Abstract
Objective:
To explore how non-research funded rehabilitation practitioners implemented dynamic Lycra® orthoses for arm recovery after stroke into rehabilitation practice, as part of a feasibility randomised controlled trial.
Design:
Qualitative interview study.
Setting:
Two in-patient stroke units and associated rehabilitation units.
Subjects:
Fifteen purposefully selected stroke rehabilitation practitioners involved in delivery of dynamic Lycra® orthoses as part of a feasibility randomised controlled trial.
Methods:
Semi-structured interviews conducted at the end of the trial. Interviews examined their experiences of orthosis implementation. Normalisation Process Theory structured the interview guide and informed data analysis. NVivo software supported data analysis.
Results:
Practitioners intuitively made sense of the intervention in the face of uncertainty about its precise mechanisms of action (Normalisation Process Theory construct: coherence) and espoused commitment to the research, despite uncertainty about orthosis effectiveness (cognitive participation). They did however adapt the intervention based on perceived therapeutic need, their own skillsets and stroke survivor preference (collective action). They were uncertain about benefits (reflexive monitoring). Across the 4 theoretical constructs, ambivalence about the intervention was detected.
Conclusions:
Ambivalence interfered with implementation – but only to an extent. ‘Good-enough’ coherence, cognitive participation, collective action and reflexive monitoring were sufficient to initiate normalisation – as long as implementation did not undermine the relationship between practitioner and stroke survivor. Ambivalence stemmed from practitioners’ uncertainty about the intervention theory and mechanisms of action. Making intervention mechanisms of action more explicit to practitioners may influence how they implement and adapt a research intervention, and may determine whether those processes undermine or enhance outcomes.
Keywords: Orthotic devices, stroke, upper extremity, rehabilitation
Introduction
Translating research into clinical practice is an unpredictable, slow process 1 : evidence of a 17-year gap between the production of research evidence and its implementation in practice is frequently quoted. 2 Establishing the clinical effectiveness of a therapeutic intervention in a randomised controlled trial does not guarantee its adoption into practice. Without clinical implementation, research evidence cannot lead to improved therapeutic outcomes. The last 2 decades has seen the emergence of implementation science, a new field of applied research to address this research-implementation gap. 1 Consequently, the Medical Research Council has highlighted the need to consider implementation processes alongside evaluation of intervention effectiveness, 3 advocating the use of process evaluations alongside randomised controlled trials to develop interventions that are not only effective but can also be adopted in routine clinical practice. 4
Rehabilitation research presents challenges which further strengthen the rationale for exploring implementation processes alongside intervention effectiveness, because it requires personalised treatment which makes fidelity to treatment protocols more difficult. 5 Rehabilitation tends to be delivered face-to-face and is influenced by relationships and aspects of human behaviour, and in thus seen as highly complex, with many interacting elements. 5 Exploring and understanding this complexity and its implications for the feasibility of routine adoption of treatments in national and internation practice contexts is therefore vital when developing and testing new rehabilitation interventions within clinical trials.
This paper reports on the implementation processes within a feasibility randomised controlled trial 6 that was examining use of dynamic Lycra® orthoses as an adjunct to arm rehabilitation after stroke. Dynamic Lycra® orthoses are made-to-measure, internationally commercially available garments, which use the tensile properties of Lycra® to generate torsion to correct imbalances in muscle forces around joints (Figure 1). Theoretically these orthoses are proposed to stretch shortened muscles, improve functional positioning, dampen involuntary movement and enhance proprioception and limb awareness. 7 The orthoses may act as dynamic splints, optimising motor conditions for task practice and potentially practice effects. Despite their widespread commercial availability, international evidence for the effectiveness of the orthoses in improving impairment after stroke was limited to small non-randomised and single case studies conducted in the UK and USA.7,8
Figure 1.

Example of dynamic Lycra® orthosis used in study.
We therefore sought to examine how orthosis wear was implemented in the feasibility randomised controlled trial, from the perspective of (non-research funded) rehabilitation therapists and nurses who were supporting trial delivery. Despite their international commercial availability, understanding how implementation of the orthoses did (or did not) become routinely embedded in typical rehabilitation practice, had not previously been explored, and could help identify emerging implementation problems and inform future dynamic Lycra® orthosis trials. Furthermore, once orthosis effects were established, this knowledge could inform introduction of dynamic Lycra® orthoses in clinical practice as a routine adjunct to rehabilitation.
The primary aim of the main study was to establish the feasibility and acceptability of undertaking an effectiveness trial and obtain an indication of magnitude and direction of change in impairment and activity limitation. 6 Evaluation of how orthosis wear was implemented during the trial by (non-research funded) practitioners within rehabilitation, which we report here, was a secondary aim of the study. Our research question was: What are the perceptions of healthcare practitioners, working in in-patient stroke rehabilitation, of the implementation of dynamic Lycra® orthoses into their practice within the context of a feasibility randomised controlled trial?
Methods
Design
This was a qualitative study using in-depth interviews with healthcare professionals involved in the implementation of dynamic Lycra® orthoses during the feasibility randomised controlled trial. This design was selected because it enables detailed examination of perceptions about implementation and offers opportunity to explore and construct meaning relevant to implementation. The East of Scotland Research Ethics Committee provided ethical approval (15/ES/0093).
