.00-1.06] | 0.03 |
| HCC | 0.75 [0.72-0.78] | <0.001 |
| NASH | 1.10 [1.06-1.15] | <0.001 |
| Other | 1.06 [1.03-1.09] | <0.001 |
| Encephalopathy | ||
| None | Reference | |
| Grade 1-2 | 1.27 [1.24-1.30] | <0.001 |
| Grade 3-4 | 1.85 [1.78-1.93] | <0.001 |
| Ascites | ||
| Absent | Reference | |
| Slight | 1.31 [1.28-1.35] | <0.001 |
| Moderate | 1.66 [1.61-1.70] | <0.001 |
| UNOS Region | ||
| Region 1 | Reference | |
| Region 2 | 0.87 [0.82-0.91] | <0.001 |
| Region 3 | 0.48 [0.46-0.51] | <0.001 |
| Region 4 | 0.85 [0.81-0.89] | <0.001 |
| Region 5 | 0.95 [0.91-1.00] | 0.04 |
| Region 6 | 0.67 [0.62-0.72] | <0.001 |
| Region 7 | 0.79 [0.75-0.84] | <0.001 |
| Region 8 | 0.72 [0.68-0.76] | <0.001 |
| Region 9 | 0.99 [0.94-1.05] | 0.81 |
| Region 10 | 0.63 [0.59-0.66] | <0.001 |
| Region 11 | 0.59 [0.56-0.62] | <0.001 |
Other race includes American Indian, Alaska Native, Native Hawaiian, Pacific Islander and multiracial. All continuous variables reported as median (IQR). All categorical variables reported as N (%). GED: general educational development; HCC: hepatocellular carcinoma
After adjusting for differences in available covariates, patients with Medicare (HR 1.20, 95% CI 1.17-1.24, p<0.001) and Medicaid (HR 1.20, 95% CI 1.16-1.24, p<0.001) remained at increased hazard of death or deterioration relative to those with private insurance. The presence of encephalopathy (HR 1.26, 95% CI 1.19-1.32, p<0.001), ascites (HR 1.25, 95% CI 1.20-1.31, p<0.001) or dialysis at listing (HR 2.22, 95% CI 2.10-2.34, p<0.001) were associated with increased death or deterioration. Compared to patients with alcoholic liver disease, those with cholestatic liver disease, hepatitis B and HCC were at a reduced hazard of delisting (Table 3).
Table 3.
Relevant factors associated with delisting due to death or clinical deterioration on adjusted analysis
| Risk Factor | Hazard Ratio [95% CI] | p-value |
|---|---|---|
| Age, per year | 1.02 [1.02-1.02] | <0.001 |
| Male | 0.86 [0.84-0.88] | <0.001 |
| Race | ||
| White | Reference | |
| Black | 1.06 [1.02-1.11] | 0.01 |
| Hispanic | 1.05 [1.02-1.09] | 0.01 |
| Asian | 0.93 [0.88-1.00] | 0.04 |
| Other* | 1.05 [0.95-1.15] | 0.37 |
| Education level | ||
| Less than high school | Reference | |
| High school diploma/GED | 0.98 [0.94-1.03] | 0.51 |
| Attended college | 0.94 [0.90-0.99] | 0.03 |
| Associate's/Bachelor's degree | 0.89 [0.84-0.94] | <0.001 |
| Graduate degree | 0.83 [0.77-0.88] | <0.001 |
| Insurance type | ||
| Private | Reference | |
| Medicare | 1.20 [1.17-1.24] | <0.001 |
| Medicaid | 1.20 [1.16-1.24] | <0.001 |
| Employed at listing | 0.81 [0.78-0.84] | <0.001 |
| Dialysis twice in prior week at listing | 2.22 [2.10-2.34] | <0.001 |
| MELD score at listing, per point | 0.99 [0.99-0.99] | <0.001 |
| Liver disease etiology | ||
| Alcoholic liver disease | Reference | |
| Acute liver failure | 0.98 [0.91-1.06] | 0.60 |
| Cholestatic liver disease | 0.86 [0.81-0.90] | <0.001 |
| Hepatitis B | 0.87 [0.78-0.95] | 0.004 |
| Hepatitis C | 0.97 [0.94-1.01] | 0.12 |
| HCC | 0.71 [0.68-0.75] | <0.001 |
| NASH | 1.02 [0.97-1.06] | 0.48 |
| Other | 1.04 [1.01-1.08] | 0.03 |
| Encephalopathy | ||
| None | Reference | |
| Grade 1-2 | 1.04 [1.02-1.07] | 0.003 |
| Grade 3-4 | 1.26 [1.19-1.32] | <0.001 |
| Ascites | ||
| Absent | Reference | |
| Slight | 1.19 [1.16-1.23] | <0.001 |
| Moderate | 1.25 [1.20-1.31] | <0.001 |
| UNOS Region | ||
| Region 1 | Reference | |
| Region 2 | 0.83 [0.78-0.88] | <0.001 |
| Region 3 | 0.39 [0.36-0.41] | <0.001 |
| Region 4 | 0.85 [0.80-0.90] | <0.001 |
| Region 5 | 0.92 [0.87-0.98] | 0.004 |
| Region 6 | 0.69 [0.63-0.76] | <0.001 |
| Region 7 | 0.77 [0.72-0.82] | <0.001 |
| Region 8 | 0.71 [0.67-0.76] | <0.001 |
| Region 9 | 0.99 [0.93-1.05] | 0.67 |
| Region 10 | 0.56 [0.53-0.60] | <0.001 |
| Region 11 | 0.51 [0.48-0.55] | <0.001 |
