Abstract
People with disabilities (PWD) are a health disparities population who experience well-documented physical, structural, attitudinal, and financial barriers to health care. The disability rights community is deeply engaged in advocacy to promote health care justice for all PWD. As the community continues to work toward systems change, there is a critical need for community-directed interventions that ensure individuals with disabilities are able to access the health care services they need and are entitled to. Peer health navigator (PHN) programs have been shown to help people from diverse underserved communities break down barriers to health care. The PHN model has not been systematically adapted to meet the needs of PWD. In this article, we describe the collaborative process of developing Our Peers—Empowerment and Navigational Supports (OP-ENS), an evidence-informed PHN intervention for Medicaid beneficiaries with physical disabilities in Chicago, IL, USA. Our Peers—Empowerment and Navigational Supports is a 12-month community-based PHN intervention that pairs Medicaid beneficiaries with physical disabilities (peers) with disability PHNs who use a structured recursive process of barrier identification and asset mapping, goal setting, and action planning to help peers meet their health care needs. Our Peers—Empowerment and Navigational Supports was developed by a collaborative team that included disability rights leaders, representatives from a Medicaid managed care organization, and academic disability health care justice researchers. We highlight both the conceptual and empirical evidence that informed OP-ENS as well as the lessons learned that can assist future developers.
Keywords: disabled persons, Medicaid, social justice, health care delivery
Article 25 of the Convention on the Rights of Persons with Disabilities recognizes that people with disabilities (PWD) have the right to the “highest attainable standard of health without discrimination on the basis of disability.” 1 Yet, according to the World Report on Disability, 2 PWD experience structural,3,4 financial,5,6 cognitive/knowledge,7,8 attitudinal, 9 and physical barriers,10,11 to preventive,12–14 primary, 15 and specialty care. 16 Adults with physical disabilities are at higher risk of foregoing or delaying necessary care, 5 having unmet medical, dental, and prescription needs compared with adults without disabilities.17,18 In the United States, PWD have higher rates of risky health behaviors, including smoking, drinking, obesity, and sedentary lifestyles. 19 The health and well-being of PWD are directly related to the availability of appropriate health care services. 20 Lack of timely access to primary and preventive care can result in the development of chronic and secondary conditions as well as the exacerbation of the disabling condition itself,21–23 resulting in poorer health outcomes for PWD.4,9,24,25 Now that the existence and some of the underlying causes of health care disparities have been established, the challenge lies in developing, implementing, and sustaining effective strategies to eliminate health disparities in community and clinical settings. 26 Confronted with multiple barriers to care and a fragmented health care system, PWD benefit from supportive resources to effectively coordinate care and access health care services, public benefit programs, legal rights, and their health condition. 27
A growing body of research suggests that peer health navigator (PHN) interventions are a promising community-directed approach to breaking down barriers to care for people from underserved communities and therefore empowering them to navigate a complex health care system more successfully. Peer health navigators (PHN) are people from the target community who have received specialized training to provide culturally appropriate services and supports. Peer health navigators’ focus is on helping people navigate the complex and often fragmented health care delivery systems. This differentiates them from other peer interventionists, such as community health workers (CHW), who are defined by the World Health Organization as individuals trained to perform one or more interventions related to a specific health care need of a community. 28 Most often, CHWs are auxiliaries recognized by the health services organizations they work within as part of the health care team addressing a narrow intervention focus. 29 Peer health navigators (PHN) are less likely to be health care professionals; rather they are individuals who are members of the community, and as a result of shared lived experiences, 30 they address broader health concerns, with a focus on individual and community empowerment. 31 PHNs use their training and experiential knowledge to empower individuals to take control of their health care by providing individualized supports and structured problem-solving skill building to help address the myriad barriers to health care access, quality, and outcomes. Peer health navigators empower the participants to identify their own needs and priorities and work with their providers to address those concerns. Peer health navigator (PHN) programs have been used successfully across diverse populations—including African American women with breast cancer, 32 Latinas with breast cancer, 33 Korean American women with no or insufficient health insurance, 34 adults with spinal cord injury, 35 HIV, 36 and mental health37,38—to reduce barriers to care, empower people from underserved communities, and improve health and health care outcomes. 39
In spite of their success across diverse populations, PHN programs have yet to be adapted to meet the needs of people with physical disabilities living in the community. To address this gap, we built on a long-term disability community-academic partnership to develop a culturally tailored PHN intervention, called Our Peers—Empowerment and Navigational Support (OP-ENS), for people with physical disabilities. In this article, we describe a community-based participatory research (CBPR) approach to develop the core components of OP-ENS by tailoring existing evidence-based PHN interventions to meet the primary care needs of people with physical disabilities. We tailored DeGroff et al’s 40 10 key areas of considerations for designing patient navigator programs to structure the OP-ENS intervention. While there are important differences between DeGroff and colleagues’ emphasis on patient navigator interventions for people with cancer and OP-ENS’ emphasis on peer navigators for people with physical disabilities, the key areas are broadly applicable and provide a practical and comprehensive framework for developers of navigator programs for PWD.
Ten Areas of Consideration When Designing a PHN Intervention: The Case of OP-ENS
Overarching approach
We developed OP-ENS using a CBPR approach that builds on a long-term community-campus collaboration between leaders in the disability rights and independent living movement all of whom have a lived experience with disability (JPR, JT, and TW) and academic researchers who focus on health care justice for PWD (SM and CP). Community-based participatory research is an approach to research that leverages the strengths of community and academic partners “with the aim of contributing knowledge and action for social change to improve community health and eliminate disparities.” 41 Both community and academic partners share the view that disability is a part of the human experience and diversity and not something that needs to be “fixed” by medical professionals while still acknowledging the importance of accessible, disability competent health care services. Inherent in our partnership is the recognition that there is tremendous strength and accumulated knowledge within the disability community and leveraging that strength is a pathway to empowerment for the individual and the community as a whole. Furthermore, peer support is a central tenet of the disability rights and Independent Living movements.42,37 We also partnered with a managed care organization (MCO) in the state of Illinois that was interested to pilot test and potentially implement a PHN program in their clinical sites. The 3 organizations (academy, community advocacy, and clinical organization) shared the goal of using PHNs to improve PWD’s access to primary care.
