Abstract
Aim:
To examine concussion-related disability in neck injuries, the Rivermead Head Injury Follow-Up Questionnaire (RHFUQ) was applied. Furthermore, we wanted to investigate symptoms found in post-concussion syndrome (PCS) and global pain, neck pain intensities obtained from acute whiplash patients within 1 week and at 6 months after injury in a prospective study on 1-year work disability.
Methods:
A total of 143 consecutive acute whiplash-injured patients were admitted to the study from the Emergency Unit (Aarhus University Hospital). Patients with direct head trauma or reported retro- or anterograde amnesia were excluded from the study. Average neck pain and global pain intensity were measured on a Visual Analogue Scale (VAS 0-10). The RHFUQ (10 items, score from 0 to 4, total score from 0 to 40) was fulfilled after 1 week and 6 months. Patients underwent neurological examination within 1 week after injury. Recovery (return to work) was assessed 1 year post-injury.
Results:
In total, 97% completed the study, and 9% (12/138) did not recover. Non-recovered patients reported more neck pain and global pain after 1 week (P < .003) and 6 months (P < .008) and higher PCS symptom score after 1 week (P < .001) and 6 months (P < .002). Using the RHFUQ total score as a predictive test, a receiver-operating characteristic curve (ROC) area of 0.77 (0.61-0.92) and a cut-off at 10 points revealed a sensitivity of 75% and a specificity of 67.2%. At 1 week, 8 of 10 items reached higher scores among non-recovered and 10 of 10 items after 6 months post-injury.
Conclusions:
RHFUQ is useful in acute whiplash patients for predicting 1-year work disability. PCS-related symptoms along with neck pain and global pain are more burdensome in the non-recovered group. This emphasizes that post-concussion symptoms are not a sign of brain injury alone, but are found in other types of mishaps like whiplash injuries.
Keywords: neck pain, whiplash, disability, recovery, Rivermead Head Injury Questionnaire, post-concussion syndrome
Introduction
Concussion-related symptoms are in general perceived as symptoms related to recent or earlier head/brain injuries. The distinction between mild traumatic brain injuries with scores on the Glasgow Coma Scale from 13 to 15 and whiplash (neck) injuries can be difficult to assess at temporal distance from the injury scene.
Whiplash injury may lead to a multi-facetted condition associated with a large variety of symptoms: neck pain, headache, stiffness of neck muscles, paraesthesia in the shoulder/arm/hand, fatigue, memory disturbances, lack of concentration, irritability, anxiety and low self-efficacy beliefs, and a syndrome designated whiplash-associated disorders (WAD).1,2 WAD can be classified by the severity of signs and symptoms from grades 0 (no complaints or physical signs) to 4 (fracture or dislocation).2,3 Factors related to poor recovery following whiplash injury are high initial neck pain intensity, socio-demographic status, compensation (litigation), psychosocial factors, and physical factors including reduced neck mobility, impaired sympathetic vasoconstriction, and reduced cold pain tolerance.4-6 Individuals sustaining apparently mild head injuries often complain of several physical, cognitive, and emotional/behavioural symptoms referred to as post-concussion symptoms7-9 and 10 main symptoms are included in the post-concussion syndrome (PCS as defined by the Mayo Clinic; https://www.mayoclinic.org/diseases-conditions/post-concussion-syndrome/symptoms-causes/syc-20353352). These symptoms include headache (post-concussion headache), dizziness, fatigue, irritability, anxiety, insomnia, concentration problems, tinnitus, blurred vision, and sensitivity to noise. This cluster of symptoms can persist from months to years following injury and cause prolonged disability.8,9 Symptoms from PCS are common complaints in chronic pain conditions in the absence of previous head injury, but in other types of mishaps, like whiplash injuries these symptoms are often reported. 10
The Rivermead Head Injury Follow-Up Questionnaire (RHFUQ) was devised on the basis of clinical experience to measure functional and social outcomes in cases of minor head injury. 11 The questionnaire was found reliable in detecting changes in patients with minor head injury. RHFUQ covers disability and the practical consequences of any loss of function.
