Abstract
Introduction
Socioeconomic differences may confound racial and ethnic differences in SARS-CoV-2 testing and COVID-19 outcomes.
Methods
A retrospective cohort study was conducted of racial/ethnic differences in SARS-CoV-2 testing and positive tests and COVID-19 hospitalizations and deaths among adults impaneled at a Northern California regional medical center and enrolled in the county Medicaid managed care plan (N=84,346) as of March 1, 2020. Logistic regressions adjusted for demographics, comorbidities, and neighborhood characteristics.
Results
Nearly 30% of enrollees were ever tested for SARS-CoV-2, and 4% tested positive. A total of 19.7 per 10,000 were hospitalized for and 9.4 per 10,000 died of COVID-19. Those identified as Asian, Black, or of other/unknown race had lower testing rates, whereas those identified as Latino had higher testing rates than Whites. Enrollees of Asian or other/unknown race had slightly higher odds of a positive test, and Latinos had much higher odds of a positive test (OR=3.77, 95% CI=3.41, 4.17) than Whites. The odds of hospitalization (OR=2.85, 95% CI=1.85, 4.40) and death (OR=4.75, 95% CI=2.23, 10.12) were higher for Latino than for White patients, even after adjusting for demographics, comorbidities, and neighborhood characteristics.
Conclusions
In a Medicaid managed care population, where socioeconomic differences may be reduced, the odds of a positive SARS-CoV-2 test, COVID-19 hospitalization, and COVID-19 death were higher for Latino but not Black patients than for White patients. Racial/ethnic disparities depend on local context. The substantially higher risk facing Latinos should be a key consideration in California's strategies to mitigate disease transmission and harm.
INTRODUCTION
Nationwide, coronavirus disease 2019 (COVID-19) has disproportionately affected racial and ethnic minorities in terms of infection, hospitalization, and mortality.1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12 The role of sociodemographic, clinical, and neighborhood factors in accounting for racial/ethnic differences in COVID-19 outcomes remains unclear. Higher rates of testing positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) among individuals identified as Black or Latino (referred to as Blacks or Latinos, respectively, in the remaining part of this paper) than among those identified as White (referred to as Whites in the remaining part of this paper) persist after adjustment.13, 14, 15, 16, 17, 18 The patterns for COVID-19 outcomes are more variable. Among confirmed COVID-19 cases, adjusted odds of hospitalization were higher for Black and Latino patients than for Whites in an integrated Wisconsin health system16 and for Black but not for Latino patients in an integrated California health system.17 By contrast, adjusted odds of hospitalization were similar for Black and Latino patients relative to the odds for White patients in a New York City health system.15 Adjusted odds of in-hospital COVID-19 mortality did not differ for Blacks relative to the odds for Whites in Louisiana,18 whereas Latino but not Black patients had higher adjusted odds of death in Wisconsin.16 The potential causes of these conflicting findings may be the unobserved differences in socioeconomic characteristics, comorbidities, trust in the medical system, and living and working conditions.19 Little evidence exists for Asian populations.
Nationally, 30-day mortality among SARS-CoV-2‒positive veterans did not differ for Blacks or Latinos relative to that for Whites.13 Because veterans differ from the overall population (e.g., mostly male), that study may not generalize. In England, Blacks and South Asians had higher odds of COVID-19 death than Whites, even after adjusting for socioeconomic and clinical factors.20 These findings may not apply to the U.S.
This study analyzed data from the county-run Medicaid managed care plan in Contra Costa County, California, an ethnically and economically diverse suburban Bay Area county with a population of about 1.2 million,21 to study racial/ethnic disparities in SARS-CoV-2 testing and positive test results and COVID-19 hospitalizations and death. The county Medicaid managed care plan and public health testing data systems are integrated, enabling this study to capture the vast majority of the tests conducted throughout the county. The analysis adjusted for demographic and clinical characteristics through November 19, 2020 and 2018 ZIP code characteristics that may affect virus transmission.22 , 23 Because all patients had Medicaid, they are similar along some unmeasured economic dimensions. The hypotheses were that racial/ethnic disparities in testing and outcomes would narrow when controlling for demographics, comorbidities, and ZIP code–level characteristics and would be reduced relative to those in previous studies given similar insurance coverage, household income, and access to healthcare providers.
