Short abstract
The B2 glenoid is defined by Walch et al. as a glenoid that is biconcave with posterior erosion accompanied by posterior humeral head subluxation. This creates unique challenges for the treating orthopedic surgeon. Bone loss, excessive retroversion, and posterior subluxation make anatomic shoulder arthroplasty in this setting fraught with increased complications, including instability, glenoid component loosening, and poor clinical outcomes. Many techniques have been devised to treat the arthritic shoulder with a B2 glenoid, including hemiarthroplasty, total shoulder arthroplasty using eccentric reaming, bone grafting and custom implantation, and reverse total shoulder arthroplasty. In this review, we will focus on anatomic total shoulder arthroplasty using augmented glenoid implants to treat the B2 glenoid. Indications, clinical results, and basic science analyses of augmented anatomic glenoids are also discussed.
Keywords: Arthritis, arthroplasty, osteoarthritis, prosthesis, replacement, shoulder
Introduction
Glenohumeral osteoarthritis is a common cause of shoulder pain and disability for which total shoulder arthroplasty is an effective surgical intervention.1–5 Glenohumeral osteoarthritis is a complex process, involving changes in joint version, morphology, and stability. Friedman et al. utilized computerized tomography to study version in osteoarthritis and found that shoulders with severe osteoarthritis had significantly more glenoid retroversion than asymptomatic controls. 6 Rouleau et al. expanded upon the findings of Friedman et al., finding that combining the Friedman method for measuring version with measuring the intermediate glenoid line—the line connecting the anterior and posterior glenoid edges—was the most reliable method of measuring version specifically in those glenoids that had a neoglenoid—an eroded glenoid surface—and a paleoglenoid—a native glenoid surface.7,8 The Walch Classification is a commonly utilized system based on the mid-glenoid axial computerized tomography slice for describing the glenoid morphology in commonly occurring wear patterns. 9 This classification scheme not only builds on the work of Friedman et al. in determining glenoid version but also takes into account wear patterns, morphology, and humeral head subluxation.6,9
In the Walch classification, a type B glenoid is characterized by a humeral head that is posteriorly subluxated. The type B2 glenoid, which constitutes between 15% and 44% of glenoids, is defined by a retroverted glenoid that is biconcave with posterior erosion.9,10 Longitudinal studies confirm that the posterior subluxation predates the posterior erosion. 11 Although premorbid retroversion appears to have been ruled out as a potential cause of subluxation, the true cause remains elusive with theories ranging from infraspinatus atrophy,12,13 to scapular position, 14 to a tight anterior capsule. 15
Treatment Options
There are a variety of different treatment approaches to handle the unique challenges presented by the B2 glenoid. Each has its own unique benefits and drawbacks. Hemiarthroplasty is one surgical approach which does not include a glenoid component, often utilized in younger patients. However, outcomes correlate significantly with the status of glenoid wear and patients with posterior glenoid erosion have the worst results. 16 There is also concern for continued glenoid erosion, which may limit postoperative outcomes, particularly in younger patients. 17 The “ream-and-run” procedure in which the glenoid is prepared to create a concentric surface also has had inconsistent results.10,18–20 Of particular concern with hemiarthroplasty is that revision to total shoulder arthroplasty may be necessary, and evidence shows that pain relief and improvements in function are not as robust as when total shoulder arthroplasty is performed as a primary procedure.20–22
Asymmetric reaming is a technique in which the “high side” of the anterior glenoid is reamed to correct glenoid retroversion and recenter the humeral head prior to resurfacing the glenoid with an implant. 23 Clinical outcomes of total shoulder arthroplasty using this technique have been mixed.24–27 Cadaveric and simulation studies have shown that there are limitations to the amount of retroversion that asymmetric reaming can correct. Reaming to correct more than 15° of retroversion compromises the anterior bone stock, leading to complications such as peg penetration through the glenoid vault, glenoid fracture, and necessitating a smaller glenoid implant which has implications for shoulder stability.28–32 Clinically, more aggressive reaming is associated with increased glenoid migration and radiographic loosening. 33
In cases in which retroversion is too severe to be solved by assymetric reaming alone, bone grafting is often employed. Clinical studies have had mixed results.26,34–38 Bone grafting presents its own set of unique complications, including graft resorption, loss of fixation, migration, and nonunion.39,40
Inset glenoids have grown in popularity for the B2 glenoid, buoyed by the belief that the implant may be left in some degree of retroversion and still have resistance to shear forces due to the inset nature. Although clinical results thus far have been limited, the presented patients have had excellent outcomes. 41
