Short abstract
The use of reverse total shoulder arthroplasty (RSA) is becoming increasingly popular, but many biomechanical aspects are poorly understood. Particularly, the role and function of the subscapularis following RSA are unclear. Several clinical and biomechanical studies have analyzed its role in range of motion and stability. There is some evidence that the subscapularis is beneficial for stability but may reduce range of motion. This review provides an overview of the current literature, which suggests that the subscapularis may have a more important role in RSA than originally thought.
Keywords: subscapularis, reverse total shoulder arthroplasty, stability, impaired range of motion, review
Introduction
As reverse total shoulder arthroplasty (RSA) implantation becomes more popular, a deeper understanding of the relevant biomechanics is required. In this context, more attention is being focused on the role of the subscapularis. Despite its main role as an abductor and internal rotator in a native joint, the subscapularis plays an important role in postoperative function as well as stability.
The role of the subscapularis in anatomical total shoulder arthroplasty (aTSA) has already been well described. Failure of subscapularis repair in aTSA is associated with anterior instability, poor range of motion, strength, and lower outcome scores.1–10 The result, however, is not uniformly described, and some studies described favorable outcomes following tenotomy.5,9,11 The trend overall, however, has been toward developing muscle-tendon unit sparing techniques. Gerber et al.1 described a technique with a lesser tuberosity osteotomy with satisfactory healing rates, while Lapner et al.8,12 showed good outcomes using a subscapularis peel-off technique in his comparative analysis to the osteotomy. The existing data regarding postoperative musculotendinous integrity or clinical outcome to this point suggest no significant differences among the described techniques. However, healing and integrity appear to be favoring the lesser tuberosity osteotomy. 13
The RSA
The introduction of the RSA by Grammont et al. 14 marked a major milestone in the treatment of a wide range of shoulder pathologies. The inherent biomechanical effect of medialization, lowering of the humeral head, and with it, the center of rotation call into question the modified roles of the rotator cuff muscles, particularly the teres minor and the subscapularis.
Collin et al. describe a subdivision of the subscapularis into a functional superior and inferior part as an analog to the infraspinatus and teres minor.15,16 These subdivisions have altered roles in the context of RSA. Beside the major role as an internal rotator, the cranial part (above the center of rotation) supports abduction through elevation of the arm, while the lower part remains a strong adductor.
To inform best practice and treatment of the subscapularis, it is important (a) to understand the altered biomechanics of the subscapularis following RSA and to determine (b) the potential role of the subscapularis handling during RSA in subsequent problems and complications and (c) the effect of its repair on internal rotation and consequently the overall clinical outcome.
Methods
We performed Pubmed®- and Medline®-based data searches using the terms “reverse shoulder arthroplasty,” “reverse total shoulder arthroplasty,” “inverse shoulder arthroplasty,” “inverse total shoulder arthroplasty,” “shoulder arthroplasty,” and “subscapularis” with various combinations. General search terms were chosen to reduce exclusion bias. We included all articles published from January 1985 to February 2018. The articles and abstracts found were reviewed for topic relevance as well as our inclusion and exclusion criteria. Further quantitative or qualitative analysis of the data was not performed.
Studies with evidence levels between I and IV were included. All studies analyzing the role and function of the subscapularis in RSA were included. Studies not fulfilling these criteria were excluded.
Results
Biomechanics of the Subscapularis in RSA17–21
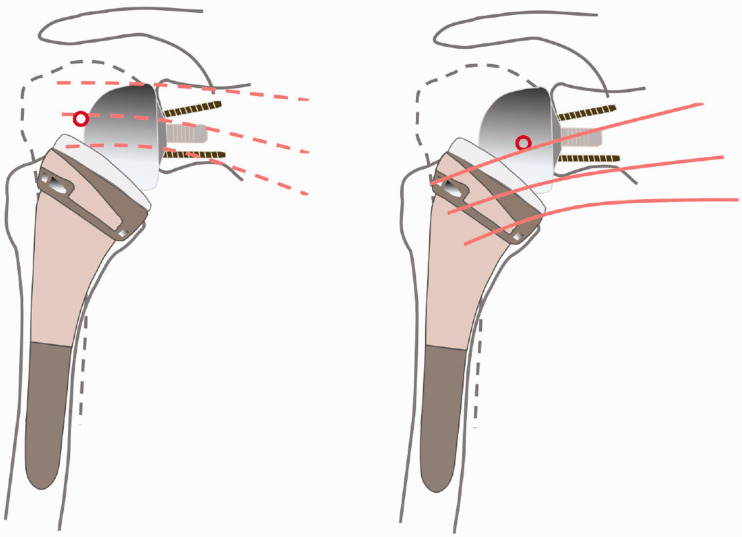
Ackland et al.17,21 were the first to perform a cadaveric biomechanical study to elucidate the changed biomechanics and muscle strength following RSA implantation. In their model, the trabecular metal reverse shoulder system (Zimmer, Warsaw, Indiana) was used on 8 fresh-frozen shoulders. In normal shoulders without a prosthesis, the subscapularis functions mainly as a flexor, abductor, and adductor. The subscapularis was the strongest internal rotator of all shoulder muscles in their study, internal rotation strength increased with arm abduction. After prosthesis implantation, it also acted as an extensor, abductor, and adductor depending on the arm position. The upper portion of the subscapularis in the native joint lies superior to the center of rotation and therefore acts as a functional abductor with the inferior part acting as a functional adductor. With the altered center of rotation, this changes from a functional abductor to an adductor in a reverse configuration (see Figure 1).