METHODS
A retrospective, observational, cohort study of all Medi-Cal patients impaneled on March 1, 2020 at Contra Costa Regional Medical Center (CCRMC), the county public hospital, and affiliated health centers was conducted. CCRMC is a 166-bed full-service health facility that along with its 10 health centers is the primary point of care for patients enrolled in the county's public Medicaid managed care plan, Contra Costa Health Plan (CCHP). CCHP enrollees are autoassigned to CCRMC as their primary healthcare access point, subject to capacity. Most impaneled patients are Medi-Cal managed care enrollees, although fee-for-service Medi-Cal enrollees who were assigned a CCRMC primary care provider and have been seen at CCRMC in the past 12 months are also included. Data were extracted from the county's electronic medical record (EMR) system. Because both CCRMC and CCHP are county run, the EMR system is synced with the county's public health SARS-CoV-2 testing data. Patients who were members of the CCHP but not impaneled at CCRMC were excluded from the study. Neighborhood factors were merged to the EMR data by ZIP code, the smallest geographic unit of observation available, from the American Community Survey 5-year (2009–2019) estimates. This study was approved by the University of Southern California IRB, which granted a waiver of informed consent (as a minimal-risk medical record review) as well as the Institutional Review Committee at Contra Costa Health Services. The study follows the STROBE guidelines for reporting observational studies.
Study Sample
All 84,346 patients aged ≥18 years impaneled at CCRMC as of March 1, 2020 were included in the analysis. All SARS-CoV-2 tests performed by the county between February 28, 2020 and March 4, 2021 were included. Tests were performed at public health testing laboratories, at CCRMC, and in commercial laboratories. Nearly all tests were reverse transcriptase-polymerase chain reaction (RT-PCR) tests, although some other test types (4.64% antibody, 0.49% antigen based) were included. A total of 4 outcomes were analyzed, including whether an individual (1) received ≥1 SARS-CoV-2 test, (2) had ≥1 positive test, (3) had a COVID-19 hospitalization, and (4) died of COVID-19. Sensitivity checks (1) restricted to RT-PCR tests and (2) analyzed the number of SARS-CoV-2 tests received. COVID-19 hospitalizations were captured in the admission diagnosis and required a positive test. No individuals had >1 COVID-19 hospitalization. COVID-19 deaths were from the California Reportable Disease Information Exchange system and were manually verified by the county.
Measures
Race and ethnicity data were from the EMR and were grouped into 5 categories: Asian, Black, Latino, White, and other/unknown. Patients who self-identified as Latino were classified as such regardless of race. Owing to small sample sizes, patients who identified as Native American/Alaska Native (n=280), multiracial (n=1,452), or another race category (n=3,573) were grouped with the <7% of the sample (n=5,663) who declined to provide or were otherwise missing race information as other/unknown race.
Adjustments were made for demographic and clinical characteristics that on the basis of previous reports2, 3, 4, 5, 6, 7, 8 were likely to affect COVID-19 outcomes, including age (indicators for ages 18–29, 30–39, 40–49, 50–64, 65–74, 75–84, and ≥85 years), sex, obesity (defined as BMI >30), and indicators for the following medical comorbidities: asthma, cancer, chronic pain, diabetes, chronic obstructive pulmonary disease, and hypertension. Comorbidities were captured as entries in health system registries for each disease as well as medical note lists documented between March 1, 2020 and November 19, 2020. Obesity was calculated from the last height and weight measurement in the EMR as of November 19, 2020.
Some models adjusted for ZIP code–level measures of work and economic status, safety net program participation, living arrangements, and access to care from the 5-year (2009–2019) American Community Survey matched to patients on the basis of ZIP code of residence; 1,031 patients (1.22%) were missing ZIP code or did not match to the American Community Survey. Matched patients were from 467 unique ZIP codes, although 98% (n=81,482) were from 45 unique ZIP codes with ≥50 patients each (Appendix Table 1, available online). The measures, hypothesized to affect SARS-CoV-2 exposure and COVID-19 outcomes, were median income; average household size; share of the population aged ≥16 years employed; share of the non-institutionalized civilian population without health insurance; share of households receiving (separately) cash public assistance income, Social Security income, and Food Stamp/Supplemental Nutrition Assistance Program benefits; and share of housing units that were single-family, detached homes.
