Short abstract
Management of the subscapularis tendon is a crucial step during the approach for total shoulder arthroplasty. The method of mobilizing the tendon and the technique used to repair it determine the initial integrity of the subscapularis and impact its capacity to heal. Currently, there exist 3 well-described and well-studied approaches to managing and repairing the subscapularis: subscapularis tenotomy, subscapularis peel, and lesser tuberosity osteotomy. More recently, a subscapularis-sparing approach has been proposed as an option. There is debate in the literature regarding which technique provides optimal strength and stability for subscapularis repair following shoulder arthroplasty. In this symposium, we provide an overview of each of the techniques and review the biomechanical studies comparing them.
Keywords: Subscapularis, total shoulder arthroplasty, tenotomy, peel, lesser tuberosity osteotomy, biomechanics
Introduction
Subscapularis repair is necessary in the majority of total shoulder arthroplasty (TSA) cases and is critical to the patient’s overall outcome. A failure of subscapularis repair in TSA has the potential for poor patient outcomes and early failure of TSA.1–3 For adequate access to the glenohumeral joint during a deltopectoral approach, the subscapularis muscle and tendon must be mobilized and retracted. In general terms, the 3 primary techniques for subscapularis mobilization include subscapularis tenotomy (ST), subscapularis peel (SP), and lesser tuberosity osteotomy (LTO). Furthermore, within each of these approaches, a multitude of different repair techniques have been published, and consensus on subscapularis repair technique has not been reached. 4 Although a majority of surgeons will mobilize the subscapularis muscle through one of these approaches, subscapularis-sparing techniques have recently been described. 5 Each technique has potential benefits and limitations that will be highlighted in the article.
The subscapularis muscle originates from the undersurface, anterior aspect of the scapula. The tendon courses laterally and anterior to the glenohumeral joint, inserting on the lesser tuberosity of the humerus in a trapezoidal footprint with the widest area superiorly. 6 The subscapularis muscle receives innervation from the C5–C7 nerve roots through the upper and lower subscapular nerves. The subscapularis is important for generating shoulder motion primarily as an internal rotator as well as glenohumeral stabilization through humeral head depression in concordance with the posterior rotator cuff muscles. Cadaveric analysis has shown that the subscapularis provides 53% of the overall rotator cuff force, making it roughly equal to the force generated by the supraspinatus, infraspinatus, and teres minor combined. 7
In TSA, an intact subscapularis is integral to a successful outcome. Deficiency or rupture of the subscapularis repair in anatomic TSA has been shown to result in anterior instability. 8 Furthermore, chronic subscapularis deficiency may cause an imbalanced loading of the glenoid component, causing it to rock and loosen over time. 1 Terrier et al. found that to satisfy a mechanical equilibrium for the humeral head, a deficient subscapularis will induce decreased infraspinatus force and an increased supraspinatus force causing a net superior migration of the humeral head based on an electromyography-driven musculoskeletal model. 9
Surgical Techniques
Subscapularis Tenotomy
Tenotomy is one option for managing the subscapularis during the approach for a TSA. This technique involves vertically incising the subscapularis tendon and underlying capsule just medial to the lesser tuberosity. Several authors have described the technique in detail.4,10
Ideally, the ST should be made medially enough so that it leaves a cuff of tendon on the lesser tuberosity substantial enough to hold several sutures during repair but lateral enough to avoid the musculotendinous junction. In general, this is roughly 1 cm lateral to the insertion on the tuberosity. The incision should be carried down to bone, and nonabsorbable sutures are then used to tag and retract the medial tendon during exposure of the glenohumeral joint.
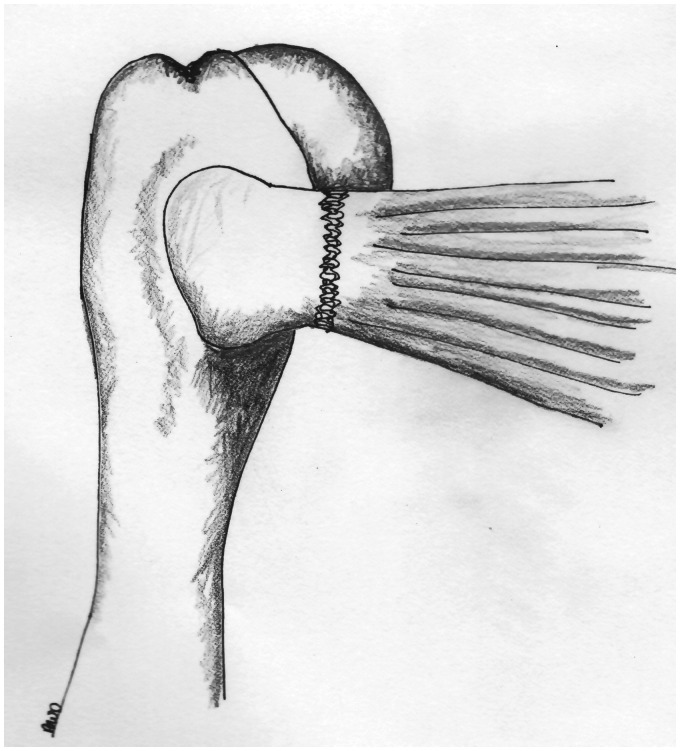
After placement of the glenoid and humeral components, the subscapularis is directly repaired to the lateral stump on the lesser tuberosity with sutures (Figure 1). There are many ways this may be accomplished, with various combinations of suture material, pattern, and number of sutures. As well, some authors augment the tendon–tendon repair with transosseous sutures through the lesser tuberosity. Others advocate suturing the superior edge of the subscapularis to the inferior edge of the supraspinatus, closing down the rotator interval and theoretically strengthening the repair.
