Abstract
Background
As the health systems around the world struggled to meet the challenges of COVID-19 pandemic, care of many non-COVID emergencies was affected.
Aims
The present study examined differences in the diagnosis, evaluation and management of stroke patients during a defined period in the ongoing pandemic in 2020 when compared to a similar epoch in year 2019.
Methods
The COVID stroke study group (CSSG) India, included 18 stroke centres spread across the country. Data was collected prospectively between February and July 2020 and retrospectively for the same period in 2019. Details of demographics, stroke evaluation, treatment, in-hospital and three months outcomes were collected and compared between these two time points.
Results
A total of 2549 patients were seen in both study periods; 1237 patients (48.53%) in 2019 and 1312 (51.47%) in 2020. Although the overall number of stroke patients and rates of thrombolysis were comparable, a significant decline was observed in the month of April 2020, during the initial period of the pandemic and lockdown. Endovascular treatment reduced significantly and longer door to needle and CT to needle times were observed in 2020. Although mortality was higher in 2020, proportion of patients with good outcome were similar in both the study periods.
Conclusions
Although stroke admissions and rates of thrombolysis were comparable, some work flow metrics were delayed, endovascular stroke treatment rates declined and mortality was higher during the pandemic study period. Reorganization of stroke treatment pathways during the pandemic has likely improved the stroke care delivery across the globe.
Keywords: COVID-19, SARS-CoV-2, Ischemic stroke, Thrombolysis, Stroke, Pandemic
Abbreviations: ASPECTS, Alberta stroke program early CT score; COVID-19, Coronavirus disease 2019; CSSG, COVID-19 Stroke Study Group; CT, Computed Tomography; CVT, Cerebral Venous Thrombosis; EVT, Endovascular Therapy; ICH, Intracerebral Hemorrhage; IQR, Inter-quartile range; LVO, Large Vessel Occlusion; mRS, modified Rankin score; NIHSS, National Institutes of Health Stroke Scale; rTPA, Recombinant Tissue Plasminogen Activator; RTPCR, Real Time Polymerase Chain Reaction; SD, Standard Deviation; TNK, Tenecteplase
1. Introduction
The COVID-19 pandemic has affected healthcare around the world. On 11 March 2020, the World Health Organization declared a global pandemic as COVID- 19 hospitalizations and emergency medical system activations increased. During its peak, stroke admissions and care were significantly affected as the health systems were overwhelmed with the management of patients affected with COVID-19. The impact was significant on the non-COVID-19 emergency profile [1]. Systems needed reorganization to balance care of non-COVID cases as well as protection of health care workers.
Studies reported a decline in the rates of stroke hospitalizations and the proportion of patients receiving reperfusion therapies like intravenous thrombolysis and/or mechanical thrombectomy for acute ischemic stroke [[2], [3], [4]]. One study from Europe showed a sharp drop in non-COVID-19 related CT scans done during the pandemic period when compared with a similar period in 2019 [5]. Also, disruption of routine health services and medical supplies resulted in increased morbidity and avoidable mortality in patients with non-communicable diseases [6]. A questionnaire-based survey conducted among neurologists in 13 major centers of India showed a 61.22% reduction in weekly stroke cases during the lockdown period [7]. In a study from Belgium, primary care providers observed disruption in the delivery of chronic care for conditions like diabetes and hypertension during the COVID-19 pandemic [8]. Individuals with multimorbidity (43%) reported more challenges compared to those with single condition (35%) [9]. The most challenging issue was physician consultation followed by diagnostic investigations (26%). Transport logistics (33%), financial arrangements (26%), mobility-restrictions (21%), and fear of going to hospital owing to the risk of contagion (18%) were other prominent reported factors [9]. There was evidence of fall in screening tests for diabetes and dyslipidemia during months of February, March 2020 with modest rebound in early April 2020 [10]. These preventive services, routine monitoring, and treatment of lipid disorders and diabetes may have both short and longterm consequences. It is therefore essential to observe how the COVID pandemic influenced care of acute stroke patients.
2. Aims
The current study aims to examine whether COVID-19 pandemic affected the management of stroke patients. We aimed to observe differences if any in the rate of stroke admissions, acute stroke management including thrombolysis or thrombectomy, stroke metrics, etiological evaluation, morbidity, and mortality between the stroke patients seen during the period of ongoing COVID-19 pandemic between February and July 2020 and a similar epoch in the year 2019.