Statistical Analysis
The demographics and clinical characteristics of patients overall and within each race/ethnicity group were compared as were the percentage of patients who had ≥1 SARS-CoV-2 test, the number of tests received, the percentage of patients who ever tested positive, the number of COVID-19 hospitalizations per 10,000 patients, and COVID-19 deaths per 10,000 patients overall and by race/ethnicity group. A total of 3 logistic regression models—Model 1 (unadjusted), Model 2 (adjusted for the demographics and clinical diagnoses mentioned earlier), and Model 3 (Model 2 with adjustment for the neighborhood characteristics mentioned earlier)—were estimated for each outcome. Computed ORs and 95% CIs were reported for each outcome. In models with neighborhood characteristics, SEs and 95% CIs were adjusted for ZIP code–level clustering. Sensitivity analyses tested robustness to (1) restricting to RT-PCR tests; (2) analyzing the number of COVID-19 tests received; (3) restricting to tested patients; and (4) recoding patients of other/unknown race as Latino, Asian, Black, or White. To address repeat testing, a negative binomial regression model was used to analyze the number of tests received. All analyses were performed using Stata/MP, version 15.1. The analysis was not meant to identify a causal model. Race/ethnicity is neither a mutable characteristic nor a risk factor per se for SARS-CoV-2 or COVID-19 outcomes. Rather, the goal was to determine whether the differences in testing and outcomes differed by race/ethnicity in a relatively socioeconomically homogenous group and after controlling for demographic, clinical, and ZIP code characteristics.
RESULTS
As of March 1, 2020, CCRMC had 84,346 impaneled adult patients. The patient population was racially/ethnically diverse: 15% (n=12,751) Asian, 16% (n=13,897) Black, 29% (n=24,153) Latino, 26% (n=21,827) White, and 15% (n=11,728) individuals of other/unknown race (Table 1 ). Blacks, Latinos, and those of other/unknown race were younger than Whites or Asians: a third of Latino and patients of other/unknown race and a quarter of Black patients were aged 18–29 years compared with 16% of Whites and Asians. Less than 14% of Black, Latino, and patients of other/unknown race were aged ≥65 years compared with 17% of Whites and about 30% of Asians. The patient population skewed more toward the female sex (56%), with the skew larger for Latinos (61%).
Table 1.
Characteristics of the Patient Population Overall and by Race/Ethnicity
| Characteristics | Patients, n (%) |
|||||
|---|---|---|---|---|---|---|
| Total | Asian | Black/African American | Latino | Other/unknowna | White/Caucasian | |
| Impaneled | 84,346 | 12,741 (15) | 13,897 (16) | 24,153 (29) | 11,728 (14) | 21,827 (26) |
| Age groups, years | ||||||
| 18‒29 | 20,023 (23.4) | 2,082 (16.3) | 3,277 (23.6) | 7,583 (31.4) | 3,642 (31.1) | 3,439 (15.8) |
| 30‒39 | 16,733 (19.8) | 1,906 (15.0) | 2,886 (20.8) | 4,695 (19.4) | 2,754 (23.5) | 4,492 (20.6) |
| 40‒49 | 12,001 (14.2) | 1,531 (12.0) | 2,114 (15.2) | 3,797 (15.7) | 1,559 (13.2) | 3,000 (13.7) |
| 50‒64 | 21,647 (25.7) | 3,349 (26.3) | 3,861 (27.8) | 4,731 (19.6) | 2,444 (20.8) | 7,262 (33.3) |
| 65‒74 | 9,523 (11.3) | 2,480 (19.5) | 1,334 (9.6) | 2,070 (8.57) | 899 (7.67) | 2,740 (12.6) |
| 75‒84 | 3,368 (3.99) | 1,052 (8.26) | 354 (2.55) | 933 (3.86) | 390 (2.72) | 710 (3.25) |
| ≥85 | 1,051 (1.25) | 341 (2.68) | 71 (0.51) | 359 (1.42) | 111 (0.95) | 184 (0.84) |
| Sex | ||||||
| Female | 47,205 (56.0) | 7,330 (57.5) | 7,678 (55.3) | 14,794 (61.3) | 5,991 (51.1) | 11,412 (52.3) |