Figure 1.
Altered biomechanics of the subscapularis following RSA implantation.
Importantly, however, it was shown that in the absence of the subscapularis, there was adequate compensation by the remaining muscle components (pectoralis major, latissimus dorsi, and teres major).
The role of subscapularis repair on the force requirements for specific movements in RSA was analyzed by Hansen et al. 18 in a cadaver study. This group used the Delta III Grammont Prosthesis (DePuy, Warsaw, Indiana) for the repair group and an Equinoxe RSA (Exatech, Gainesville, Florida) for the nonrepair group. Unlike the Grammont Prosthesis, the Equinoxe design increases the lateral offset of the humeral shaft and lowers the center of rotation by lowering the glenoid component. As previously mentioned, the subscapularis muscle in this context functions in 2 parts. Both protheses alter the centers of rotation making most or all of the subscapularis act as an adductor. This change in biomechanics leads to dramatic changes in motion arms and forces. In both the repair and nonrepair groups, there was a marked increased force required for abduction. Further conclusions cannot be made as it was not a comparative study with refixation of the SSC in both prosthetic design groups.
The biomechanical effects on the subscapularis of different humeral neck-shaft-angles (HNSA) were examined by Oh et al. 19 Using the Aequalis reversed shoulder prosthesis (Wright/Tornier, Memphis, Tennessee) with 3 different HNSA (155°, 145°, and 135°) and once a loaded subscapularis and once unloaded in 6 cadaver shoulder models, they found that the forces necessary for dislocation were generally higher when the subscapularis was loaded/repaired. The 155° prosthesis design was the most stable design in internal rotation and neutral positions, while the subscapularis had the greatest role in shoulder stabilization in 135°. According to this biomechanical study, repairing the subscapularis increased the stability at all HNSA, while comparable forces were required for dislocation in the nonrepair models at all angles. This suggests that with a 135° prosthesis, a subscapularis repair is more likely to be required to gain stability than with higher HNSA since higher angles seem to provide more stability.
Pastor et al. 22 performed a cadaveric study using the Delta Xtend Prosthesis (DePuy Synthes, Warsaw, Indiana) with an emphasis on stability. Here, the effect of glenosphere size with subscapularis and/or posterior cuff loading on RSA stability was assessed. They showed that greater dislocation forces were required with a larger glenosphere (42 mm compared with 38 mm). Moreover, the greatest required forces were seen in the context of an intact rotator cuff including the subscapularis. When just the subscapularis was detached, the mean force necessary to dislocate the joint decreased by 18%; in conjunction with the posterior cuff, this increased to 25%. They showed that an intact subscapularis is beneficial for stability. In a clinical context, a larger glenosphere may improve stability.
A recent study compared different glenoid configurations on range of motion and muscle length in a computer model. 23 This study demonstrated an increased inferior component length in all rotator cuff muscles with RSA implantation, with exception of the subscapularis. In terms of component choice, a 36-mm eccentric glenosphere yielded the best range of motion of all those studied. Compared with different 36 mm glenospheres (36 mm centered, tilted, and with Bio RSA, and 42 mm centered glenosphere). The eccentric glenosphere seems to be optimal for preservation of adduction (native: 48.7°, 36° eccentric: 62.7°) and external rotation. This increased external rotation could compensate for the external rotation deficit sometimes described and seen in subscapularis repair. 24
Humeral component retroversion has been explored in multiple studies.25–27 Placing the humeral component in up to 20° retroversion increases the tension in the posterior rotator cuff and therefore may improve force for external rotation while not restricting internal rotation. This is important as maintaining good rotational forces following RSA is a major challenge.