Use of a CBPR approach 35 to the development and implementation of the OP-ENS interventions was important for 3 primary reasons. First, it is consistent with the existing long-term collaborative relationship between community and academic partners26,35 aimed at the identification and elimination of barriers to health care access and quality and outcomes for PWD. Second, it reflects the disability rights and Independent Living movements’ mantra of “Nothing about us without us” 42 as the disability community seeks to counteract the historical tendency of the medical establishment to exert control over the lives of PWD. 43 People with disabilities are demanding leadership roles related to the services, supports, and programming that affect their lives. It was critically important from a research equity and health care justice perspectives 41 that disability community leaders occupy leadership roles in all stages of this project including intervention development, implementation, and evaluation. Finally, best practices in the development of PHN interventions highlight the importance of input from local communities and target users to ensure trust, responsiveness, and community buy-in. 44
Theoretical Framework and Program Goals
The OP-ENS program goals were to empower and support individuals to (1) break down barriers to care through a structured process of goal setting, barrier identification and asset mapping, and action planning; (2) develop a repertoire of successes within the health care system that they can draw on once the intervention is over; and (3) develop and maintain skills and supports long term post intervention. These program goals were developed by the first author (SM) in collaboration with members of the disability community in Chicago, IL, USA. Specifically, the 2 partners co-wrote and conducted multiple qualitative research studies (n > 140 people) to understand the disability community’s health care experiences. Participants identified physical, attitudinal, and informational barriers to care but were uncertain how to effectively break down these barriers through their individual efforts. We also identified tremendous strengths and knowledge within the disability community. The OP-ENS intervention was developed to address the community identified needs by systematizing and leveraging the strengths within the disability community.
A thorough literature review of peer and patient navigation programs and studies identified a program to support Black men who have sex with men (MSM) at risk for HIV (HPTN 061) 36 that shares many of the values and challenges as the OP-ENS program. The MSM study 36 targeted men at risk for developing HIV who had a broad range of fluctuating needs and an undefined trajectory in contrast to PHN programs aimed at helping people complete a well-defined (and often linear) course of treatment. Given that PWD live with a thinner margin of health and vacillate between periods of relative stability and high health care and medical needs, we modeled key intervention components of OP-ENS on the MSM protocol, including frequency, duration, and a broad view of health based on a social determinants of health framework. 45 The core component of the intervention is a structured process of rapport building, goal setting, barrier identification and asset mapping, action planning, and follow-up to address participants’ needs and priorities. Using a person-centered approach,46,47 the PHNs provide structure and ongoing support while helping participants use and develop skills in the recursive process of goal setting, action planning, and follow-up.
The OP-ENS intervention operates at the nexus of provision of social support and promotion of self-efficacy, 48 each of which takes primacy depending on individual participant’s needs and priorities at the time and may shift during the 12-month intervention period. Provision of social support is based on the stress and coping perspective that social support, especially when provided by peers, promotes adaptive coping through the exchange of emotional and informational support.48,49 Knowing that there is someone who understands what you are going through, whom you can trust and rely on, is thought to have both a direct and moderating effect on health. It also lays a foundation of trust so that if a health care concern or need arises participants have an established relationship to reach out for more direct support.
When participants have more pressing health care needs, the PHNs use the structured process of goal setting and action planning to promote self-efficacy within the participant and help them break down barriers to care. This approach is rooted in Bandura social cognitive theory, 50 so that as PHNs and participants work together to address a specific need or barrier, the participant builds a repertoire of success that they draw on when future health care challenges emerge.
Community Characteristics
When designing a PHN intervention, it is important to clearly define the specific community characteristics of the target population to be served. In the United States, adults with disabilities are more likely to be insured through federal and state entitlement programs such as Medicaid and Medicare. Medicaid services in the United States are characterized by restricted access to providers, provision of a narrower range of services, and strategic ambiguity, which makes the system hard for many PWD to understand and navigate. 51 The OP-ENS intervention targets people with physical disabilities who receive health care coverage through Medicaid and who are eligible for home- and community-based services waivers through the following 2 programs: Persons with Disabilities and Persons with Brain Injury waivers in Cook County, Chicago, IL, USA. Given that the OP-ENS team was committed to the cross disability community, people were eligible to participate if they self-identified as a person with a physical disability and screened as positive for physical disability using the standard 6-disability items from the American Community Survey. 52 Admittedly, people with physical disabilities are a heterogeneous population with a wide variety of individual health needs, yet evidence suggests that there are important overarching barriers that people experience, such as transportation, access to durable medical equipment, patient-provider communications, and social isolation, regardless of the diagnostic origin of their disability. It is these types of modifiable barriers that PHNs are well positioned and trained to help address. Given that community partners have a deep commitment to serving the cross-disability community, it was important to us as a team not to exclude people based on diagnostic labels.
The PHN research literature27–34,38–40,42,43 indicates that people with higher support needs reap greater benefits from PHN services; therefore, we targeted Medicaid beneficiaries who received home and community-based service waivers (HCBS) that allow PWD to be eligible for community-based supports such as personal care assistants. Eligibility for HCBS waivers is determined by their level of support needs as assessed by the State Department of Health and Human Services. We excluded people with primary diagnoses of serious, persistent mental illness, substance abuse, and pain with narcotic management. While these groups may represent high-need sub-groups within the disability community, additional knowledge and training is required to adequately address those needs.
