Abstract
Background
There is currently no established consensus on best treatment for complex proximal humerus fractures (PHFs) in the elderly. Reverse total shoulder arthroplasty (RTSA) is a viable option in this population but many times is used as a salvage procedure.
Methods
A systematic review of studies comparing RTSA as a primary treatment for PHF versus as a salvage procedure following failed open reduction internal fixation (ORIF), humeral intramedullary nailing, hemiarthroplasty (HA) or non-operative treatment was conducted using PRISMA guidelines. Pooled outcomes and sub-group analyses assessing range of motion, patient reported outcomes and complications were examined using RevMan.
Results
Five articles were included in final analysis with 104 patients in the primary RTSA group and 147 in the salvage RTSA group compromising 251 total patients. Primary RTSA had a statistically significant advantage in range of motion (forward flexion and external rotation), patient reported outcomes, and complications compared to salvage RTSA.
Conclusions
Based on the best available evidence, primary RTSA may result in slightly better patient reported outcomes, range of motion and a lower rate of complication when compared to salvage RTSA. Further high-quality prospective studies are needed to confirm the findings of the current review.
Keywords: Failed fixation, malunion, nonunion, arthroplasty, reverse total shoulder
Introduction
Proximal humerus fractures (PHFs) account for approximately six percent of all adult fractures and disproportionately affect older patients and women. 1 As the population ages, the incidence of PHFs is projected to triple by 2030. 2 While most PHFs are nondisplaced or one part fractures that can be treated non-operatively,3,4 the optimal treatment strategy for more complex fractures (e.g., three and four-part) remains unclear. 5
Traditionally, open reduction and internal fixation (ORIF) or hemiarthroplasty (HA) have been the surgical treatment of choice, but they have many potential complications such as nonunion and poor tuberosity healing. 6 While many times HA treatment provides excellent outcomes, when complications arise they are frequently complex. This exacerbated in the elderly population where bone quality is diminished, and comorbidities are common. Consequently, achieving adequate fixation in this population is technically challenging as low bone mineral density is one of the biggest predictors of fixation failure. 7 Since the controversial Proximal Fracture of the Humerus: Evaluation by Randomization (ProFHER) trial in 2015 suggested non-operative treatment of these injuries is equivalent to surgery, 8 identifying both surgical candidates and optimal fixation technique continues to be contentious with no consensus on best treatment strategy.
Reverse total shoulder arthroplasty (RTSA) has provided surgeons with a reliable option for managing complex PHFs. Traditionally, RTSA was used primarily as a salvage procedure after failed HA, ORIF, or non-operative fracture sequelae when no other options remained.9–24 However, these patients frequently experience only mild improvements in their activities of daily living (ADLs)15,25 and face a high risk of complications.24,26,27 Several systematic reviews have suggested that RTSA may be superior to HA for acute PHFs28–30 and in recent years RTSA has become an increasingly popular initial option for these injuries.31–35 As such, the purpose of this systematic review was to compare outcomes of RTSA used as a primary versus salvage procedure for complex PHFs among the elderly population.
Methods
We conducted a systematic review in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. 36
Literature Search
A literature search of EMBASE, MEDLINE, PubMed and the Cochrane trials registry was conducted using the following keywords in combination: “shoulder fractur*”, “humer* fractur*, proximal”, and “reverse adj2 shoulder” for MEDLINE and “reverse shoulder arthroplasty”, “proximal humerus”, and “fracture” for EMBASE and Cochrane for studies published between 2015-2020. Systematic reviews from our search were retrieved, and their references were reviewed for any additional studies that could be included.
Eligibility Criteria
All studies comparing RTSA as a primary treatment for PHF with RTSA as a salvage procedure for failed treatment of PHF were eligible for inclusion. Failed treatment included non-operative, hemiarthroplasty, intramedullary nailing, or ORIF. Only prospective and retrospective comparative studies evaluating functional outcomes (e.g., simple shoulder test, constant score, American Shoulder and Elbow Surgeons [ASES] score) were included. Study inclusion criteria included minimum of 12-month follow-up and a minimum of 10 patients in each treatment group. A study was excluded if data from the same patients were included in another eligible study with longer follow-up. Conference abstracts were also excluded.
Study Selection
Two reviewers screened the titles and abstracts generated by the literature search for eligibility. If there was any uncertainty or ambiguity regarding eligibility, the study was included for full-text review. The reviewers independently assessed each full report to determine whether inclusion criteria were met. Disagreements were resolved by discussion with the senior author, when necessary.
Data Extraction
Two reviewers extracted relevant data from each included study and recorded them into Microsoft Excel worksheets. Data collected in the worksheets included first author, journal, year of publication, level of evidence, number of patients, follow-up duration, average age of patient, definition of proximal humerus fracture and outcomes observed. A comments section was included for any other relevant data pertinent to each study. Common outcome data were entered into a meta-analysis software package 37 for pooled analysis.