In summary, RSA implantation converts the subscapularis to a functional adductor and internal rotator and potentially limits external rotation. Although seldom described, the significance of the subscapularis in internal rotation should not be underestimated. Subscapularis repair can be used to improve stability, particularly when 135° angle implants are used, but this adversely affects joint loading. In addition, implant design can greatly influence the functional role of the subscapularis. With an onlay system, a larger sized glenosphere, and a higher HNSA, the offset is increased and therefore the tension of the SSC is also raised, not only leading to improved stability and internal rotation but also potentially limiting and weakening external rotation.
Complications of RSA and the Role of the Subscapularis
In this section, we want to give an overview of possible techniques to treat the subscapularis during implantation of an RSA and its influence on potential intraoperative problems and the instability as one of the major postoperative complication.
The deltopectoral and the superolateral approaches are the most commonly described.28,29 The superolateral approach maintains subscapularis integrity but may adversely affect deltoid function, either directly through muscle damage or indirectly by potential axillary nerve injury. The deltopectoral approach may be used with different variations according to the strategy for addressing the subscapularis. Compared to aTSA, lesser tuberosity osteotomy and refixation is more challenging, as the lesser tuberosity attachment zone may be damaged during reaming of the metaphyseal part and could create an intraoperative problem. Both other described techniques (tenotomy and peel off) are more reproducible for subscapularis management.
One study described a novel subscapularis-sparing implantation technique using the deltopectoral approach through the ruptured supraspinatus window cranial to the subscapularis. 30 This yielded favorable results at 2-year follow-up. 31 In particular, as there are no muscle releases, full range of motion is possible immediately following surgery. All techniques described are showing good results in follow-up analysis. While initial results are promising, further, larger studies are required to determine the optimal implantation technique. 13 Chae et al. 32 reviewed the literature regarding the subscapularis and especially the role of the approach for stability. They found no difference between the proposed approaches, but the surgeon should be aware that when choosing a subscapularis sparing approach, the poorer vizualization of the inferior osteophytes can lead to impingement, levering, and dislocation. 33
According to the previsouly analyzed complications in a systematic review by Zumstein et al., 29 instability following RSA is one of the most controversial topics and a common complication seen in up to 8.6% of patients. 34 Although the most cited cause for instability is inadequate tensioning of the deltoid, the conjoined tendon,33–35 and direct abutment of the humeral component and glenoid, 36 the role of the subscapularis following RSA is one of the most discussed topics in contemporary literature. In a retrospective case–control study on 510 RSA, Padegimas et al.34 found 1 modifiable and 3 nonmodifiable risk factors for instability including subscapularis insufficiency:
Increased body mass index (odds ratio= 1.09, P = .047)
Male sex (odds ratio= 3.011, P= .019)
Revision arthroplasty (odds ratio = 7.515, P= .042)
Subscapularis insufficiency
This study built upon findings by Chalmers et al. 33 and Edwards et al. 37 which demonstrated similar, albeit statistically insignificant findings.
Analyzing the various complications, this may give clues as to the best way to reattach and repair the subscapularis, maintaining function of the 2 muscle subdivisions previously described.
Infection and hematoma
The lack of a tamponade effect normally provided by an intact rotator cuff following RSA may result in a higher bleeding tendency. 29 Therefore, a reconstruction of the subscapularis may reduce dead space anteriorly and thereby reduce bleeding. Speculatively, hematoma reduction could also potentially reduce infection rates, as fluid collections may act as foci for infections, but this has not been studied to date.
Fractures
Increased deltoid tension is seen with the lowered rotational center of the shoulder which may partially explain the increased rate of acromial fractures described.10,38 The management of these is normally conservative, but this may adversely affect the clinical outcome following RSA, so osteosynthesis may be required in some instances.
Subscapularis reconstruction, particularly above the center of rotation, if the prosthesis design allows, may serve to antagonise the increased stress on the acromion, which may reduce fracture incidence. Alternatively, fracture tendency may equally be due to the increased subscapularis force required for abduction because of increased glenohumeral load. These hypotheses, however are based on models and clinical evidence is required. 18
Clinical Outcomes
Subscapularis integrity is associated with better internal rotation which is important for activities of daily living.24,39,40 However, no studies to date have clearly demonstrated whether a subscapularis-sparing technique is advantageous. The precise effect of the potentially increased “adductor” effect of the superior subscapularis is unclear. Some studies have favored sparing or repair techniques,34,37 while others suggest no difference or worse outcomes and suggest foregoing the repair.41–43 Next, we compare the 2 approaches with regard to different factors.