Study context, sampling and recruitment
Stroke survivors (n = 43) admitted to 2 acute stroke units and their associated rehabilitation hospitals in Scotland were screened and recruited as study participants 2 to 4 weeks post stroke, if they had persistent arm impairment, were able to provide informed consent and could participate in rehabilitation. To capture implementation issues from different contexts, making findings broadly relevant to national and international contexts, the settings to which patients were subsequently admitted from the acute stroke units differed in key characteristics. One was a mixed acute and rehabilitation stroke unit, in which local patients remained until discharge, and others moved through quickly to general community rehabilitation hospitals distant from the acute setting. The other was an acute stroke unit from which patients moved rapidly to specialist brain injury rehabilitation if they were under 65 years; to elderly rehabilitation if older, or to a specialised stroke rehabilitation unit, in which patinets remained until discharge. Participants were randomised in a 2:1 ratio to receive a made-to-measure dynamic Lycra® orthosis plus usual care (n = 27) or usual care only (n = 16). Orthoses were to be worn for 8 h daily over 8 weeks. Outcome assessment (impairment and activity limitation) took place at 8 and 16 weeks. Full trial details and results are published elsewhere. 6
Occupational therapy, physiotherapy and nursing staff on the rehabilitation units and within community hospital rehabilitation teams were trained by researchers, and were responsible for implementing the orthoses with study participants. Their duties involved identifying potential participants, informing them about the study, supporting study participants to don and doff the orthoses, ensuring appropriate duration of wear, recording daily wear and rehabilitation activities, washing of the orthoses to manufacturer instructions and reporting adverse reactions to researchers.
At the end of the study, a sample of these practitioners was purposefully recruited, by profession and by rehabilitation unit or community-based team. We purposefully sampled participants from a range professional backgrounds to ensure that we captured broad variations in settings and experience across the sample. Different professionals, physiotherapists, nurses, occupational therapists and support workers have different roles in rehabilitation, and their perceptions of the role of DLO in the rehabilitation process, and their experiences of implementing it will vary according their roles. Similarly, we purposefully recruited participants from across the different rehabilitation settings participating in the trial, because the organisational processes, and therefore implementation strategies and experiences of implementation were likely to vary, providing us with rich data from across the study settings. Potential participants from within the participating units, and who had been involved in delivering the study intervention were approached by the study researcher after the last stroke survivor had completed orthosis wear on the basis of their profession, and were provided with an information sheet and invited to indicate interest in participation. Those expressing interest were given the opportunity to discuss the study with the study researcher before providing written consent for participation. The researcher then contacted them to arrange an interview.
Data collection
Semi-structured interviews took place in participants’ workplaces and were conducted by a study researcher (AJ), a female academic speech and language therapist with 25 years of qualitative research experience in communication research in disabled populations and people with aphasia. Analysis was conducted by AJ, JD and JM. JD was a female physiotherapist and qualitative social researcher with 12 years of qualitative research experience. JM is a female academic physiotherapy researcher with 18 years’ experience of rehabilitation research in stroke and has expertise in qualitative and mixed methods research and implementation research. Interviews lasted approximately 45 min and were audio-recorded and transcribed verbatim.
Theoretical framework: Normalisation Process Theory
The topic guide (Table 1) was informed by Normalisation Process Theory. 9 Normalisation Process Theory is a sociological theory which explains the processes people adopt when implementing new interventions, to allow the intervention to become ‘normalised’ or embedded in routine practice. 9 Four core constructs describe generative mechanisms that facilitate normalisation: coherence (work to make sense of an intervention), cognitive participation (work to engage with an intervention), collective action (work to enable an intervention to happen) and reflexive monitoring (work to appraise an intervention). 10 The core constructs each have 4 key sub-constructs (Table 2). Normalisation Process Theory has been widely used in intervention studies, including in stroke rehabilitation, 11 and has been endorsed as explanatory theoretical framework.11,12
Table 1.
Topic guide details.
| Theoretical construct | Sample questions |
|---|---|
| Coherence | • What was your initial opinion of the study? • How do you think the study was valued by the team? • What do you think about using the orthosis as part of arm rehabilitation in stroke survivors? Describe in what ways you think the intervention might be beneficial? |
| Cognitive participation | • What helped or hindered the process of making sure procedures were undertaken? • Were there issues with co-ordinating or undertaking any particular procedures? For example, therapy diaries? • How well did the team co-ordination work over time? |
| Collective action | • Can you describe exactly what people did to ensure study procedures were carried out? • How well were the procedures enacted? What helped or hindered the procedures? • Were there specific issues or concerns? How could these be addressed in future? |
| Reflexive monitoring | • Can you give me your thoughts about the support provided by the researchers during the study? • How did the information gathering work? Were there difficulties? • How do you think the intervention was viewed by participants? • How useful was it considered to be by participants? In what ways? • Were there adverse responses? • How useful was the orthosis thought to be in assisting the achievement of rehabilitation goals? • Did you observe changes in arm movement, use or positioning in participants when participants were wearing the orthosis? • Did participants report change in sensation or awareness of the limb when wearing the orthosis? |
Table 2.