Assessment of Risk of Bias in Eligible Studies
The Newcastle-Ottawa Scale (NOS) 38 was used to evaluate the quality of eligible prospective and retrospective cohort studies. The NOS assesses each study on 3 domains: selection, comparability, and outcome. Two reviewers independently assessed the methodological quality of eligible studies. Any disagreements were resolved with consensus discussion.
Statistical Methods
Descriptive statistics were calculated with categorical data presented as frequency with percentages and continuous data as mean ± standard deviation (SD). Weighted means with their corresponding SDs were calculated for all parameters. For studies that did not report the mean and SD directly, these values were imputed from the p-value, confidence interval (CI) and range using well-established statistical techniques.37,39 Mean differences were calculated for continuous outcomes. Ninety-five percent CIs were reported for all point estimates. Pooled estimates were calculated using Review Manager (RevMan) 5.3 (Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014). 37 A funnel plot was used to assess for publication bias. An a priori subgroup analyses was planned to examine the differences in range of motion (ROM) and patient reported outcome measures (data permitting) following primary RTSA versus RTSA as a salvage after each of: ORIF, HA and non-operative treatment (resulting in non-union or malunion). 37
Results
Literature Search and Study Characteristics
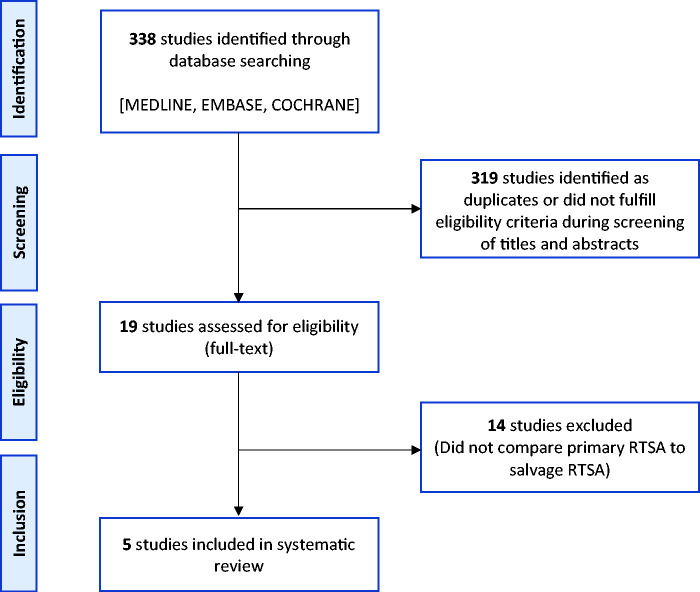
The results of our comprehensive search, the selection process, and the number of studies excluded with the corresponding rationale are depicted in Figure 1. Five studies were identified that satisfied all inclusion and exclusion criteria.26,40–43 Three studies were retrospective cohorts26,42,43 while the other two were matched case-control.40,41 All studies were published between 2016–2020. A total of 147 patients underwent RTSA as a salvage procedure (78% female), while 104 patients underwent RTSA for acute PHF (79% female) for a total of 251 patients. Mean follow-up time was 31.8 months (SD ± 2.5) and mean age was 73.0 years (SD ± 2.1). Two of the studies included failed hemiarthroplasty, ORIF, and non-operative treatment as part of the salvage group,41,42 one included failed hemiarthroplasty, ORIF and intramedullary nailing, 43 and two studies only included patients who failed ORIF.26,40 Common outcomes between the studies included forward flexion,26,40–43 external rotation,26,40–43 ASES,26,41,42 UCLA score,40,41 and Constant Score.40,41,43 The characteristics of each study are summarized in Table 1.
Figure 1.
Flow diagram summarizing the literature search, screening, and selection process. RTSA, reverse total shoulder arthroplasty.
Table 1.
Baseline Characteristics for All Included Studies.
| Author | Journal | Year | Sample Size (N) | Primary RTSA (N) | Age, Years (SD) | Follow-Up, Months (SD) | Comparison | Functional Outcomes |
|---|---|---|---|---|---|---|---|---|
| Dezfuli | JSES | 2016 | 49 | 13 | 71.0 (1.73) | 32 (1.7) | Failed Non-op (13)Failed HA (12)Failed ORIF (11) | ASESConstantSF-12SPADISSTUCLAROM |
| Katthagen | Obere Extremität | 2020 | 51 | 28 | 73 (2.16) | 18 (2.9) | Failed ORIF (9)Failed HA (9)Failed locked intramedullary nail (5) | ConstantDASHSSV |
| Sebastia-Forcada | JOT | 2017 | 60 | 30 | 73.2 (2.04) | 30 (3.0) | Failed ORIF (30) | ConstantDASHUCLA |
| Seidl | ABJS | 2017 | 47 | 15 | 72.7 (2.48) | 45 (1.3) | Failed ORIF (15)Failed HA (10)Failed Non-op (7) | ASESSANESST |
| Shannon | JSES | 2016 | 44 | 18 | 75 (2.16) | 36 (3.5) | Failed ORIF (26) | ASESROM |
Abbreviations: RTSA, reverse total shoulder arthroplasty; SD, standard deviation; JSES, Journal of Shoulder and Elbow Surgery; HA, hemiarthroplasty; ORIF, open reduction internal fixation; ASES, American Shoulder and Elbow Surgeon score; SF-12, 12-item short form health survey; SPADI, shoulder pain and disability index; SST, simple shoulder test; UCLA, University of California at Los Angeles score; ROM, range of motion; DASH, disabilities of the arm, shoulder hand score; SSV, subjective shoulder value; JOT, Journal of Orthopaedic Trauma; ABJS, Archives of Bone and Joint Surgery; SANE, single assessment numerical evaluation; HO, heterotopic ossification.