Reverse total shoulder arthoplasty (RTSA) has offered promising results for osteoarthritis with a B2 glenoid because the constrained prothesis addresses the posterior instability associated with the subluxated humeral head.42,43 However, it does not completely eliminate the need for asymmetric reaming or bone grafting. In addition, there is concern about the longevity of the reverse total arthroplasty, particularly in younger patients.44–46 For example, in a study by Mizuno et al. of patients undergoing reverse total shoulder arthroplasty for primary osteoarthritis, results were positive, with significant improvements in postoperative range of motion and patient-reported outcomes, with complications occurring in 4 of 27 patients, resulting in only 1 revision. However, the average patient age was 74 years (range, 66–82 years), driving home the point that while RTSA may be an excellent option for elderly patients, these data cannot be extrapolated to the younger and potentially more active patient population who frequently present with a B2 glenoid erosion pattern. 43
Anatomic Total Shoulder Arthroplasty With Glenoid Augments
Glenoid augmentation is an attractive option in total shoulder arthroplasty for the B2 glenoid. It is able to correct retroversion without the complications of other techniques, such as loss of bone stock, that is caused by excessing reaming. There is less medialization of the joint line when using augments and thus important biomechanical length–tension relationships are persevered for optimal muscle functioning and joint stability. As a construct, it is biomechanically sturdier than those relying on bone grafting in which large bone grafts are subject to complications associated with graft preparation, fixation, and graft incorporation.8,26,35,36
Historical Review of Augmented Glenoid Implant Designs
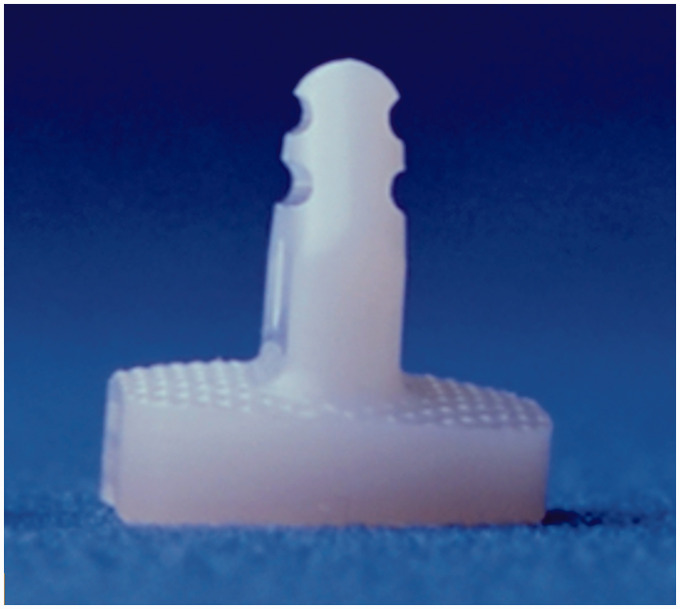
Early results using glenoid augments had disappointing outcomes, resulting in the earliest models being discontinued and no longer available for clinical use. The Cofield 2 (Smith and Nephew, Inc, Memphis, TN) (Figure 1) is a keeled, asymmetric polyethylene component available for commercial use from 1995 to 1999. Rice et al. studied 14 consecutive shoulders treated with the Cofield 2 for a minimum of 2 years. At follow-up, there were 5 excellent, 7 satisfactory, and 2 unsatisfactory results due to moderate pain. At postoperative radiographic assessment, 4 shoulders had more than mild subluxation of the humeral head, 3 had moderate posterior subluxation, and 1 had severe anterior subluxation. There was grade 1 periprosthetic lucency in 7 shoulders and grade 5 lucency in 1 shoulder, with the component having shifted in position. There were no revision surgeries at the time of follow-up. 47 The Cofield 2 offered minimal correction of retroversion of only 4° and was associated with a high rate of revision. It was subsequently pulled from the market as a result of high rates of persistent instability and minimal clinical utility due to the minimal correction. 48
Figure 1.
The Cofield 2 glenoid augment (Smith and Nephew, Inc, Memphis, TN). Image courtesy of Grant E. Garrigues, MD.
The concerning finding about persistent instability was repeated in a study by Cil et al. They reviewed 38 patients undergoing primary or revision total shoulder arthroplasty using 1 of 3 nonstandard glenoid components, an angled keel, an extra thick, or an augmented metal back, with a minimum of 2-year follow-up. Moreover, 14 glenoids were classified as B2. All of the nonstandard glenoid components were Cofield glenoid components. There was a significant improvement in pain and range of motion. The average American Shoulder and Elbow Surgeons (ASES) score was 55 points. There were 11 excellent results, 11 shoulders had satisfactory results, and 16 shoulders had unsatisfactory results, of which 10 shoulders required revision surgery. Of the 10 clinical failures, 3 (21%) occurred in type B2 glenoids: 2 of these were due to persistent posterior dislocation and 1 due to infection. At postoperative follow-up, 8 shoulders had no or mild subluxation and 11 had moderate to severe subluxation. Significantly, 5 patients had newly developed subluxation in the postoperative period. The estimated survival rate for radiographic glenoid loosening was 97% at 2 years, 93% at 5 years, and 79% at 10 years. By far, the posteriorly augmented, metal-backed glenoid fared the worst with a 10-year survival of only 31%, which, of the glenoid components utilized in the study, is the type of augment specifically designed to address the challenges of the B2 glenoid. 49
Outside of the commonly used, commercially available glenoid augments, case series have reported success utilizing augments from less frequently applied technology. Sandow and Schultz followed 10 patients with a minimum of 2-year follow-up, who underwent total shoulder arthroplasty utilizing trabecular metal wedged augments (Zimmer, Warsaw, IN), which have proven to be successful to treat bone loss in the hip and knee. Moreover, 4 patients had B2 glenoids, and 6 patients had type C glenoids. There were no major complications in any patient, nor any need for revision surgery. All patients had correction of retroversion and posterior humeral subluxation. All patients had significant improvement in postoperative pain scores, Oxford Shoulder Scores, and ASES scores. This study supports wedge-shaped trabecular metal augments as a viable technique as part of total shoulder arthroplasty in the B2 glenoid, which is an appealing option due to its ability to consistently achieve bony in-growth. 50
Currently Available Augmented Glenoid Implant Designs
There are 3 commonly used glenoid augments that are currently commercially available for the B2 glenoid in the U.S. market. These devices all differ from the Cofield device in that the correction is achieved through geometry which, with a stepped, wedged, or hemi-wedged design, occurs on the bony side and not the articular side. This allows for a more profound correction while still maintaining the stability of the construct, by allowing the pegs or keel to remain firmly in the glenoid vault. Despite their early failures, more recent clinical studies have demonstrated that glenoid augments are an effective technique to treat the challenges of the B2 glenoid.