| Male | 37,123 (44.0) | 5,410 (42.5) | 6,213 (44.7) | 9,359 (38.8) | 5,730 (48.9) | 10,411 (47.7) |
| Nonbinary or unknown | 18 (0.02) | 1 (0.01) | 6 (0.05) | 0 | 7 (0.06) | 4 (0.02) |
| Diagnoses | ||||||
| Asthma | 8,849 (10.5) | 963 (7.56) | 2,207 (15.9) | 2,456 (10.2) | 755 (6.44) | 2,468 (11.3) |
| Cancer | 3,220 (3.82) | 498 (3.91) | 428 (3.1) | 753 (3.12) | 236 (2.01) | 1,305 (5.98) |
| Painb | 11,449 (13.6) | 1,407 (11.0) | 2,477 (17.8) | 2,791 (11.6) | 878 (7.49) | 3,896 (17.9) |
| Diabetes | 12,216 (14.5) | 2,693 (21.1) | 2,053 (14.8) | 3,908 (16.2) | 1,000 (8.53) | 2,562 (11.7) |
| COPD | 2,611 (3.10) | 305 (2.39) | 567 (4.08) | 273 (1.13) | 192 (1.64) | 1,274 (5.84) |
| Hypertension | 22,479 (26.7) | 4,645 (36.5) | 4,675 (33.6) | 5,304 (22.0) | 1,738 (14.8) | 6,117 (28.0) |
| BMI ≥30 | 30,179 (35.3) | 2,364 (18.6) | 5,210 (37.5) | 7,764 (32.2) | 9,925 (59.1) | 6,764 (31.0) |
| Testedc | 24,508 (29.1) | 3,368 (26.4) | 3,852 (27.7) | 8,397 (34.8) | 2,531 (21.6) | 6,360 (29.1) |
| Number of tests|test>0d | 1.91 | 1.94 | 1.87 | 1.79 | 1.98 | 2.04 |
| Tested positivee | 3,351 (3.97) | 360 (2.83) | 282 (2.03) | 1,934 (8.01) | 282 (2.4) | 493 (2.26) |
| Hospitalizedf | 166 (19.7) | 26 (20.4) | 22 (15.8) | 85 (35.2) | 6 (5.12) | 27 (12.4) |
| Diedf | 79 (9.37) | 14 (11.0) | 12 (8.63) | 42 (17.4) | 3 (2.56) | 8 (3.67) |
Owing to small numbers (n=280), American Indian/Native Alaskan is included with other/unknown.
Patients with a chronic pain diagnosis in the electronic health record.
Tested positive means tested positive at least once.
Number of tests conditional on at least 1 test for SARS-CoV-2.
Patients who had at least 1 test for SARS-CoV-2.
Hospitalization and death rate in parentheses are per 10,000.
COPD, chronic obstructive pulmonary disease.
Nearly 15% of patients had diagnoses of diabetes, and about 35% were obese, the 2 key risk factors for severe illness from COVID-19.24 Asians had higher rates of diabetes (21%), and Whites had lower rates (12%) than other race/ethnicity groups. Patients of other/unknown race were disproportionately obese (59%). About a quarter of patients had hypertension.25 Asians and Black patients had the highest rates of hypertension at 37% and 34%, respectively. Latinos had lower rates of all diagnosed diseases except diabetes than Whites.
A total of 29% (n=24,508) of individuals were tested at least once for SARS-CoV-2, with 4% (n=3,351) ever testing positive; 19.7 per 10,000 (n=166) had a COVID-19‒related hospitalization, and 9.37 per 10,000 (n=79) died of COVID-19. Testing rates varied modestly across race/ethnicity groups (Appendix Figure 1A, available online): Latinos had slightly higher rates of testing (34.8%) than Whites (29.1%), Blacks (27.7%), Asians (26.4%), or individuals of other/unknown race (21.6%). The percentage of patients who ever had a positive test was considerably higher for Latinos at 8% (n=1,934) than for Asians at 2.8% (n=360), for individuals of other/unknown race at 2.4% (n=282), for Whites at 2.26% (n=493), and for Blacks at 2.03% (n=282). Among tested patients, the mean number of tests received was similar across groups at about 2 tests (Table 1).
Hospitalization rates varied markedly and were highest for Latinos. Hospitalizations per 10,000 were 35.2 (n=85) for Latinos compared with 20.4 (n=26) for Asians, 15.8 (n=22) for Blacks, 12.4 (n=27) for Whites, and 5.12 (n=5) for individuals of other/unknown race. COVID-19 deaths per 10,000 followed a similar pattern: 17.4 (n=42) for Latinos, 11.0 (n=14) for Asians, 8.63 (n=12) for Blacks, 3.67 (n=8) for Whites, and 2.56 (n=3) for patients of other/unknown race.