Figure 1.
Tenotomy technique. The subscapularis tendon is directly repaired to the tendon stump still attached to the lesser tuberosity. This is often accomplished via modified Mason-Allen sutures.
Multiple investigators have performed biomechanical studies with cadaveric specimens to examine cyclic displacement and load to failure of ST repair as compared to other techniques. These studies have shown mixed results. The summarized results of these studies are shown in Table 1.
Table 1.
Summary of Biomechanical Studies of Subscapularis Repair Techniques.
| Tenotomy |
Peel |
LTO |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Author | Date | Technique | Cyclic Displacement (mm) | Ultimate Strength (N) | Technique | Cyclic Displacement (mm) | Ultimate Strength (N) | Technique | Cyclic Displacement (mm) | Ultimate Strength (N) |
| Van Den Berghe | 2007 | Four #4 Fiberwire sutures, horizontal mattress | 150 N: - 1/6 partial failure, - 1/6 complete failure, - 4/6 success; 300 N: - 3/6 complete failure, - 2/6 partial failure; - 0 success | NA | Four #2 Fiberwire sutures through drill holes, horizontal mattress configuration | 150 N: - 4/6 complete failure, - 0/6 partial failure, - 2/6 success300 N: - 2/6 complete failure, - 0/6 partial failure; - 0/6 success | NA | 5–8 mm thick LTO; #2 Fiberwire sutures through bone tunnels and tendon in “backpack” (tension-band) fashion | 150 N: - 0/7 complete failure, - 4/7 partial failure, - 3/7 success300 N: - 4/7 complete failure, - 3/7 partial failure; - 0/7 success | NA |
| Van Thiel | 2010 | Three #5 Fiberwire sutures through 3 tunnels in lesser tuberosity | 1.7 ± 1.7 | 487.1 ± 68.3 | Four #5 Fiberwire sutures through 4 bone tunnels 5–8 mm lateral to humeral cut; modified Mason-Allen | 1.8 ± 0.7 | 431.2 ± 131.3 | Thin LTO; 4 bone tunnels lateral to lesser tuberosity; two #5 Fiberwire sutures in mattress fashion through tendon, tied over titanium plate at greater tuberosity | NA | 543.3 ± 187.4 |
| Ahmad | 2007 | Four #2 Fiberwire sutures through four 2.5 mm drill holes in lesser tuberosity; three #2 Fiberwire sutures in tendon and stump | NA | 448.0 ± 190.7 | Four #2 Fiberwire sutures through four 2.5 mm drill holes along humeral cut; modified Mason-Allen | NA | 279.7 ± 167.6 | NA | NA | NA |
| Giuseffi | 2012 | Eight interrupted figure-of-eight sutures using #0 Ethibond in tendon only | 0.8 ± 0.2 | 439 ± 96 | NA | NA | NA | 4–5 mm thick; two #2 Fiberwire sutures through drill holes medial/lateral to osteotomy and around prosthesis | 1.8 ± 0.6 | 447 ± 89 |
| Fishman | 2013 | Four #2 Fiberwire sutures in tendon using modified Mason-Allen configuration | 6.0 ± 3.9 | 299.8 ± 91.8 | NA | NA | NA | Dual-row fleck LTO | 2.5 ± 2.2 | 375.2 ± 125.4 |
| Single cable large LTO | 2.4 ± 2.8 | 303.8 ± 201.8 | ||||||||
| Two suture large LTO | 3.8 ± 3.0 | 405.3 ±117.5 | ||||||||
| Krishnan | 2009 | Four #5 Ethibond sutures in modified Mason-Allen configuration | NA | 252 | NA | NA | NA | Fleck osteotomy, single row | 430.2 | |
| Fleck osteotomy, double row | 466.2 | |||||||||
| Ponce | 2005 | Tendon-to-tendon | 2.72 ± 1.24 | 334 ± 88 | Transosseous sutures | 2.11 ± 1.41 | 506 ± 175 | 4–5 mm thick; four #5 Fiberwire sutures through drill holes medial/lateral to osteotomy and around prosthesis | 0.88 ± 0.54 | 738 ± 261 |
| Schmidt | 2014 | NA | NA | NA | NA | NA | NA | Thick wafer (∼9 mm, 100% of lesser tuberosity height), compression (two #2 Fiberwire sutures around prosthesis and lesser tuberosity) | 2.4 ± 1.1 | 249.0 ± 150.1 |
| Thin wafer (∼4 mm, 50% of lesser tuberosity height), compression (two #2 Fiberwire sutures around prosthesis and lesser tuberosity) | 4.2 ± 2.3 | 234.7 ± 97.0 | ||||||||
| Thick wafer (∼9 mm, 100% of lesser tuberosity height), tension (compression plus #2 Fiberwire tension band with suture button) | 3.4 ± 2.7 | 301 ± 134.5 | ||||||||
| Thin wafer (∼4 mm, 50% of lesser tuberosity height), tension (compression plus #2 Fiberwire tension band with suture button) | 3.2 ± 2.2 | 281.8 ± 45.8 | ||||||||
Abbreviations: LTO, lesser tuberosity osteotomy; NA, not applicable.