Point of Intervention
Point of intervention refers to where in an illness trajectory or course of care the PHN intervention occurs. While this model works well in say cancer care, it does not reflect the uncertain course of fluctuating needs of community-dwelling adults with disabilities, who may be reasonably expected to have periods of stability and low need punctuated by times of high need. The existing literature on PHN programs shows tremendous variability in the duration of PHN programs from a few weeks to a year or more. 53 To capture the potential variability and fluctuation in needs of PWD, we structured OP-ENS to last 12 months. This allowed PHNs a protracted period of time to build trust and rapport. Since many PWD have had repeated negative experiences with health care providers and payers, trust building is important. The yearlong intervention also affords the peers and PHNs time to address what are often complex and interconnected needs around identified goals. A targeted period of transition and discharge planning was deemed vital to ensure that participants are ready to assume responsibility for their care and apply the knowledge and skills they learned over the course of the intervention.
Setting
There is no one best place to house PHN services. Indeed, the research literature indicates that PHN programs are based in a variety of settings ranging from highly medicalized (such as primary care practices, cancer centers, and hospitals) to community-based settings. 40 While Chicago is a large urban center with many hospitals and health care clinics, there is no “go-to” facility for Medicaid beneficiaries with physical disabilities. It is likely that no single clinic has a predictable flow of PWD to warrant the hiring of a full-time on-site PHN. Furthermore, research suggests that when embedded within a clinical or administrative health care setting, peer providers are rapidly “professionalized” and lose some of their autonomy as peers. 54 In addition, disability community partners expressed concerns that if embedded within a health care organization, PHNs might be susceptible to power differentials within the health care team and lose their ability to address participant-identified needs compared with provider-identified priorities. Therefore, we chose to embed the navigators in a community-based setting providing office space and infrastructure within the university. Emphasis was placed on creating a welcoming non-clinical environment for meetings with comfortable seating, welcoming decor and snacks. This environment sought to cultivate peer relationships and decrease power differentials between participants and PHNs.
Services
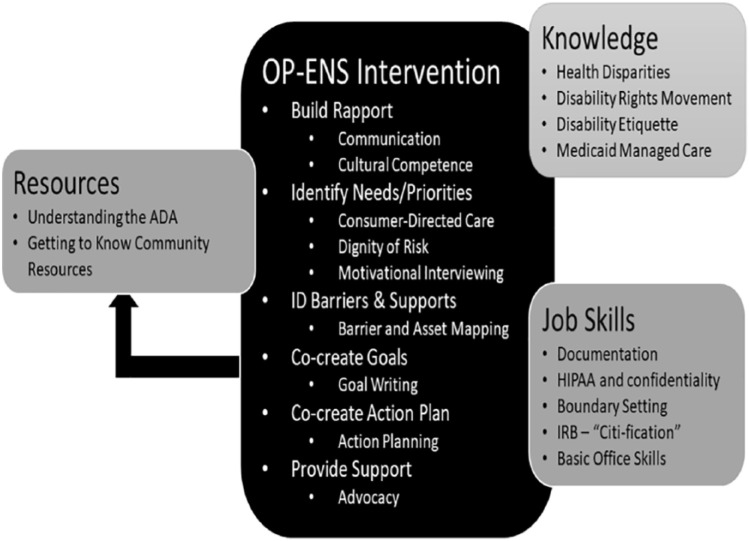
When designing a PHN intervention, it is important to identify clearly the services that will be offered and how these services will be rendered. The OP-ENS team developed a manualized intervention that addresses the core components of rapport building, goal setting, barrier identification and asset mapping, and action planning to address participant-identified needs and priorities. The operational manual was built after the community-based PHN intervention for MSM study. 36 Briefly, the core components of the OP-ENS intervention are (see Figure 1) as follows:
Figure 1.
The OP-ENS intervention process (middle column) and trainee curriculum areas. ADA indicates Americans with Disabilities Act; HIPAA, Health Insurance Portability and Accountability Act; IRB, institutional review board; OP-ENS, Our Peers—Empowerment and Navigational Support.
Rapport building among PHNs and participants to get to know each other, explain PHN services, and build trust among the two. Interactions occurred in-person or by phone with PHNs taking the time to actively empathize and validate participants’ concerns.
Goal setting—Through dialogue and PHN guidance, participants identify their needs and priorities. Peer health navigators and participants then worked together to co-create actionable, achievable goals to address participants’ needs and priorities. This motivational phase empowered participants to envision alternatives to their current situation and break down barriers to care.
Barrier identification and asset mapping—PHNs work with participants to critically analyze their situation to identify both barriers and facilitators to goal achievement. Peer health navigators were taught to use an asset mapping approach to help participants recognize strengths and supports in themselves, their social networks, and their communities at large by realistically evaluating the factors that can influence goal achievement and help foster success.
Action planning is the co-creation of specific, action-oriented, and achievable steps toward goal achievement. Peer health navigators and participants broke down goals into a series of achievable steps. The PHN’s role was to ensure that the goals and plans were achievable and reflected the needs and priorities of participants. Action plans helped to hold both parties responsible for what they needed to do to accomplish goals. To foster participant empowerment, PHNs used a “do with” rather “than do” for approach whereby the onus is on the participant work toward their goal with the PHNs’ support and guidance. Action planning moves a goal from something that is wished for to something that is actively and intentionally worked for.
Follow through and next steps: The PHNs followed-up with participants about their action plan and progress toward their goals. As goals were achieved, new goals developed and the process was repeated. Peer health navigators provided ongoing informational and emotional support to participants.
As already mentioned, OP-ENS is built on the premise that the participants’ needs and priorities were validated and addressed (when feasible). The OP-ENS intervention is flexible enough to enable participants to address those issues of primary importance to them. Some examples of personal goals included improving communication with their health care provider, increasing physical activity, getting their wheelchair repaired or replaced, and accessing disability transportation services. Within OP-ENS, we adopted a broad conceptualization of health that encompasses primarily health care services as well as many of the social determinants of health-like housing, healthy eating and food security, and transportation. 45 PHNs also offered emotional support and had the benefit of relative low caseloads that enabled them to spend more time with participants than is typically afforded health care and social support professionals.