Study Quality
The studies involved were comparable with respect to important demographic variables (i.e. age, follow-up, definition of fracture). Overall study quality was moderate to high (see Supplemental Digital Content 1, which provides complete results of the NOS). Funnel plots were used to assess for publication bias and were found to be symmetrical (see Supplemental Digital Content 2).
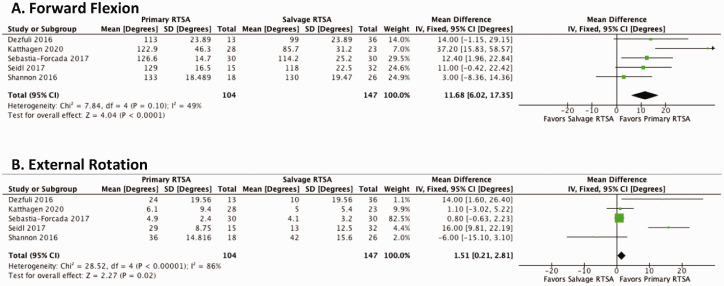
Range of Motion
The mean forward flexion (FF) and external rotation (ER) were both significantly higher in the primary RTSA group compared to the salvage RTSA group with a mean difference (MD) of 11.7 degrees for FF (95% CI, 6.0–17.4; P < 0.0001) (Figure 2(A)) and 1.5 for ER (95% CI 0.2–2.8; P = 0.02) (Figure 2(B)). Subgroup analyses demonstrated significantly greater FF and ER with primary RTSA compared to RTSA after ORIF (MD, 8.9° FF [95% CI, 1.5 to 16.3]; P = 0.02) (MD, 6.0° ER [95% CI, 2.2 to 9.8]; P = 0.002) or HA (MD, 18.1° FF [95% CI, 6.1 to 30.1]; P = 0.003) (MD, 18.5° ER [95% CI, 7.4 to 29.5]; P = 0.001). When comparing Primary RTSA to RTSA following non-operative treatment, primary RTSA was found to have significantly greater ER (MD, 5.5° [95% CI, 2.6 to 8.4]; P = 0.0002) but no difference in FF (MD, 9.8° [95% CI, −7.7 to 27.2]; P = 0.27).
Figure 2.
Pooled mean difference of range of motion in patients undergoing primary RTSA compared with salvage RTSA. A, forward flexion; B, external rotation. RTSA, reverse total shoulder arthroplasty; SD, standard deviation; CI, confidence interval.
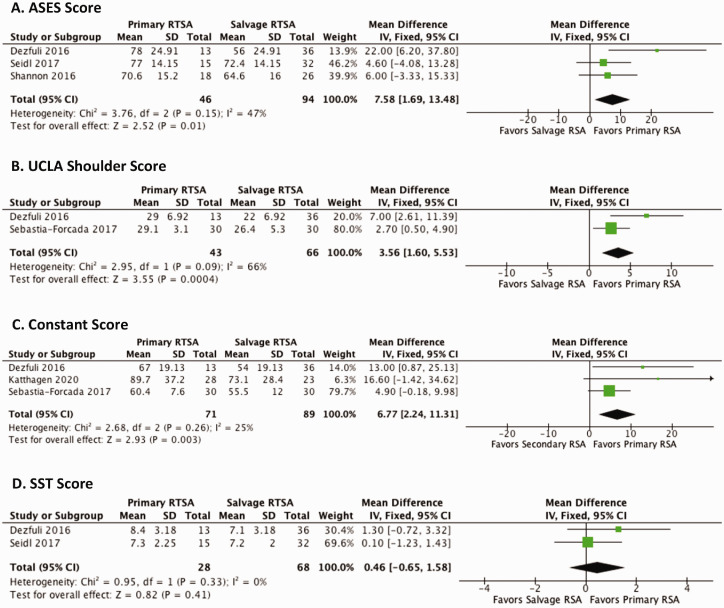
Functional Outcomes
Primary RTSA for PHFs was found to have significantly higher ASES (MD, 7.6; CI, 1.7–13.5; P = 0.01) (Figure 3(A)), UCLA (MD, 3.6; 95% CI, 1.6–5.5; P = 0.0004) (Figure 3(B)) and Constant (MD, 6.8; 95% CI, 2.2–11.3; P = 0.003) (Figure 3(C)) scores when compared to salvage RTSA for failed treatment of PHFs. There was no statistically significant difference between the groups for the SST (Figure 3(D)).