Subscapularis Peel
An alternative to the ST is the subscapularis “peel” technique in which the tendon is stripped away from its insertion on the lesser tuberosity. Beginning laterally on the subscapularis footprint on the lesser tuberosity, electrocautery or scalpel is used to develop the plane between tendon and underlying bone. The subscapularis tendon is then elevated subperiosteally in a lateral-to-medial fashion until the entire tendon is free from its insertion. Nonabsorbable suture is then used to tag the tendon for future repair.
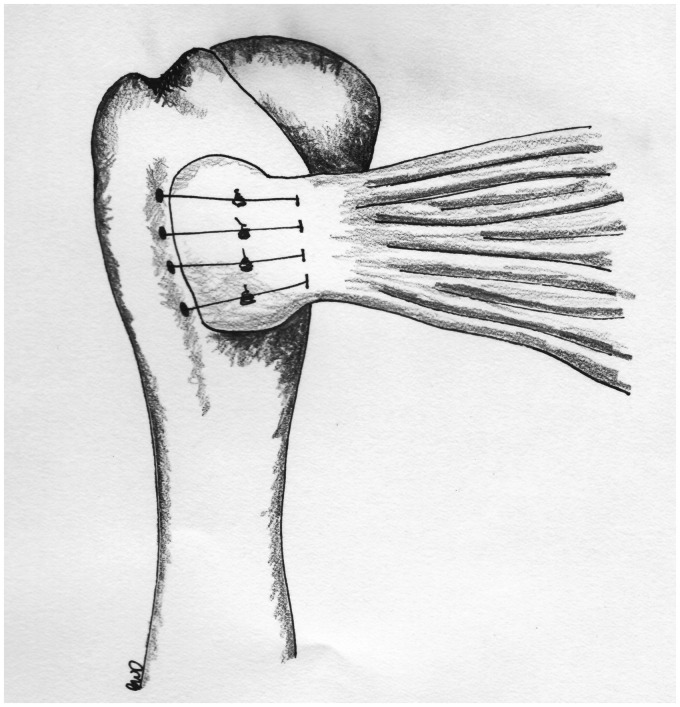
After placement of glenoid and humeral components, the subscapularis tendon is repaired back to its footprint. The surgeon uses a drill to make several bone tunnels in the lesser tuberosity, exiting on the medial aspect of the bicipital groove where strong bone is ideal for suture fixation (Figure 2). There is some variability in the literature regarding placement of the drill holes. Some authors describe their exiting on the lateral greater tuberosity. 11 In addition, the drill holes can be augmented with miniplates to prevent pull through of the sutures. Ultimately, the SP technique relies on tendon-to-bone healing.
Figure 2.
Peel technique. After placing drill holes in the lesser tuberosity and the medial aspect of the bicipital groove, sutures are tied to repair the tendon down to its footprint on the lesser tuberosity.
Lesser Tuberosity Osteotomy
The third general category of subscapularis mobilization during TSA is with an LTO. During exposure of the glenohumeral joint, instead of violating the subscapularis tendon itself, a small wafer of bone is removed from the lesser tuberosity with the subscapularis tendon attached. Several different techniques for LTO exist, but generally speaking, it involves creating a wafer of bone starting at the medial aspect of the bicipital groove using an osteotome, chisel, or saw. 12 The subscapularis and lesser tuberosity may then be retracted medially in order to gain access to the glenohumeral joint.
Theoretical benefits of using an LTO is that it allows for bone-to-bone healing as opposed to tendon-to-bone healing or tendon-to-tendon healing. Furthermore, removal of part of the lesser tuberosity may allow for better visualization of the glenoid during that part of the shoulder arthroplasty. Potential risks of the LTO include violation of the metaphysis and loss of metaphyseal bone in the proximal humerus. LTO and its repair may also be more technically demanding and time consuming. 4
A number of different techniques for LTO have been published and studied biomechanically. The techniques are briefly described below, and a summary of their biomechanical properties is found in Table 2.
Table 2.
Summary of Biomechanical Studies of Lesser Tuberosity Repair Techniques.
| LTO Techniques | ||||
|---|---|---|---|---|
| Author | Year | Technique | Cyclic Displacement (mm) | Load to Failure (N) |
| Krishnan | 2009 | 3–4 mm fleck, SR | N/A | 430.2 |
| 3–4 mm fleck, DR | N/A | 466.2 | ||
| Giuseffi | 2012 | 4–5 mm fleck, comp | 1.8 | 447 |
| Schmidt | 2014 | 9 mm, compression sutures | 2.4 | 249 |
| 9 mm, compression + tension sutures | 3.4 | 301 | ||
| 4 mm, compression sutures | 4.2 | 234.7 | ||
| 4 mm, compression + tension sutures | 3.2 | 281.8 | ||
| Heckman | 2011 | 8 mm, tension sutures | 6.9 | 510.9 |
| 8 mm, DR | 4.6 | 632.3 | ||
| Fishman | 2013 | Fleck, DR | 2.5 | 375.2 |
| Large, SR | 2.4 | 303.8 | ||
| Large, DR | 3.8 | 405.3 | ||
| Ponce | 2005 | 4–5 mm, tension sutures | 0.88 | 738 |
| Van Thiel | 2010 | 5 mm, tension sutures | 1.2 | 543.3 |
Abbreviations: DR, double row; LTO, lesser tuberosity osteotomy; SR, single row.