Other race includes American Indian, Alaska Native, Native Hawaiian, Pacific Islander and multiracial. All continuous variables reported as median (IQR). All categorical variables reported as N (%). GED: general educational development; HCC: hepatocellular carcinoma
Discussion
Despite the role of liver transplantation as the gold standard treatment for patients with end-stage liver disease and select unresectable HCC (1,6), disparities in both pre- and post-transplant outcomes persist. The current study is the first to examine the impact of payer status on delisting across disease etiologies at the national level. In this work, we found public insurance to be associated with increased likelihood of death or delisting due to deterioration among candidates listed for LT. These findings persisted both before and after risk adjustment where, specifically, LT candidates with Medicare or Medicaid had 20% increased adjusted hazard of death or delisting due to clinical deterioration compared to those with private insurance. In addition, patients with public insurance were delisted due to death or deterioration at a more rapid rate, and regional disparities in the hazard of delisting were noted.
Our study expands on previously reported data demonstrating unique challenges for publicly insured patients who are potential candidates for LT (6,7,15). A 2010 study of 144,507 patients hospitalized with liver-related disease showed that publicly insured patients had longer wait times and higher mortality prior to listing (7). Furthermore, a 2019 study including 705 HCC patients on the LT waitlist found that those who were publicly insured were nearly 70% more likely to drop out than those covered by Kaiser Permanente (6). The same study also found that publicly insured patients were more likely to drop out due to inadequate social support, non-adherence or loss to follow-up—highlighting the associations among socioeconomic factors, payer status and delisting (6). It is therefore plausible that these factors could partially explain the differences in waitlist outcomes observed in our largescale analysis.
Consistent with studies demonstrating the impact of socioeconomic burden on pre-transplant management and referral (8,16,17,18), we found that higher levels of education and employment were protective against waitlist mortality and deterioration. These findings may, in part, be explained by greater compliance with medical recommendations, access to care prior to LT or disease severity (6). Female sex was also associated with increased risk of delisting, which is consistent with previous findings demonstrating that women are less likely to get referred for LT and more likely to die on the waitlist than men (19). These sex-based disparities have been attributed to factors such as body size, as women are more likely to have an organ offer declined due to small stature (19). In addition, publicly insured patients were not only more likely to get delisted due to death or deterioration, but were also delisted at a faster rate at any given point in time. Although there are mixed findings regarding the impact of payer status on total waitlist time (6,20), our finding suggests that payer-based variations may exist in disease severity at listing as well as in clinical management while on the waitlist. Moreover, patients who were ultimately delisted spent more time on the waitlist. Mehta et al. (2018) similarly found UNOS regions with longer LT waitlist times to suffer from greater proportions of delisting. Patients in regions with long waitlist times were also more likely to receive grafts from older donors with a higher donor risk index, perhaps contributing to worse outcomes. These disparities are concerning particularly for patients with HCC, who are at greater risk of post-LT recurrence if waitlist time exceeds 18 months (21).