Figure 3.
Pooled mean difference of qualitative function measures in patients undergoing primary RTSA compared with salvage RTSA. A, American Shoulder and Elbow Surgeons Shoulder Score (ASES); B, UCLA Shoulder Score; C, Constant Score; D, Simple Shoulder Test (SST). RTSA, reverse total shoulder arthroplasty; SD, standard deviation; CI, confidence interval.
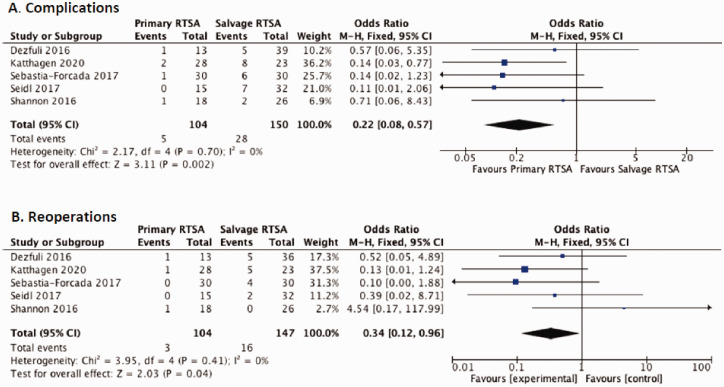
Complications
Breakdown of specific complications is included in Table 2. The overall complication rate in the primary RTSA and salvage RTSA groups was 4.8% (5/104) and 18.7% (28/150), respectively. This included five intraoperative complications in the salvage group and one in the primary group. The odds of having a complication were 78% lower amongst those undergoing RTSA primarily versus as a salvage procedure (P = 0.002) (Figure 4(A)). The most common complications in the salvage group included dislocation (6), periprosthetic fracture (5), infection (3), implant loosening (3), cortical perforation (2) and component malposition (2).
Table 2.
Summary of Complications.
| Complication | Primary RTSA(N, [%]) | Salvage RTSA(N, [%]) |
|---|---|---|
| Intraoperative | ||
| Humerus fracture | 1 (1.0) | 0 (0) |
| Cortical perforation | 0 (0) | 4 (2.7) |
| Retained cement | 0 (0) | 1 (0.7) |
| Postoperative | ||
| Periprosthetic humerus fracture | 1 (1.0) | 5 (3.3) |
| Wound infection | 2 (1.9) | 3 (2.0) |
| Component loosening | 0 (0) | 3 (2.0) |
| Dislocation | 1 (1.0) | 6 (4.0) |
| Major hematoma | 0 (0) | 2 (1.3) |
| Axillary nerve injury | 0 (0) | 1 (0.7) |
| Acromial fracture | 0 (0) | 1 (0.7) |
| Extensive heterotopic ossification | 0 (0) | 1 (0.7) |
| Nickel allergy | 0 (0) | 1 (0.7) |
| Total complications | 5 (4.8) | 28 (18.7) |
Figure 4.
Pooled odds ratio for (A) complications and (B) reoperations among patients undergoing primary RTSA compared with salvage RTSA. RTSA, reverse total shoulder arthroplasty; CI, confidence interval.
Reoperation
Reoperation was defined as any subsequent surgical procedure that occurred as a direct result of the initial operation including incision and drainage for infection or hematoma removal. If the text did not explicitly state a procedure occurred, it was not counted. The overall reoperation rate in the primary RTSA group was 2.9% (3/105) and 10.7% (16/150) in the salvage group (P = 0.04) (Figure 4(B)).
Discussion
The results of the current systematic review demonstrate that primary RTSA may result in greater forward flexion, fewer complications and superior functional outcomes when compared to RTSA as a salvage procedure. The clinical significance of these results is especially timely as the ProFHER trial, 8 which reported no significant difference in outcome between operative and non-operative management of displaced proximal humerus fractures involving the surgical neck, continues to receive widespread media attention, despite well-documented concerns over study methodology.44,45 Consequently, this may result in a greater proportion of patients being inappropriately treated non-operatively initially, leading to a potential increase in the rate of fracture sequalae such as malunion and non-union. 46
An exploratory subgroup analyses of primary RTSA compared to salvage RTSA after either failed HA or ORIF for PHFs demonstrated that patients may have better ROM and functional outcomes with primary RTSA in both subgroups. Two recent studies have noted that patients undergoing salvage RTSA for failed non-operative management may have better outcomes when compared to those undergoing RTSA for failed HA of PHFs.47,48 These findings would suggest that patients at high risk of failing HA may fare better with non-operative management initially with the option to undergo RTSA in the future, if indicated. While this review found statistical significance favoring primary RTSA compared to RTSA as a salvage procedure, the clinical significance of these results is less clear.