Setting professional boundaries around what is outside of the PHN’s scope of services is also important. Our Peers—Empowerment and Navigational Supports PHNs are not health care providers or social workers, and as a result, they did not provide medical advice instead facilitated linkages and outreach to community-based services when appropriate.
Communication
There are a variety of communication methods between navigators and participants described in the navigator literature. The OP-ENS intervention was designed to be conducted using a combination of in-person and telephone check-in meetings. While PHNs and participants had the flexibility to meet as often as necessary, a minimum of monthly contacts were stipulated as part of the manualized intervention protocol. Within the state of Illinois Medicaid Managed Care program, PWD are assigned a care coordinator who must contact them monthly. We chose to replicate this frequency of contact. It was deemed acceptable and familiar to Medicaid beneficiaries with physical disabilities and provided a reasonable opportunity support but not replicate the ongoing work of the Medicaid MCO.
In-person meetings were required during pivotal junctures in the OP-ENS intervention, including the initial meeting to establish rapport, relationship building, and trust: at 6 months to foster a mid-term connection and ensure that participants are on track with working toward their goals and identified priorities; at month 11 to work on a transition plan; and at month 12 to review progress made throughout the year, promote closure, and finalize the discharge process. Telephone contact was recommended for the intervening months. While PHNs may support participants in communicating with their health care team or care coordinator within their Medicaid MCO, they were not authorized to communicate directly with these entities.
Navigator Background and Qualifications
The success of PHN interventions depends in large part of the quality and attributes of the navigators themselves. 55 As a team, we identified both skills that people need coming into the role as well as specific knowledge, skills, and abilities that mapped to the intervention components. Critical qualifications for potential candidates were as follows:
Personal experience as a person with a physical disability and comfortable sharing that experience with others.
Firsthand experience utilizing the health care system and community resources.
Working knowledge of Medicaid preferred.
History of advocating, educating, and supporting people with physical disabilities.
Ability to interact positively with health care professionals.
Skills in mentoring, leadership, taking initiative, and completing assignments.
Minimum of high school diploma or equivalent (to enable hiring through the university system).
Ability to pass background check (to ensure participant safety).
Consistent with best practices for PHN recruitment and hiring, 44 we provided applicants with multiple points of exit from the OP-ENS hiring process. First, we advertised for the position through local disability and clinical organizations, and then, we held an informational meeting for interested individuals to learn about the project and position. Interested individuals were instructed to contact the OP-ENS project team to schedule an interview. A total of 10 candidates were invited to complete the paid 40-hour OP-ENS PHN training. Individuals who completed the training were invited to join the OP-ENS PHN team. Through this process, we were able to evaluate candidates’ level of motivation and commitment to the program while also determining their level of fit for the role. The OP-ENS team employed 9 PHNs as part-time employees with renewable annual contracts. They were paid hourly, and their typical case load was 3-5 participants per PHN. We originally budgeted 1 full-time equivalence (eg, 40 hours per week) for the PHN; these hours were divided between the PHN team. This approach conferred the advantages of a strong team-based approach with opportunities for peer support and social learning among the PHNs, keeping caseloads low as PHNs develop their navigational skills, and preventing PHN burn-out. Furthermore, the decision to employ a large team of part-time PHNs ensured that PHNs would not lose disability benefits. All PHNs passed criminal background checks and adhered to other organizational hiring practices and regulations, and these posed no undue logistical or practical difficulties for the PHNs.
Training
Evidence suggests that PHNs face a steep learning curve as they work to acquire the necessary knowledge and skills to be effective in their role. 55 We created a training program that gradually scaffolds learning of knowledge, skills, and abilities overtime with extensive opportunities for discussion, practice, and strategic repetition of core concepts. We based the training on our literature reviews of existing PHN programs,27–34,38–40,42,43,55–57 consultation with PHN program directors,36,58 our professional expertise as educators, advocates and health care providers, and the active engagement of disability community partners. In this section, we explain in detail the OP-ENS PHN training to facilitate future developers to learn from our experiences and use our methods to organize and structure their interventions.
Figure 1 shows the 3 large categories of skills, knowledge, and resources included in the PHN intervention and addressed during the PHN training. The OP-ENS team worked collaboratively to map the knowledge, skills, and competencies needed to deliver the intervention to the core components of the manualized intervention. The team met every 2 weeks to co-write the modules and monthly to review and update each other regarding module development, problem solving and discuss each other’s work. The multiple perspectives of each partner presented an opportunity for learning from each other, as well as a need to communicate clearly and often. The curriculum was reviewed and approved by all team members prior to implementation. We outline the 6 key domains of navigator training that Wells et al 59 have suggested, which are relevant when describing PHN trainings. These domains are duration, location, format, occupation of trainer, learning strategies, and training content or topics.
Duration and location
The OP-ENS PHN curriculum was a bi-weekly, 10-week, 40-hour in-person training. Each session lasted approximately 4 hours. In-person participation was mandatory and we allowed one excused absence.
Training content
The topics included in training content are health disparities; disability history; disability rights, advocacy, and etiquette; motivational interviewing; understanding Medicaid-managed care; Health Insurance Portability and Accountability Act (HIPAA) and client confidentiality; culturally competent communication; goal setting, asset mapping, and action planning; boundary setting; and office organizational skills. A lead trainer from the academic team facilitated the training sessions, with community and clinical partners delivering key components of the training. For example, disability community partners lead the sessions on the history and development of the disability rights movement, the Americans with Disabilities Act, the systemic discrimination experienced by persons with disabilities within the US health care system, and advocacy. The clinical partner took the lead on delivering content related to how Medicaid works in the state of IL and in their clinical care settings, as well as ethical consideration when interacting with clients, including adherence to HIPAA privacy guidelines. Guest speakers with expert knowledge delivered content on issues such as cultural competence and motivational interviewing.