The ACA Medicaid expansion in 2014 reduced income eligibility requirements to 138% of the federal poverty level, paving the way for millions of new Medicaid beneficiaries and vastly improving access to transplantation among patients who were previously uninsured (20,22). Although 14 states have chosen not to adopt the expansion, a 2016 study including 169,194 transplant candidates found no significant difference in post-transplant mortality between states that adopted the expansion and those that did not (20). However, our study demonstrates that UNOS regions with the highest percentage of patients delisted also have the highest percentage covered by Medicaid. Furthermore, prior studies have reported regional variations in LT waitlist outcomes (23, 24). A study in 2007 found that among 2,948 patients listed for LT in UNOS Region 4, certain donation service areas had higher rates of delisting due to death or deterioration than others (23). Taken together, these findings highlight how geographic variations in organ availability and allocation can impact LT waitlist outcomes.
Organ transplantation is unique given the social, ethical and legal implications associated with allocating a lifesaving but limited pool of donor organs. Rooted in the National Organ Transplant Act of 1984, the current system for allocation was in part a response to the sale of organs, a practice which placed those with lower socioeconomic standing at a particular disadvantage (25,26). In mandating that organs be allocated “equitably”, it is conceivable that Congress implied that inequalities at any stage of the transplant process are not only unfair, but also controvert public policy. In the current era, the Medicaid expansion has improved access to transplantation (20,27) but concomitantly places an increased number of patients at risk of delisting and denial of a life-saving treatment. Our findings are important in identifying factors toward which attention can be directed to reduce delisting among the publicly insured. We additionally hope to draw the attention of policymakers who have the ability to reform current transplant allocation policy to match Congress’s initial intent.
Our study has several limitations, including its retrospective design and limitations inherent to large, national databases. The UNOS database is subject to missing data and variation in coding practices. It also does not specify a reason for waitlist removal beyond medical deterioration, which limits characterization of this cohort and prevents further analysis of the unique factors contributing to delisting. Although we examined the differences in baseline characteristics across payer types, we did not account for the wide heterogeneity in health services used among our privately insured cohort as this data is not available through UNOS (28). Because UNOS also does not track patients prior to listing, regional variations in Medicaid coverage noted in this study do not account for potential differences in LT referral patterns. Furthermore, data on insurance status at waitlist removal is only available for patients who were transplanted and not for those who were delisted due to death or deterioration, limiting our analysis to insurance status at listing. However, we found that approximately 19% of transplanted patients had a change in insurance status between listing and waitlist removal, indicating that the majority of our cohort retained the same payer type as what is coded in UNOS. Lastly, waitlisted candidates can enter a “Temporarily Inactive” status in which they are ineligible to receive a transplant due to disease progression or unresolved finances, among other reasons (29). In this study, periods of temporary waitlist inactivity were not included in the analysis of waitlist outcomes.
Given the evidence presented in this study and elsewhere, insurance status should be an important consideration when assessing risk of waitlist mortality and deterioration among LT candidates. Transplant programs should thus develop waitlist management protocols targeting publicly insured patients to lower the risk of delisting among this vulnerable population. Because patients with public insurance—particularly Medicaid— tend also to experience greater levels of socioeconomic burden, potential interventions may center on adherence and increased social support. These findings should gain the attention of policymakers at the local, regional and national levels in order to reduce existing disparities in organ allocation.