The mean forward flexion among the primary RTSA group was 125° compared to 110° in the salvage RTSA group. Based on previous reports, it has been noted that 120° of forward flexion is required to perform the majority of ADLs that involve the shoulder. 49 Therefore, the 15° mean difference between the primary and salvage RTSA group demonstrated in the current review may represent an important clinical difference. When considering external rotation (ER), studies evaluating functional ER measure ROM with the shoulder abducted 90° and have found approximately 60 ± 10° is necessary to perform most ADLs. 49 The studies included in this review measured ER with arm at the side with neither primary nor salvage RTSA coming within 25° of this threshold (30.3 and 19.9, respectively). However, Simovitch and colleagues found that among patients undergoing RTSA, the minimal clinically important difference (MCID) for active external rotation was −5.3 ± 3.1 degrees, suggesting that restoration of external rotation may not be as important as pain relief, joint stability, and a low complication rate when evaluating the success of RTSA in this patient population. 50
Patients in the primary RTSA group had statistically significantly higher Constant, ASES, and UCLA scores. However, it is difficult to determine whether these differences are clinically important. The MCID for the Constant score among patients undergoing RTSA for rotator cuff arthropathy or glenohumeral arthritis has been reported to be as high as 8.0 51 and as low as 5.7. 50 As such, the observed mean difference of 6.1 among the primary RTSA cohort in the current review may be clinically significant. 50 The mean difference in ASES of 7.6 observed between the primary RTSA and salvage RTSA groups in the current study closely approximates the previously reported MCIDs of 8.4 and 10.3 but falls short of achieving clinical significance.50,52 Finally, the observed mean difference in UCLA score (3.56) between the primary and salvage groups did not fall within the reported MCID of 7.0. 50 It is important to note that among the few published studies that evaluate the MCID for the aforementioned outcome measures in patients with RTSA, the majority do so for the rotator cuff tear arthropathy population. Extrapolating these findings to patients receiving RTSA for PHFs may overestimate the difference required for clinical significance in the trauma population and even small differences may be important to these patients given the difficulty in achieving good outcomes in these complex fractures.
It has been reported that the initial costs associated with undergoing HA and RTSA are approximately $30,000 and $55,000 respectively.53,54 However, these costs can vary significantly depending on the cost of the implant (between $1,000-10,000). 55 Several recent studies have found RTSA to be more cost-effective over the long term with an incremental cost-effectiveness ratio of <$14,000 per quality adjust life year (QALY) gained compared to HA.54,55 In fact, Osterhoff et al. noted that the cost-effectiveness of RTSA is similar to other highly successful orthopaedic procedures such as total hip and knee arthroplasty. 55
In the current review patients undergoing primary RTSA were found to have a significantly lower rate of complication when compared to salvage RTSA. Saltzman and colleagues reported similar findings with primary RTSA and revision RTSA having complication rates of 25% and 69%, respectively. 56 Given the cost-effectiveness, lower rate of complication and superior functional outcomes of primary compared to salvage RTSA, the use of RTSA as a first line treatment option among patients who are at increased risk of treatment failure, such as older patients, those with osteoporosis, varus displacement and medial comminution may be justified.7,57
This study has several limitations. First, the results of the current review are based on the results of five small comparative studies. Second, all the studies included in this review were retrospective in nature. Therefore, the conclusions are subject to the inherent biases associated with these types of studies, such as selection bias. For example, patients undergoing acute RTSA may have had more complex fracture patterns, therefore leading to a possible underestimation of our findings. This is compounded by the fact that only two of the five studies specified the type of fracture pattern for their inclusion criteria.26,40 Furthermore, none of the studies commented on surgeon experience with RTSA in the trauma setting as this could have affected the outcome. It has previously been noted that RTSA done by less experienced surgeons can result in a higher rate of complications. 58 Additionally, the time from index to salvage procedure was not reported in the majority of included studies; a shorter interval would suggest that primary RTSA may be worthwhile among those patients who are at higher risk of early failure. Finally, potential confounding factors such as comorbidities and bone quality were not evaluated in the current review due to the lack of reporting among included studies.
Conclusion
Based on the current available evidence, elderly patients with displaced PHF may have significantly greater range of motion, a lower risk of complications, and slightly better patient reported outcomes with primary RTSA compared to those undergoing RTSA as a salvage procedure. The clinical significance of these results is less clear and requires additional prospective studies to confirm our findings.
Supplemental Material
Supplemental material, sj-pdf-1-sea-10.1177_2471549220949731 for Primary Versus Salvage Reverse Total Shoulder Arthroplasty for Displaced Proximal Humerus Fractures in the Elderly: A Systematic Review and Meta-analysis by Patrick A Nelson MD Changyow C MD Tjong KVehniah Kwan MD Michael A Terry MD Ujash Sheth MD, MSc, FRCSC in Journal of Shoulder and Elbow Arthroplasty
Authors’ Note
Presented in part at the 2019 Canadian Orthopaedic Association Annual Meeting, Montreal, Quebec, June 22, 2019.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Patrick A Nelson https://orcid.org/0000-0002-5484-8336
Supplemental Material
Supplemental material for this article is available online.