Learning strategy and format
We applied principles of adult and transformational learning 60 to develop the instructional strategy and format of the curriculum. Every session included information sharing as well as engaged discussions with the trainees. The first 5 trainings were content-heavy; that is, we introduced a lot of information on disability rights, health disparities, how the intervention will work, who the clinical partner is, and what they expect. The second half of the training was more skills-based; allowing trainees practice and apply what they learned through more active hands-on approaches, such as role-playing, case studies, and practicum. We also used peer observation and feedback cycles to deepen the comprehension of the person doing the task and the person observing and providing feedback. All trainings were conducted in a round table discussion format and incorporated trainee sharing and exchanging of their experiences, learning, and brainstorming/problem-solving exercises.
Occupation of the trainers
The lead trainer was an occupational therapist who was a PhD candidate with 20 years’ clinical experience (LVP). Our Peers—Empowerment and Navigational Supports team members were present and presented including the members of the academic team (PhDs), disability community, and clinical team (communications expert and care coordinator supervisor).
Ongoing training
Ongoing training of navigators is important to ensure that they retain and appropriately apply what they have learned. Based on PHNs feedback, we created opportunities for ongoing review, practice, and support prior to working with participants. Using the Learning Circle Training approach, 61 a highly interactive approach that helps create deeper understanding and integration of content, each PHN reviewed and presented a module of the original training to the rest of the PHN team, thereby enabling them to take ownership of the curriculum and shift from passive to active learners, leaders, and teachers. Peer health navigators also identified topic areas for additional education based on their experiences working with clients, such as mental health first aid and supports. At their request, PHNs participated in the 8-hour mental health first aid training and then received follow-up support related to mental health stigma and community-based resources.
Supervision
Peer health navigation is a demanding job, 55 and the creation of a supportive infrastructure and centralized coordination is needed to ensure success of PHN programs.38,39 We, therefore, created an infrastructure of support and supervision. A clinical coordinator was hired to oversee the work of the PHN team. The clinical coordinator was a licensed occupational therapist or social worker with a minimum of 5 years clinical and supervisory experience and worked closely with the PHNs to support decision making and problem solving, lending professional judgment to PHNs’ developing expertise and confidence.
The clinical coordinator facilitated PHN team meetings every 2 weeks to provide an opportunity for peer support among the PHNs, group problem solving on challenging cases, as well as opportunities for clear and consistent communication to ensure that the manualized OP-ENS intervention was delivered as intended. As PHNs gained skills and confidence in their role, the level of support provided by the clinical coordinator was scaled back and natural leaders within the team emerged. Peer health navigators recognized each other’s strengths and expertise and used each other as resources to fill in gaps in their own knowledge. For example, one PHN was involved in the local disability rights movement and became the go to person related to advocacy issues. The PHNs also recognized that no one person had all the answers, but by working together they could come up with workable strategies and suggestions for most of their participants’ concerns.
Evaluation
There are no standardized metrics to evaluate navigator interventions, indeed the outcomes are determined by the project goals, population, and setting. 40 There are several important areas of consideration when evaluating a PHN intervention including health and health care outcomes chosen to measure the effects of the intervention, as well as whether intervention processes are reviewed and evaluated, and whether PHN trainings effectively build the required knowledge and skill.
Intervention outcomes
The OP-ENS intervention was designed to help PWD break down barriers to health care using a structured process of goal setting, barrier identification and asset mapping, and action planning delivered by a trained PHN with lived experience of disability. Short-term primary outcomes include patient activation and social support and improved health care access and quality. The long-term secondary outcomes include increased global health status and community participation and decreased secondary conditions and high cost utilization. Data collection and outcome management were conducted by a separate collection team who were not involved in the development and implementation of the intervention.
Evaluation of the training
We chose formal and informal evaluation formats and drew from Willock et al 61 who use 4 levels of evaluation of Kirkpatrick. 62 For instance, we inquired about the PHNs’ reaction to the content and delivery of the training after each session (did they like it?), about their perceived learning (did they increase their knowledge, skills, etc), and their perceived ability to use the information and skills learned (can they transfer newly acquired learnings?).
Review of intervention processes
There is a need to evaluate not only the outcomes but the process of a PHN program and PHNs’ satisfaction of this novel and complex intervention. The OP-ENS academic team paid close attention to navigator caseload; for example, how many participants to assign to each navigator, with teams of PHNs sharing caseloads, as well as how much time was spent per participant. The clinical coordinator and OP-ENS team worked closely with the PHNs to ensure that they were supported with the caseload and work allotments and made adjustments wherever possible. Documenting and reporting were important tasks for the PHNs to report the ways they communicated with participants, time spent communicating, as well as general topics coved during those encounters. We offered accessible documentation tools as well as multiple types of documentation and communication options (paper, digital, and audio). The OP-ENS team reviewed these processes often and on an as-needed basis to ensure that barriers were addressed and problem solved in a timely fashion.
Careful attention to each of the 10 key considerations for designing a PHN program enabled the collaborative OP-ENS team of academic, community, and clinical partners to work together in a systematic, evidence-informed fashion and develop a rigorous intervention. Following the step-wise process enabled the team to keep track and support decisions across the collaborative team. The process while beneficial and productive was not without its challenges.
Lessons Learned
This article described the main processes involved in the intervention development of OP-ENS, a peer health navigation program for people with physical disabilities located in Chicago, IL, USA. In this section, we outline lessons learned specific to the intervention development process to help future developers plan community-directed PHN interventions. In a future article, we will outline the lessons we learned from the PHN training and pilot testing of the intervention.
Overall team learning
The OP-ENS intervention development process involved shared learning among all members of the team. We developed OP-ENS during the first 2 years of a 5-year federal research grant. We formed work groups with specific tasks to tailor the PHN training curriculum. As expected, when the academy-community-clinical partners met, each brought unique positions and perspectives based on their particular experiences and professional responsibilities and priorities. During the early phases of our work, it was important to take the time to understand and acknowledge each other’s diverse values, interests, and priorities. For example, the disability community partners ensured that the OP-ENS intervention put the needs of participants at the center of our focus.