The aim of this study was to apply The Rivermead Head Injury Questionnaire 11 in a group of neck-injured patients. Do so-called ‘head-injury symptoms’ relate to region of injury or are they less specific. 10 The hypothesis of this study is that concussion-related disabilities derived from the RHFUQ scores and the burden of so-called concussion-related symptoms in similarity with neck pain and global pain predict non-recovery after whiplash injury.
Methods
Study design
During a 1-year period, patients admitted to 1 of 2 emergency departments from an area covered by Aarhus University Hospital Denmark, being exposed to a whiplash injury during rear-end collision motor vehicle accidents within 48 hours after a car accident were invited to participate in this study. Consecutive patients who gave informed written and verbal consent to participate were followed in a prospectively designed 1-year follow-up study. In this study of concussion-related symptoms, the whiplash-injured subjects underwent a semi-structured interview, questionnaires and a thorough neurological examination within 1 week and after 6 months post-injury. Recovery (return to work) and work disability were registered after 1-year post-injury. 12 Work disability was determined by a semi-structured interview where whiplash-injured patients were asked to choose between 6 items after 1 year: (1) My working capacity is the same as before whiplash injury. (2) I work the same hours as before whiplash injury, but my tasks have been simplified or reduced due to problems after injury. (3) I have reduced working hours and reduced work capacity due to problems after whiplash injury. (4) I have been dismissed from my job or have changed job due to problems after whiplash injury. (5) I am in job training due to problems after injury. (6) I have applied for or have received disability pension due to problems after injury.
A person was regarded as work disabled if he or she selected item 3, 4, 5, or 6. Number of days until return to work or daily activities after injury was also obtained. Observation time was often more than 365 days. Written and verbal informed consent was obtained from the participants at first visit. The study was approved by the local Ethics Committée for Aarhus County (registration number 1996/3799) and was conducted in accordance with the Helsinki II Declaration.
Inclusion/exclusion
Participants met the following inclusion criteria: age between 18 and 70 years, exposure to a rear-end car accident with preserved consciousness during collision, and classification of WAD grades I-III. Exclusion criteria were WAD grades 0 or IV, retrograde or anterograde amnesia after the accident, alcohol or substance abuse, severe psychiatric disorder or somatic disease, and previously recognized chronic pain conditions.
Outcome measures
Self-reported neck pain intensity was measured on a 10 cm (100 points) Visual Analogue Scale (VAS 0-10), from 0 = no pain to 10 = unbearable pain.
RHFUQ was based on 10 items and a total range of scores between 0 and 40 was obtained from the graded response (0-4). The RHFUQ assessed different bio-psycho-social aspects of life by addressing functional activities such as ability to participate in conversation with one or more people, performance of routine domestic activities, ability to participate in previous social activities, ability to enjoy leisure activities, ability to maintain previous work/load standard, finding work more fatiguing, ability to keep relationship with friends or partner, and ability to cope with family demands. The rating score was 0 to 4, with 0 = no change in comparison with the function level before the injury; 1 = no change, but more difficult; 2 = a mild change; 3 = a moderate change; 4 = a very marked change. 10 Pain scores and RHFUQ were obtained at 1 week and 6 months post-injury. Recovery (return to work) was registered at 1-year post-injury. Patients, who did not return to work due to WAD symptoms, were registered as non-recovered. 12
Statistical analysis
Non-parametric tests for 2-sample data were used when comparing data of whiplash patients who recovered (returned to work) after the observation period with non-recovered patients. Proportions were analysed with Fisher exact test. VAS pain intensities were calculated as median values.
P-values indicate tests of group differences: P < .05 was considered significant. For multiple comparisons, Bonferroni correction was applied. Receiver-operating characteristic curves (ROCs) and sensitivity and specificity plots were provided to examine the predictive value of RHFUQ. A multiple regression model was fitted to examine the relationship between PCS symptom score, total RHFUQ score, and reported neck pain (VAS 0-10).