The Step-Tech (DePuy Orthopaedics, Warsaw, IN) (Figure 2) is used to correct retroversion, provide a stable fixation of the glenoid implant, and recreate the original glenohumeral joint line. It has a dual-surface design with various heights of the posterior step of 3 mm, 5 mm, or 7 mm to enact various degrees of correction. Favorito et al. studied 20 shoulders with osteoarthritis with posterior glenoid bone loss treated with total shoulder arthroplasty using the Step-Tech glenoid augment that had at least 2-year follow-up. There was significant improvement in visual analog scale (VAS) scores, Western Ontario Osteoarthritis of the Shoulder index, the physical component summary score of the Short Form-36, forward flexion, and external rotation. In addition, 1 shoulder showed osteolysis, 6 shoulders showed bone adjacent to the central-peg flange without osseous integration, and the remaining 12 demonstrated central-peg flange osseous integration. The average Lazarus lucency score was .53 with all shoulders having a perfect grade A seating score. Two postoperative complications consisted of instability events—1 anterior and 1 posterior dislocation, both necessitating revision surgery. 51
Figure 2.
The Step-Tech glenoid augment (DePuy Orthopaedics, Warsaw, IN). Image courtesy of Grant E. Garrigues, MD.
Stevens et al. found similar results in a study of 21 patients with B2 or C glenoid morphology treated with total shoulder arthroplasty using the Step-Tech glenoid augment. There was significant improvement in range of motion, VAS pain scores, ASES scores, and Simple Shoulder Test scores. There was radiographic improvement in postoperative glenoid version, humeral scapular alignment, and humeral glenoid alignment. Postoperatively, there were 4 cases of peg penetration; 1 of which involved the central peg. There were 4 grade 1 radiolucencies and 1 grade 2 radiolucencies surrounding the glenoid, which did not show signs of progression throughout the course of follow-up. In 19 patients, component seating was grade A, with grade 3 radiodensity surrounding the central flange. There were no major complications, nor any need for revision surgery. 52
These findings were corroborated by Ho et al., who studied 71 shoulders with B2 or B3 glenoid morphology who underwent total shoulder arthroplasty using the Step-Tech glenoid augment with a minimum of 2-year follow-up. Postoperatively, Penn Shoulder Scores (PSS), range of motion, humeral head centering, and glenoid version were significantly improved. Moreover, 10% of patients had persistent posterior subluxation on postoperative imaging. In addition, 15% of patients had central-peg osteolysis, 24% had bone growth to the edges of the flange of the central peg, and 63% had bone growth within the flange of the central peg. Higher PSS were associated with less preoperative retroversion, less preoperative humeral subluxation, and better preoperative range of motion. Patients who had postoperative posterior subluxation had higher preoperative retroversion and more commonly had grade 2 or higher fatty infiltration of the teres minor. Thus, a stepped augment design offered satisfactory results in the majority of patients undergoing total shoulder arthroplasty, though those who presented preoperatively with more severe deformities were more likely to have suboptimal outcomes, such as lower clinical outcome scores, persistent instability, and osteolysis.
The Equinoxe (Exactech, Gainesville, FL) (Figure 3) is a wedge-shaped device used to treat posterior wear. They are available in multiple sizes from small to extra-large to correct defects of 8° and 16° of retroversion. A product to correct 12° of retroversion was recently discontinued. Only one study has published clinical results on this implant, with positive results. Wright et al. studied a population of 24 patients who were treated for shoulder osteoarthritis with posterior wear using total shoulder arthroplasty utilizing the Equinoxe posterior augmented glenoid with a minimum of 2-year follow-up. They were then age, sex, and follow-up matched to a group of patients without posterior glenoid erosion who were treated using total shoulder arthroplasty with an all-polyethylene nonaugmented glenoid. All patients demonstrated significant improvement in pain and function. There were no surgical complications in either group. Moreover, 60% of the patients treated with the posterior augmented glenoid had a radiolucent line with an average radiographic line score of 1.10. One glenoid was considered radiographically, but not clinically, loose. On the Grashey view, 2 humeral heads had superior subluxation, while on the axillary lateral, 3 humeral heads were anteriorly subluxated. There were no posterior subluxations. In addition, 33% of the patients treated with a nonaugmented glenoid had a radiolucent line with an average radiographic line score of 0.438. Unlike the poor results using nonaugmented glenoids to treat posterior glenoid erosion,26,27 the Equinoxe performed as well clinically in the difficult patient population of posterior glenoid erosion as the control group. 53
Figure 3.
The Equinoxe glenoid augment (Exactech, Gainesville, FL). Image courtesy of Grant E. Garrigues, MD.
The Aequalis Perform + (Tornier/Wright Medical Group, Memphis, TN) (Figure 4) is a glenoid augment that treats asymmetric glenoid wear through its biconvex design. It consists of small, medium, large, and extra-large sizes and has wedge angles of 15°, 25°, and 35°. Clinical outcomes of a multicenter study are currently being analyzed. Although final results are not yet available, the overall impression is favorable.
Figure 4.
Forty-eight year old motocross racer with severe osteoarthritis with B2 glenoid morphology treated with anatomic total shoulder arthroplasty with Perform + glenoid augment (Tornier/Wright Medical, Memphis, TN). Image courtesy of Grant E. Garrigues, MD.