Academia, disability community agencies, and clinical providers each move at different paces and are able to prioritize different aspects of their overall workload and the individual project demands very differently. Transparency about and respect for these differences were important for team cohesion and to manage expectations.
Factors in the sociopolitical and economic environment are well outside of the team’s control but can have significant effects on project development, collaborations, and opportunities. While it is not always possible to anticipate these problems, they do need to be attended to and managed within the context of the project. For example, due to state budget cuts, new restrictions were imposed on Medicaid funding. As a result, there were some contentious moments in the project development process. It is important for program developers to understand how these macro-level issues influence the project and its intended objectives without getting bogged down in the politics. Therefore, partners must figure out how to strike a balance between pragmatism, idealism, and scientific rigor.
Team process
Communicating among team members from diverse organizations (academy, disability community, and clinical site) can be challenging. We learned early on that a productive way to organize team meetings was to repeatedly communicate the common goals and purpose of the overall project, ask for team input often, and make decisions only after consulting and including all team members. Regular partnership meetings on the phone or face to face proved significant in the early stages of our development work because team members needed to assert their perspectives privately with the academic team. We learned that while traveling between sites was time-consuming, the goodwill and reinforcement of a shared sense of purpose that it created was worth the investment.
Generally, some of the factors that needed to be considered across and within members of the team were how to balance making the OP-ENS intervention processes implementable and administratively feasible, ensuring that CBPR methodology and research methods remained rigorous while infusing disability rights and Independent Living philosophy. The academic team took the lead to interact with the funder as well as resolve administrative (such as financial, legal, and technical) issues for the team. Negotiating differences, managing expectations, and resolving misunderstanding can be time-consuming and stressful, but ultimately result in a stronger product that is endorsed by all collaborators.
Discussion
People with disabilities are increasingly recognized as a health disparities population, 63 who experience significant barriers to health care access and quality, which in turn negatively impacts their health, function, and social participation. While disability rights activists do the important work of advocating for systems change, PWD need care in the here and now. In an increasingly under-resourced and fragmented health care system, peer support interventions, such as PHN programs, are proving to be effective at empowering and supporting patients to break down barriers to care.
Our community-academic-clinical partnership has sought to build on the legacy of PHN development and implementation programs to address the community-identified and evidence-supported barriers to care. Through a systematic and collaborative development process, we tailored best practices in PHN programming to address the needs of people with physical disabilities. While more research is clearly needed to determine the feasibility, acceptability, efficacy, scalability, and sustainability of OP-ENS, or indeed any PHN intervention, we have created an intervention and training that reflects and embraces community needs, priorities, and values.
While the community-engaged and collaborative team processes are not always smooth or easy, 64 deep commitment to the project goals and purposes, attention to process, and a focus on equitable relationships have led to the development of a program that is responsive to community needs. By sharing how we designed the OP-ENS intervention, we hope to inform the field of health care navigation of key considerations that may lead to rigorous navigation programs. Future developers can use our process to develop navigation intervention to serve community-dwelling adults with disabilities.
Conclusions
The co-creation of the OP-ENS PHN intervention to address the health care needs of PWD using CBPR and research equity principles was grounded on decade-long partnerships among the academic and community members, with the shared goal of designing solutions to systemic problems within the US Medicaid system by actively collaborating with relevant community stakeholders. This community-engaged approach to research and scholarship presents unique opportunities to breakdown research and clinical silos to address the health care disparities that PWD continue to experience today.
Footnotes
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship and/or publication of this article: Funding for the project was received from the National Institute on Disability, Independent Living, and Rehabilitation Research (90RT5027).
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: SM - Designed the original study and obtained funding, framed and drafted manuscript.
CP - Designed the original study, framed and co-authored manuscript.
JPR - Community co-investigator, conceptualized the original study, provided substantive input on manuscript.
KT - Provided substantive input on manuscript.
JT - Conceptualized the OP-ENS peer health navigator program, provided substantive input on manuscript.
LV - Conceptualized the OP-ENS peer health navigator program, provided substantive input on manuscript.
TW - Community co-investigator,, conceptualized the original study, provided substantive input on manuscript.