Results
During a 1-year period, 230 patients exposed to acute whiplash injury were admitted to 1 of the 2 Emergency Departments at Aarhus University Hospital, Denmark, covering an area of approximately 380 000 citizen (from 1997 to 1999). Thirty-two patients with a medical record of previous neck or low back disorders, head injuries (including post-concussion syndrome), severe headache, migraine or widespread pain, severe psychiatric disease, and medication or alcohol abuse were excluded. Of the remaining 198 subjects, 55 did not show up at the first examination. One hundred and forty-three whiplash-exposed subjects (WAD grades I-III) were examined and completed semi-structured interviews on pain and PCS symptoms and the RHFUQ 1 week post-injury. At 6-month follow-up, 122 patients underwent semi-structured interview and 112 completed RHFUQ. One year after the injury, 12 (8%) of the initial 143 participants did not regain the same work capacity as before the injury, 96.5% (138/143) completed the study. Of these 12 non-recovered subjects, 11 participated in the 6-month follow-up, 10 completed RHFUQ.
Recovered and non-recovered patients did not differ with respect to age, sex, weight, height, body mass index, marital status, educational status, work intensity, car speed, or estimated car damage (see Table 1).
Table 1.
Characteristics of whiplash patients.
| Initial cohort | Participant recovered after 1 year | Non-recovered participants | Statistics | ||
|---|---|---|---|---|---|
| No. | 143 | 126 | 12 | ||
| Age (y) | |||||
| Mean + SD | 35.8 ± 10.5 | 35.9 ± 10.8 | 39.1 ± 11.2 | P = .27 | t test |
| Male/Female | 68/75 | 59/67 | 6/6 | P = 1.00 | Fisher |
| Weight (kg) | 74.7 ± 16.1 | 73.8 ± 15.6 | 80.1 ± 14.9 | P = .20 | t test |
| Height (cm) | 174.3 ± 8.5 | 174.3 ± 8.1 | 170.2 ± 8.9 | P = .11 | t test |
| Marital status | |||||
| Single | 41 | 37 | 2 | P = .51 | KW |
| Married/Common law husband/wife | 102 | 89 | 10 | ||
| Highest education | |||||
| Primary school | 7 | 3 | 3 | P = .13 | KW |
| Secondary school | 22 | 20 | 2 | ||
| Practical education/Professional school | 80 | 73 | 5 | ||
| University graduate | 16 | 15 | 1 | ||
| University, uncompleted | 15 | 13 | 0 | ||
| Other | 3 | 2 | 1 N.S. | ||
| Working with raised arm | |||||
| Y/N (123 responders) | 20/103 | 17/94 | 3/6 | P = .17 | Fisher |
| Work intensity | |||||
| Mainly seated | 43 | 39 | 3 | P = .23 | KW |
| Walks some/seated | 41 | 39 | 2 | ||
| Walks around mainly | 27 | 23 | 3 | ||
| Heavy lifting | 7 | 7 | 0 | ||
| Unreported | 25 | 18 | 4 | ||
| Motor vehicle collision | |||||
| Deltaspeed (Δ km/h), Mean ± SD | 43.1 ± 1.7 | 42.5 ± 19.7 | 48.2 ± 14.6 | P = .33 | t test |
| Car damage (0-100%) | 44.6 ± 3.3 | 45.8 ± 36.8 | 30.9 ± 36.5 | P = .10 | t test |
Abbreviations: Fisher: Fisher exact, 2-sided; KW, Kruskal-Wallis; t test: Student’s t test.
A comparison of RHFUQ answers in all 10 items at 1 week and 6 months post-injury between recovered and non-recovered patients (see Table 2) revealed higher total scores after 1 week (p < .023). After Bonferroni correction, 4 of 10 items (3, 5, 6, 7) were not different. After 6 months 10 of 10 items were different, most affected activities in the non-recovered group were ability to maintain previous work load/standard, performance of routine domestic activities and participate in conversation with 2 or more persons, and finding work more tiring.