References
- 1.Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006; 37(8):691–697. [DOI] [PubMed] [Google Scholar]
- 2.Palvanen M, Kannus P, Niemi S, et al. Update in the epidemiology of proximal humeral fractures. Clin Orthop Relat Res. 2006; 442:87–92. [DOI] [PubMed] [Google Scholar]
- 3.Koval KJ, Gallagher MA, Marsicano JG, et al. Functional outcome after minimally displaced fractures of the proximal part of the humerus. J Bone Joint Surg Am. 1997; 79:203–207. [DOI] [PubMed] [Google Scholar]
- 4.Lee SH, Dargent-Molina P, Bréart G. Risk factors for fractures of the proximal humerus: results from the EPIDOS prospective study. J Bone Miner Res. 2002; 17(5):817–825. [DOI] [PubMed] [Google Scholar]
- 5.Handoll HH, Brorson S. Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev. 2015: Cd000434:11–13. [DOI] [PubMed] [Google Scholar]
- 6.Boileau P, Krishnan SG, Tinsi L, et al. Tuberosity malposition and migration: reasons for poor outcomes after hemiarthroplasty for displaced fractures of the proximal humerus. J Shoulder Elbow Surg. 2002; 11(5):401–412. [DOI] [PubMed] [Google Scholar]
- 7.Krappinger D, Bizzotto N, Riedmann S, et al. Predicting failure after surgical fixation of proximal humerus fractures. Injury 2011; 42:1283–1288. [DOI] [PubMed] [Google Scholar]
- 8.Rangan A, Handoll H, Brealey S; PROFHER Trial Collaborators et al. Surgical vs nonsurgical treatment of adults with displaced fractures of the proximal humerus: the PROFHER randomized clinical trial. JAMA. 2015; 313(10):1037–1047. [DOI] [PubMed] [Google Scholar]
- 9.Grubhofer F, Wieser K, Meyer DC, et al. Reverse total shoulder arthroplasty for failed open reduction and internal fixation of fractures of the proximal humerus. J Shoulder Elbow Surg. 2017; 26(1):92–100. [DOI] [PubMed] [Google Scholar]
- 10.Hattrup SJ, Waldrop R, Sanchez-Sotelo J. Reverse total shoulder arthroplasty for posttraumatic sequelae. J Orthopaed Trauma. 2016; 30:e41–e47. [DOI] [PubMed] [Google Scholar]
- 11.Holschen M, Siemes MK, Witt KA, et al. Five-year outcome after conversion of a hemiarthroplasty when used for the treatment of a proximal humeral fracture to a reverse total shoulder arthroplasty. Bone Joint J 2018; 100-B:761–766. [DOI] [PubMed] [Google Scholar]
- 12.Hussey MM, Hussey SE, Mighell MA. Reverse shoulder arthroplasty as a salvage procedure after failed internal fixation of fractures of the proximal humerus: outcomes and complications. Bone Joint J 2015; 97-B:967–972. [DOI] [PubMed] [Google Scholar]
- 13.Levy J, Frankle M, Mighell M, et al. The use of the reverse shoulder prosthesis for the treatment of failed hemiarthroplasty for proximal humeral fracture. J Bone Joint Surg Am. 2007; 89:292–300. [DOI] [PubMed] [Google Scholar]
- 14.Lollino N, Paladini P, Campi F, et al. Reverse shoulder prosthesis as revision surgery after fractures of the proximal humerus, treated initially by internal fixation or hemiarthroplasty. Chir Organi Mov. 2009; 93(Suppl 1):S35–S39. [DOI] [PubMed] [Google Scholar]
- 15.Maier MW, Zeifang F, Caspers M, et al. Can reverse shoulder arthroplasty in post-traumatic revision surgery restore the ability to perform activities of daily living? Orthop Traumatol Surg Res. 2015; 101(2):191–196. [DOI] [PubMed] [Google Scholar]
- 16.Martin TG, Iannotti JP. Reverse total shoulder arthroplasty for acute fractures and failed management after proximal humeral fractures. Orthop Clin North Am. 2008; 39(4):451–457, vi. [DOI] [PubMed] [Google Scholar]
- 17.Martinez AA, Bejarano C, Carbonel I, et al. The treatment of proximal humerus nonunions in older patients with reverse shoulder arthroplasty. Injury. 2012; 43:S3–S6. [DOI] [PubMed] [Google Scholar]
- 18.Merolla G, Tartarone A, Sperling JW, et al. Early clinical and radiological outcomes of reverse shoulder arthroplasty with an eccentric all-polyethylene glenosphere to treat failed hemiarthroplasty and the sequelae of proximal humeral fractures. Int Orthopaed (Sicot). 2017; 41(1):141–148. [DOI] [PubMed] [Google Scholar]
- 19.Raiss P, Edwards TB, Collin P, et al. Reverse shoulder arthroplasty for malunions of the proximal part of the humerus (type-4 fracture sequelae). J Bone Joint Surg Am. 2016; 98:893–899. [DOI] [PubMed] [Google Scholar]