Basic Science Studies on Augmented Anatomic Glenoid Implants
Bone loss
Glenoid augmentation offers an advantage in treating B2 glenoids because it preserves valuable bone stock, particularly when compared to asymmetrical reaming. Preservation of the structurally robust subarticular bone in anatomic arthroplasty has been correlated with improved implant longevity, as the primary failure mode for glenoid implants is subsidence into the glenoid vault. 33 Multiple finite element analyses demonstrate that wedged augments remove less bone than stepped augments and asymmetric reaming.54–57 In a finite element analysis (FEA) by Knowles et al., the hemi-wedged Aequalis Perform + removed less bone for implantation than the full-wedged Equinoxe at 0° of retroversion, but there was no significant difference between the 2 implants at 10° of retroversion. 55 There were variable results as to whether stepped augments or standard components removed less bone, with the majority opinion being that standard components implanted through asymmetric reaming removes the most bone, followed by stepped implants, with standard components implanted in neutral removing the least amount bone.56,57 Conversely, for larger defects, Roche et al. found that stepped components remove more bone than asymmetric reaming. 54
These results are consistent with findings that correlate with loss of bone stock. Because wedged augments preserve the most bone the remaining bone is of higher quality, which is an important consideration for implantation. Compared to the stepped design, the bone remaining within the posterior half of the glenoid was significantly denser when using the Aequalis Perform+. 55 Therefore, the wedge-shaped augments had the most cortical support. 57 Indeed, for the standard nonaugmented design, more of the implant was supported by cancellous bone at 18.2%, followed by the stepped design at 8.8%, and 4.3% with the wedged design. In addition, the maximum depth of bone removed for the wedged design was also significantly less than the stepped design and the standard design. 56 Thus, multiple studies have replicated the findings that wedge-shaped and hemi-wedged glenoid designs are most effective at removing the least amount of bone and preserving high-quality bone in which to implant the glenoid component.
Medialization
Medialization of the glenohumeral joint line that occurs due to joint wear and erosion can be iatrogenically exacerbated by reaming as part of total shoulder arthroplasty. Medialization has important implications for the length–tension relationships of muscles that allow them to function optimally and for maintaining joint stability. Removing more bone will further medialize the joint line. An FEA by Roche et al. of 3 different size glenoid defects demonstrated muscle shortening of the rotator cuff and teres major that occurred with each defect, with larger defects causing more shortening and more medialization of the humerus. Eccentric reaming resulted in more medialization and rotator muscle shortening of the humerus compared to the wedged posterior augment. Because it required additional bone to implant the stepped posterior augment, it is unsurprising that the stepped augment resulted in slight medialization and additional muscle shortening compared to the wedged posterior augment. 54 Thus, there is a direct correlation between bone loss and medialization, with wedge-shaped augments being most effective at both resisting medialization and removing less bone.
In addition to bone loss, medialization has an intimate relationship to retroversion. Sabesan et al. performed an FEA on 29 shoulders undergoing total shoulder arthroplasty, as they investigated medialization as a function of retroversion. The use of the stepped Step-Tech augmented glenoid component resulted in less medialization of the joint line than when a standard glenoid component was used at both neutral and 6° of retroversion. The severity of glenoid retroversion was correlated with the amount of glenoid bone loss. In addition, there was a significant relationship between the amount of medialization and the severity of the retroversion. With the stepped augmented glenoid component, there existed an increased ability to correct retroversion with less medialization, likely due to the decreased need to remove bone in order to implant the component. In this study, there were 4 cases of central-peg perforation with the standard glenoid component and 1 case of central-peg perforation with the stepped augmented component, due to the increased medialization seen with the nonaugmented design. This study echoes prior studies about the importance of correcting glenoid retroversion and advances the stepped glenoid augment design as an effective way to treat this problem. 58
Implant Stability
A number of studies have evaluated the stability of glenoid augments, either as a comparison of various implants or against other techniques.57,59–64 In 2012, Kirane et al. established the potential for glenoid augments in their cadaver study of 2 novel prototypes. They found that there were not significant differences in the loading-induced peri-glenoid strain between a traditional total shoulder arthroplasty in shoulders without bony defects and the total shoulder arthroplasty performed with a polyethylene step block performed in shoulders with a biconcave posterior bony deficit, while strain was higher in a model with titanium step blocks. 59 This paved the way for other studies to examine glenoid augments using current clinical models.