Funding/Financial Support:
NIH/NCATS/UCLA CTSI Grant UL1TR001881
Abbreviations:
- ACA
Affordable Care Act
- HCC
hepatocellular carcinoma
- LT
liver transplantation
- UNOS
United Network for Organ Sharing
Footnotes
Conflicts of Interest: None
References
- 1.Mustian MN, Shelton BA, Maclennan PA, Reed RD, White JA, Eckhoff DE, et al. Ethnic and age disparities in outcomes among liver transplant waitlist candidates. Transplantation. 2019. doi: 10.1097/TP.0000000000002523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim WR, Lake JR, Smith JM, Schladt DP, Skeans MA, Noreen SM, et al. OPTN/SRTR 2017 Annual Data Report: Liver. Am J Transplant. 2019;19:184–283. doi: 10.1111/ajt.15276 [DOI] [PubMed] [Google Scholar]
- 3.Bodzin AS, Baker TB. Liver Transplantation Today: Where We Are Now and Where We Are Going. Liver Transplant. 2018;24(10):1470–1475. doi: 10.1002/lt.25320 [DOI] [PubMed] [Google Scholar]
- 4.Fayek SA, Quintini C, Chavin KD, Marsh CL. The Current State of Liver Transplantation in the United States. Am J Transplant. 2016;16(11):3093–3104. doi: 10.1111/ajt.14017 [DOI] [PubMed] [Google Scholar]
- 5.Yu JC, Neugut AI, Wang S, Jacobson JS, Ferrante L, Khungar V, et al. Racial and insurance disparities in the receipt of transplant among patients with hepatocellular carcinoma. Cancer. 2010;116(7):1801–1809. doi: 10.1002/cncr.24936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gutin L, Yao F, Dodge JL, Grab J, Mehta N. Comparison of Liver Transplant Wait-List Outcomes Among Patients With Hepatocellular Carcinoma With Public vs Private Medical Insurance. JAMA Netw open. 2019. doi: 10.1001/jamanetworkopen.2019.10326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bryce CL, Chang C-CH, Angus DC, Arnold RM, Farrell M, Roberts MS. The Effect of Race, Sex, and Insurance Status on Time-to-Listing Decisions for Liver Transplantation. J Transplant. 2010. doi: 10.1155/2010/467976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wilder JM, Oloruntoba OO, Muir AJ, Moylan CA. Role of patient factors, preferences, and distrust in health care and access to liver transplantation and organ donation. Liver Transplant. 2016;22(7):895–905. doi: 10.1002/lt.24452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cholankeril G, Gonzalez HC, Satapathy SK, Gonzalez SA, Hu M, Khan MA, et al. Increased Waitlist Mortality and Lower Rate for Liver Transplantation in Hispanic Patients With Primary Biliary Cholangitis. Clin Gastroenterol Hepatol. 2018. doi: 10.1016/j.cgh.2017.12.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peters NA, Javed AA, He J, Wolfgang CL, Weiss MJ. Association of socioeconomics, surgical therapy, and survival of early stage hepatocellular carcinoma. J Surg Res. 2017. doi: 10.1016/j.jss.2016.11.042 [DOI] [PubMed] [Google Scholar]
- 11.Tumin D, Beal EW, Mumtaz K, Hayes D Jr, Tobias JD, Pawlik TM, et al. Medicaid Participation among Liver Transplant Candidates after the Affordable Care Act Medicaid Expansion. J Am Coll Surg. 2017. doi: 10.1016/j.jamcollsurg.2017.05.004 [DOI] [PubMed] [Google Scholar]
- 12.Oliveira GH, Al-Kindi SG, Simon DI. Implementation of the Affordable Care Act and solid-organ transplantation listings in the United States. JAMA Cardiol. 2016;1(6):737–738. doi: 10.1001/jamacardio.2016.2067 [DOI] [PubMed] [Google Scholar]
- 13.Roberts MS, Angus DC, Bryce CL, Valenta Z, Weissfeld L. Survival after liver transplantation in the United States: A disease-specific analysis of the UNOS database. Liver Transplant. 2004;10(7):886–897. doi: 10.1002/lt.20137 [DOI] [PubMed] [Google Scholar]