3. Methods
The COVID stroke study group (CSSG) India included 18 stroke centers spread across east, west, north and south of the country. This study had a retrospective as well as a prospective component. The study was approved by the institutional ethics committee. Written informed consent was taken from the patients or their legally authorized representative. Stroke data was prospectively collected for the period between February 2020 to July 2020. The retrospective data between February 2019 and July 2019 was collected from in-hospital patient records. All admitted acute stroke patients were included. Details of total stroke patients seen, monthly stroke admissions, demographics, type of stroke, treatment details, interventions, duration of stay, investigations, subtyping of ischemic stroke, in hospital complications, mortality and three months outcome on the modified Rankin score (mRS) were analyzed. Details of timings including door to CT, CT to needle, door to needle, onset to needle (for patients undergoing thrombolysis) and CT to puncture time, recanalization and total procedure time (among patients undergoing endovascular treatment) were recorded. Three months mRS was prospectively collected telephonically for patients seen in 2020 and retrospectively retrieved from either the database maintained by stroke centers or assessed from medical records for the year 2019. Data that was available was included in the final analysis. Data was presented as mean (SD) or median (IQR) and frequency(%). Continuous variables were compared using students t-test (following normal distributions) or Wilcoxon's rank sum test (Non-normal distribution). Qualitative variables were compared using Chi-square/Fisher's exact test. A two-tailed p value of ≤ 0.05 was considered as significant. Adjusted p values (q value) for comparisons between different variables during the two periods of the study were generated using Benjamini-Hochberg procedure. q values <0.05 were considered significant.Stata version14 (StataCorp, Lakeway Drive College Station, Texas, USA) was used for analysis.
4. Results
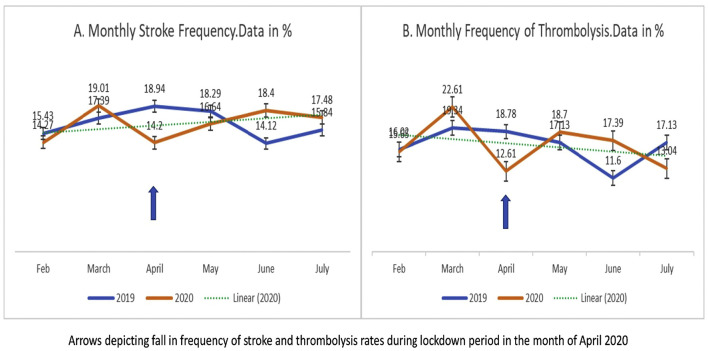
A total of 2549 patients were seen in both study periods; 1237 patients (48.53%) in year 2019 and 1312 (51.47%) in the year 2020. Although overall monthly stroke frequency did not reflect any specific trend, a sharp decline in stroke admissions was observed in the month of April 2020, which seemed to improve and stabilize by July 2020 (Fig. 1A). Among 1237 strokes in 2019, 1032 (83.43%) were ischemic stroke, 185(14.95%) were intracerebral hemorrhage (ICH) and 20 (1.62%) were diagnosed as cerebral venous thrombosis (CVT). Of 1312 strokes in 2020, 1056 (80.55%) were ischemic stroke, 237(18.08%) were ICH and 18 (1.37%) were CVT (p = 0.09).
Fig. 1.
Line diagram showing monthly frequency of stroke patients and thrombolysis rates during the study period in 2019 and 2020.
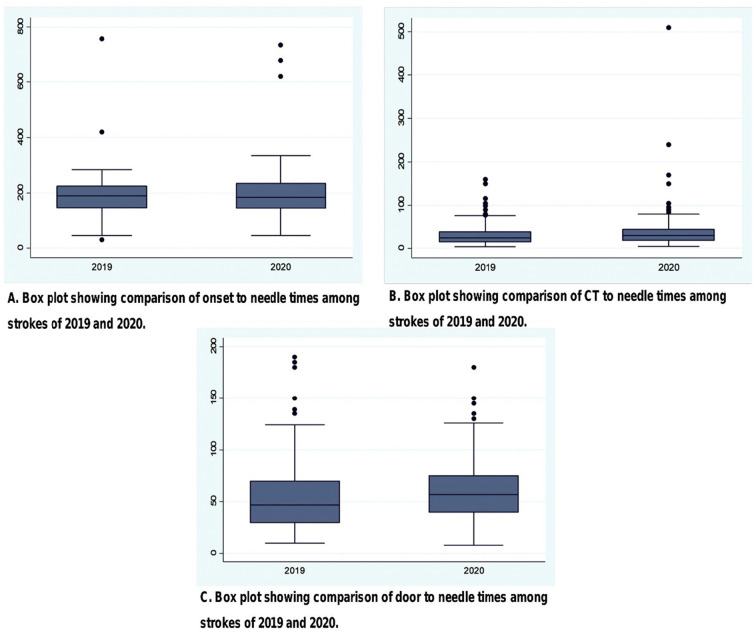
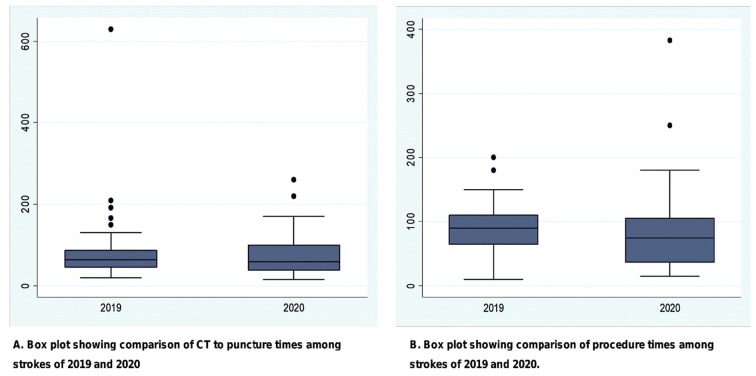