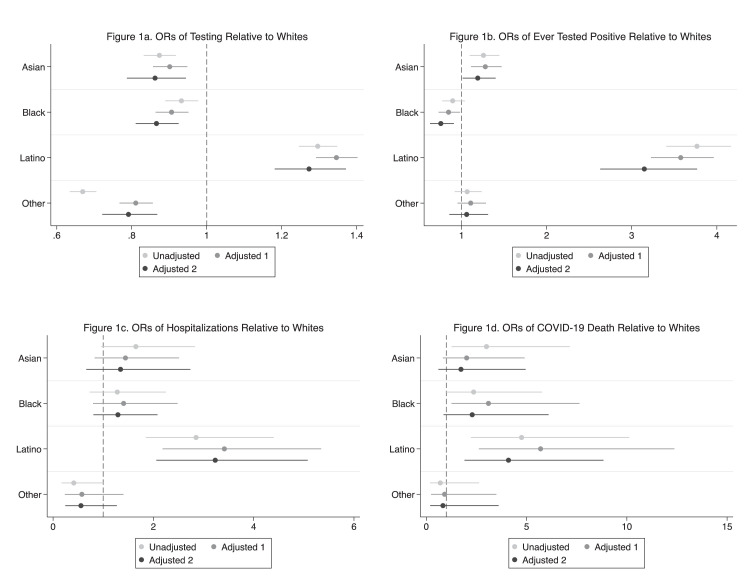
Latinos had higher unadjusted odds of testing at least once (OR=1.30, 95% CI=1.25, 1.35) than Whites; all other groups had lower unadjusted odds (Asians: OR=0.87, 95% CI=0.83, 0.92; Blacks: OR=0.93, 95% CI=0.89, 0.98; individuals of other/unknown race: OR=0.67, 95% CI=0.63, 0.71) (Table 2 , Panel A). Adjusting for age and comorbidities and including neighborhood characteristics did little to alter these patterns (Figure 1A and Appendix Table 2, available online). The results were qualitatively similar for RT-PCR tests only (Appendix Table 3, available online) and for negative binomial regression models of SARS-CoV-2 test counts (Appendix Table 4, available online).
Table 2.
Unadjusted ORs
| Variables | Panel A: ever tested for SARS-CoV-2 | Panel B: ever tested positive for SARS-CoV-2 | Panel C: COVID-19 hospitalization | Panel D: COVID-19 death |
|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| White (ref) | ||||
| Asian | 0.87 (0.83, 0.92) | 1.26 (1.10, 1.44) | 1.65 (0.96, 2.83) | 3.00 (1.26, 7.15) |
| Black | 0.93 (0.89, 0.98) | 0.90 (0.77, 1.04) | 1.28 (0.73, 2.25) | 2.36 (0.96, 5.77) |
| Latino | 1.30 (1.25, 1.35) | 3.77 (3.41, 4.17) | 2.85 (1.85, 4.40) | 4.75 (2.23, 10.12) |
| Othera | 0.67 (0.63, 0.71) | 1.07 (0.92, 1.24) | 0.41 (0.17, 1.00) | 0.70 (0.19, 2.63) |
| Observations | 84,346 | 84,346 | 84,346 | 84,346 |
| Mean rate | 29.1b | 3.97c | 19.7d | 9.37d |
Owing to small numbers (n=280), American Indian/Native Alaskan is included with other/unknown.
The percentage of patients who had at least 1 test for SARS-CoV-2.
Ever tested positive is denominated by all impaneled patients, irrespective of whether they were ever tested for SARS-CoV-2.
Hospitalizations and deaths are per 10,000.
Figure 1.
Unadjusted ORs and AORs of testing, positivity, and hospitalizations.
Note: Estimates labeled Adjusted 1 control for patient demographics and comorbidities. Estimates labeled Adjusted 2 further control for neighborhood characteristics. Specific controls are detailed in the text. Bars correspond to 95% CIs.
Unadjusted odds of a positive SARS-CoV-2 test (Table 2, Panel B) were not significantly higher for Blacks or those of other/unknown race than for Whites but were significantly higher for Asians (OR=1.26, 95% CI=1.10, 1.44) and, most notably, for Latinos (OR=3.77, 95% CI=3.41, 4.17) relative to Whites. Adjusting for age and comorbidities and including ZIP code characteristics only modestly reduced these disparities (Figure 1B). ORs for Latinos relative to those for Whites remained very high (Appendix Table 2, available online): OR=3.58 (95% CI=3.23, 3.96) with demographic and clinical adjustment and OR=3.15 (95% CI=2.63, 3.77) with the further addition of neighborhood characteristics. Results were similar for RT-PCR tests (Appendix Table 5, available online) and positive cases relative to those for SARS-CoV-2 tests (Appendix Table 6, available online).