- 14.Parrish NF, Feurer ID, Matsuoka LK, Rega SA, Perri R, Alexopoulos SP. The Changing Face of Liver Transplantation in the United States: The Effect of HCV Antiviral Eras on Transplantation Trends and Outcomes. Transplant Direct. 2019;5(3). doi: 10.1097/TXD.0000000000000866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Robinson A, Hirode G, Wong RJ. Ethnicity and Insurance-Specific Disparities in MELD Score at Time of Liver Transplant Waitlist Registration and Its Impact on Mortality. J Clin Exp Hepatol. August 2020. doi: 10.1016/j.jceh.2020.07.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee BP, Vittinghoff E, Pletcher MJ, Dodge JL, Terrault NA. Medicaid Policy and Liver Transplant for Alcohol-Associated Liver Disease. Hepatology. May 2020:hep.31027. doi: 10.1002/hep.31027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ebel NH, Hsu EK, Berry K, Horslen SP, Ioannou GN. Disparities in Waitlist and Posttransplantation Outcomes in Liver Transplant Registrants and Recipients Aged 18 to 24 Years: Analysis of the UNOS Database. Transplantation. 2017;101(7):1616–1627. doi: 10.1097/TP.0000000000001689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mathur AK, Schaubel DE, Gong Q, Guidinger MK, Merion RM. Racial and ethnic disparities in access to liver transplantation. Liver Transplant. 2010;16(9):1033–1040. doi: 10.1002/lt.22108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Verna EC, Lai JC. Time for Action to Address the Persistent Sex-Based Disparity in Liver Transplant Access. JAMA Surg. 2020;155(7):545–547. doi: 10.1001/jamasurg.2020.1126 [DOI] [PubMed] [Google Scholar]
- 20.DuBay DA, MacLennan PA, Reed RD, Shelton BA, Redden DT, Fouad M, et al. Insurance Type and Solid Organ Transplantation Outcomes: A Historical Perspective on How Medicaid Expansion Might Impact Transplantation Outcomes. J Am Coll Surg. 2016;223(4):611–620.e4. doi: 10.1016/j.jamcollsurg.2016.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mehta N, Dodge JL, Hirose R, Roberts JP, Yao FY. Increasing Liver Transplantation Wait-List Dropout for Hepatocellular Carcinoma with Widening Geographical Disparities: Implications for Organ Allocation. Liver Transplant. 2018;24(10):1346–1356. doi: 10.1002/lt.25317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kaiser Family Foundation. The Effects of Medicaid Expansion under the ACA: Updated Findings from a Literature Review. https://www.kff.org/report-section/the-effects-of-medicaid-expansion-under-the-aca-updated-findings-from-a-literature-review-report. Accessed September 2020.
- 23.Barshes NR, Becker NS, Washburn WK, Halff GA, Alola TA, Goss JA. Geographic disparities in deceased donor liver transplantation within a single UNOS region. Liver Transplant. 2007;13(5):747–751. doi: 10.1002/lt.21158 [DOI] [PubMed] [Google Scholar]
- 24.Hart A, Schladt DP, Zeglin J, Pyke J, Kim WR, Lake JR, et al. Predicting Outcomes on the Liver Transplant Waiting List in the United States: Accounting for Large Regional Variation in Organ Availability and Priority Allocation Points. Transplantation. 2016. doi: 10.1097/TP.0000000000001384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Francis DL, Robert A, Nancy S-H, Laura SA, Jeffrey K, Stuart YJ. The New Eng Land Jour Nal of Medicine Sounding Board ETHICAL INCENTIVES-NOT PAYMENT-FOR ORGAN DONATION; 2002. www.nejm.org. Accessed August 21, 2020. [Google Scholar]
- 26.Robertson JA. Paid Organ Donations and the Constitutionality of the National Organ Transplant Act. Hastings Constit Law Q. 2012;40. https://heinonline.org/HOL/Page?handle=hein.journals/hascq40&id=245&div=11&collection=journals. Accessed August 2020. [Google Scholar]
- 27.Guth M, Garfield R, Rudowitz R. The Effects of Medicaid Expansion under the ACA: Updated Findings from a Literature Review; 2020. [Google Scholar]
- 28.Andersen R, Newman JF. Societal and individual determinants of medical care utilization in the United States. Milbank Q. 2005;83(4). doi: 10.1111/j.1468-0009.2005.00428.x [DOI] [PubMed] [Google Scholar]
- 29.Hansen L, Yan Y, Rosenkranz SJ. The power of the liver transplant waiting list: A case presentation. Am J Crit Care. 2014;23(6):510–515. doi: 10.4037/ajcc2014399 [DOI] [PMC free article] [PubMed] [Google Scholar]