Demographic and clinical details are presented in Table 1 . The mean age of patients was comparable in the two study periods; 58.5±15.11 years in 2019 and 59.21±14.32 years in 2020 (p = 0.17). No differences in proportion of male or female gender were observed. NIHSS and ASPECTS scores and mean ICH volume were comparable between patients seen in both time points. However, the mean ICH score was less in patients seen in 2020 than in 2019 (2.14±1.46 vs 1.86±1.37 respectively, (p = 0.04). 91.64% patients underwent vascular imaging for stroke assessment in 2019 compared with 83.19% in 2020 (p = 0.00001). Treatment and evaluation details are outlined in Table 2 . The door to CT time was comparable for both years. (p = 0.47). Intravenous thrombolysis was given in 182 (17.93%) patients during the study period in 2019 compared with 230 (21.84%) patients in 2020 (p = 0.03). There was a fall in rate of intravenous thrombolysis during the month of April 2020, which stabilized thereafter (Fig. 1B). rTPA (recombinant tissue plasminogen activator) was used in 152 (83.06%) patients and TNK (tenecteplase) in 31 (16.94%) patients in the year 2019 compared with 203 (88.65%) and 26 (11.35%) respectively in 2020 (p = 0.11). Door to needle and CT to needle time were higher among patients treated in 2020 (p = 0.01 and 0.005 respectively, Fig. 2 ). Among eligible patients, 74 (63.25%) patients underwent endovascular therapy (EVT) in 2019, compared with only 43 (36.75%) patients in 2020 (p = 0.00007). No significant difference was observed in the CT to puncture time, recanalization time and total procedure time between the two years (Fig. 3 ). Echocardiography was performed in 1014 (89.18%) patients in 2019 and 970 (79.38%) patients in 2020 (p = 0.00001). Among patients where data was available, Holter was performed in 448 of 771 (58.1%) ischemic stroke patients in 2019 and 433 of 808 (53.6%) ischemic strokes in 2020 (p = 0.07).
Table 1.
Comparison Of Patient Demographics, Evaluation, and Outcomes during the study period between strokes of 2019 and 2020.
| Feb-July 2019 | Feb-July 2020 | p value | q value | |
|---|---|---|---|---|
| Total patients | 1237 | 1312 | - | |
| Age | 58.50+/-15.11 | 59.21+/-14.32 | 0.17 | |
|
Type of stroke IS ICH CVT |
1032 (83.43%) 185 (14.96%) 20 (1.62%) |
1056 (80.55%) 237 (18.08%) 18 (1.37%) |
0.09 |
0.16 |
| Vascular imaging | 1042(91.64%) N= 1137 |
1025(83.19%) N= 1232 |
0.00001 | 0.0002 |
| NIHSS | 9.86 +/-6.12 N=1088 |
9.99+/-6.0 N=1214 |
0.49 | |
| ASPECTS | 9 (2) N=976 |
9 (1) N=888 |
0.10 | |
| ICH volume | 24.04+/-25.4 N=151 |
20.68+/-21.9 N=168 |
0.21 | |
| ICH score | 2.14+/-1.46 N=154 |
1.86+/-1.37 N=165 |
0.04 | |
| Echo | 1014 (89.18%) N=1137 |
970 (79.38%) N= 1222 |
0.00001 | 0.0001 |
| Holter | 448 (58.1%) N=771 |
433 (53.58%) N= 808 |
0.07 | |
| In hospital complications | 170 (15.08%) N=1127 |
208 (17.92%) N=1161 |
0.06 | |
|
Complication type Pneumonia DVT Bedsore Blood stream infection Cardiac UTI More than one |
78 (50%) 7 (4.48%) 24 (15.38%) 16 (10.25%) 6 (3.84%) 19 (12.17%) 6 (3.85%) N=156 |
110(57.5%) 3 (1.57%) 13 (6.8%) 18 (9.42%) 4 (2.09%) 20 (10.47%) 23 (12.04%) N=191 |
0.09 0.09 0.008 0.46 0.25 0.36 0.004 |
0.15 |
| Total hospital stay | 7.66+/-7.34 N=1132 |
7.99+/-6.53 N=1183 |
0.0006 | 0.002 |
| In hospital mortality | 47 (4.12%) N=1142 |
82 (6.91%) N=1187 |
0.003 | 0.01 |
| 3 months mortality | 85 (8.3%) N=1024 |
149 (11.96%) N=1245 |
0.004 | 0.01 |
| 3 Months mRS (0-2) | 585 (59.09%) N=990 |
724 (56.87%) N= 1273 |
0.30 |
Data is in n% or mean+/SD or median (IQR). IS: ischemic stroke; ICH: intracerebral hemorrhage; CVT: cerebral venous thrombosis; NIHSS: National Institutes of Health Stroke Scale; ASPECTS: Alberta stroke program early CT score; DVT: Deep Venous Thrombosis; UTI: Urinary Tract Infection.