Unadjusted associations between COVID-19 related hospitalizations and race (Table 2, Panel C) were only statistically distinguishable for Latinos relative to Whites. The unadjusted OR of hospitalizations for Latinos relative to Whites was 2.85 (95% CI=1.85, 4.40). Adjusting for demographic and clinical factors and further with neighborhood characteristics did little to alter these patterns (Figure 1C).
The unadjusted ORs of COVID-19 deaths (Table 2, Panel D) were statistically distinguishable from 0 and were higher for Asians (OR=3.0, 95% CI=1.26, 7.15) and Latinos (OR=4.75, 95% CI=2.23, 10.1) than for Whites. The ORs were also higher for Blacks, although they were not statistically distinguishable from 0 (OR=2.36, 95% CI=0.96, 5.77). Adjusting for demographic and clinical factors and further with neighborhood characteristics did little to alter the pattern or significance of the results for Latinos (Figure 1C and Appendix Table 2, available online). In the fully adjusted models, the ORs remained sizable but were statistically indistinguishable from Whites for Asians and Blacks. The pattern of results for deaths and all other outcomes was unaffected by recoding those categorized as other/unknown race as either Asian, Black, or Latino (Appendix Table 7, available online).
DISCUSSION
By analyzing data from a diverse Medicaid Managed Care population, disparities in SARS-CoV-2 testing and COVID-19 outcomes could be compared for not only Blacks but also Latinos and Asians. Latinos were more likely to be tested for SARS-CoV-2 and to receive a positive result than Whites. By contrast, Blacks and Asians were less likely to be tested, with Asians more likely to test positive, than Whites. Higher testing rates among Latinos may be partly attributable to concerted county efforts to target this group in response to their observed higher disease burden.
Latinos were the only group that had higher ORs of COVID-19 hospitalization and death than Whites after adjustment for demographic, clinical, and neighborhood characteristics. The disparities for Latinos were particularly noteworthy given the magnitudes and the fact that Latinos were disproportionately younger. Moreover, the magnitudes were scarcely affected by adjustment for individual- or ZIP code–level characteristics.
Because controlling for underlying comorbidities and neighborhood characteristics did little to narrow the disparities measured in this study, the results suggest that other unobserved structural factors, such as inequitable distribution of scarce hospital resources and ability to work from home or take paid leave and ongoing discrimination, are key drivers of the differential impacts of COVID-19.26 However, one key limitation is the inherent measurement error in comorbidities owing to both a lack of data on disease severity as well as the potential differences in registry inclusion caused by disparities in undiagnosed disease.27 , 28
Also of note is the finding of lower odds of positive COVID-19 tests for Blacks than for Whites. This contrasts with findings for veterans,13 patients from a Greater Houston area health system,14 patients from a New York City health system,15 and patients from a Wisconsin health system.16 However, the lack of a Black–White disparity in hospitalizations and mortality is consistent with the findings of previous work.13 , 15 Caution should be used in interpreting these findings, given that the point estimates were consistent with higher odds of hospitalization and death among Blacks than among Whites. Estimates indicated higher odds of death for Asian patients than for White patients but also became imprecise with adjustment. As the pandemic continues, the patterns may become more precise.
The findings for Latinos, who are projected to make up about half of Californians by 2060,29 are particularly troubling. Consistent with work from a single census tract in San Francisco, Latinos had starkly higher odds of a positive test than Whites.30 This disparity suggests that Latinos have considerably higher rates of undiagnosed SARS-CoV-2 infection than the general population. Assuming that all severe cases of COVID-19 lead to hospitalization and that severity is equal across groups after controlling for clinical, demographic, and neighborhood characteristics, the odds of SARS-CoV-2 infection among the CCHP Latino population is >2.5 times that of Whites.
Limitations
Data were from 1 county in California and may not generalize. The data did not capture individuals without contact with the healthcare system and may be confounded by selection into health care or Medicaid, an issue sometimes referred to as collider bias. Such selection is problematic if it is differential across race/ethnicity. SARS-CoV-2 testing differs by race/ethnicity, complicating the interpretation of the differences in positive tests; hospitalizations and death are less prone to selection bias. Hospitalizations outside of the county medical center and privately paid SARS-CoV-2 tests were also not captured. Privately paid tests were likely rare because the county provides free testing at multiple sites and the study population is low income. The data capture the presence of specific diseases not disease severity, an important contributor to hospitalization and death. Because the limited data set only contained the ZIP codes of residence, the analysis could not capture neighborhood deprivation or other Census tract measures of disadvantage that may contribute to disparities. The data did not separately identify patients who were both Latino and from another racial group. Owing to limited sample size, Native American/Alaska Natives (0.33%) and individuals indicating >1 race (1.7%) or another race category (4.24%) were grouped with individuals with unknown race/ethnicity (6.7%). Sensitivity analysis of this coding was performed.