Normalisation process theory constructs as applied in the study.
| Coherence | Differentiation | Do practitioners seek to understand how orthosis wear differs from their usual arm rehabilitation practice? |
|---|---|---|
| Communal specification | Do practitioners seek to develop a shared understanding of the aims and objectives of orthosis wear? | |
| Individual specification | Do practitioners seek to understand their own tasks and responsibilities relating to orthosis wear? | |
| Internalisation | Do practitioners seek to understand the value, benefits and importance of orthosis wear? | |
| Cognitive participation | Initiation | Are practitioners working to drive orthosis wear forward? |
| Enrolment | Are practitioners buying in to orthosis wear and (re-)organising themselves to collectively contribute to implementing orthosis wear? | |
| Legitimation | Are practitioners working to ensure that others believe it is right for them to be involved in implementing orthosis wear? | |
| Activation | Have practitioners established the necessary actions and procedures to maintain their involvement and sustain implementation of orthosis wear? | |
| Collective action | Interactional workability | How do practitioners interact with each other, the orthosis itself and the different procedures relating to orthosis wear (eg, donning and doffing) while using the orthoses in clinical practice? |
| Relational integration | How do practitioners ensure that orthosis implementation does not undermine their relationship with each other and with stroke survivors? | |
| Skillset workability | How do practitioners allocate tasks – who does what when implementing orthosis wear? | |
| Contextual integration | How do practitioners take into account the availability of resources (including time) and the wider clinical context when implementing orthosis wear? | |
| Reflexive monitoring | Systemisation | Do practitioners collect information to determine how effective and useful orthosis wear is? |
| Communal appraisal | Do practitioners work together to evaluate orthosis wear? | |
| Individual appraisal | Do practitioners individually evaluate the effect of orthosis wear on them? | |
| Reconfiguration | Do practitioners attempt to redefine or modify the implementation of orthosis wear? |
Data analysis
Interview transcripts were imported into NVivo software (version 11). Data was analysed using the Framework Approach. 13 Following an initial stage of data familiarisation, the data was analysed through an iterative process of coding. Three researchers read the transcripts in full to familiarise themselves with the interviews. Subsequently, 2 parallel coding processes took place. Two researchers individually open-coded 4 transcripts before coming together to agree and define the coding framework. The framework was applied to subsequent interviews and codes refined and added. In a second stage, the 2 researchers met again to examine how the codes obtained through open-coding fitted with Normalisation Process Theory core concepts. The third researcher directly coded the transcripts to the 16 sub-constructs of Normalisation Process Theory. The results of the 2 coding processes were compared, differences were discussed in detail and final Normalisation Process Theory codes were assigned to all interview excerpts based on a consensus process. The final stage was a series of meetings between the researchers to generate and agree relevant themes that explained the implementation process.
Findings
Participants
Fifteen practitioners were interviewed (Table 3): 7 occupational therapists, 1 occupational therapy assistant, 4 physiotherapists and 3 nurses, working in stroke rehabilitation units (8 individuals), brain injury units (3), community-based settings (2) and acute stroke units (1). One individual worked across different settings.
Table 3.
Participant characteristics.
| Profession | Location | |
|---|---|---|
| 1 | OT | Brain injury unit |
| 2 | OT | Acute stroke unit |
| 3 | OT | Stroke rehab unit |
| 4 | OT | Stroke rehab unit |
| 5 | OT | Stroke rehab unit |
| 6 | OT | Community rehab |
| 7 | OT | Community rehab |
| 8 | OT Assistant | Stroke rehab unit |
| 9 | Physiotherapist | Stroke rehab unit |
| 10 | Physiotherapist | Brain injury unit |
| 11 | Physiotherapist | Brain injury unit |
| 12 | Physiotherapist | Acute stroke unit and community rehab |
| 13 | Staff Nurse | Stroke rehab unit |
| 14 | Staff Nurse | Stroke rehab unit |
| 15 | Staff Nurse | Stroke rehab unit |
Findings
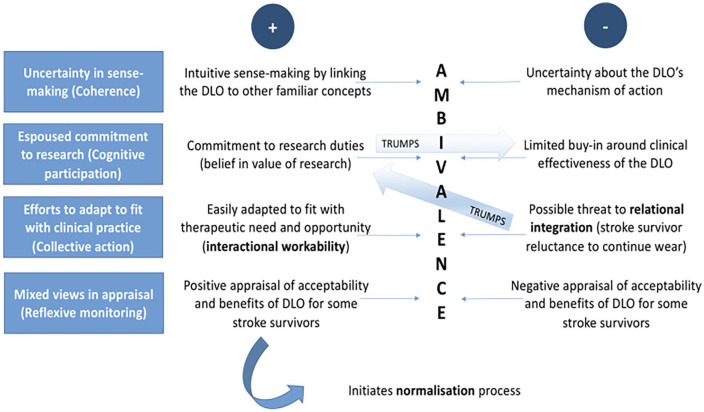
Four main themes each linked with a core Normalisation Process Theory construct (in parenthesis), were generated: (i) uncertainty in sense-making (coherence), (ii) espoused commitment to research (cognitive participation), (iii) efforts to adapt the intervention to fit with practice (collective action) and (iv) mixed views in appraisal (reflexive monitoring). Across the 4 constructs, ambivalence about orthosis wear was detected. We address the 4 themes in turn, with sub-themes in italics. Where appropriate, explanatory Normalisation Process Theory sub-constructs (defined in Table 2) have been added (in italics within parenthesis). Figure 2 summarises our analysis, describing the relationship between the themes and Normalisation Process Theory constructs. We will refer to Figure 2 throughout the next section.