Table 2.
Comparison of stroke treatment details during the study period between 2019 and 2020.
| Feb-July 2019 | Feb-July 2020 | p value | q value | |
|---|---|---|---|---|
| Door to CT time | 30(30) | 30(30) | 0.47 | |
| N = 1073 | N = 1136 | |||
| Thrombolysis | 182(17.93%) | 230 (21.84%) | 0.03 | 0.06 |
| N = 1015 | N = 1053 | |||
| *Onset to needle time | 190 (77.5) | 185.5(88.5) | 0.74 | |
| N = 168 | N = 216 | |||
| *Door to needle | 47(40) | 57(35) | 0.01 | 0.02 |
| N = 167 | N = 214 | |||
| *CT to needle | 24(25) | 30(26) | 0.005 | 0.001 |
| N = 166 | N = 214 | |||
| EVT | 74 (63.25%) | 43 (36.75%) | 0.00007 | 0.0003 |
| N = 471 | N = 542 | |||
| *CT to puncture time | 64(41) | 59(61) | 0.46 | |
| N = 67 | N = 39 | |||
| *Puncture to recanalization time | 56 (46) | 45(36) | 0.35 | |
| N = 52 | N = 35 | |||
| Recanalization | 57 (82.6%) | 38 (92.6%) | 0.13 | |
| N = 69 | N = 41 | |||
| *Total procedure time | 90 (45) | 75 (68) | 0.21 | |
| N = 54 | N = 34 | |||
| Aspirin | 833(86.77%) | 806(86.75%) | 0.99 | |
| N = 960 | N = 929 | |||
| Clopidogrel | 468(54.86%) | 515(55.97%) | 0.23 | |
| N = 853 | N = 920 | |||
| Statin | 885 (91.52%) | 854(86.18%) | 0.0001 | |
| N = 967 | N = 991 | |||
| OAC | 109 (22.19%) | 64 (21.47%) | 0.81 | |
| N = 491 | N = 298 | |||
| Surgical intervention | 100 (18.38%) | 67 (17.31%) | 0.67 | |
| N = 544 | N = 387 | |||
| Type of surgical intervention | ||||
| DCH | 57 (58.1%) | 32(49.23%) | ||
| Hematoma evacuation | 13(13.26%) | 11(16.92%) | ||
| EVD | 10 (10.2%) | 6 (9.23%) | ||
| DCH + HE | 11(11.22%) | 8(12.3%) | ||
| Endarterectomy | 0 | 4 (6.15%) | ||
| Stenting | 7 (7.14%) | 4 (6.15%) | ||
| N = 98 | N = 65 |
Data is in n% or mean+/SD or median (IQR). N denotes available data; * duration in minutes; EVT: Endovascular Therapy; OAC: Oral Anticoagulant; DCH: Decompressive Hemicraniectomy; EVD: External Ventricular Drain; HE: Hematoma Evacuation.
Fig. 2.
Comparison Of Time Intervals For Thrombolysis during the study period in 2019 and 2020.
Fig. 3.
Comparison Of Time Intervals For endovascular treatment during the study period in 2019 and 2020.
Although data was not available for all patients, the use of antiplatelets and oral anticoagulation were comparable and statin was lower compared to year 2019 (Table 2). Surgical intervention where indicated was performed among 100 (18.38%) patients in 2019 compared with 67 (17.31%) patients in 2020 (p = 0.67). In-hospital complications and type of complications were comparable (p = 0.06). However, higher patients had multiple infections in 2020 [23(12.04%)] versus 6(3.85%) in 2019 (p = 0.04)].Table 1. Mean total hospital stay (in days) was higher in 2020; 7.66±7.34 in 2019 compared to 7.99±6.53 days in 2020, p = 0.0006. Both in-hospital mortality and three months mortality was higher in the year 2020 compared to 2019 (Table 1). mRS data was available for 990 (1237) patients for the year 2019 and 1273 (1312) patients for the year 2020. The mRS was dichotomized into good (0–2) and poor (3–6) outcome. 585 (59.09%) patients achieved good outcome in the year 2019 compared with 724 (56.87%) in 2020 (p = 0.30) (Fig. 4 ).
Fig. 4.