Range of motion
Wall et al. 39 (n = 191) demonstrated improved internal rotation from L5/S1 to L3 postoperatively. In this study, the Delta III (DePuy Orthopaedics, Warsaw, Indiana) until 2002 and the Aequalis system after 2002 (Tornier, Memphis, Tennessee). Both inlay prosthesis designs medialize the center of rotation. The HNSA was 155° in both prostheses, but no detailed information concerning glenosphere size was provided.
Friedman et al. 24 found that the SSC repair group had slightly but statistically significant range of motion improvement pre- and postoperatively, specifically with regard to internal rotation. The Internal Rotation Score was 5.1 (±1.3) postoperatively for the repair group and 4.4 (±1.6, P < .0001) for the nonrepair group. Conversely, the nonrepair group had significantly better abduction (Repair 107° vs Nonrepair 119°, P < .0001) and passive external rotation (Repair 45° vs Nonrepair 50°, P < .0001). This is consistent with the biomechanical studies previously mentioned.
Using the Delta III Prosthesis (DePuy Orthopaedics, Warsaw, Indiana), Boileau et al. 44 found that repair had no influence on movement or functional scores. This study used a 20° to 30° retroversion for the humeral component to most closely approximate the native joint biomechanics. The standard glenosphere used was the 36 mm component, except in 4 cases where a 42 mm glenosphere was used. The HNSA of the prosthesis was 155°.
These findings are supported by Clark et al. 41 and Vourazeris et al. 45 In a cohort of 120 Shoulders using a RSP-Shoulder Prosthesis (DonJoy Surgical, Vista, California), Clark et al. found that flexion postoperatively was improved in the subscapularis repair group (112° vs 94°); however, overall improvements were seen in both groups compared to the preoperative baseline. The same is true of internal rotation. Retrospectively comparing the results of 202 Patients with a follow-up of more than 3 years, Vourazeris et al. recently found similar clinical outcome scores, range of motion, strength, and complications including dislocations. The authors used the Equinoxe Prothesis (Exatech, Gainesville, Florida).
Boulahia et al. 46 demonstrated improved external rotation in the nonrepair group (P = .0234). He used the Delta III shoulder prosthesis (DePuy Orthopaedics, Warsaw, Indiana). Implantation technique and glenosphere size were not described. The implant HNSA was 155°.
Werner et al. 43 retrospectively analyzed patients undergoing RSA with glenohumeral osteoarthritis or glenoid deformity. Here, the Biomet Comprehensive Reverse Shoulder System prosthesis was used (Zimmer Biomet, Warsaw, Indiana) with a neck-shaft angle of 147° and included 109 patients with a 2-year follow-up. Of the 109 patients, 104 received a 36 mm glenosphere. They divided the cohort into SSC-repair and nonrepair groups, as well as glenosphere lateralization or no lateralization. Patients with subscapularis repair and lateralization showed much lower ASES score improvements than patients with subscapularis repair without lateralization. Patients’ scores with subscapularis repair improved less with a lateralized glenosphere than patients without. Patients without a lateralized glenosphere showed no significant difference whether the subscapularis was repaired or not. The nonrepair group yielded much higher ASES score improvements than the repair group.
In summary, repairing the subscapularis may improve internal rotation while not repairing the subscapularis may enhance external rotation. This is in keeping with previously described biomechanical concepts. The difference of repair on abduction is currently unclear.
Clinical stability
Edwards et al. 37 demonstrated that dislocation risk doubled in the context of an irreparable subscapularis (P = .013). In this study, the Aequalis reverse total shoulder system (Tornier Inc, Memphis, Tennessee) with a 36 mm glenosphere was used and the humeral component was cemented in 10° of retroversion. Since this type of prosthesis uses a Grammont design, the HNSA was 155°, with medialization.
Examining the same cohort of patients as Edwards et al., Trappey et al. 47 published similar results. Patients with subscapularis tendon insufficiency at surgery had a rate of instability of 12% (14/123) while only 1 out of 161 patients suffered instability when the subscapularis could be repaired. Patients undergoing RSA due to fracture sequalae had the highest rate for instability followed by patients with massive cuff tear and pseudoparalysis.