CONCLUSIONS
California is home to diverse racial and ethnic populations, with more Latinos than any other state.31 In a Northern California Medicaid population, Latinos had consistently worse outcomes than Whites, whereas Blacks did not. These data highlight that racial/ethnic disparities may not be uniform across geography and that such disparities are not fully explained by differences in SES and underlying health.
ACKNOWLEDGMENTS
The authors thank Scott Osborn and Chris Lynch for help with the data extracts and for answering questions about how certain information is captured in the county systems. The authors also thank the editor and 3 anonymous referees for helpful comments that improved the analysis and clarity of the paper.
No financial disclosures were reported by the authors of this paper.
Footnotes
Supplemental materials associated with this article can be found in the online version at https://doi.org/10.1016/j.amepre.2021.05.015.
Appendix. SUPPLEMENTAL MATERIAL
REFERENCES
- 1.Garg S, Kim L, Whitaker M, et al. Hospitalization rates and characteristicsof patients hospitalized with laboratory-confirmed coronavirus disease 2019 - COVID-NET, 14 states, March 1-30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(15):458–464. doi: 10.15585/mmwr.mm6915e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Killerby ME, Link-Gelles R, Haight SC, et al. Characteristics associated with hospitalization among patients with COVID-19 - metropolitan Atlanta, Georgia, March-April 2020. MMWR Morb Mortal Wkly Rep. 2020;69(25):790–794. doi: 10.15585/mmwr.mm6925e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stokes EK, Zambrano LD, Anderson KN, et al. Coronavirus Disease 2019 case surveillance - United States, January 22-May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(24):759–765. doi: 10.15585/mmwr.mm6924e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gold JAW, Wong KK, Szablewski CM, et al. Characteristics and clinical outcomes of adult patients hospitalized with COVID-19 - Georgia, March 2020. MMWR Morb Mortal Wkly Rep. 2020;69(18):545–550. doi: 10.15585/mmwr.mm6918e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention; 2021. Health equity considerations and racial and ethnic minority groups.https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html Updated February 12Accessed April 5, 2021. [Google Scholar]
- 6.Wortham JM, Lee JT, Althomsons S, et al. Characteristics of persons who died with COVID-19 - United States, February 12-May 18, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(28):923–929. doi: 10.15585/mmwr.mm6928e1. [DOI] [PubMed] [Google Scholar]
- 7.Moore JT, Ricaldi JN, Rose CE, et al. Disparities in incidence of COVID-19 among underrepresented racial/ethnic groups in counties identified as hotspots during June 5-18, 2020 - 22 States, February-June 2020. MMWR Morb Mortal Wkly Rep. 2020;69(33):1122–1126. doi: 10.15585/mmwr.mm6933e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sze S, Pan D, Nevill CR, et al. Ethnicity and clinical outcomes in COVID-19: a systematic review and meta-analysis. EClinicalMedicine. 2020;29 doi: 10.1016/j.eclinm.2020.100630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen YH, Glymour MM, Catalano R, et al. Excess mortality in California during the coronavirus disease 2019 pandemic, March to August 2020. JAMA Intern Med. 2021;181(5):705–707. doi: 10.1001/jamainternmed.2020.7578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zelner J, Trangucci R, Naraharisetti R, et al. Racial disparities in coronavirus disease 2019 (COVID-19) mortality are driven by unequal infection risks. Clin Infect Dis. 2021;72(5):e88–e95. doi: 10.1093/cid/ciaa1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Andrasfay T, Goldman N. Reductions in 2020 U.S. life expectancy due to COVID-19 and the disproportionate impact on the Black and Latino populations. Proc Natl Acad Sci U S A. 2021;118(5) doi: 10.1073/pnas.2014746118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lieberman-Cribbin W, Tuminello S, Flores RM, Taioli E. Disparities in COVID-19 testing and positivity in New York City. Am J Prev Med. 2020;59(3):326–332. doi: 10.1016/j.amepre.2020.