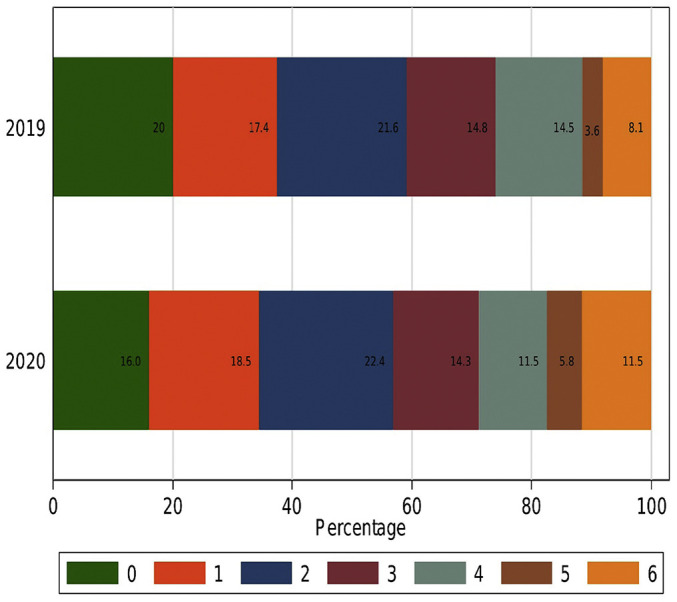
Outcome comparison on mRS scores for stroke patients seen during the study period in 2019 and 2020.
5. Discussion
The present study did not find any difference in the total number of stroke admissions between the two study periods although a decline in the April 2020 correlated with the increasing surge of COVID-19 cases and the acute lockdown period starting from late March 2020. Earlier reports have suggested a significant decline in stroke and coronary artery admissions, possibly related to the reduced number of patients reporting to the hospitals due to fear of COVID-19 or overwhelmed health systems not prioritizing such admissions [[11], [12], [13], [14], [15]]. It is possible that since most of the centres were not admitting COVID positive patients, the usual number of stroke admissions remained constant. Another study observed that although stroke codes were reduced in 2020, stroke admissions remained constant as in the present study [16]. Interestingly, contrary to what was perceived and has been observed previously, the overall rate of thrombolysis was not changed during the pandemic period [17]. However, as mentioned above, the sharp decline in thrombolysis in April 2020 correlates well with the reduction of stroke admissions during the sudden surge of COVID-19 cases, lockdowns and overwhelmed health care facilities [18]. As most of the sites in the present study are established stroke centres, it is likely that acute stroke management remained a priority and reorganization of care pathways during the pandemic stabilized the rate of stroke admissions and thrombolysis [19]. However, higher door to needle and CT to needle times do suggest a possible delay during the screening process in the emergency department or systems being reorganised to optimise treatments in the emergency. This could also reflect a possible influence of risk concerns and delay in acceptance by the patient/families to consent for thrombolysis during the pandemic period [20]. A significant reduction in rates of EVT was observed. As reported in other countries as well, EVT may have declined due to stricter screening guidelines, concerns of COVID risk to the health care workers, apprehension of interventional teams in the absence of RTPCR (Real Time Polymerase Chain reaction) reports (as it takes few hours), overwhelmed health care systems for COVID care, delay in interhospital transfer etc. [[21], [22], [23]] For such reasons, protected stroke code was introduced as a concept [24]. Guidelines and recommendations were made to continue comprehensive stroke treatment by system changes and strengthening the spokes in a hub and spoke model to maintain work flow metrics [[25], [26], [27], [28]].
Reorganization of services evolved with time. In a survey conducted among the study sites, designated COVID positive and negative zones were established in the emergency. A protected stroke code was initiated and majority of the centres started rapid triaging of stroke patients through a separate stroke corridor. Limited centers also maintained a dedicated imaging for COVID patients and CT lung was parallelly performed as an add on screening tool. Although most centres thrombolysed without mandatory COVID testing, some centres used Rapid Antigen test for screening. However, COVID testing was mandatory before thrombectomy, preferably by using Rapid antigen test in most sites.
To maintain optimum care for non-COVID emergencies, a second triage using a more inclusive, dynamic checklist and a mandatory holding in the system-specific in-patient area was helpful among one of the study sites [29]. A reduction in number of investigations during the pandemic period is likely due to the concerns of increased patient movement within the hospital and risk of COVID exposure and vice versa. It is possible that the focus was on providing optimum acute care and shortening the hospital stay. During the lockdown period, in hospitals where COVID care was also being provided, specialized investigations were limited to patients who needed them most. Reorganization of health systems, however did improve the overall care of stroke patients [30].