Table 2.
Rivermead Head Injury Follow-Up Questionnaire comparison of RHFUQ scores at 1 week and 6 months after a whiplash injury based on 1-year recovery.
| Recovered n = 126 Mean ± SD |
One week Non-recovered n = 12 Mean ± SD |
KW | Recovered n = 102 Mean ± SD |
6 Months Non-recovered n = 10 Mean ± SD |
KW | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Ability to participate in conversation with 1 person | 0.2 | 0.6 | 1.3 | 1.1 | .0001 | 0.2 | 0.6 | 1.4 | 1.2 | .0001 |
| 2. Ability to participate in conversation with 2 or more | 0.3 | 0.7 | 1.5 | 1.6 | .0005 | 0.4 | 0.9 | 2.3 | 1.6 | .0001 |
| 3. Performance of routine domestic activities | 0.8 | 1.0 | 1.8 | 1.6 | .016 | 0.6 | 1.0 | 2.5 | 1.6 | .0001 |
| 4. Ability to participate in previous social activities | 0.7 | 1.1 | 1.7 | 1.3 | .007 | 0.5 | 1.0 | 2.2 | 1.5 | .0001 |
| 5. Ability to enjoy previous leisure activities | 1.2 | 1.4 | 1.6 | 1.7 | .61 | 0.7 | 1.2 | 2.4 | 1.9 | .0024 |
| 6. Ability to maintain your previous work load/standard | 1.3 | 1.4 | 2.3 | 1.7 | .060 | 1.0 | 1.3 | 3.3 | 1.3 | .0001 |
| 7. Finding work more tiring | 1.3 | 1.4 | 2.4 | 1.4 | .0134 | 0.9 | 1.2 | 2.9 | 1.3 | .0001 |
| 8. Relationship with previous friends | 0.2 | 0.6 | 0.8 | 1.1 | .0071 | 0.2 | 0.5 | 1.9 | 1.6 | .0001 |
| 9. Relationship with your partner | 0.2 | 0.5 | 1.1 | 1.2 | .0001 | 0.2 | 0.6 | 1.4 | 1.4 | .0001 |
| 10. Ability to cope with family demands | 0.5 | 0.9 | 1.8 | 1.6 | .0004 | 0.4 | 0.8 | 1.9 | 1.4 | .0001 |
| Total sum | 6.8 | 7.3 | 16.2 | 11.2 | .023 | 5.0 | 7.1 | 22.2 | 11.3 | .0001 |
Abbreviation: KW, Kruskal-Wallis (*P < .05, **P < .01, ***P < .001).
Scoring from 0 to 4: 0 = No change—I’m that same as before the injury. 1 = No recent change but still more difficult than before injury. 2 = A mild change in my ability compared to before injury. 3 = A moderate change in my ability compared to before injury. 4 = A very marked change in my ability compared to before injury.
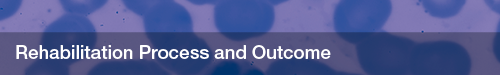
Receiver-operating characteristics of RHFUQ total score after 1 week used to predict 1-year work disability revealed an ROC area of 0.76 (95% CI: 0.61; 0.92) and with a cut-off of 10 points (score from 0 to 40) a sensitivity of 75% and a specificity of 67.2% was yielded (Figure 1).
Figure 1.
Rivermead Head Injury Follow-Up Questionnaire and 1-year recovery.