Friedman et al.24 demonstrated comparable stability in the repair and nonrepair groups (0.5%). Here, a prosthesis design that lateralizes the humerus and medializes the glenoid was used (Equinoxe RSA by Exactech, Gainesville, Florida). The humeral neck-shaft-angle as well as the size of the glenosphere are not described. The conclusion is made that the prosthesis design obviates the question of subscapularis repair for the purposes of joint stability. The proposed mechanism is humeral component lateralization which increases deltoid and rotator cuff tension which enhances stability.
With regard to dislocation, pain, and postoperative range of motion, Clark et al. 41 found no significant effect with or without repair of the subscapularis. A retrospective study was performed including 111 patients (120 shoulders) undergoing implantation of a RSP-Shoulder Prosthesis (DonJoy Surgical, Vista, California) with a 135° inlay system. Dislocation was observed in 9% of the patients with no statistical difference between the repair and nonrepair groups.
Grassi et al. 42 found no effect on stability with subscapularis resection and RSA implantation. The study of 15 patients (19 shoulders) used a Delta Xtend Prosthesis (DePuy Synthes, Warsaw, Indiana); 20° retrotorsion of the humeral shaft was used to compensate for subscapularis resection. This arguably enhances external rotation and increases anterior soft tissue tension which improves joint stability. Because of the small number of patients, the retrospective design and all patients undergoing surgery due to fracture the conclusion of this article is limited.
In a case series analyzing instability following RSA implantation, Gallo et al. 48 found no difference between the repair and nonrepair groups. In this study, the Delta III prosthesis (DePuy Orthopaedics, Warsaw, Indiana) and the Encore reverse shoulder prosthesis (Encore Medical, Vista, California) were used. Of the 57 patients studied, instability was reported in 9 patients. In 4 of these patients, there was a concurrent joint infection, of which 1 was ascertained prior to surgery. The 5 patients with aseptic instability were found to have component malpositioning or inadequate deltoid tensioning. Subscapularis integrity was not correlated to instability.
Werner et al. 43 retrospectively analyzed patients undergoing RSA with glenohumeral osteoarthritis or glenoid deformity using the Biomet Comprehensive Reverse Shoulder System prosthesis (Zimmer Biomet, Encore Medical) with an HNSA of 147° and included 109 patients with a 2-year follow-up. Of the 109 patients, 104 received a 36 mm glenosphere. With regard to stability, there was no observed statistical difference dislocation or instability rates regardless of subscapularis repair or lateralization at 2-year follow-up. No instability or dislocation were reported in patients in the no-repair group.
Some of inherent limitations of these studies are as follows: a small sample size, different prosthesis designs, different rehabilitation protocols, different inclusion and exclusion criteria. Lack of matching Stability following RSA seems to be associated with multiple factors. This may explain in part the heterogeneity of conclusions reached by these studies. Moreover, in terms of instability, the various factors responsible are not uniformly described. For example, data regarding implantation technique and choice of implants such as glenosphere size and/or the HNSA are not consistently mentioned. In general, however, there is some evidence that good component positioning and adequate soft tissue tensioning may be of more importance for stability than the integrity of the subscapularis in the context of RSA.
Discussion
Studies heretofore have been unclear in proposing the treatment of the subscapularis in RSA implantation. Due to the many factors influencing clinical outcomes as well as various different study designs with lack of long-term outcome data, it is probably too soon to comment in this regard. High-quality, randomized control trials could potentially address this uncertainty.
With regard to range of motion, there is a suggestion that subscapularis preservation may result in improved internal rotation, while potentially being at the cost of passive external rotation.
Regarding stability, the effect of repair is unclear. It is likely that good implant positioning and proper soft tissue tensioning may be of more importance than subscapularis integrity.
The healing process and inherent innervation changes of the subscapularis after aTSA are under constant investigation.1–3,6 The same should be explored in the context of the RSA. In conjunction with the significantly altered biomechanics, this is likely to be very different.
Authors’ Preferred Method
As the subscapularis is a functional internal rotator and since biomechanical studies suggest improved stability using SSC repair especially in higher neck angles, we favor SSC-Refixation. Our preferred method is a RSA with an HNSA of 145°. For passive rotation and adduction, a lateralized glenosphere with an inferior offset seems advantageous. Prostheses that are modular with comprehensive and fully convertible designs including variation of the HNSA and retroversion in the metaphyseal part gives the operator greater flexibility with regard to preserves a significant anterior soft tissue border. This may serve as previously stated, may serve as an important structure for revision surgery, as well as the prevention of bleeding and potentially infection.
Further work might investigate the varying effects of subscapularis repair and nonrepair with regard to revision surgery. A nonrepaired subscapularis could adversely affect a revision situation, as this is naturally a vital landmark in an approach to the shoulder. As the use of RSA increases, it would follow that revision rates will also likely increase, so this is an important factor to consider.