Figure 2.
Normalisation Process Theory analysis of study findings – summary.
Coherence: Uncertainty in Sense-making
Coherence refers to the sense-making work people do to understand an intervention. Making sense of the orthoses required practitioners from all professions to grapple with degrees of uncertainty about the purpose of the orthoses in rehabilitation. Faced with uncertainty, participants sought to intuitively make sense of the orthoses, by speculating about potential mechanisms of action and by linking it to familiar concepts.
Degrees of uncertainty
Practitioners easily made sense of the purpose of the trial – all were able to describe, at least partially, the aims of the trial (communal specification). However, despite formal presentation to introduce the trial and explanations delivered by the researchers, detailed understanding of the orthoses was lacking.
To be honest, I didn’t have a huge understanding of them prior to this study. I’d even say just now my understanding probably of everything behind them is probably still quite limited. (OT1)
Potential mechanisms of action
Some practitioners speculated on potential neural mechanisms through which the garment might work; others had no understanding.
I remember having it explained to me at the time but, I can’t, for the life of me remember at the moment. (SN2)
Views on the rationale for orthosis use varied, ranging from prevention of neglect and support for oedema control to support for neural pathway recovery through sensory stimulation and arm alignment.
My understanding of it is for a dense weakness that the Lycra® sleeve is made in such a way that it might help with any neglect that the person has got with their arm. (SN1)
It can work with patients that have got spasticity or an increased tone in helping to stretch the joints, the muscles out. (PT3)
Linking to familiar concepts
Practitioners also employed an intuitive sense-making process, linking the orthosis to other familiar concepts. They compared donning the orthosis to helping stroke survivors with splints or items of clothing.
As OTs we would look at things like self-caring: you are trying to put on a bra, a T-shirt and now they have got something else that they need to put on. (OT3)
The overall impression (Figure 2) was one of uncertainty in sense-making: coherence was facilitated by intuitively linking the orthosis to familiar concepts, but hindered by uncertainty about its mechanism of action, resulting in ambivalence.
Cognitive Participation: Espoused Commitment to Research
Cognitive participation relates to people committing to implementing the intervention. Two sub-themes explaining ambivalence were identified. First, there was a tension between practitioners’ espoused and practised commitment to the research. Second, espoused commitment to the research was present despite lack of buy-in around the orthoses’ effectiveness.
Espoused versus practised commitment to research
Practitioners considered it a legitimate part of their role to be involved in the research (enrolment, legitimation).
It is quite exciting to be involved in a study if it then goes onto show that it is, you know, something that could benefit a lot of people in the future. (OT3)
Despite believing that involvement in the study was worthwhile, practitioners acknowledged that their participation in research processes faltered over time. Small numbers of participants were coming through at any given time, which meant the research was not always a priority.
I think with documentation, I think – hands up – I think we started off well with that, doing the task form, but I think that fell by the wayside as time went on. . . As I say because it is not a number one priority unfortunately. You know, during the day, other things creep up. (PT1)
The people driving forward the study were not the participating practitioners (initiation). Instead, researchers or participating stroke survivors reminded practitioners about what needed to be done. Practitioners who missed the initial researcher-led information meetings learnt about the project by observing orthosis-related activity. Community therapists were often not informed by their hospital-based colleagues, but sometimes learnt about the study from a stroke survivor.
There was no information, so it wasn’t until I got out to her setting and saw the garment on and then knew what it was. There wasn’t any handover from the therapist. (PT3)
Limited buy-in around the effectiveness of the orthoses
Practitioners approached the orthoses with open mind, but modest expectations. The value of the orthoses was described in terms of possibilities rather than firm conviction of clinical effectiveness. This led to ambivalence about its likely effects and reluctance to promote orthosis wear beyond the research context until more evidence emerged to support its use.
I think until there is much more evidence there we couldn’t really, as physios, be promoting that with them. (PT2)
Practitioners did not however see the uncertain clinical effectiveness of the orthoses as ground for discontinuing orthosis wear during the trial. Views on clinical effectiveness, normally a core component in clinical decision-making, did not feature in practitioners’ decision-making. Practitioners remained committed to implementation: they acknowledged the value of the research and were willing to suspend their evaluation of the clinical effectiveness of the orthosis for the trial’s duration.
Everything has to be studied, everything has to be investigated and tried and trialled and to have new things coming out, everything has to be tested. (SN2)
Figure 2 summarises these findings: cognitive participation was facilitated by practitioners’ beliefs in the value of the research but hindered by their uncertainty around the clinical effectiveness of the orthosis. This resulted in ambivalence but their belief in the research’s value took priority.