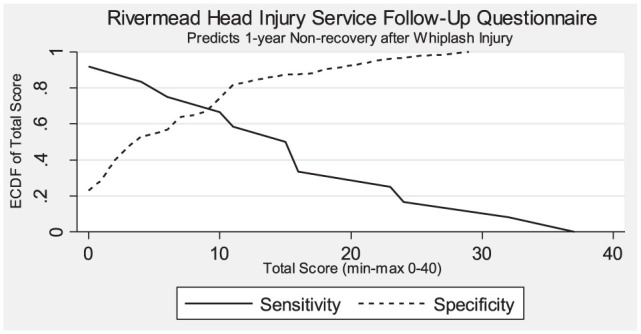
The non-recovered reported, early after injury, significantly higher intensities of neck pain, headache, shoulder-arm pain, and lower back pain as well as global pain (Figure 2).
Figure 2.
Average pain 1 week after whiplash injury.
*P < .05, **P < .001 (Kruskal-Wallis).
To assess symptoms known to be associated with concussion, we also examined the initial frequencies of headache, dizziness, fatigue, irritability, anxiety, insomnia, concentration loss, tinnitus, blurred vision, and noise sensitivity. As shown in Figure 3, marked difference in response is shown in the group that did not recover regarding irritability, insomnia, and concentration loss.
Figure 3.
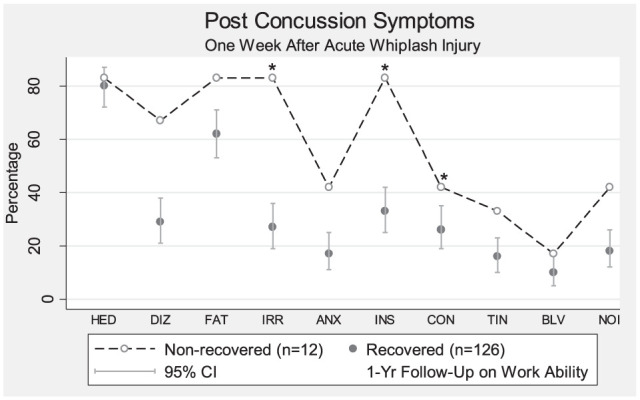
Post concussion symptoms.
ANX indicates anxious; BLV, blurred vision; CON, concentration problems; DIZ, dizziness; FAT, fatigue; HED, headache; INS, insomnia; IRR, irritable; NOI, noise sensitivity; TIN, tinnitus.
*P < .05 (Fisher exact test).
A multiple regression model was fitted to examine the relationship between RHFUQ (score: 0-40) and PCS symptoms (score: 0-10) and neck pain assessed by VAS (score: 0-10). Estimated relationship:
The standard deviation of the error was of 5.66 (95% CI, 5.06; 6.43)
Discussion
This prospective study finds that concussion-related symptoms and disabilities are frequently encountered after whiplash injury and shows that the RHFUQ adequately predicts 1-year work disability after whiplash injury.
Whiplash patients included in this study were not unconscious during or after whiplash injury. They did not endure direct head trauma or other associated injuries and did not report retrograde or anterograde amnesia at the time of injury. The RHFUQ 11 after 1 week detected non-recovery (ROC of 0.76, 95% CI, 0.61; 0.92). When we applied a cut-off of 10 (min. 0, max. 40), sensitivity was of 75% and specificity of 67% as a stand-alone test for 1-year work disability. The scores of all individual 10 items worsened in the non-recovered group, and, as a result, the sum score rose from 16.2 to an average of 22.2. An improvement was seen in the recovered group in RHFUQ score from 6.8 to 5.0 after 6 months.
Brain strains may develop during rear-end car collision as shown in kinematic studies. 10 We did not perform biomechanical evaluation in this study. As surrogate measures, we used patient-reported outcomes describing the whiplash injury and used their information on car damage. We found no difference in reported car speed (difference in speed between the 2 colliding cars) or car damage in recovered and non-recovered patients. Our results showed no difference in age, sex, educational status, or marital status between recovered and non-recovered patients. Our findings support previous studies of disability following acute whiplash injury, emphasizing the influence of the patients’ reaction to their injury.13-15
The RHFUQ questionnaire assessed changes in ability for different tasks after the injury by asking the patients to describe the extent to which they considered that there had been a change in some of the basic aspects of their everyday lives. One week post-injury, the non-recovered patients tended to have difficulties in coping with their partner, family, and friends. As would be anticipated, a significant impairment indicated by RHFUQ correlates positively with disability. RHFUQ scores were higher after 6 months in non-recovered whiplash patients as compared to initial scores and to the recovered group.