By correcting glenoid retroversion, glenoid augmentation may theoretically improve implant longevity by lowering the risk of early loosening by decreasing edge loading, eccentric loading, and shear and tensile stresses at the bone–implant, cement–implant, and cement–bone interfaces. An FEA by Hermida et al. established wedge-shaped augments as a viable tool to correct retroversion. Wedge-shaped glenoid components dissipated compressive stress and predicted greater cyclic fatigue life by correcting retroversion. Cement volume survival followed similar trends, with lower stresses generated in the scapulae with neutral alignment and in those implanted with the wedge component, predicting a longer survival for those components than those implanted in retroversion. This study argues for the importance of correcting retroversion while performing total shoulder arthroplasty because of the high magnitude of stresses that are placed on the glenoid components and the surrounding bone when significant retroversion is left uncorrected. In their model, a wedge-shaped glenoid augment is an effective technique for tackling the challenge of retroversion that is encountered in the B2 glenoid, which has important implications for implant stability, as high stresses are a harbinger for implant loosening. 60
One advantage of glenoid augments is that they offer superior biomechanical stability in addressing the challenges of posterior erosion and glenohumeral instability associated with the B2 glenoid compared with bone grafting that is subject to nonunion and bone resorption. However, there is some concern for stresses generated in augmented implants compared to asymmetric reaming. Iannotti et al. studied 5 different glenoid designs in a biomechanical study in which the glenoid augments were eccentrically loaded and cycled, while the anterior glenoid liftoff was measured throughout testing under 2 conditions to stimulate both initial and long-term fixation. For both conditions, the stepped glenoid had significantly lower lift-off values at both initial and final measurements when compared to specific other designs at various points of testing. For the final fixation simulation, all augmented designs had a higher lift-off values than nonaugmented designs with the exception of the stepped glenoid design, which had lower lift-off value, but this was not a significant difference. Thus, the findings of this study demonstrate that the glenoid augments tested in this study are at higher risk for loss of fixation and glenoid loosening because they were less resistant to liftoff. The exception to this was the stepped glenoid design, which was built to resemble the Step-Tech glenoid augment, as it was the only augmented design that did not have a higher lift-off value than the nonaugmented device in the setup designed to simulate long-term fixation. 61
Joint stability and implant fixation were assessed in an FEA by Sabesan et al. under conditions of 2 different glenohumeral radial mismatches in which the stepped Step-Tech augment was compared to the wedged Equinoxe. The stepped model showed higher levels of shear stress at both radial mismatch settings at the backside of the implant and in the cement mantle. Thus, while both designs performed similarly, the stepped design had high levels of stress, which indicates a higher risk for loosening, and higher amounts of micromotion in high-risk conditions, which is an important consideration in the B2 glenoid in which persistent instability is not an infrequent cause of failure. 63
Multiple studies have investigated implant stability and sought to compare glenoid augmentation with asymmetric reaming. 57 Preparing the glenoid for implantation of a component induces strain that puts surrounding bone at risk. According to Allred et al., asymmetrically reamed bone generated strain levels that put the largest volume of bone at risk of damage, whereas the strain levels associated with the wedged augment put the smallest volume of bone at risk of damage. 57 Conversely, Wang et al. demonstrated greater stability as measured by implant edge displacement in standard, nonaugmented glenoid components implanted through asymmetric reaming, as opposed to the posterior wedged Equinoxe glenoid augments in a biomechanical study using synthetic scapulae. 62 Similar findings were corroborated by Sowa et al. in which asymmetric reaming was found to be a more stable construct in synthetic scapulae made to resemble B2 morphology, as measured by the amount of micromotion, as compared to the hemi-wedged Aequelis Perform +. 64 Thus, while glenoid augmentation appears to have many advantages over asymmetric reaming in terms of bone preservation and resistance to medialization, the biomechanically stability of the implant appears to be an area of continued debate and investigation.
Conclusion