Collective Action: Efforts to Adapt to Fit with Practice
Collective action refers to the effort invested in implementing the intervention. Practitioners adapted orthosis wear to fit with practice. They were active agents in the decision-making on when to temporarily remove or discontinue orthosis wear. Decisions were made because of therapeutic need and opportunity, stroke survivor preference and safety issues. Practitioner skills influenced their involvement.
Therapeutic need and opportunity
Orthosis use fitted easily into the therapeutic interactions between stroke survivor and practitioner (interactional workability). During rehabilitation sessions, orthosis wear was stopped and restarted as dictated by therapeutic need. Movement facilitation physically supported by therapists and sensory re-education work were sometimes triggers for removing the orthosis, as were activities requiring forearm pronation (eg, holding a walking stick). The orthosis was removed if there was a risk of stains (eg, cooking practice). Donning the orthosis was used to add value to rehabilitation: the orthosis was sometimes used as an additional component during dressing practice and as a mechanism for directing attention towards the arm at the start of upper limb work.
Apart from when I was doing the sensory stimulation because obviously that was on the palm so that would’ve impeded it, so we took it off for that. (OT8)
Stroke survivor preferences
Orthosis wear was mostly compatible with maintaining a good stroke survivor-practitioner relationship (relational integration) – which mattered to practitioners. Stroke survivor preference was the main factor in the decision-making around discontinuing orthosis wear. Stroke survivor reluctance to wear the sleeve did not lead to practitioners encouraging continued use – irrespective of the reasons for this reluctance, be it discomfort, perceived ineffectiveness or aesthetic considerations. Practitioners allowed perceptions of stroke survivor preferences to take priority over, or trump, their sense of responsibility towards their research duties.
I think he was taking it off a lot more towards the end of his stay here. I didn’t notice any particular patterns. I think the pattern came really with the length of stay. He would have it on a lot more at the start and then he, he tailored it off himself. (PT4)
Practitioner skills
Orthosis-related tasks were performed by different professions in different settings, but occupational therapists, physiotherapists and nurses were all involved in recruiting participants, completing research paperwork, donning, doffing and laundering the orthoses and checking for adverse events (skillset workability). Donning the garment was initially challenging for some but became second-nature with practice. Lack of practice resulted in de-skilling. Practitioners taught each other but some waited until a colleague with more experience of donning the garment came on shift.
The very, very first time I put the first one on I was absolutely sweating buckets, because it seemed horrendous at the time . . . the more we did it the better it got, definitely. (OT4)
Figure 2 summarises these findings: collective action was supported by the easy adaptability of the orthoses to fit the therapeutic context but undermined by a possible threat to relational integration (ie, the stroke survivor-practitioner relationship), resulting in ambivalence. Relational integration took priority over (trumped) the adaptability of the orthoses to therapeutic need and participants’ sense of their research duties.
Reflexive Monitoring: Mixed Views in Appraisal
Reflexive monitoring refers to appraisal activities, assessing the value of the intervention. There was evidence of practitioners and stroke survivor ambivalence in the face of uncertain benefits and adverse effects.
Uncertain benefits and adverse effects
Practitioners consistently noted better arm alignment and increased stroke survivor awareness of the arm (communal appraisal), however views about impacts on muscle tone or sensation were mixed. Practitioners did not notice improvements to active movement or strength.
I would definitely say that putting the gauntlet or the glove on did improve patients’ positioning of their arm; [the] hand was in a better position for using it in functional tasks. I don’t think I could say that I saw any improved motor functioning. (OT3)
Views on the acceptability of the orthosis were similarly mixed: practitioners reported that most stroke survivors accepted the orthosis, but some disliked it. The main adverse effects were tightness, swelling and skin markings.
She found things like where the seams were sitting were very uncomfortable for her, so much so, that if it hadn’t managed to be corrected she said she wouldn’t continue wearing the garment. (PT2)
As Figure 2 shows, mixed views in appraisal resulted in ambivalence in reflexive monitoring, with positive appraisal of the acceptability and benefits of the orthoses for some, but not other stroke survivors.
Discussion
To our knowledge, this is one of the first studies to investigate how stroke rehabilitation professionals understand and implement experimental interventions about which effectiveness is uncertain. Implementation of orthosis use in our study occurred against a backdrop of ambivalence: easy intuitive sense-making, strong belief in the value of the research and the adaptability of the orthosis to fit with practice were in evidence alongside uncertainty about the mechanisms of action and effectiveness of the orthosis, and reluctance to undermine the stroke survivor-practitioner interaction (Figure 2). This ambivalence mirrors the uncertainty in the literature about orthosis use. A single case study 8 and crossover trial 7 showed improved outcomes but, prior to our feasibility study, 6 no randomised controlled trial evidence on the effectiveness of dynamic Lycra® orthoses was available.