When creating the LTO, the size of the bone wafer does have implications on the strength of repair. Schmidt et al. compared thin osteotomies (50% of the lesser tuberosity height) and thick osteotomies (100% of the lesser tuberosity height) in cadaveric shoulders. This study determined that thin LTOs have less displacement than thick LTOs, and that a combination of tension and compression suturing techniques had better properties than just compression suture technique. 13 Furthermore, Fishman et al. found improved biomechanical results in a cadaveric model in LTO compared to ST, but no significant differences when comparing a fleck LTO and a large thickness LTO. 14
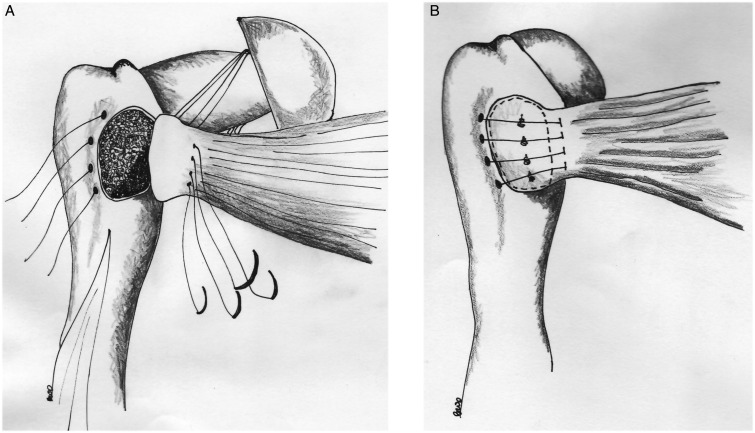
A number of different methods for suture repair of the LTO have been studied. Compression suturing involves capturing the lesser tuberosity via a cerclage technique with the sutures anchored around the humeral head or the stem of the humeral prosthesis, causing a compression force on the LTO (Figure 3). Tension-band suture differs from compression suture technique in that the subscapularis tendon is captured with suture material, secured through a drill hole across the humeral head, and fixated through drill tunnels or a button on the greater tuberosity. This technique gives a tension band type of effect, resisting the subscapularis from displacing during force application. This technique has also been called the “backpack” technique. 12 A combination of tension-band and compression sutures has been shown to have improved biomechanical cyclic displacement and load to failure compared to compression suture alone. 13 Suture may be passed around the humeral head or around the stem of the humeral implant. Biomechanical studies have shown that, for tension suturing, passing suture around the humeral stem provides overall better strength than passing suture through humeral bone only.13–17
Figure 3.
Lesser tuberosity osteotomy. A, Drill holes are placed medial and lateral to the lesser tuberosity, and suture is wrapped around the stem of the prosthesis. B, After seating the prosthesis, the sutures are tied to compress the fleck of bone to its donor site.
Single-row and dual-row repair techniques have also been described. Krishnan et al. described a single-row technique that involved a 3- to 4-mm fleck LTO that was repaired with four #5 Ethibond sutures through the subscapularis tendon in simple fashion and passed transosseously lateral to the bicipital groove. The dual-row technique involved the same technique with the addition of a medial row of 4 more #5 Ethibond sutures at the anatomic humeral neck. 15
Subscapularis Sparing
A subscapularis sparing approach was first described by Lafosse et al. in 2009 as a technique to preserve the superior 50% of the subscapularis tendon insertion while gaining exposure to the glenohumeral joint. 18 Originally described using a superolateral incision, this technique has been adapted by other surgeons to be performed via the deltopectoral interval. 19 After identifying the subscapularis insertion, the inferior 30% to 50% of the tendon is elevated off of the lesser tuberosity in a manner similar to the SP, thus preserving the upper tendinous portion of the subscapularis insertion. Dissection is then performed medially around the humeral head as the arm is progressively externally rotated. The subscapularis muscle is then “flipped” over the humeral head to provide exposure to the articular surface. After reaming and placement of the prosthesis, the arm is internally rotated and adducted to reduce the humeral head. The inferior 30% to 50% of the subscapularis tendon is then repaired to the lesser tuberosity footprint using nonabsorbable suture in a transosseous fashion, just as in the SP technique.
The subscapularis-sparing technique is not as widely utilized as the other approaches because it is more technically challenging and does not allow for the same amount of exposure. However, it does offer the advantage of keeping at least a portion of the subscapularis tendon attachment intact, which may prevent a significant portion of TSA failures. 5 A recent biomechanical study by Simovitch et al. compared load to failure in cadaveric shoulders with an intact subscapularis tendon, a 50% released tendon with repair, and a 100% released tendon with repair. The study found a load to failure of 1341.2 N in the intact subscapularis group, 744.3 N in the 50% release with repair, and 380.1 N in the 100% release and repair group. 20
As TSA techniques move toward a more minimally invasive approach, the complete or partial subscapularis sparing techniques may gain popularity. Currently, no biomechanical studies compare subscapularis sparing techniques to ST, SP, or LTO.