References
- 1. Hendricks A. UN convention on the rights of persons with disabilities. Eur J Health L. 2007;14:273–298. [DOI] [PubMed] [Google Scholar]
- 2. World Health Organization, World Bank. World Report on Disability. Geneva, Switzerland: WHO; 2011. [Google Scholar]
- 3. McDoom MM, Koppelman E, Drainoni M-L. Barriers to accessible health care for Medicaid eligible people with disabilities: a comparative analysis. J Disabil Policy Stud. 2014;25:154–163. [Google Scholar]
- 4. Kirschner KL, Breslin ML, Iezzoni LI. Structural impairments that limit access to health care for patients with disabilities. JAMA. 2007;297:1121–1125. [DOI] [PubMed] [Google Scholar]
- 5. Reichard A, Stransky M, Phillips K, McClain M, Drum C. Prevalence and reasons for delaying and foregoing necessary care by the presence and type of disability among working-age adults. Disabil Health J. 2017;10:39–47. [DOI] [PubMed] [Google Scholar]
- 6. Pendo E. Reducing disparities through health care reform: disability and accessible medical equipment. Utah L Rev. 2010;4:1057. [Google Scholar]
- 7. Iezzoni LI, Long-Bellil LM. Training physicians about caring for persons with disabilities: “Nothing about us without us!” Disabil Health J. 2012;5:136–139. [DOI] [PubMed] [Google Scholar]
- 8. Kirschner KL, Curry RH. Educating health care professionals to care for patients with disabilities. JAMA. 2009;302:1334–1335. [DOI] [PubMed] [Google Scholar]
- 9. Kirschner KL, Breslin ML, Iezzoni LI, Sandel E. Attending to inclusion: people with disabilities and health-care reform. PM R. 2009;1:957–963. [DOI] [PubMed] [Google Scholar]
- 10. Mudrick NR, Breslin ML, Liang M, Yee S. Physical accessibility in primary health care settings: results from California on-site reviews. Disabil Health J. 2012;5:159–167. [DOI] [PubMed] [Google Scholar]
- 11. Kroll T, Jones GC, Kehn M, Neri MT. Barriers and strategies affecting the utilisation of primary preventive services for people with physical disabilities: a qualitative inquiry. Health Soc Care Community. 2006;14:284–293. [DOI] [PubMed] [Google Scholar]
- 12. Gimm G, Wood E, Zanwar P. Access to preventive services for working-age adults with physical limitations. Arch Phys Med Rehabil. 2017;98:2442–2448. [DOI] [PubMed] [Google Scholar]
- 13. Chevarley FM, Thierry JM, Gill CJ, Ryerson AB, Nosek MA. Health, preventive health care, and health care access among women with disabilities in the 1994-1995 national health interview survey, supplement on disability. Womens Health Iss. 2006;16:297–312. [DOI] [PubMed] [Google Scholar]
- 14. Horner-Johnson W, Dobbertin K, Lee JC, Andresen EM. Disparities in health care access and receipt of preventive services by disability type: analysis of the medical expenditure panel survey. Health Serv Res. 2014;49:1980–1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lofters A, Guilcher S, Maulkhan N, Milligan J, Lee J. Patients living with disabilities: the need for high-quality primary care. Can Fam Physician. 2016;62:e457–e464. [PMC free article] [PubMed] [Google Scholar]
- 16. Lagu T, Hannon NS, Rothberg MB, et al. Access to subspecialty care for patients with mobility impairment: a survey. Ann Intern Med. 2013;158:441–446. [DOI] [PubMed] [Google Scholar]
- 17. Mahmoudi E, Meade MA. Disparities in access to health care among adults with physical disabilities: analysis of a representative national sample for a ten-year period. Disabil Health J. 2015;8:182–190. [DOI] [PubMed] [Google Scholar]
- 18. Goodridge D, Rogers M, Klassen L, et al. Access to health and support services: perspectives of people living with a long-term traumatic spinal cord injury in rural and urban areas. Disabil Rehabil. 2015;37:1401–1410. [DOI] [PubMed] [Google Scholar]
- 19. Brucker DL, Houtenville AJ. People With Disabilities in the United States. Arch Phys Med Rehabil. 2015;96:771–774. [DOI] [PubMed] [Google Scholar]
- 20. Mitra S, Palmer M, Kim H, Mont D, Groce N. Extra costs of living with a disability: a review and agenda for research. Disabil Health J. 2017;10:475–484. [DOI] [PubMed] [Google Scholar]
- 21. Iezzoni LI. Blocked. Health Affairs. 2008;27:203–209. [DOI] [PubMed] [Google Scholar]
- 22. Iezzoni LI. Public health goals for persons with disabilities: looking ahead to 2020. Disabil Health J. 2009;2:111–115. [DOI] [PubMed] [Google Scholar]
- 23. Iezzoni LI. Eliminating health and health care disparities among the growing population of people with disabilities. Health Aff. 2011;30:1947–1954. [DOI] [PubMed] [Google Scholar]
- 24. Rowland M, Peterson-Besse J, Dobbertin K, Walsh ES, Horner-Johnson W. Health outcome disparities among subgroups of people with disabilities: a scoping review. Disabil Health J. 2014;7:136–150. [DOI] [PubMed] [Google Scholar]
- 25. Panko Reis J, Breslin M, Iezzonl L, Kirschner K. It Takes More Than Ramps to Solve the Crisis in Healthcare for People with Disabilities. Chicago, IL: Rehabilitation Institute of Chicago; 2004. [Google Scholar]
- 26. Wallerstein N, Duran B. Community-based participatory research contributions to intervention research: the intersection of science and practice to improve health equity. Am J Public Health. 2010;100:S40–S46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mitra M, Bogen K, Long-Bellil LM, Heaphy D. Unmet needs for home and community-based services among persons with disabilities in Massachusetts. Disabil Health J. 2011;4:219–228. [DOI] [PubMed] [Google Scholar]
- 28. World Health Organization. Community Health Workers: What Do We Know About Them. Geneva, Switzerland: WHO Department of Human Resources for Health; 2007. [Google Scholar]
- 29. Olaniran A, Smith H, Unkels R, Bar-Zeev S, van den Broek N. Who is a community health worker? a systematic review of definitions. Glob Health Action. 2017;10:1272223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Koester KA, Morewitz M, Pearson C, et al. Patient navigation facilitates medical and social services engagement among HIV-infected individuals leaving jail and returning to the community. AIDS Patient Care STDS. 2014;28:82–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kelly E, Fulginiti A, Pahwa R, Tallen L, Duan L, Brekke JS. A pilot test of a peer navigator intervention for improving the health of individuals with serious mental illness. Community Ment Health J. 2014;50:435–446. [DOI] [PubMed] [Google Scholar]