Ambivalence interfered with the process of implementation – but only to an extent. Intuitive sense-making, espoused commitment to the research, the easy therapeutic adaptability of the orthosis and partially positive views on acceptability were sufficient to facilitate implementation. ‘Good-enough’ coherence, cognitive participation, collective action and reflexive monitoring acted as the generative mechanisms described within Normalisation Process Theory, kick-starting the normalisation process. Researchers investigating a triaging tool for individuals with low back pain similarly found that poor coherence did not stop the tool from being used by (some) GPs 14 – temporarily. As in our study, the research context generated a willingness to temporarily suspend apprehension about the tool among GPs. Researchers elsewhere have described barriers to implementation where interventions do not match the beliefs of practitioners, leading to what they have termed ‘patchy’ coherence. 15 Patchy coherence was apparent in our study where practitioners believed in research, but not entirely in the intervention. It explains their willingness to adopt the intervention, but then adapt or stop the intervention as they saw fit.
Stroke survivor acceptance and preference emerged as the core value guiding practitioners’ decision-making around orthosis wear. An implementation study of robotic therapy as adjunct to upper limb stroke rehabilitation similarly identified acceptance by stroke survivors as vital to practitioner perspectives about the intervention. 16 Congruently, the theoretical construct of relational integration emerged as central to the normalisation narrative in our study: ‘good enough’ coherence, cognitive participation, collective action and reflexive monitoring supported implementation, but only as long as the stroke survivor-practitioner relationship was not threatened. Stroke survivor reluctance to wear the orthosis trumped any sense of research duties. Holtrop 17 similarly postulated the importance of relational integration in her implementation study of a chronic condition care management approach, identifying relational integration as obligatory point of passage through which other Normalisation Process Theory constructs operate. 11
In our study, practitioners adapted orthosis wear to fit with practice, which reflects findings from other rehabilitation studies. For example, physiotherapists implementing an evidence-based arm rehabilitation exercise programme adapted the programme to fit with concerns about how the exercises were performed. 18 Flexibility to adapt research-based interventions to the unique context of the individual practitioner-patient interaction may be a precondition for successful implementation: Connell 19 has argued that giving practitioners the autonomy to adapt interventions increases their motivation to implement the intervention. However, adapting protocols in a trial context (as in our study) may be more problematic than implementing an intervention that has already been tested for effectiveness (as in Connell’s study). That practitioners did so in the present study, possibly reflects a need for more training to enhance their understanding of research methods. It is more likely, however, that they simply adapted the intervention to meet the perceived needs of their patients. These adaptations may partly explain findings of the feasibility trial, which indeed showed no indications of benefits of dynamic Lycra® orthoses on arm recovery in this population. 6
Any intervention adaptations need to be considered against the backdrop of “the fidelity and adaptation debate” 4 (p.39). This debate calls for a distinction between ‘innovation’, whereby skilled implementers adapt an intervention to better fit the context, and ‘drift’, whereby adaptations could potentially undermine an intervention’s effectiveness. A third category, ‘subversion’ occurs when practitioners consciously decide not to implement elements of the intervention because these elements go against their values. Whether an adaptation represents innovation or drift depends on the intervention theory and on how the active ingredients of the intervention interact to produce change.
A challenge for our study, reflected in practitioners’ perspectives and responses to implementation, is that there is not yet any detailed intervention theory around how dynamic Lycra® orthoses could lead to motor function improvements, and with whom. Hypothetically, the orthoses may provide enhanced multi-sensory input through compression, muscle stretch and joint positioning, leading to improved function, however this proposition has not been fully explored. 7 Furthermore, it is unclear whether a sub-group of stroke survivors, with less (or more) severe upper limb disability, might respond better to orthosis wear. Our feasibility trial requirements were that participants had persistent arm impairment. 6 We adopted this broad approach as appropriate for a first-ever, exploratory randomised controlled trial and intended to evaluate the effects on sub-groups related to impairment severity. Because of attrition, sub-groups were however too small for meaningful conclusions. 6
It is similarly unclear whether responses to orthosis wear might vary depending on when the orthosis is worn (eg, outside or during task practice). We prescribed orthosis wear for 8 h daily, according to manufacturer’s guidance, intending that the orthosis would be worn during the most active parts of the day, including during task practice. Our study demonstrated that orthosis wear was discontinued as dictated by therapeutic need. It is unclear whether this represents ‘drift’ or ‘innovation’ or indeed the uncertainty for therapists of how and why the orthoses might work. Orthosis design and development, and orthosis use in practice, predate our study. These commercially available orthoses were not custom-developed for our study using a logic model to address specific problems. Rather, we wanted to explore potential orthosis effects in this population to understand if and how they might influence a range of outcomes, which would then inform development of a logic model for the intervention within this context. The exploratory nature of the study may partially explain some of the problems (for therapists) inherent in understanding the mechanism(s) of action of the orthoses. Future research on dynamic Lycra® orthoses will need to fine-tune the intervention theory, taking the feasibility randomised controlled trial findings into account. 6
Use of the Normalisation Process Theory
We selected Normalisation Process Theory because it is an internationally recognised model, and key components of the theory resonated with our previous experience, as rehabilitation therapists, of healthcare change processes. Clinical users of research are more likely to acknowledge the added value of theory-based analysis if the basic concepts of the theory ring true to their experience. 19 In addition, previous stroke rehabilitation studies successfully employed Normalisation Process Theory18,20-23 and endorsed its value as explanatory theoretical framework.13,14
The degree of normalisation we observed could be explained through Normalisation Process Theory. However, it was not always straightforward to link interview data to theoretical constructs: as researchers elsewhere 14 have found, we noted a degree of overlap between constructs. Nor could Normalisation Process Theory address all aspects of implementation
Our exploration of the coherence construct also raised questions about the Normalisation Process Theory proposition that interventions become routinely embedded because of what people do rather than what they believe. Drawing the line between sense-making as action and sense-making as belief was not straightforward. Making sense of the orthoses through reference to other familiar concepts could be construed as (cognitive) action, but we found that practitioners’ uncertainty about the mechanisms of action of the orthosis was conceptualised more easily as belief. Researchers elsewhere have similarly emphasised “understanding and conceptualisation of interventions” when applying the coherence construct 14 (p. 5), suggesting that the Normalisation Process Theory proposition that it explores what people do, and not what they believe may need revisiting.