Discussion
Subscapularis Tenotomy
Several authors have shown that ST repair has equal or superior biomechanics compared to alternative techniques. In 2007, Van Den Berghe et al. tested the strengths of ST repair, SP technique, and LTO in 19 fresh frozen cadaveric shoulders. The authors tested the fatigue strength of the 3 techniques with 500 cycles of 150 N followed by 2500 cycles of 300 N. They found that tendon-to-tendon repair had comparable strength to LTO and SP techniques. 21 Also, in 2007, Ahmad et al. randomized 12 paired fresh frozen cadaveric shoulders to either SP or ST repair augmented with transosseous suture. They preloaded the specimens with 5 N for 1 minute, then increased the load in 25 N increments for 40 cycles each to a maximum load of 330 N, followed by an increasing load of 1 mm/s until ultimate failure. They found that tendon–tendon repair with transosseous sutures showed superior stiffness compared to SP with transosseous sutures. 22 In 2010, Van Thiel et al. randomized 24 cadaveric shoulders to 3 groups: ST with transosseous suture, SP, and LTO. They preloaded the repairs with 10 N for 1 minute, followed by increasing loads of 10–100 N for 150 cycles each, and then an increasing load at 1 mm/s until failure. They found no statistically significant differences in elongation, maximum load, and stiffness among the 3 repair techniques. 23 In 2012, Giuseffi et al. published a comparison of ST and LTO in 20 paired cadaveric shoulder specimens which were loaded cyclically to 100 N for 3000 cycles and then loaded at 2 mm/s until failure. They showed no significant difference in load to failure between the 2 groups, but the ST specimens did show significantly less cyclic displacement compare to the LTO specimens. 16
Although the above studies showed the ST repair to have similar stiffness, load to failure and cyclic elongation when compared to SP and LTO, other studies have shown the ST to be biomechanically inferior. For instance, Ponce et al. performed direct comparison of ST, SP, and LTO. They divided 27 cadaveric shoulders into 3 groups, performed the repairs, loaded the specimens to 100 N for 3000 cycles, and finally at 33 mm/s until failure. They found ST to have significantly greater cyclic displacement and a significantly lower ultimate failure load when compared to LTO. 17 The authors commented that weak point of the ST repair appeared to be the tendon itself because, they observed, each ST specimen failed via suture cutout through tendon. In 2009, Krishnan et al. compared ST repair to 2 types of LTO fixation (single and double row) in 15 cadaveric specimens. They loaded each specimen from 0 to 180 N at for 400 cycles each and then increased by 180 N per 400 cycles until failure. They demonstrated that the ST had significantly lower load to failure than either of the LTO techniques. 15 In 2013, Fishman et al. published the results of a study comparing ST repair to 3 variations of LTO in 20 fresh frozen cadaveric shoulders. Each of the constructs was preloaded to 5 N, cyclically loaded from 25 to 250 N for 40 cycles each, and then loaded at 1 mm/s until ultimate failure. Interestingly, no significant difference in ultimate load to failure was noted among the ST and various LTO techniques. However, the ST repair demonstrated significantly greater cyclic displacement than any of the LTO repair techniques. 14
In recent years, multiple investigators have examined the clinical outcomes of the ST technique, in comparison to the other subscapularis management techniques. Much like the biomechanical data, these studies have yielded mixed results. In 2010, Scalise et al. published a retrospective cohort study of comparing 14 patients who underwent ST and 20 who underwent LTO. 24 At a minimum of 1-year postop, the patients were assessed with a physical examination (belly press, lift-off tests), measurement of internal rotation strength with hand-held dynamometer, clinical outcome questionnaires (Penn Shoulder Score), as well as radiographic assessment of healing and ultrasound assessment of subscapularis healing. Although the LTO group had higher Penn Shoulder Scores than the ST group 92 ± 11 points vs 81 ± 20 points, P = .04), there were no significant differences noted in internal rotation strength or physical examination maneuvers. On ultrasound assessment, 7 of the 14 points who underwent ST had abnormal subscapularis tendon findings (6 with tendon attenuation and 1 with full-thickness tear) compared to just 2 of the 20 points who underwent LTO (both attenuation) (P = .01). The authors concluded that the ST results in lower functional scores, higher rate of postoperative tears compared to LTO. In a similar retrospective cohort study, Buckley et al. compared 32 patients who underwent ST to 28 points who underwent LTO. 25 The patients were assessed with physical examination, ultrasound, and functional scoring systems (the Western Ontario Osteoarthritis of the Shoulder [WOOS] index, the Disability of the Arm, Shoulder, and Hand, and Constant Scores). The ST group had greater external rotation than the LTO group, but no differences were noted on in belly-press, bear-hug tests, or functional scores. Ultrasound demonstrated abnormal tendons in 4 (12.5%) of the 32 ST patients, but none of the LTO patients. These 2 studies were included in a 2017 systematic review by Louie et al. comparing the clinical and radiographic outcomes of ST and LTO. 26 Twenty studies were included, comprising 1420 shoulders in 1392 patients. Overall, the authors noted no differences in Constant scores, pain scores, or radiographic evidence of healing. The only statistically significant difference was that the ST group experienced greater increase in forward elevation compared to the LTO group (+50.9 ± 17.5° vs +31.3 ± 0.9°, P < .01). No significant differences were detected with regard to complication or revision rates. Similar results were found in a 2019 randomized controlled trial by Levine et al. 27 In their study, 60 shoulders were randomized to receive either ST or LTO. Follow-up was at regular intervals to 1 year postoperatively, with outcome measures including ultrasound/radiographic assessment of tendinous/osseous healing, as well as range of motion and clinical outcome scores. The investigators found that LTO healed more reliably than ST (93.1% vs 86.7%), but no differences were noted in range of motion or any clinical outcome score.