- 20.Raiss P, Edwards TB, da Silva MR, et al. Reverse shoulder arthroplasty for the treatment of nonunions of the surgical neck of the proximal part of the humerus (type-3 fracture sequelae). J Bone Joint Surg Am. 2014; 96:2070–2076. [DOI] [PubMed] [Google Scholar]
- 21.Schliemann B, Theisen C, Kosters C, et al. Reverse total shoulder arthroplasty for type I fracture sequelae after internal fixation of proximal humerus fractures. Arch Orthop Trauma Surg. 2017; 137(12):1677–1683. [DOI] [PubMed] [Google Scholar]
- 22.Uri O, Beckles V, Higgs D, et al. Increased-offset reverse shoulder arthroplasty for the treatment of failed post-traumatic humeral head replacement. J Shoulder Elbow Surg 2014; 23:401–408. [DOI] [PubMed] [Google Scholar]
- 23.Willis M, Min W, Brooks JP, et al. Proximal humeral malunion treated with reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2012; 21(4):507–513. [DOI] [PubMed] [Google Scholar]
- 24.Zafra M, Uceda P, Flores M, et al. Reverse total shoulder replacement for nonunion of a fracture of the proximal humerus. Bone Joint J. 2014; 96-B(9):1239–1243. [DOI] [PubMed] [Google Scholar]
- 25.Young SW, Segal BS, Turner PC, et al. Comparison of functional outcomes of reverse shoulder arthroplasty versus hemiarthroplasty in the primary treatment of acute proximal humerus fracture. ANZ J Surg. 2010; 80(11):789–793. [DOI] [PubMed] [Google Scholar]
- 26.Shannon SF, Wagner ER, Houdek MT, et al. Reverse shoulder arthroplasty for proximal humeral fractures: outcomes comparing primary reverse arthroplasty for fracture versus reverse arthroplasty after failed osteosynthesis. J Shoulder Elbow Surg. 2016; 25(10):1655–1660. [DOI] [PubMed] [Google Scholar]
- 27.Alentorn-Geli E, Guirro P, Santana F, et al. Treatment of fracture sequelae of the proximal humerus: comparison of hemiarthroplasty and reverse total shoulder arthroplasty. Arch Orthop Trauma Surg. 2014; 134(11):1545–1550. [DOI] [PubMed] [Google Scholar]
- 28.Shukla DR, McAnany S, Kim J, et al. Hemiarthroplasty versus reverse shoulder arthroplasty for treatment of proximal humeral fractures: a Meta-analysis. J Shoulder Elbow Surg. 2016; 25(2):330–340. [DOI] [PubMed] [Google Scholar]
- 29.Wang J, Zhu Y, Zhang F, et al. Meta-analysis suggests that reverse shoulder arthroplasty in proximal humerus fractures is a better option than hemiarthroplasty in the elderly. Int Orthop. 2016; 40(3):531–539. [DOI] [PubMed] [Google Scholar]
- 30.Gallinet D, Ohl X, Decroocq L, et al. Is reverse total shoulder arthroplasty more effective than hemiarthroplasty for treating displaced proximal humerus fractures in older adults? A systematic review and meta-analysis. Orthopaed Traumatol Surg Res 2018; 104:759–766. [DOI] [PubMed] [Google Scholar]
- 31.Law TY, Rosas S, George F, et al. Short-term projected use of reverse total shoulder arthroplasty in proximal humerus fracture cases recorded in Humana’s National Private-Payer Database. Am J Orthop. 2017; 46:E28–E31. [PubMed] [Google Scholar]
- 32.Acevedo DC, Mann T, Abboud JA, et al. Reverse total shoulder arthroplasty for the treatment of proximal humeral fractures: patterns of use among newly trained orthopedic surgeons. J Shoulder Elbow Surg. 2014; 23(9):1363–1367. [DOI] [PubMed] [Google Scholar]
- 33.Sabesan V, Lombardo D, Petersen-Fitts G, et al. National trends in proximal humerus fracture treatment patterns. Aging Clin Exp Res. 2017; 29(6):1277–1283. [DOI] [PubMed] [Google Scholar]
- 34.Savin DD, Zamfirova I, Iannotti J, et al. Survey study suggests that reverse total shoulder arthroplasty is becoming the treatment of choice for four-part fractures of the humeral head in the elderly. Int Orthop. 2016; 40(9):1919–1925. [DOI] [PubMed] [Google Scholar]
- 35.Schairer WW, Nwachukwu BU, Lyman S, et al. Arthroplasty treatment of proximal humerus fractures: 14-year trends in the United States. Phys Sportsmed. 2017; 45(2):92–96. [DOI] [PubMed] [Google Scholar]
- 36.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Review Manager (RevMan). [Computer program] Version 5.3. Copenhagen: The Nordic Cochrane Center, The Cochrane Collaboration; 2014.
- 38.Wells G, Shea B, O’Connell J. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. Ottawa, ON: Ottawa Hospital Research Institute; 2014.