Higher mortality was observed in the pandemic study period. Published observations suggest both an increase in mortality during the pandemic period and no significant change [[31], [32], [33]]. However, a higher number of patients with missing information in 2019 may have caused an imbalance in results. Many factors could potentially contribute to this observation including delayed patient arrivals to the hospital, delayed in-hospital treatment, decline in use of EVT for LVO (Large Vessel Occlusion) patients, increased in-hospital complications, suboptimum rehabilitation and home care by the family members (although data was not explicitly collected for this) and inadequate follow up. Family members may have had difficulty bringing patients to the hospitals during the peak of pandemic and lockdown period as routine outpatient department care was affected. However, reorganization of health systems from established stroke centre showed that outcomes and workflow metrics were preserved even during the pandemic [2,30]. Improvement in stroke admissions and thrombolysis rates after April 2020 in the present study could also reflect a similar phenomenon.
The study has limitations. 2019 data being retrospective, contributed to missing information of outcomes and investigations and may have introduced some bias. Even during the pandemic, complete data reporting was not possible due to limitations of retrieval and follow-up of patients at some centres.
6. Conclusions
Although, overall number of stroke admissions and rates of thrombolysis were similar in both years, some workflow metrics were delayed and mortality was higher during the pandemic study period. Reorganization of stroke treatment pathways during the pandemic has likely improved the delivery of stroke care across the globe.
Data access statement
The relevant anonymized patient-level data are available via request from the authors.
Sources of Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Disclosures
None.
Grant support
None.
Declaration of Competing Interest
The Authors declare that there is no conflict of interest.
Acknowledgments
Acknowledgement
We thank Ayush Mohan, Archana Sharma, Deepak Yadav, Mohit Anand, Rahul Singhal, Rahul Onam, Prashant Bhatale, Seetha Lakshmi, Saranya Gomathy, Priyanka Sehrawat, Kamlesh Tayade, Ankit Goyal, Akhil Sahib, Govinda Siripurapu, Srujana Billa, Saman Fatima, Satish Barki and Pedapati Radhakrishna for their help in the data collection. We thank all the faculty, residents and nursing staff who were involved in management of stroke patients.
References
- 1.Steinman M., de Sousa J.H.B., Tustumi F., Wolosker N. The burden of the pandemic on the non-SARS-CoV-2 emergencies: A multicenter study. Am. J. Emerg. Med. 2021;42:9–14. doi: 10.1016/j.ajem.2020.12.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rudilosso S., Laredo C., Vera V., Vargas M., Renú A., Llull L., Obach V., Amaro S., Urra X., Torres F., Jiménez-Fàbrega F.X., Chamorro Á. Acute Stroke Care Is at Risk in the Era of COVID-19: Experience at a Comprehensive Stroke Center in Barcelona. Stroke. 2020;51:1991–1995. doi: 10.1161/STROKEAHA.120.030329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yaghi S., Ishida K., Torres J. SARS-CoV-2 and stroke in a New York Healthcare System. Stroke. 2020;51:2002–2011. doi: 10.1161/STROKEAHA.120.030335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Onteddu S.R., Nalleballe K., Sharma R., Brown A.T. Underutilization of health care for strokes during the COVID-19 outbreak. Int. J. Stroke. 2020;15:NP9–NP10. doi: 10.1177/1747493020934362. [DOI] [PubMed] [Google Scholar]
- 5.Boeken T., Le Berre A., Mebazaa A., Boulay-Coletta I., Hodel J., Zins M. Non-COVID-19 emergencies: where have all the patients gone? Eur. Radiol. 2020:1–2. doi: 10.1007/s00330-020-06961-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kluge H.H.P., Wickramasinghe K., Rippin H.L., Mendes R., Peters D.H., Kontsevaya A. Prevention and control of non-communicable diseases in the COVID-19 response. Lancet. 2020;395:1678–1680. doi: 10.1016/S0140-6736(20)31067-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sylaja P.N., Srivastava M.V.P., Shah S., Bhatia R., Khurana D., Sharma A., Pandian J.D., Kalia K., Sarmah D., Nair S.S., Yavagal D.R., Bhattacharya P. The SARS-CoV-2/COVID-19 pandemic and challenges in stroke care in India. Ann. N. Y. Acad. Sci. 2020;1473:3–10. doi: 10.1111/nyas.14379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Danhieux K., Buffel V., Pairon A., Benkheil A., Remmen R., Wouters E. The impact of COVID-19 on chronic care according to providers: a qualitative study among primary care practices in Belgium. BMC Fam. Pract. 