Subscapularis Peel
Several of the studies regarding ST have also examined the biomechanics of SP repairs. Again, several of these cadaveric studies have shown the SP technique to be similar to ST and LTO. In 2007, Van Den Berghe et al. demonstrated that the SP technique showed similar cyclic displacement and failure rates as either the ST or LTO techniques. 21 In their 2010 paper, Van Thiel et al. demonstrated the SP technique to have similar cyclic elongation, ultimate strength and stiffness when compared to ST or LTO repairs. 23
Other studies have shown the SP to be biomechanically inferior to the alternative techniques. For instance, the 2007 paper by Ahmad et al. showed that SP repair with transosseous sutures to have inferior stiffness compared to ST repair with transosseous sutures. The authors also noted that the repaired subscapularis footprint after the peel was significantly smaller than the native footprint, which, they hypothesized, could compromise final mechanical strength after healing has occurred. 22 In 2005, Ponce et al. demonstrated that, like the ST, the SP repair technique had significantly greater cyclic displacement and significantly inferior ultimate strength when compared to LTO. 17 They also noted that all of the failures of the SP specimens occurred at the bone-tendon junction.
Lesser Tuberosity Osteotomy
A majority of biomechanical models have demonstrated improved ultimate strength with LTO repair when compared to ST. Krishnan et al. compared 2 different LTO techniques to ST and demonstrated almost double the ultimate strength in the LTO groups. 15 Fishman et al. found that LTO repairs trended toward better strength, but these results did not reach statistical significance. However, the authors did demonstrate significantly increased gapping during cyclical loading in the ST group. 14 Giuseffi et al. conversely found similar construct strengths and greater cyclical displacement in the LTO group; however, the LTO group was fixated with a compression suture only. 16
Three additional biomechanical studies compared LTO to SP and ST. Ponce et al. found superior maximum load to failure and decreased cyclic displacement in LTO repairs with compression technique when compared to both SP and ST. 17 Van Thiel et al. compared LTO repair with tension-band sutures not encompassing the humeral stem and found no significant differences in load to failure or cyclic displacement compared to SP or ST techniques. 23 Finally, Van Den Berghe et al. concluded that the SP technique resulted in significantly earlier failure compared to LTO and ST techniques. No significant difference between ST and LTO existed in failure rate during cyclical loading. However, the ST group did have significantly more tendon shortening due to repair technique, and the authors concluded that LTO repair provided the best combination of strength and restoration of tendon length. 21 Larger reviews of the literature have reinforced the superiority of the LTO over ST and SP. In 2016, Schrock et al. published a systematic review and meta-analysis of all existing biomechanical studies of subscapularis management techniques. In both papers, the authors found the LTO to provide the greatest load to failure and least cyclical displacement of the described techniques.28,29
Several authors have directly compared SP to LTO with regard to clinical outcomes, with results that slightly favor LTO over SP. In 2017, Shafritz et al. published a retrospective cohort study of 90 consecutive total shoulder surgeries performed, 46 via SP and 44 via LTO by a single surgeon. 30 Outcome measures included the lift-off test, range of motion, and functional scores. Patients undergoing LTO had a higher rate of normal lift-off test at final follow-up compared to those undergoing SP (91.0% vs 69.6%, P = .01). The LTO group also had significantly higher Simple Shoulder Test and Visual Analog Scale scores than the SP group. The only level I evidence comparing SP to LTO was published by Lapner et al. in 2012.11 In this randomized controlled trial, 87 patients undergoing shoulder arthroplasty were randomized to LTO (n = 43) or SP (n = 44) and followed for 2 years. The primary outcome measure was subscapularis strength, measured via handheld dynamometer in the belly-press position. Secondary measures included the WOOS and American Shoulder and Elbow Surgeons (ASES) score. No significant difference was detected in subscapularis strength between the LTO group (4.4 ± 2.9 kg) and SP group (5.5 ± 2.6 kg, P = .131). Also, no significant differences in WOOS and ASES scores were detected between the LTO and SP groups at any time point. A year later, the same authors published a follow-up study comparing these patients with regard to radiographic evidence of healing and subscapularis function, as measured by Goutallier grade of fatty infiltration. Again, no significant differences were detected in healing rate (95% bony union for LTO and 100% tendon healing for SP), postop Goutallier fatty infiltration grade or (means 0.9 ± 0.89 for LTO and 0.95 ± 0.85 for SP).