Furthermore, NPT focuses primarily on practice change, examining how interventions are adopted, embedded, and integrated into practice. It has been criticised for placing undue emphasis on individual and collective agency, in this case, practitioner agency, without exploring wider contextual and organisational factors that act on this agency. 21 Using NPT within our feasibility RCT, meant we collected nuanced data about agency to influence practice change in relation to the protocolised intervention, but it provided us with little information about the wider sociocultural and organisation context, and workplace practices surrounding implementation. Furthermore, the focus of the NPT on practitioner agency means implementation from the perspective of recipients of the intervention is not considered. Recipient views on how it is implemented are particularly important in the context of developing and delivering an intervention within an RCT and may have the strongest influence on whether the intervention is implemented or not. There is thus a general consensus that to fully understand implementation, the NPT should not be used in isolation from other frameworks. 18
The concepts identified in our analysis provide important insights about the rehabilitation processes practitioners adopt in the context of uncertainty and ambivalence about an experimental intervention. Of particular importance to researchers is the willingness of practitioners to adapt the research intervention protocol to ensure that participants’ needs were met. This phenomenon been identified in previous studies as a potential confounding influence on study results. 24 However, it also provides insight into the priorities and reasoning of practitioners, who place the perceived needs of patients above research processes. The lesson is for researchers to seek to fully understand and anticipate the decision making processes of rehabilitation practitioners whom they expect to deliver experimental rehabilitation interventions.
Strengths and limitations
A strength of our study was the use of a theoretical framework, allowing us to work with consistent terminology and enabling more direct comparison with other implementation studies. To counter the risk of bias that comes from working with a preconceived framework, 2 researchers open-coded the data prior to application of the framework. The researchers involved in this study have clinical experience in stroke rehabilitation and may have had preconceived ideas about implementation challenges. Reflexive practice was used to counter this. There was a risk of social desirability bias: the interviewer was part of the research team, which may have made interviewees less likely to criticise the implementation process. As with any interview study, we depended on the recall of interviewees.
Finally, our findings suggest that the research facilitated orthosis wear; uncertainty about the effectiveness of the orthoses was temporarily suspended because of commitment to the research. Our study cannot provide definite insights in orthosis implementation outside a research context, where practitioners’ belief about effectiveness may be more important.
Conclusion
Our study suggests, first, that ‘good-enough’ coherence, cognitive participation, collective action and reflexive monitoring may be sufficient to kick-start a normalisation process. This was despite a degree of ambivalence towards the intervention. Second, the construct of relational integration, in interactions between therapists and patients, appeared central to the normalisation narrative (see Figure 2). Further research is needed to explore the implications of these propositions. Further orthosis research will need to fine-tune the intervention theory and mechanisms of action of orthosis wear. More generally, making intervention mechanisms of action more explicit (to practitioners) can help (them) determine whether adaptations to treatment protocols are likely to enhance or undermine an intervention.
Clinical Messages
Dynamic Lycra© orthoses fits easily into the stroke survivor-practitioner interaction and is broadly compatible with rehabilitation practitioners’ skillsets – however findings from this study cannot be used for clinical decision making on the use of these orthoses. Their effectiveness needs to be clearly established first.
Non-research funded practitioners may be willing to temporarily suspend their views on the clinical effectiveness of an intervention to support a research process.
However, practitioners are likely to prioritise maintaining a good clinical relationship with the individuals participating in rehabilitation over their sense of responsibility towards their research duties.
Acknowledgments
The authors gratefully acknowledge the collaboration of NHS Tayside staff and use of NHS Tayside premises. They also thank Rosa Mendes for her contribution to the initial conception of the project, and other steering group members.
Footnotes
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: this study was funded by the Chief Scientist Office at the Scottish Government [grant number CZH/4/1075].
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author contributions: JHM and LW initiated, designed and obtained funding for the study; JHM had overall responsibility for the conduct of the study and for monitoring progress, in collaboration with LW and AJ; AJ undertook the data collection and JMD, AJ and JHM undertook the qualitative analysis; JMD and JHM wrote the manuscript and all authors contributed to critically revising it.