2020;21(1):255. doi: 10.1186/s12875-020-01326-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pati S., Mahapatra P., Kanungo S., Uddin A., Sahoo K.C. Managing Multimorbidity (Multiple Chronic Diseases) Amid COVID-19 Pandemic: A Community Based Study From Odisha, India. Frontiers in Public Health. 2021;8:1026. doi: 10.3389/fpubh.2020.584408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wright A., Salazar A., Mirica M., Volk L.A., Schiff G.D. The Invisible Epidemic: Neglected Chronic Disease Management During COVID-19. J. Gen. Intern. Med. 2020 Jul;14:1–2. doi: 10.1007/s11606-020-06025-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pines J.M., Zocchi M.S., Black B.S., Celedon P., Carlson J.N., Moghtaderi A. The effect of the COVID-19 pandemic on emergency department visits for serious cardiovascular conditions. Am. J. Emerg. Med. 2021;47:42–51. doi: 10.1016/j.ajem.2021.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.de Havenon A., Ney J., Callaghan B. Decreased Stroke, Acute Coronary Syndrome, and Corresponding Interventions at 65 US Hospitals Following COVID-19. “Preprint.”. medRxiv. 2020 doi: 10.1101/2020.05.07.20083386. [DOI] [Google Scholar]
- 13.Diegoli H., Magalhães P.S.C., Martins S.C.O., Moro C.H.C., França P.H.C., Safanelli J., Nagel V., Venancio V.G., Liberato R.B., Longo A.L. Decrease in Hospital Admissions for Transient Ischemic Attack, Mild, and Moderate Stroke During the COVID-19 Era. Stroke. 2020;51:2315–2321. doi: 10.1161/STROKEAHA.120.030481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bersano A., Kraemer M., Touzé E., Weber R., Alamowitch S., Sibon I., Pantoni L. Stroke care during the COVID-19 pandemic: experience from three large European countries. Eur. J. Neurol. 2020;27:1794–1800. doi: 10.1111/ene.14375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Clotilde Balucani, Ricardo Carhuapoma J., Canner Joseph K., Roland Faigle, Brenda Johnson, Anna Aycock. Exploring the Collateral Damage of the COVID-19 Pandemic on Stroke Care. Stroke. 2021;52(5):1822–1825. doi: 10.1161/STROKEAHA.121.034150. [DOI] [PubMed] [Google Scholar]
- 16.Bres Bullrich M., Fridman S., Mandzia J.L., Mai L.M., Khaw A., Vargas Gonzalez J.C., Bagur R., Sposato L.A. COVID-19: Stroke Admissions, Emergency Department Visits, and Prevention Clinic Referrals. Can J Neurol Sci. 2020;47:693–696. doi: 10.1017/cjn.2020.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hsiao J., Sayles E., Antzoulatos E., Stanton R.J., Sucharew H., Broderick J.P., Demel S.L., Flaherty M.L., Grossman A.W., Kircher C., Kreitzer N., Peariso K., Prestigiacomo C.J., Shirani P., Walsh K.B., Lampton H., Adeoye O., Khatri P. Effect of COVID-19 on Emergent Stroke Care: A Regional Experience. Stroke. 2020;51:e2111–e2114. doi: 10.1161/STROKEAHA.120.030499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Altersberger Valerian L., Stolze Lotte J., Heldner Mirjam R., Hilde Henon, Nicolas Martinez-Majander, Christian Hametner, TRISP Collaborators. Maintenance of Acute Stroke Care Service During the COVID-19 Pandemic Lockdown. Stroke. 2021;52(5):1693–1701. doi: 10.1161/STROKEAHA.120.032176. (STROKEAHA.120.032176) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hoyer C., Ebert A., Huttner H.B., Puetz V., Kallmünzer B., Barlinn K., Haverkamp C., Harloff A., Brich J., Platten M., Szabo K. Acute Stroke in Times of the COVID-19 Pandemic: A Multicenter Study. Stroke. 2020;51:2224–2227. doi: 10.1161/STROKEAHA.120.030395. [DOI] [PubMed] [Google Scholar]
- 20.Siegler J.E., Zha A.M., Czap A.L., Ortega-Gutierrez S., Farooqui M., Liebeskind D.S. Influence of the COVID-19 Pandemic on Treatment Times for Acute Ischemic Stroke. Stroke. 2021 Jan;52(1):40–47. doi: 10.1161/STROKEAHA.120.032789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kerleroux B., Fabacher T., Bricout N., Moïse M., Testud B., Vingadassalom S., Ifergan H., Janot K., Consoli A., Ben Hassen W., Shotar E., Ognard J., Charbonnier G., L’Allinec V., Guédon A., Bolognini F., Marnat G., Forestier G., Rouchaud A., Pop R., Raynaud N., Zhu F., Cortese J., Chalumeau V., Berge J., Escalard S., Boulouis G. SFNR, the ETIS registry, and the JENI-Research Collaborative. Mechanical Thrombectomy for Acute Ischemic Stroke Amid the COVID-19 Outbreak: Decreased Activity, and Increased Care Delays. Stroke. 2020;51:2012–2017. doi: 10.1161/STROKEAHA.120.030373. [DOI] [PubMed] [Google Scholar]