Conclusion
In RSA, the subscapularis is particularly important with regard to range of motion, especially internal rotation, and potentially stability.
Reverse shoulder arthroplasty with or without subscapularis repair is a safe and successful method to improve range of motion and reduce pain in patients with a variety of shoulder pathologies. The precise role of the subscapularis is yet to be elucidated.
Regarding the range of motion, there is some evidence that repairing the subscapularis increases the ability for internal rotation while not repairing the muscle may lead to improved passive external rotation.
Good positioning of the implants and proper soft tissue tensioning may be of more importance for stability than the integrity of the subscapularis.
In general, future literature should include high-quality, larger studies analyzing these aspects, and possibly the role of subscapularis-sparing techniques in revision surgery.
Acknowledgments
The authors thank Paul Gilbert Fairhurst for editing and correcting our article.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Gerber C, Yian EH, Pfirrmann CA, Zumstein MA, Werner CM. Subscapularis muscle function and structure after total shoulder replacement with lesser tuberosity osteotomy and repair. J Bone Joint Surg Am. 2005; 87(8):1739–1745. [DOI] [PubMed] [Google Scholar]
- 2.Armstrong AD, Southam JD, Horne AH, Hollenbeak CS, Flemming DJ, Kothari MJ. Subscapularis function after total shoulder arthroplasty: electromyography, ultrasound, and clinical correlation. J Shoulder Elbow Surg. 2016; 25(10):1674–1680. [DOI] [PubMed] [Google Scholar]
- 3.Gobezie R, Denard PJ, Shishani Y, Romeo AA, Lederman E. Healing and functional outcome of a subscapularis peel repair with a stem-based repair after total shoulder arthroplasty. J Shoulder Elbow Surg. 2017; 26(9):1603–1608. [DOI] [PubMed] [Google Scholar]
- 4.Jackson JD, Cil A, Smith J, Steinmann SP. Integrity and function of the subscapularis after total shoulder arthroplasty. J Shoulder Elbow Surg. 2010; 19(7):1085–1090. [DOI] [PubMed] [Google Scholar]
- 5.Louie PK, Levy DM, Bach BR Jr, Nicholson GP, Romeo AA. Subscapularis tenotomy versus lesser tuberosity osteotomy for total shoulder arthroplasty: a systematic review. Am J Orthop (Belle Mead NJ). 2017; 46(2):E131–E138. [PubMed] [Google Scholar]
- 6.Miller SL, Hazrati Y, Klepps S, Chiang A, Flatow EL. Loss of subscapularis function after total shoulder replacement: a seldom recognized problem. J Shoulder Elbow Surg. 2003; 12(1):29–34. [DOI] [PubMed] [Google Scholar]
- 7.Moeckel BH, Altchek DW, Warren RF, Wickiewicz TL, Dines DM. Instability of the shoulder after arthroplasty. J Bone Joint Surg Am. 1993; 75(4):492–497. [DOI] [PubMed] [Google Scholar]
- 8.Sacevich N, Athwal GS, Lapner P. Subscapularis management in total shoulder arthroplasty. J Hand Surg Am. 2015; 40(5):1009–1011. [DOI] [PubMed] [Google Scholar]
- 9.Shields E, Ho A, Wiater JM. Management of the subscapularis tendon during total shoulder arthroplasty. J Shoulder Elbow Surg. 2017; 26(4):723–731. [DOI] [PubMed] [Google Scholar]
- 10.Bohsali KI, Bois AJ, Wirth MA. Complications of shoulder arthroplasty. J Bone Joint Surg Am. 2017; 99(3):256–269. [DOI] [PubMed] [Google Scholar]
- 11.Kany J Jose J Katz Det al. The main cause of instability after unconstrained shoulder prosthesis is soft tissue deficiency. J Shoulder Elbow Surg. 2017; 26(8):e243–e251. [DOI] [PubMed] [Google Scholar]
- 12.Lapner PL, Sabri E, Rakhra K, Bell K, Athwal GS. Comparison of lesser tuberosity osteotomy to subscapularis peel in shoulder arthroplasty: a randomized controlled trial . J Bone Joint Surg Am. 2012; 94(24):2239–2246. [DOI] [PubMed] [Google Scholar]
- 13.Choate WS, Kwapisz A, Momaya AM, Hawkins RJ, Tokish JM. Outcomes for subscapularis management techniques in shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg. 2018; 27(2):363–370. [DOI] [PubMed] [Google Scholar]