The B2 glenoid is a challenging problem for the orthopedic surgeon in treating a patient with osteoarthritis. Posterior bone loss, retroversion, and instability are all problems that must be addressed at the time of surgery. Currently, there are a variety of surgical techniques available to address these challenges, including hemiarthroplasty, total shoulder arthroplasty with eccentric reaming, bone grafting and custom implantation, and reverse total arthroplasty. All of these options have their own unique drawbacks. The use of glenoid augments has numerous advantages, including correcting retroversion while preserving bone stock, resisting medialization of the joint line, and offering a biomechanically stable construct. Numerous clinical studies and basic science studies offer promising results about their clinical utility and their ability to address the problems associated with B2 glenoid. Further studies are needed to compare the clinical outcomes of the different designs directly to one another and to specify the situations in which certain designs might be uniquely indicated. Neither ethics approval nor patient consent was required for this review.
Declaration of Conflicting Interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr. Garrigues is a paid consultant for Wright Medical/Tornier, DJO/Encore.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by research and educational funding from Arthrex, Smith and Nephew, and Breg.
References
- 1. Izquierdo R, Voloshin I, Edwards S, et al. Treatment of glenohumeral osteoarthritis. J Am Acad Orthop Surg. 2010; 18(6):375–382. [DOI] [PubMed] [Google Scholar]
- 2.Lo IK, Litchfield RB, Griffin S, Faber K, Patterson SD, Kirkley A. Quality-of-life outcome following hemiarthroplasty or total shoulder arthroplasty in patients with osteoarthritis: a prospective, randomized trial. J Bone Joint Surg Am. 2005; 87(10):2178–2185. [DOI] [PubMed] [Google Scholar]
- 3.Norris TR, Iannotti JP. Functional outcome after shoulder arthroplasty for primary osteoarthritis: a multicenter study. J Shoulder Elb Surg. 2002; 11(2):130–135. [DOI] [PubMed] [Google Scholar]
- 4.Singh JA, Sperling JW, Cofield RH. Revision surgery following total shoulder arthroplasty: analysis of 2588 shoulders over three decades (1976 to 2008). Bone Joint J. 2011; 93(11):1513–1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Godenèche A, Boileau P, Favard L, et al. Prosthetic replacement in the treatment of osteoarthritis of the shoulder: early results of 208 cases. J Shoulder Elb Surg. 2002; 11(1):11–18. [DOI] [PubMed] [Google Scholar]
- 6.Friedman RJ, Hawthorne KB, Genez BM. The use of computerized tomography in the measurement of glenoid version. J Bone Joint Surg Am. 1992; 74(7):1032–1037. [PubMed] [Google Scholar]
- 7.Rouleau DM, Kidder JF, Pons-Villanueva J, Dynamidis S, Defranco M, Walch G. Glenoid version: how to measure it? Validity of different methods in two-dimensional computed tomography scans. J Shoulder Elb Surg. 2010; 19(8):1230–1237. [DOI] [PubMed] [Google Scholar]
- 8.Hendel MD, Werner BC, Camp CL, et al. Management of the biconcave (B2) glenoid in shoulder arthroplasty: technical considerations. Am J Orthop (Belle Mead NJ). 2016; 45(4):220–227. [PubMed] [Google Scholar]
- 9.Walch G, Badet R, Boulahia A, Khoury A. Morphologic study of the glenoid in primary glenohumeral osteoarthritis. J Arthroplasty. 1999; 14(6):756–760. [DOI] [PubMed] [Google Scholar]
- 10.Somerson JS, Neradilek MB, Service BC, Hsu JE, Russ SM, Matsen FA. Clinical and radiographic outcomes of the ream-and-run procedure for primary glenohumeral arthritis. J Bone Joint Surg Am. 2017; 99(15):1291–1304. [DOI] [PubMed] [Google Scholar]
- 11.Walch G, Ascani C, Boulahia A, Nové-Josserand L, Edwards TB. Static posterior subluxation of the humeral head: an unrecognized entity responsible for glenohumeral osteoarthritis in the young adult. J Shoulder Elb Surg. 2002; 11(4):309–314. [DOI] [PubMed] [Google Scholar]
- 12.Walker KE, Simcock XC, Jun BJ, Iannotti JP, Ricchetti ET. Progression of glenoid morphology in glenohumeral osteoarthritis. J Bone Joint Surg Am. 2018; 100(1):49–56. [DOI] [PubMed] [Google Scholar]
- 13.Donohue KW, Ricchetti ET, Ho JC, Iannotti JP. The association between rotator cuff muscle fatty infiltration and glenoid morphology in glenohumeral osteoarthritis. J Bone Joint Surg Am. 2018; 100(5):381–387. [DOI] [PubMed] [Google Scholar]
- 14.Sabesan VJ, Callanan M, IYouderian A, Iannotti JP. 3D CT assessment of the relationship between humeral head alignment and glenoid retroversion in glenohumeral osteoarthritis. J Bone Joint Surg Am. 2014; 96(8):e64. [DOI] [PubMed] [Google Scholar]
- 15.Chainani A, Matson A, Chainani ML, Colon AJM, Toth AP, Garrigues GE, Little D. Synovitis, Fibrosis, and Transient Receptor Potential Channel Upregulation in the Anterior Shoulder Joint Capsule of Total Shoulder Arthroplasty Patients. Poster Presentation and Abstract #1102 at Orthopaedic Research Society; 2019; Austin, TX. [Google Scholar]
- 16.Levine WN, Djurasovic M, Glasson JM, Pollock RG, Flatow EL, Bigliani LU. Hemiarthroplasty for glenohumeral osteoarthritis: results correlated to degree of glenoid wear. J Shoulder Elbow Surg. 1997; 6(5):449–454. [DOI] [PubMed] [Google Scholar]
- 17.Franta AK, Lenters TR, Mounce D, Neradilek B, Matsen FA. The complex characteristics of 282 unsatisfactory shoulder arthroplasties. J Shoulder Elb Surg. 2007; 16(5):555–562. [DOI] [PubMed] [Google Scholar]
- 18.Gilmer BB, Comstock BA, Jette JL, Warme WJ, Jackins SE, Matsen FA. The prognosis for improvement in comfort and function after the ream-and-run arthroplasty for glenohumeral arthritis: an analysis of 176 consecutive cases. J Bone Joint Surg Am. 2012; 94(14):e102. [DOI] [PubMed] [Google Scholar]