- 22.Chowdhury T., Rizk A.A., Daniels A.H., Al Azazi E., Sharma D., Venkatraghavan L. Management of Acute Ischemic Stroke in the Interventional Neuroradiology Suite During the COVID-19 Pandemic: A Global Survey. J. Neurosurg. Anesthesiol. 2021;33:44–50. doi: 10.1097/ANA.0000000000000734. [DOI] [PubMed] [Google Scholar]
- 23.Hajdu S.D., Pittet V., Puccinelli F., Ben Hassen W., Ben Maacha M., Blanc R. Acute Stroke Management During the COVID-19 Pandemic: Does Confinement Impact Eligibility for Endovascular Therapy? Stroke. 2020;51(8):2593–2596. doi: 10.1161/STROKEAHA.120.030794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Khosravani H., Rajendram P., Notario L., Chapman M.G., Menon B.K. Protected Code Stroke: Hyperacute Stroke Management During the Coronavirus Disease 2019 (COVID-19) Pandemic. Stroke. 2020;51:1891–1895. doi: 10.1161/STROKEAHA.120.029838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yaeger K.A., Fifi J.T., Lara-Reyna J., Rossitto C., Ladner T., Yim B., Hardigan T., Maragkos G.A., Shigematsu T., Majidi S., Mocco J. Initial Stroke Thrombectomy Experience in New York City during the COVID-19 Pandemic. AJNR Am. J. Neuroradiol. 2020;41:1357–1360. doi: 10.3174/ajnr.A6652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bhatia R., Sylaja P.N., Srivastava M.V.P., Khurana D., Pandian J.D., Suri V., Kumar V.G.P., Kumaravelu S., Huded V., Surya N., Sharma A., Kaul S. Consensus Statement - Suggested Recommendations for Acute Stroke Management during the COVID-19 Pandemic: Expert Group on Behalf of the Indian Stroke Association. Ann. Indian Acad. Neurol. 2020;23:S15–S23. doi: 10.4103/aian.AIAN_302_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Papanagiotou P., Parrilla G., Pettigrew L.C. Thrombectomy for Treatment of Acute Stroke in the COVID-19 Pandemic. Cerebrovasc. Dis. 2021;50(1):20–25. doi: 10.1159/000511729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Qureshi A.I., Abd-Allah F., Al-Senani F., Aytac E., Borhani-Haghighi A., Ciccone A., Gomez C.R., Gurkas E., Hsu C.Y., Jani V., Jiao L., Kobayashi A., Lee J., Liaqat J., Mazighi M., Parthasarathy R., Miran M.S., Steiner T., Toyoda K., Ribo M., Gongora-Rivera F., Oliveira-Filho J., Uzun G., Wang Y. Management of acute ischemic stroke in patients with COVID-19 infection: Insights from an international panel. Am J Emerg Med. 2020;38 doi: 10.1016/j.ajem.2020.05.018. 1548.e5-1548.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gupta A., Vishnu V.Y., Singh M.B., Bhatia R., Rajan R., Vibha D. Managing Non-COVID acute neurology amidst the pandemic: Challenges and work in progress. Annals of Indian Academy of Neurology. 2021 Jan 1;24 doi: 10.4103/aian.AIAN_999_20. cited 2021 Apr 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fuentes B., Alonso de Leciñana M., Calleja-Castaño P., Carneado-Ruiz J., Egido-Herrero J., Gil-Núñez A., Masjuán-Vallejo J., Vivancos-Mora J., Rodríguez-Pardo J., Riera-López N., Ximénez-Carrillo Á., Cruz-Culebras A., Gómez-Escalonilla C., Díez-Tejedor E. en representación de los hospitales del Plan Ictus Madrid. Impact of the COVID-19 pandemic on the organisation of stroke care. Madrid Stroke Care Plan. Neurologia. 2020;35(6):363–371. doi: 10.1016/j.nrl.2020.05.007. English, Spanish. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Richa Sharma, Kuohn Lindsey R., Weinberger Daniel M., Warren Joshua L., Sansing Lauren H., Adam Jasne. Excess Cerebrovascular Mortality in the United States During the COVID-19 Pandemic. Stroke. 2021 Feb 1;52(2):563–572. doi: 10.1161/STROKEAHA.120.031975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sarfo F.S., Mensah N.O., Opoku F.A., Adusei-Mensah N., Ampofo M., Ovbiagele B. COVID-19 and stroke: Experience in a Ghanaian healthcare system. Journal of the Neurological Sciences. 2020:416. doi: 10.1016/j.jns.2020.117044. cited 2021 Apr 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wallace A.N., Asif K.S., Sahlein D.H., Warach S.J., Malisch T., LaFranchise E.F. Patient Characteristics and Outcomes Associated with Decline in Stroke Volumes During the Early COVID-19 Pandemic. J. Stroke Cerebrovasc. Dis. 2021;30:105569. doi: 10.1016/j.jstrokecerebrovasdis.2020.105569. [DOI] [PMC free article] [PubMed] [Google Scholar]