- 39.Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005; 5(1):13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sebastia-Forcada E, Lizaur-Utrilla A, Cebrian-Gomez R, et al. Outcomes of reverse total shoulder arthroplasty for proximal humeral fractures: primary arthroplasty versus secondary arthroplasty after failed proximal humeral locking plate fixation. J Orthop Trauma. 2017; 31(8):e236–e240. [DOI] [PubMed] [Google Scholar]
- 41.Dezfuli B, King JJ, Farmer KW, et al. Outcomes of reverse total shoulder arthroplasty as primary versus revision procedure for proximal humerus fractures. J Shoulder Elbow Surg. 2016; 25(7):1133–1137. [DOI] [PubMed] [Google Scholar]
- 42.Seidl AJ, Sholder D, Warrender W, et al. Early vs. late reverse shoulder arthroplasty for proximal humerus fractures: does it matter? J Shoulder Elbow Surg. 2017; 26(10):e333–e334. [PMC free article] [PubMed] [Google Scholar]
- 43.Katthagen J, Hesse E, Lill H, et al. Outcomes and revision rates of primary vs. secondary reverse total shoulder arthroplasty for proximal humeral fractures. Obere Extremität. 2020; 15(1):35–41. [Google Scholar]
- 44.Ghert M, McKee M. To operate or not to operate, that is the question: the proximal humerus fracture. Bone Joint Res. 2016; 5(10):490–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dean BJ, Jones LD, Palmer AJ, et al. A review of current surgical practice in the operative treatment of proximal humeral fractures: does the PROFHER trial demonstrate a need for change? Bone Joint Res. 2016; 5(5):178–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jefferson L, Brealey S, Handoll H, et al. Impact of the PROFHER trial findings on surgeons' clinical practice: an online questionnaire survey. Bone Joint Res. 2017; 6(10):590–599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cicak N, Nikola C, Klobucar H, et al. Reverse shoulder arthroplasty in acute fractures provides better results than in revision procedures for fracture sequelae. Int Orthop. 2015; 39(2):343–348. [DOI] [PubMed] [Google Scholar]
- 48.Santana F, Alentorn-Geli E, Guirro P, et al. Reverse shoulder arthroplasty for fracture sequelae: How the initial fracture treatment influences the outcomes of joint replacement. Acta Orthop Traumatol Turc. 2019; 53(4):278–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Namdari S, Yagnik G, Ebaugh DD, et al. Defining functional shoulder range of motion for activities of daily living. J Shoulder Elbow Surg 2012; 21:1177–1183. [DOI] [PubMed] [Google Scholar]
- 50.Simovitch R, Flurin PH, Wright T, et al. Quantifying success after total shoulder arthroplasty: the minimal clinically important difference. J Shoulder Elbow Surg. 2018; 27(2):298–305. [DOI] [PubMed] [Google Scholar]
- 51.Torrens C, Guirro P, Santana F. The minimal clinically important difference for function and strength in patients undergoing reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2016; 25(2):262–268. [DOI] [PubMed] [Google Scholar]
- 52.Werner BC, Chang B, Nguyen JT, et al. What change in American shoulder and elbow surgeons score represents a clinically important change after shoulder arthroplasty? Clin Orthop Relat Res. 2016; 474(12):2672–2681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Solomon JA, Joseph SM, Shishani Y, et al. Cost analysis of hemiarthroplasty versus reverse shoulder arthroplasty for fractures. Orthopedics. 2016; 39(4):230–234. [DOI] [PubMed] [Google Scholar]
- 54.Nwachukwu BU, Schairer WW, McCormick F, et al. Arthroplasty for the surgical management of complex proximal humerus fractures in the elderly: a cost-utility analysis. J Shoulder Elbow Surg. 2016; 25(5):704–713. [DOI] [PubMed] [Google Scholar]
- 55.Osterhoff G, O’Hara NN, D'Cruz J, et al. A cost-effectiveness analysis of reverse total shoulder arthroplasty versus hemiarthroplasty for the management of complex proximal humeral fractures in the elderly. Value Health. 2017; 20(3):404–411. [DOI] [PubMed] [Google Scholar]
- 56.Saltzman BM, Chalmers PN, Gupta AK, et al. Complication rates comparing primary with revision reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2014; 23(11):1647–1654. [DOI] [PubMed] [Google Scholar]
- 57.Maier D, Jaeger M, Izadpanah K, et al. Proximal humeral fracture treatment in adults. J Bone Joint Surg Am. 2014; 96(3):251–261. [DOI] [PubMed] [Google Scholar]
- 58.Walch G, Bacle G, Lädermann A, et al. Do the indications, results, and complications of reverse shoulder arthroplasty change with surgeon’s experience? J Shoulder Elbow Surg. 2012; 21(11):1470–1477. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-sea-10.1177_2471549220949731 for Primary Versus Salvage Reverse Total Shoulder Arthroplasty for Displaced Proximal Humerus Fractures in the Elderly: A Systematic Review and Meta-analysis by Patrick A Nelson MD Changyow C MD Tjong KVehniah Kwan MD Michael A Terry MD Ujash Sheth MD, MSc, FRCSC in Journal of Shoulder and Elbow Arthroplasty