- 32. Mollica MA, Nemeth LS, Newman SD, Mueller M, Sterba K. Peer navigation in African American breast cancer survivors. Patient Relat Outcome Meas. 2014;5:131–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ramirez A, Perez-Stable E, Penedo F, et al. Reducing time-to-treatment in underserved Latinas with breast cancer: the six cities study. Cancer. 2014;120:752–760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Maxwell AE, Jo AM, Crespi CM, Sudan M, Bastani R. Peer navigation improves diagnostic follow-up after breast cancer screening among Korean American women: results of a randomized trial. Cancer Causes Control. 2010;21:1931–1940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Houlihan BV, Brody M, Everhart-Skeels S, et al. Randomized trial of a peer-led, telephone-based empowerment intervention for persons with chronic spinal cord injury improves health self-management. Arch Phys Med Rehabil. 2017;98:1067.e1–1076.e1. [DOI] [PubMed] [Google Scholar]
- 36. Shangani S, Escudero D, Kirwa K, Harrison A, Marshall B, Operario D. Effectiveness of peer-led interventions to increase HIV testing among men who have sex with men: a systematic review and meta-analysis. AIDS Care. 2017;29:1003–1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Corrigan PW, Pickett S, Batia K, Michaels PJ. Peer navigators and integrated care to address ethnic health disparities of people with serious mental illness. Soc Work Public Health. 2014;29:581–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kelly E, Duan L, Cohen H, Kiger H, Pancake L, Brekke J. Integrating behavioral healthcare for individuals with serious mental illness: a randomized controlled trial of a peer health navigator intervention. Schizophr Res. 2017;182:135–141. [DOI] [PubMed] [Google Scholar]
- 39. Natale-Pereira A, Enard KR, Nevarez L, Jones LA. The role of patient navigators in eliminating health disparities. Cancer. 2011;117:3543–3552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. DeGroff A, Coa K, Morrissey KG, Rohan E, Slotman B. Key considerations in designing a patient navigation program for colorectal cancer screening. Health Promot Pract. 2014;15:483–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Minkler M, Wallerstein N. Community-based Participatory Research for Health: From Process to Outcomes. Hoboken, NJ: John Wiley & Sons; 2011. [Google Scholar]
- 42. Charlton JI. Nothing about Us without Us: Disability Oppression and Empowerment. Berkeley, CA: University of California Press; 1998. [Google Scholar]
- 43. DeJong G. Independent living: from social movement to analytic paradigm. Arch Phys Med Rehabil. 1979;60:435–446. [PubMed] [Google Scholar]
- 44. Steinberg ML, Fremont A, Khan DC, et al. Lay patient navigator program implementation for equal access to cancer care and clinical trials: essential steps and initial challenges. Cancer. 2006;107:2669–2677. [DOI] [PubMed] [Google Scholar]
- 45. Marmot M. Social determinants of health inequalities. The Lancet. 2005;365:1099–1104. [DOI] [PubMed] [Google Scholar]
- 46. Gupta J, Taff SD. The illusion of client-centred practice. Scand J Occup Ther. 2015;22:244–251. [DOI] [PubMed] [Google Scholar]
- 47. Durocher E, Kinsella EA, Ells C, Hunt M. Contradictions in client-centred discharge planning: through the lens of relational autonomy. Scand J Occup Ther. 2015;22:293–301. [DOI] [PubMed] [Google Scholar]
- 48. Simoni JM, Franks JC, Lehavot K, Yard SS. Peer interventions to promote health: conceptual considerations. Am J Orthopsychiatry. 2011;81:351–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Uchino BN. Social support and health: a review of physiological processes potentially underlying links to disease outcomes. J Behav Med. 2006;29:377–387. [DOI] [PubMed] [Google Scholar]
- 50. Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31:143–164. [DOI] [PubMed] [Google Scholar]
- 51. Altman D, Frist WH. Medicare and Medicaid at 50 years: perspectives of beneficiaries, health care professionals and institutions, and policy makers. JAMA. 2015;314:384–395. [DOI] [PubMed] [Google Scholar]
- 52. Statistics D. Disability statistics: online resource for U.S. Disabil Stat. 2016. https://libguides.umn.edu/az.php?t=30801.
- 53. Ustjanauskas AE, Bredice M, Nuhaily S, Kath L, Wells KJ. Training in patient navigation: a review of the research literature. Health Promot Pract. 2016;17:373–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Mathers J, Taylor R, Parry J. The challenge of implementing peer-led interventions in a professionalized health service: a case study of the national health trainers service in England. Milbank Q. 2014;92:725–753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Meade CD, Wells KJ, Arevalo M, et al. Lay navigator model for impacting cancer health disparities. J Cancer Educ. 2014;29:449–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Calhoun EA, Whitley EM, Esparza A, et al. A national patient navigator training program. Health Promot Pract. 2010;11:205–215. [DOI] [PubMed] [Google Scholar]
- 57. Lorhan S, Wright M, Hodgson S, van der Westhuizen M. The development and implementation of a volunteer lay navigation competency framework at an outpatient cancer center. Support Care Cancer. 2014;22:2571–2580. [DOI] [PubMed] [Google Scholar]
- 58. Samaras AT, Murphy K, Nonzee NJ, et al. Community-campus partnership in action: lessons learned from the DuPage county patient navigation collaborative. Prog Community Health Partnersh. 2014;8:75–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Wells KJ, Valverde P, Ustjanauskas AE, Calhoun EA, Risendal BC. What are patient navigators doing, for whom, and where? a national survey evaluating the types of services provided by patient navigators. Patient Educ Couns. 2018;101:285–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Mezirow J. Transformative Dimensions of Adult Learning. Bristol, UK: ERIC; 1991. [Google Scholar]
- 61. Willock RJ, Mayberry RM, Yan F, Daniels P. Peer training of community health workers to improve heart health among African American women. Health Promot Pract. 2015;16:63–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Kirkpatrick DL. Implementing the Four Levels: A Practical Guide for Effective Evaluation of Training Programs. Oakland, CA: Berrett-Koehler Publishers; 2009. [Google Scholar]
- 63. Krahn GL, Walker DK, Correa-De-Araujo R. Persons with disabilities as an unrecognized health disparity population. Am J Public Health. 2015;105:S198–S206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Connected Communities. Community-based Participatory Research: Ethical Challenges. Durham, NC: Community Research Team, Centre for Social Justice and Community Action, Durham University; 2011. https://www.dur.ac.uk/resources/beacon/CCDiscussionPapertemplateCBPRBanksetal7Nov2011.pdf. Accessed March 2, 2014. [Google Scholar]