- 14.Grammont P, Trouilloud P, Laffay JP, Deries X. Etude et réalisation d´une nouvelle prothèse d´épaule. Rheumatologie. 1987; 39:407–418. [Google Scholar]
- 15.Alexandre L, Stephen SB, Pierre H, et al. Classification of full-thickness rotator cuff lesions: a review. EFORT Open Rev. 2016; 1(12):420–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Collin P, Lädermann A, Le Bourg M, Walch G. Subscapularis minor—an analogue of the Teres minor? Orthop Traumatol Surg Res. 2013; 99(4 Suppl):S255–S258. [DOI] [PubMed] [Google Scholar]
- 17.Ackland DC, Richardson M, Pandy MG. Axial rotation moment arms of the shoulder musculature after reverse total shoulder arthroplasty. J Bone Joint Surg Am. 2012; 94(20):1886–1895. [DOI] [PubMed] [Google Scholar]
- 18.Hansen ML Nayak A Narayanan MSet al.. Role of subscapularis repair on muscle force requirements with reverse shoulder arthroplasty. Bull Hosp Jt Dis. 2015; 73(Suppl 1):S21–S27. [PubMed] [Google Scholar]
- 19.Oh JH, Shin SJ, McGarry MH, Scott JH, Heckmann N, Lee TQ. Biomechanical effects of humeral neck-shaft angle and subscapularis integrity in reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2014; 23(8):1091–1098. [DOI] [PubMed] [Google Scholar]
- 20.Giles JW, Langohr GD, Johnson JA, Athwal GS. The rotator cuff muscles are antagonists after reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2016; 25(10):1592–1600. [DOI] [PubMed] [Google Scholar]
- 21.Ackland DC, Roshan-Zamir S, Richardson M, Pandy MG. Moment arms of the shoulder musculature after reverse total shoulder arthroplasty. J Bone Joint Surg Am. 2010; 92(5):1221–1230. [DOI] [PubMed] [Google Scholar]
- 22.Pastor MF, Kraemer M, Wellmann M, Hurschler C, Smith T. Anterior stability of the reverse shoulder arthroplasty depending on implant configuration and rotator cuff condition. Arch Orthop Trauma Surg. 2016; 136(11):1513–1519. [DOI] [PubMed] [Google Scholar]
- 23.Lädermann A, Denard PJ, Boileau P, Farron A, Deransart P, Walch G. What is the best glenoid configuration in onlay reverse shoulder arthroplasty? Int Orthop, 2018;42:1339--1346. doi: 10.1007/s00264-018-3850-x [DOI] [PubMed] [Google Scholar]
- 24.Friedman RJ, Flurin PH, Wright TW, Zuckerman JD, Roche CP. Comparison of reverse total shoulder arthroplasty outcomes with and without subscapularis repair. J Shoulder Elbow Surg. 2017; 26(4):662–668. [DOI] [PubMed] [Google Scholar]
- 25.Gulotta LV Choi D Marinello Pet al.. Humeral component retroversion in reverse total shoulder arthroplasty: a biomechanical study. J Shoulder Elbow Surg. 2012; 21(9):1121–1127. [DOI] [PubMed] [Google Scholar]
- 26.Rhee YG, Cho NS, Moon SC. Effects of humeral component retroversion on functional outcomes in reverse total shoulder arthroplasty for cuff tear arthropathy. J Shoulder Elbow Surg. 2015; 24(10):1574–1581. [DOI] [PubMed] [Google Scholar]
- 27.Aleem AW Feeley BT Austin LSet al.. Effect of humeral component version on outcomes in reverse shoulder arthroplasty. Orthopedics. 2017; 40(3):179–186. [DOI] [PubMed] [Google Scholar]
- 28.Daniel M Frank W Charles D Philippe V,François S. Surgical technique: the anterosuperior approach for reverse shoulder arthroplasty. Clin Orthop Relat Res. 2011; 469(9):2461–2468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zumstein MA, Pinedo M, Old J, Boileau P. Problems, complications, reoperations, and revisions in reverse total shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg. 2011; 20(1):146–157. [DOI] [PubMed] [Google Scholar]
- 30.Lädermann A, Lo EY, Schwitzguébel AJ, Yates E. Subscapularis and deltoid preserving anterior approach for reverse shoulder arthroplasty. Orthop Traumatol Surg Res. 2016; 102(7):905–908. [DOI] [PubMed] [Google Scholar]