The items from the RHFUQ seem important for the disability found after whiplash injury. Difficulties in coping relationship and conversation after 1 week and scoring marked changes in the aspects of everyday life 6 months post-injury, suggesting that long-term disability after whiplash may be the result of other factors than the collision trauma.16-18 Significant differences between the recovered and non-recovered whiplash patients reflected by the RHFUQ demonstrate the importance of bio-psycho-social aspects of developing long-term disability after acute whiplash injury. 19 RHFUQ scores in mild traumatic brain injuries in a Swedish study were similar to our findings in whiplash-injured patients. 20
The simplicity of the items in the RHFUQ makes the questionnaire useful in clinical services and provides acceptable predictive value. Better tests are however available.3,13 Even so, the findings of this study suggest the appropriateness of performing causal considerations regarding the origin of symptoms ascertained in or reported by victims/injured subjects, eg, carefully considering stress-related mechanisms, neuroinflammation, genetic susceptibility, and social constructions, but also reconsidering head-neck kinematics.10,21-23
Conclusions
This study found the presence of symptoms usually reported after known brain trauma/injury in a cohort of whiplash-injured (WAD grade I-III) subjects reporting significant disabling symptoms on the so-called RHFUQ. Non-recovery was not related to patient-reported injury-related properties. The study underlines the need for a better understanding of the post-injury mechanisms pertaining to minor injuries, ie, whether they are ‘psychological’ or ‘biological’ stress/neuroinflammation, social constructions, or of unknown (micro-) biological origin. This should be investigated.
Footnotes
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: HK conceived and designed the work, acquired data and interpreted results, drafted and revised the manuscript and approved the final version and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. LJ acquired data and interpreted results and drafted and revised the manuscript and approved the final version and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
ORCID iD: Helge Kasch  https://orcid.org/0000-0002-9302-4946
https://orcid.org/0000-0002-9302-4946
References
- 1. Walton DM, Carroll LJ, Kasch H, et al. An overview of systematic reviews on prognostic factors in neck pain: results from the International Collaboration on Neck Pain (ICON) Project. Open Orthop J. 2013;7:494–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Spitzer WO, Skovron ML, Salmi LR, et al. Scientific monograph of the Quebec Task Force on Whiplash-Associated Disorders: redefining ‘whiplash’ and its management. Spine (Phila Pa 1976). 1976;1995;20:1S-73S. [PubMed] [Google Scholar]
- 3. Kasch H, Kongsted A, Qerama E, Bach FW, Bendix T, Jensen TS. A new stratified risk assessment tool for whiplash injuries developed from a prospective observational study. BMJ Open. 2013;3:e002050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kasch H, Qerama E, Kongsted A, Bendix Jensen TS, Bach FW. Clinical assessment of prognostic factors for long-term pain and handicap after whiplash injury: a 1-year prospective study. Eur J Neurol. 2008;15:1222–1230. [DOI] [PubMed] [Google Scholar]
- 5. Barnsley L, Lord S, Bogduk N. Whiplash injury. Pain. 1994;58:283–307. [DOI] [PubMed] [Google Scholar]
- 6. Sterling M, Carroll LJ, Kasch H, Kamper SJ, Stemper B. Prognosis after whiplash injury. Spine (Phila Pa 1976). 2011;36:S330–S334. [DOI] [PubMed] [Google Scholar]