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rentsch CT, Kidwai-Khan F, Tate JP, et al. Patterns of COVID-19 testing and mortality by race and ethnicity among United States veterans: a nationwide cohort study. PLoS Med. 2020;17(9) doi: 10.1371/journal.pmed.1003379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vahidy FS, Nicolas JC, Meeks JR, et al. Racial and ethnic disparities in SARS-CoV-2 pandemic: analysis of a COVID-19 observational registry for a diverse U.S. metropolitan population. BMJ Open. 2020;10(8) doi: 10.1136/bmjopen-2020-039849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ogedegbe G, Ravenell J, Adhikari S, et al. Assessment of racial/ethnic disparities in hospitalization and mortality in patients with COVID-19 in New York City. JAMA Netw Open. 2020;3(12) doi: 10.1001/jamanetworkopen.2020.26881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Egede LE, Walker RJ, Garacci E, Raymond JR., Sr. Racial/ethnic differences in COVID-19 screening, hospitalization, and mortality in Southeast Wisconsin. Health Aff (Millwood) 2020;39(11):1926–1934. doi: 10.1377/hlthaff.2020.01081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Azar KMJ, Shen Z, Romanelli RJ, et al. Disparities in outcomes among COVID-19 patients in a large health care system in California. Health Aff (Millwood) 2020;39(7):1253–1262. doi: 10.1377/hlthaff.2020.00598. [DOI] [PubMed] [Google Scholar]
- 18.Price-Haywood EG, Burton J, Fort D, Seoane L. Hospitalization and mortality among Black patients and White patients with COVID-19. N Engl J Med. 2020;382(26):2534–2543. doi: 10.1056/NEJMsa2011686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Webb Hooper M, Nápoles AM, Pérez-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA. 2020;323(24):2466–2467. doi: 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Williamson EJ, Walker AJ, Bhaskaran K, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584(7821):430–436. doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.QuickFacts, Contra Costa County, California: population estimates, July 1, 2019. U.S. Census Bureau. https://www.census.gov/quickfacts/fact/table/contracostacountycalifornia/PST045219. Accessed April 28, 2021.
- 22.Tenforde MW, Fisher KA, Patel MM. Identifying COVID-19 risk through observational studies to inform control measures. JAMA. 2021;325(14):1464–1465. doi: 10.1001/jama.2021.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Andersen LM, Harden SR, Sugg MM, Runkle JD, Lundquist TE. Analyzing the spatial determinants of local COVID-19 transmission in the United States. Sci Total Environ. 2021;754 doi: 10.1016/j.scitotenv.2020.142396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention; 2021. COVID-19: people with certain medical conditions.https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html Updated March 29Accessed April 5, 2021. [PubMed] [Google Scholar]
- 25.Matsushita K, Ding N, Kou M, et al. The relationship of COVID-19 severity with cardiovascular disease and its traditional risk factors: a systematic review and meta-analysis. Glob Heart. 2020;15(1):64. doi: 10.5334/gh.814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Egede LE, Walker RJ. Structural racism, social risk factors, and COVID-19 - a dangerous convergence for Black Americans. N Engl J Med. 2020;383(12):e77. doi: 10.1056/NEJMp2023616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Barcellos SH, Goldman DP, Smith JP. Undiagnosed disease, especially diabetes, casts doubt on some of reported health ‘advantage’ of recent Mexican immigrants. Health Aff (Millwood) 2012;31(12):2727–2737. doi: 10.1377/hlthaff.2011.0973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim EJ, Kim T, Conigliaro J, Liebschutz JM, Paasche-Orlow MK, Hanchate AD. Racial and ethnic disparities in diagnosis of chronic medical conditions in the USA. J Gen Intern Med. 2018;33(7):1116–1123. doi: 10.1007/s11606-018-4471-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.California Senate Office of Research . California Senate Office of Research; Sacramento, CA: 2017. A statistical picture of Latinos in California: 2017 update. https://latinocaucus.legislature.ca.gov/sites/latinocaucus.legislature.ca.gov/files/forms/Statistical%20Picture%20of%20Latinos%20in%20California%20-%202017%20Update.pdf. Accessed April 5, 2021. [Google Scholar]
- 30.Chamie G, Marquez C, Crawford E, et al. SARS-CoV-2 community transmission disproportionately affects Latinx population during Shelter-in-Place in San Francisco. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa1234. In press. Online August 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Krogstad JM. Pew Research Center; Washington, DC: 2020. Hispanics have accounted for more than half of total U.S. population growth since 2010. https://www.pewresearch.org/fact-tank/2020/07/10/hispanics-have-accounted-for-more-than-half-of-total-u-s-population-growth-since-2010/. Accessed April 5, 2021. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.