- 31.Lädermann A, Denard PJ, Tirefort J, Collin P, Nowak A, Schwitzguebel AJ. Subscapularis- and deltoid-sparing vs traditional deltopectoral approach in reverse shoulder arthroplasty: a prospective case-control study. J Orthop Surg Res. 2017; 12(1):112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chae J, Siljander M, Wiater JM. Instability in reverse total shoulder arthroplasty. J Am Acad Orthop Surg. 2018; 26(17):587–596. [DOI] [PubMed] [Google Scholar]
- 33.Chalmers PN, Rahman Z, Romeo AA, Nicholson GP. Early dislocation after reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2014; 23(5):737–744. [DOI] [PubMed] [Google Scholar]
- 34.Padegimas EM Zmistowski BM Restrepo Cet al. Instability after reverse total shoulder arthroplasty: which patients dislocate? Am J Orthop (Belle Mead NJ). 2016; 45(7):E444–E450. [PubMed] [Google Scholar]
- 35.Kohan EM, Chalmers PN, Salazar D, Keener JD, Yamaguchi K, Chamberlain AM. Dislocation following reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2017; 26(7):1238–1245. [DOI] [PubMed] [Google Scholar]
- 36.Lädermann A Denard PJ Boileau Pet al. Effect of humeral stem design on humeral position and range of motion in reverse shoulder arthroplasty. Int Orthop, 2015; 39(11):2205–2213. [DOI] [PubMed] [Google Scholar]
- 37.Edwards TB, Williams MD, Labriola JE, Elkousy HA, Gartsman GM, O'Connor DP. Subscapularis insufficiency and the risk of shoulder dislocation after reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2009; 18(6):892–896. [DOI] [PubMed] [Google Scholar]
- 38.Alentorn-Geli E, Samitier G, Torrens C, Wright TW. Reverse shoulder arthroplasty. Part 2: systematic review of reoperations, revisions, problems, and complications. Int J Shoulder Surg. 2015; 9(2):60–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wall B, Nové-Josserand L, O'Connor DP, Edwards TB, Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am. 2007; 89(7):1476–1485. [DOI] [PubMed] [Google Scholar]
- 40.Dedy NJ, Gouk CJ, Taylor FJ, Thomas M, Tan SLE. Sonographic assessment of the subscapularis after reverse shoulder arthroplasty: impact of tendon integrity on shoulder function. J Shoulder Elbow Surg, 2018; ▪:▪. [DOI] [PubMed] [Google Scholar]
- 41.Clark JC Ritchie J Song FSet al.. Complication rates, dislocation, pain, and postoperative range of motion after reverse shoulder arthroplasty in patients with and without repair of the subscapularis. J Shoulder Elbow Surg. 2012; 21(1):36–41. [DOI] [PubMed] [Google Scholar]
- 42.Grassi FA, Zorzolo I. Reverse shoulder arthroplasty without subscapularis repair for the treatment of proximal humeral fractures in the elderly. Musculoskelet Surg. 2014; 98 Suppl 1:5–13. [DOI] [PubMed] [Google Scholar]
- 43.Werner BC Wong AC Mahony GTet al.. Clinical outcomes after reverse shoulder arthroplasty with and without subscapularis repair: the importance of considering glenosphere lateralization. J Am Acad Orthop Surg. 2018; 26(5):e114–e119. [DOI] [PubMed] [Google Scholar]
- 44.Boileau P, Watkinson D, Hatzidakis AM, Hovorka I. Neer Award 2005: The Grammont reverse shoulder prosthesis: results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg. 2006; 15(5):527–540. [DOI] [PubMed] [Google Scholar]
- 45.Vourazeris JD, Wright TW, Struk AM, King JJ, Farmer KW. Primary reverse total shoulder arthroplasty outcomes in patients with subscapularis repair versus tenotomy. J Shoulder Elbow Surg. 2017; 26(3):450–457. [DOI] [PubMed] [Google Scholar]
- 46.Boulahia A, Edwards TB, Walch G, Baratta RV. Early results of a reverse design prosthesis in the treatment of arthritis of the shoulder in elderly patients with a large rotator cuff tear. Orthopedics, 2002; 25(2):129–133. [DOI] [PubMed] [Google Scholar]
- 47.Trappey GJ. 4th, O'Connor DP, Edwards TB. What are the instability and infection rates after reverse shoulder arthroplasty? Clin Orthop Relat Res. 2011; 469(9):2505–2511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gallo RA Gamradt SC Mattern CJet al. Instability after reverse total shoulder replacement. J Shoulder Elbow Surg. 2011; 20(4):584–590. [DOI] [PubMed] [Google Scholar]