- 7. Cassidy JD, Carroll L, Cote P, Holm L, Nygren A. Mild traumatic brain injury after traffic collisions: a population-based inception cohort study. J Rehabil Med. 2004;43:15–21. [DOI] [PubMed] [Google Scholar]
- 8. Carroll LJ, Cassidy JD, Peloso PM, et al. Prognosis for mild traumatic brain injury: results of the WHO collaborating centre task force on mild traumatic brain injury. J Rehabil Med. 2004;43:84–105. [DOI] [PubMed] [Google Scholar]
- 9. Hoffman JM, Dikmen S, Temkin N, Bell KR. Development of posttraumatic stress disorder after mild traumatic brain injury. Arch Phys Med Rehabil. 2012;93:287–292. [DOI] [PubMed] [Google Scholar]
- 10. Elkin BS, Elliott JM, Siegmund GPJ. Whiplash injury or concussion? a possible biomechanical explanation for concussion symptoms in some individuals following a rear-end collision. Orthop Sports Phys Ther. 2016;46:874–885. [DOI] [PubMed] [Google Scholar]
- 11. Crawford S, Wenden FJ, Wade DT. The Rivermead head injury follow up questionnaire: a study of a new rating scale and measures to evaluate outcome after head injury. J Neurol Neurosurg Psychiatry. 1996;60:510–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kasch H, Bach FW, Jensen TS. Handicap after acute whiplash injury: a 1-year prospective study of risk factors. Neurology. 2001;56:1637–1643. [DOI] [PubMed] [Google Scholar]
- 13. Sterling M, Hendrikz J, Kenardy J. Similar factors predict disability and posttraumatic stress disorder trajectories after whiplash injury. Pain. 2011;152:1272. [DOI] [PubMed] [Google Scholar]
- 14. McLean SA, Ulirsch JC, Slade GD, et al. Incidence and predictors of neck and widespread pain after motor vehicle collision among US litigants and nonlitigants. Pain. 2014;155:309–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sterling M, Jull G, Vicenzino B, Kenardy J, Darnell R. Physical and psychological factors predict outcome following whiplash injury. Pain. 2005;114:141–148. [DOI] [PubMed] [Google Scholar]
- 16. Myrtveit SM, Carstensen T, Kasch H, Ornbol E, Frostholm L. Initial healthcare and coping preferences are associated with outcome 1 year after whiplash trauma: a multicentre 1-year follow-up study. BMJ Open. 2015;5:e007239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Carstensen TB, Frostholm L, Oernboel E, et al. Post-trauma ratings of pre-collision pain and psychological distress predict poor outcome following acute whiplash trauma: a 12-month follow-up study. Pain. 2008;139:248–259. [DOI] [PubMed] [Google Scholar]
- 18. Sullivan MJ, Scott W, Trost Z. Perceived injustice: a risk factor for problematic pain outcomes. Clin J Pain. 2012;28:484–488. [DOI] [PubMed] [Google Scholar]
- 19. Kasch H, Turk DC, Jensen TS, Kasch H. Whiplash Injury: Perspectives on the Development of Chronic Pain. Seattle, WA: IASP Press; 2016. [Google Scholar]
- 20. Stalnacke BM, Elgh E, Sojka P. One-year follow-up of mild traumatic brain injury: cognition, disability and life-satisfaction of patients seeking consultation. J Rehabil Med. 2007;39:405–411. [DOI] [PubMed] [Google Scholar]
- 21. Duffy SA, Teknos T, Taylor JM, et al. Health behaviors predict higher interleukin-6 levels among patients newly diagnosed with head and neck squamous cell carcinoma. Cancer Epidemiol Biomarkers Prev. 2013;22:374–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Diatchenko L, Nackley AG, Slade GD, et al. Catechol-O-methyltransferase gene polymorphisms are associated with multiple pain-evoking stimuli. Pain. 2006;125:216–224. [DOI] [PubMed] [Google Scholar]
- 23. Schaible HG, Grubb BD. Afferent and spinal mechanisms of joint pain. Pain. 1993;55:5–54. [DOI] [PubMed] [Google Scholar]