In a 2018 systematic review, Choate et al. attempted the most comprehensive 3-way comparison of clinical outcome measures of ST, SP, and LTO to date. 31 The 14 studies included in the review were heterogeneous with respect to specific operative techniques as well as outcomes measures. The outcomes of interest were musculotendinous integrity, subscapularis testing/strength, shoulder range of motion, and various functional scores. Overall, they found the healing rate, as measured by radiographic (computed tomography, magnetic resonance imaging, or ultrasonography) evidence of intact musculotendinous unit, was higher in for LTO (93.1%) than for either SP (84.1%) or ST (75.7%). All techniques resulted in some fatty atrophy of the subscapularis muscle, and there were no significant differences among techniques. On physical examination, patients with LTO had a higher rate of normal belly-press and lift-off tests (79.1% and 80.7%, respectively) compared to those with ST (66.7% and 65.6%). Of note, however, the authors noted no correlation between these test results and tendon integrity on imaging. Functional scores showed mixed results: LTO resulted in higher Constant and WOOS scores compared to SP, but the ST resulted in higher ASES scores than either LTO or SP.
Conclusion
The chosen technique for subscapularis tendon mobilization in shoulder arthroplasty is still a widely debated topic. While tenotomy and peel procedures may preserve more proximal humerus bone stock, these do not offer the theoretical advantage of direct bone to bone healing that the LTO has. Available biomechanical studies have shown that an LTO is biomechanically superior in strength and durability, and while there are a number of variations on repair techniques for LTOs, a thin wafer of bone with a dual-row repair and the suture being anchored around the humeral stem appear to offer the most biomechanically stable construct. 29 In clinical outcomes studies, the LTO has been shown to result in favorable healing rates and equivalent functional scores when compared to other techniques. Ultimately, surgeons should use the approach that they are most comfortable with as there is no definitive answer on which technique is superior, and these biomechanical differences have not yet been elucidated in the clinical realm.25,31 Our recommendation based on the available data is to mobilize the subscapularis with a thin lesser tuberosity osteotomy in TSA when possible due to its biomechanical superiority, though we look forward to clinical data to support or refute this practice.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Utz C, Bauer T, Iannotti J. Glenoid component loosening due to deficient subscapularis: a case study of eccentric loading. J Shoulder Elbow Surg. 2011; 20(8):e16–e21. [DOI] [PubMed] [Google Scholar]
- 2.Miller B, Joseph T, Noonan T, Horan M, Hawkins R. Rupture of the subscapularis tendon after shoulder arthroplasty: diagnosis, treatment, and outcome. J Shoulder Elbow Surg. 2005; 14(5):492–496. [DOI] [PubMed] [Google Scholar]
- 3.Jackson J, Cil A, Smith J, Steinmann S. Integrity and function of the subscapularis after total shoulder arthroplasty. J Shoulder Elbow Surg. 2010; 19(7):1085–1090. [DOI] [PubMed] [Google Scholar]
- 4.Shields E, Ho A, Wiater J. Management of the subscapularis tendon during total shoulder arthroplasty. J Shoulder Elbow Surg. 2017; 26(4):723–731. [DOI] [PubMed] [Google Scholar]
- 5.Ding D, Mahure S, Akuoko J, Zuckerman J, Kwon Y. Total shoulder arthroplasty using a subscapularis-sparing approach: a radiographic analysis. J Shoulder Elbow Surg. 2015; 24(6):831–837. [DOI] [PubMed] [Google Scholar]
- 6.Richards D, Burkhart S, Tehrany A, Wirth M. The subscapularis footprint: an anatomic description of its insertion site. Arthroscopy. 2007; 23(3):251–254. [DOI] [PubMed] [Google Scholar]
- 7.Keating J, Waterworth P, Shaw-Dunn J, Crossan J. The relative strengths of the rotator cuff muscles. A cadaver study. J Bone Joint Surg Br. 1993; 75(1):137–140. [DOI] [PubMed] [Google Scholar]
- 8.Moeckel B, Altcheck D, Warren R, Wickiewicz T, Dines D. Instability of the shoulder after arthroplasty. J Bone Joint Surg Am. 1993; 75(4):492–497. [DOI] [PubMed] [Google Scholar]
- 9.Terrier A, Larrea X, Malfroy Camine V, Pioletti D, Farron A. Importance of the subscapularis muscle after total shoulder arthroplasty. Clin Biomech (Bristol, Avon). 2013; 28(2):146–150. [DOI] [PubMed] [Google Scholar]
- 10.DeFranco M, Higgins L, Warner J. Subscapularis management in open shoulder surgery. J Am Acad Orthop Surg. 2010; 18(1):707–717. [DOI] [PubMed] [Google Scholar]
- 11.Lapner P, Sabri E, Rakhra K, Bell K, Athwal G. Comparison of lesser tuberosity osteotomy to subscapularis peel in shoulder arthroplasty: a randomized controlled trial. J Bone Joint Surg Am. 2012; 94(2):2239–2246. [DOI] [PubMed] [Google Scholar]