- 19.Virk MS, Thorsness RJ, Griffin JW, et al. Short-term clinical outcomes of hemiarthroplasty with concentric glenoid reaming: the ream and run procedure. Orthopedics. 2018; 41(6):e854–e860. [DOI] [PubMed] [Google Scholar]
- 20.Getz CL, Kearns KA, Padegimas EM, Johnston PS, Lazarus MD, Williams GR. Survivorship of hemiarthroplasty with concentric glenoid reaming for glenohumeral arthritis in young, active patients with a biconcave glenoid. J Am Acad Orthop Surg. 2017; 25(10):715–723. [DOI] [PubMed] [Google Scholar]
- 21.Carroll RM, Izquierdo R, Vazquez M, Blaine TA, Levine WN, Bigliani LU. Conversion of painful hemiarthroplasty to total shoulder arthroplasty: long-term results. J Shoulder Elb Surg. 2004; 13(6):599–603. [DOI] [PubMed] [Google Scholar]
- 22.Sassoon AA, Rhee PC, Schleck CD, Harmsen WS, Sperling JW, Cofield RH. Revision total shoulder arthroplasty for painful glenoid arthrosis after humeral head replacement: the nontraumatic shoulder. J Shoulder Elb Surg. 2012; 21(11):1484–1491. [DOI] [PubMed] [Google Scholar]
- 23.Hsu JE, Ricchetti ET, Huffman GR, Iannotti JP, Glaser DL. Addressing glenoid bone deficiency and asymmetric posterior erosion in shoulder arthroplasty. J Shoulder Elb Surg. 2013; 22(9):1298–1308. doi:10.1016/j.jse.2013.04.014. [DOI] [PubMed] [Google Scholar]
- 24.Orvets ND, Chamberlain AM, Patterson BM, et al. Total shoulder arthroplasty in patients with a B2 glenoid addressed with corrective reaming. J Shoulder Elb Surg. 2018; 27(6):S58–S64. [DOI] [PubMed] [Google Scholar]
- 25.Gerber C, Costouros JG, Sukthankar A, Fucentese SF. Static posterior humeral head subluxation and total shoulder arthroplasty. J Shoulder Elb Surg. 2009; 18(4):505–510. [DOI] [PubMed] [Google Scholar]
- 26.Walch G, Moraga C, Young A, Castellanos-Rosas J. Results of anatomic nonconstrained prosthesis in primary osteoarthritis with biconcave glenoid . J Shoulder Elb Surg. 2012; 21(11):1526–1533. [DOI] [PubMed] [Google Scholar]
- 27.Iannotti JP, Norris TR. Influence of preoperative factors on outcome of shoulder arthroplasty for glenohumeral osteoarthritis. J Bone Joint Surg Am. 2003; 85(2):251–258. [DOI] [PubMed] [Google Scholar]
- 28.Gillespie R, Lyons R, Lazarus M. Eccentric reaming in total shoulder arthroplasty: a cadaveric study. Orthopedics. 2009; 32(1):21. [DOI] [PubMed] [Google Scholar]
- 29.Clavert P, Millett PJ, Warner JJP. Glenoid resurfacing: what are the limits to asymmetric reaming for posterior erosion? J Shoulder Elb Surg. 2007; 16(6):843–848. [DOI] [PubMed] [Google Scholar]
- 30.Nowak DD, Bahu MJ, Gardner TR, et al. Simulation of surgical glenoid resurfacing using three-dimensional computed tomography of the arthritic glenohumeral joint: the amount of glenoid retroversion that can be corrected. J Shoulder Elb Surg. 2009; 18(5):680–688. [DOI] [PubMed] [Google Scholar]
- 31.Tammachote N, Sperling JW, Berglund LJ, Steinmann SP, Cofield RH, An KN. The effect of glenoid component size on the stability of total shoulder arthroplasty. J Shoulder Elb Surg. 2007; 16(3):S102–S106. [DOI] [PubMed] [Google Scholar]
- 32.Chen X, Reddy AS, Kontaxis A, et al. Version correction via eccentric reaming compromises remaining bone quality in B2 glenoids: a computational study. Clin Orthop Relat Res. 2017; 475(12):3090–3099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Walch G, Young AA, Melis B, Gazielly D, Loew M, Boileau P. Results of a convex-back cemented keeled glenoid component in primary osteoarthritis: multicenter study with a follow-up greater than 5 years. J Shoulder Elb Surg. 2011; 20(3):385–394. [DOI] [PubMed] [Google Scholar]
- 34.Neer CS, Morrison DS. Glenoid bone-grafting in total shoulder arthroplasty. J Bone Joint Surg Am. 1988; 70(8):1154–1162. [PubMed] [Google Scholar]
- 35.Steinmann SP, Cofield RH. Bone grafting for glenoid deficiency in total shoulder replacement. J Shoulder Elb Surg. 2000; 9(5):361–367. [DOI] [PubMed] [Google Scholar]
- 36.Hill JM, Norris TR. Long-term results of total shoulder arthroplasty following bone-grafting of the glenoid. J Bone Joint Surg Am. 2001; 83(6):877–883. [PubMed] [Google Scholar]
- 37.Sabesan V, Callanan M, Ho J, Iannotti JP. Clinical and radiographic outcomes of total shoulder arthroplasty with bone graft for osteoarthritis with severe glenoid bone loss. J Bone Joint Surg Am. 2013; 95(14):1290–1296. [DOI] [PubMed] [Google Scholar]
- 38.Nicholson GP, Cvetanovich GL, Rao AJ, O’Donnell P. Posterior glenoid bone grafting in total shoulder arthroplasty for osteoarthritis with severe posterior glenoid wear. J Shoulder Elb Surg. 2017; 26(10):1844–1853. [DOI] [PubMed] [Google Scholar]
- 39.Scalise JJ, Iannotti JP. Bone grafting severe glenoid defects in revision shoulder arthroplasty. Clin Orthop Relat Res. 2008; 466(1):139–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Iannotti JP, Frangiamore SJ. Fate of large structural allograft for treatment of severe uncontained glenoid bone deficiency. J Shoulder Elb Surg. 2012; 21(6):765–771. [DOI] [PubMed] [Google Scholar]
- 41.Gunther SB, Lynch TL. Total shoulder replacement surgery with custom glenoid implants for severe bone deficiency. J Shoulder Elb Surg. 2012; 21(5):675–684. [DOI] [PubMed] [Google Scholar]
- 42.Wall B, Nové-Josserand L, O’Connor DP, Edwards TB, Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am. 2007; 89(7):1476–1485. [DOI] [PubMed] [Google Scholar]