Peer Review Statement: An Editor of Rehabilitation Process and Outcome is an author of this paper, therefore, the peer review process was managed by an alternative board member and the submitting editor had no involvement in the decision-making process.
ORCID iD: Jacqui Morris  https://orcid.org/0000-0002-9130-686X
https://orcid.org/0000-0002-9130-686X
References
- 1. Eccles M, Armstrong D, Baker R, et al. An implementation research agenda. Implement Sci. 2009;4:1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Morris Z, Wooding S, Grant J. The answer is 17 years, what is the question: understanding time lags in translational research. J R Soc Med. 2011;104:510-520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Medical Research Council (MRC) [Internet]. Developing and evaluating complex interventions. 2008. https://mrc.ukri.org/documents/pdf/complex-interventions-guidance/
- 4. Moore G, Audrey S, Barker M, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ. 2015;350:h1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Masterson-Algar P, Burton C, Rycroft-Malone J. The generation of consensus guidelines for carrying out process evaluations in rehabilitation research. BMC Med Res Methodol. 2018;18:180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Morris J, John A, Wedderburn L, Rauchhaus P, Donnan PT. Dynamic Lycra® orthoses as an adjunct to arm rehabilitation after stroke: a single-blind, two-arm parallel group, randomized controlled feasibility trial. Clin Rehabil. 2019;33:1331-1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Watson M, Crosby P, Matthews M. An evaluation of the effects of a dynamic lycra orthosis on arm function in a late stage patient with acquired brain injury. Brain Inj. 2007;21:753-761. [DOI] [PubMed] [Google Scholar]
- 8. Gracies J, Marosszeky J, Renton R, Sandanam J, Gandevia SC, Burke D. Short-term effects of dynamic lycra splints on arm in hemiplegic patients. Arch Phys Med Rehabil. 2000;81:1547-1555. [DOI] [PubMed] [Google Scholar]
- 9. Murray E, Treweek S, Pope C, et al. Normalisation process theory. A framework for developing, evaluating and implementing complex interventions. BMC Med. 2010;8:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. May C, Finch T. Implementing, embedding, and integrating Practices. An outline of Normalization process theory. Sociology. 2009;43: 535-554. [Google Scholar]
- 11. May C, Cummings A, Girling M, et al. Using normalization process theory in feasibility studies and process evaluations of complex healthcare interventions: a systematic review. Implement Sci. 2018;13:80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. McEvoy R, Ballini L, Maltoni S, O’Donnell CA, Mair FS, MacFarlane A. A qualitative systematic review of studies using the normalization process theory to research implementation processes. Implement Sci. 2014;9:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gale N, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sanders T, Foster N, Ong B. Perceptions of general practitioners towards the use of a new system for treating back pain: a qualitative interview study. BMC Med. 2011;9:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lloyd A, Joseph-Williams N, Edwards A, Rix A, Elwyn G. Patchy ‘coherence’. Using normalization process theory to evaluate a multi-faceted shared decision making implementation program (MAGIC). Implement Sci. 2013;8:102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Stephenson A, Stephens J. An exploration of physiotherapists’ experiences of robotic therapy in upper limb rehabilitation within a stroke rehabilitation centre. Disabil Rehabil Assist Technol. 2018;13:245-252. [DOI] [PubMed] [Google Scholar]
- 17. Holtrop J, Potworowski G, Fitzpatrick L, Kowalk A, Green LA. Effect of care management program structure on implementation: a normalization process theory analysis. BMC Health Serv Res. 2016;16:386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Connell L, McMahon N, Harris J, et al. A formative evaluation of the implementation of an arm stroke rehabilitation intervention in clinical practice. A qualitative interview study. Implement Sci. 2014;9:90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Connell L, McMahon N, Tyson S, Watkins CL, Eng JJ. Mechanisms of action of an implementation intervention in stroke rehabilitation: a qualitative interview study. BMC Health Serv Res. 2016;16:534-534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ballinger C, Taylor A, Loudon D, Macdonald AS. Rehabilitation professionals’ perceptions of the use of new visualisation software tools with people with stroke. Disability Rehab Assist Technol. 2016;11:139-149. [DOI] [PubMed] [Google Scholar]
- 21. Clarke D, Godfrey M, Hawkins R, et al. Implementing a training intervention to support caregivers after stroke. A process evaluation examining the initiation and embedding of programme change. Implement Sci. 2013;8:96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Jones F, Bailey N. How can we train stroke practitioners about patient self-management? Description and evaluation of a pathway wide training programme. Eur J Per Centered Healthcare. 2013;1:246-254. [Google Scholar]
- 23. Thomas L, French B, Burton C, et al. Evaluating a systematic voiding programme for patients with urinary incontinence after stroke in secondary care using soft systems analysis and Normalisation Process Theory. Findings from the ICONS case study phase. Int J Nurs Stud. 2014;51:1308-1320. [DOI] [PubMed] [Google Scholar]
- 24. Pomeroy VM, Rowe P, Clark A, et al. A randomized controlled Eevaluation of the efficacy of an ankle-foot cast on walking recovery early after stroke: SWIFT cast trial. Neurorehabil Neural Repair 2016;30:40-48. [DOI] [PMC free article] [PubMed] [Google Scholar]