- 12.Gerber C, Pennington S, Yian E, Pfirrmann C, Werner C, Zumstein M. Lesser tuberosity osteotomy for total shoulder arthroplasty: surgical technique. J Bone Joint Surg Am. 2006; 88(Suppl 1):170–177. [DOI] [PubMed] [Google Scholar]
- 13.Schmidt C, Jarrett C, Brown B, et al. Effect of lesser tuberosity osteotomy size and repair construct during total shoulder arthroplasty. J Shoulder Elbow Surg. 2014; 23(1):117–127. [DOI] [PubMed] [Google Scholar]
- 14.Fishman M, Budge M, Moravek J, et al. Biomechanical testing of small versus large lesser tuberosity osteotomies: effect on gap formation and ultimate failure load. J Shoulder Elbow Surg. 2014; 23(4):470–476. [DOI] [PubMed] [Google Scholar]
- 15.Krishnan S, Stewart D, Reineck J. Subscapularis repair after shoulder arthroplasty: biomechanical and clinical validation of a novel technique. J Shoulder Elbow Surg. 2009; 18(2):184–192. [DOI] [PubMed] [Google Scholar]
- 16.Giuseffi S, Wongtriratanachai P, Omae H, et al. Biomechanical comparison of lesser tuberosity osteotomy versus subscapularis tenotomy in total shoulder arthroplasty. J Shoulder Elbow Surg. 2012; 21(8):1087–1095. [DOI] [PubMed] [Google Scholar]
- 17.Ponce B, Ahluwalia R, Mazzocca A. Biomechanical and clinical evaluation of a novel lesser tuberosity repair technique in total shoulder arthroplasty. J Bone Joint Surg Am. 2005; 87(Suppl 2):1–8. [DOI] [PubMed] [Google Scholar]
- 18.Lafosse L, Schnaser E, Haag M, Gobezie R. Primary total shoulder arthroplasty performed entirely thru the rotator interval: technique and minimum two-year outcomes. J Shoulder Elbow Surg. 2009; 18:864–873. [DOI] [PubMed] [Google Scholar]
- 19.Routman HD, Savoie FH. Subscapularis-sparing approaches to total shoulder arthroplasty: ready for prime time? Clin Sports Med. 2018; 37:559–568. [DOI] [PubMed] [Google Scholar]
- 20.Simovitch R, Nayak A, Scalise J, et al. Biomechanical characteristics of subscapularis-sparing approach for anatomic total shoulder arthroplasty. J Shoulder Elbow Surg. 2018; 27:133–140. [DOI] [PubMed] [Google Scholar]
- 21.Van Den Berghe G, Nguyen B, Patil S, et al. A biomechanical evaluation of three surgical techniques for subscapularis repair. J Shoulder Elbow Surg. 2008; 17(1):156–161. [DOI] [PubMed] [Google Scholar]
- 22.Ahmad C, Wing D, Gardner T, Levine W, Bigliani L. Biomechanical evaluation of subscapularis repair used during shoulder arthroplasty. J Shoulder Elbow Surg. 2007; 16(3):S59–S64. [DOI] [PubMed] [Google Scholar]
- 23.Van Thiel G, Wang V, Wang F, et al. Biomechanical similarities among subscapularis repairs after shoulder arthroplasty. J Shoulder Elow Surg. 2010; 19(5):657–663. [DOI] [PubMed] [Google Scholar]
- 24.Scalise JJ, Ciccone J, Iannotti J. Clinical, radiographic, and ultrasonographic comparison of subscapularis tenotomy and lesser tuberosity osteotomy for total shoulder arthroplasty. J Bone Joint Surg Am. 2010; 92:1627–1634. [DOI] [PubMed] [Google Scholar]
- 25.Buckley T, Miller R, Nicandri G, Lewis R, Voloshin I. Analysis of subscapularis integrity and function after lesser tuberosity osteotomy versus subscapularis tenotomy in total shoulder arthroplasty using ultrasound and validated clinical outcome measures. J Shoulder Elbow Surg. 2014; 23:1309–1317. [DOI] [PubMed] [Google Scholar]
- 26.Louie PK, Levy DM, Bach BR, Jr, Nicholson GP, Romeo AA. Subscapularis tenotomy versus lesser tuberosity osteotomy for total shoulder arthroplasty: a systematic review. Am J Orthop. 2017; 46(2):E131–E138. [PubMed] [Google Scholar]
- 27.Levine WN, Munoz J, Hsu S, et al. Subscapularis tenotomy versus lesser tuberosity osteotomy during total shoulder arthroplasty for primary osteoarthritis: a prospective, randomized controlled trial. J Shoulder Elbow Surg. 2019; 28:407–414. [DOI] [PubMed] [Google Scholar]
- 28.Schrock J, Kraeutler M, Houck D, Provenzano G, McCarty E, Bravman J. Lesser tuberosity osteotomy and subscapularis tenotomy repair techniques during total shoulder arthroplasty: a meta-analysis of cadaveric studies. Clin Biomech (Bristol, Avon). 2016; 40:33–36. [DOI] [PubMed] [Google Scholar]
- 29.Schrock J, Kraeutler M, Crellin C, McCarty E, Bravman J. How should I fixate the subscapularis in total shoulder arthroplasty? A systematic review of pertinent subscapularis repair biomechanics. Shoulder Elbow. 2017; 9(3):153–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shafritz AB, Fitzgerald MG, Beynnon BD, DeSarno MJ. Lift-off test results after lesser tuberosity osteotomy versus subscapularis peel in primary total shoulder arthroplasty. J Am Acad Orthop Surg. 2017; 25:304–313. [DOI] [PubMed] [Google Scholar]
- 31.Choate S, Kwapisz A, Momaya A, Hawkins R, Tokish J. Outcomes for subscapularis management techniques in shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg. 2018; 27:363–370. [DOI] [PubMed] [Google Scholar]