- 43.Mizuno N, Denard PJ, Raiss P, Walch G. Reverse total shoulder arthroplasty for primary glenohumeral osteoarthritis in patients with a biconcave glenoid. J Bone Joint Surg Am. 2013; 95(14):1297–1304. [DOI] [PubMed] [Google Scholar]
- 44.Favard L, Berhouet J, Colmar M, et al. Massive rotator cuff tears in patients younger than 65 years. What treatment options are available? Orthop Traumatol Surg Res. 2009; 95(4):19–26. [DOI] [PubMed] [Google Scholar]
- 45.Guery J, Favard L, Sirveaux F, Oudet D, Mole D, Walch G. Reverse total shoulder arthroplasty: survivorship analysis of eighty replacements followed for five to ten years. J Bone Joint Surg Am. 2006; 88(8):1742–1747. [DOI] [PubMed] [Google Scholar]
- 46.Ek ETH, Neukom L, Catanzaro S, Gerber C. Reverse total shoulder arthroplasty for massive irreparable rotator cuff tears in patients younger than 65 years old: results after five to fifteen years. J Shoulder Elb Surg. 2013; 22(9):1199–1208. doi:10.1016/j.jse.2012.11.016. [DOI] [PubMed] [Google Scholar]
- 47.Rice RS, Sperling JW, Miletti J, Schleck C, Cofield RH. Augmented glenoid component for bone deficiency in shoulder arthroplasty. Clin Orthop Relat Res. 2008; 466(3):579–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sears BW, Johnston PS, Ramsey ML, Williams GR. Glenoid bone loss in primary total shoulder arthroplasty: evaluation and management. J Am Acad Orthop Surg. 2012; 20(9):604–613. [DOI] [PubMed] [Google Scholar]
- 49.Cil A, Sperling JW, Cofield RH. Nonstandard glenoid components for bone deficiencies in shoulder arthroplasty. J Shoulder Elb Surg. 2014; 23(7):e149–e157. [DOI] [PubMed] [Google Scholar]
- 50.Sandow M, Schutz C. Total shoulder arthroplasty using trabecular metal augments to address glenoid retroversion: the preliminary result of 10 patients with minimum 2-year follow-up. J Shoulder Elb Surg. 2016; 25(4):598–607. [DOI] [PubMed] [Google Scholar]
- 51.Favorito PJ, Freed RJ, Passanise AM, Brown MJ. Total shoulder arthroplasty for glenohumeral arthritis associated with posterior glenoid bone loss: results of an all-polyethylene, posteriorly augmented glenoid component. J Shoulder Elb Surg. 2016; 25(10):1681–1689. [DOI] [PubMed] [Google Scholar]
- 52.Stephens SP, Spencer EE, Wirth MA. Radiographic results of augmented all-polyethylene glenoids in the presence of posterior glenoid bone loss during total shoulder arthroplasty. J Shoulder Elb Surg. 2017; 26(5):798–803. [DOI] [PubMed] [Google Scholar]
- 53.Wright TW, Grey SG, Roche CP, Wright L, Flurin P-H, Zuckerman JD. Preliminary results of a posterior augmented glenoid compared to an all polyethylene standard glenoid in anatomic total shoulder arthroplasty. Bull Hosp Joint Dis. 2015; 73(1):S79. [PubMed] [Google Scholar]
- 54.Roche CP, Diep P, Grey SG, Flurin PH. Biomechanical impact of posterior glenoid wear on anatomic total shoulder arthroplasty. Bull NYU Hosp Joint Dis. 2013; 71(2):S5. [PubMed] [Google Scholar]
- 55.Knowles NK, Ferreira LM, Athwal GS. Augmented glenoid component designs for type B2 erosions: a computational comparison by volume of bone removal and quality of remaining bone. J Shoulder Elb Surg. 2015; 24(8):1218–1226. [DOI] [PubMed] [Google Scholar]
- 56.Kersten AD, Flores-Hernandez C, Hoenecke HR, D’Lima DD. Posterior augmented glenoid designs preserve more bone in biconcave glenoids. J Shoulder Elb Surg. 2015; 24(7):1135–1141. [DOI] [PubMed] [Google Scholar]
- 57.Allred JJ, Flores-Hernandez C, Hoenecke HR, D’Lima DD. Posterior augmented glenoid implants require less bone removal and generate lower stresses: a finite element analysis. J Shoulder Elb Surg. 2016; 25(5):823–830. [DOI] [PubMed] [Google Scholar]
- 58.Sabesan V, Callanan M, Sharma V, Iannotti JP. Correction of acquired glenoid bone loss in osteoarthritis with a standard versus an augmented glenoid component. J Shoulder Elb Surg. 2014; 23(7):964–973. [DOI] [PubMed] [Google Scholar]
- 59.Kirane YM, Lewis GS, Sharkey NA, Armstrong AD. Mechanical characteristics of a novel posterior-step prosthesis for biconcave glenoid defects. J Shoulder Elb Surg. 2012; 21(1):105–115. [DOI] [PubMed] [Google Scholar]
- 60.Hermida JC, Flores-Hernandez C, Hoenecke HR, D’Lima DD. Augmented wedge-shaped glenoid component for the correction of glenoid retroversion: a finite element analysis. J Shoulder Elb Surg. 2014; 23(3):347–354. [DOI] [PubMed] [Google Scholar]
- 61.Iannotti JP, Lappin KE, Klotz CL, Reber EW, Swope SW. Liftoff resistance of augmented glenoid components during cyclic fatigue loading in the posterior-superior direction. J Shoulder Elb Surg. 2013; 22(11):1530–1536. [DOI] [PubMed] [Google Scholar]
- 62.Wang T, Abrams GD, Behn AW, Lindsey D, Giori N, Cheung EV. Posterior glenoid wear in total shoulder arthroplasty: eccentric anterior reaming is superior to posterior augment. Clin Orthop Relat Res. 2015; 473(12):3928–3936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sabesan VJ, Lima DJL, Whaley JD, Pathak V, Zhang L. The effect of glenohumeral radial mismatch on different augmented total shoulder arthroplasty glenoid designs: a finite element analysis. J Shoulder Elb Surg. 2019; 28(6):1146–1153. [DOI] [PubMed] [Google Scholar]
- 64.Sowa B, Bochenek M, Braun S, et al. Replacement options for the B2 glenoid in osteoarthritis of the shoulder: a biomechanical study. Arch Orthop Trauma Surg. 2018; 138(7):891–899. [DOI] [PubMed] [Google Scholar]