Abstract
Background and aim
During the Coronavirus 2019 (COVID-19) crisis, there has been a huge demand for medications and unprecedented utilization of intensive care unit (ICU) services that subsequently and profoundly impacted the quality of medical care provided to COVID-19 patients. This study aimed to shed light on the role of pharmacists on the health care provided to critically ill COVID-19 patients.
Methods
A retrospective study, was conducted in Diriyah hospital in Riyadh, Saudi Arabia on all COVID-19 patients admitted to the ICU between June 27th and August 15th, 2020 until patients were transferred to the medical ward, discharged, or deceased. All medication related interventions performed by pharmacists have been documented electronically, collected and subsequently categorized and analyzed.
Results
The mean age of patients was 58.8 years (±12.98 SD), with age of >64 years in approximately 37%. Four hundred and seventy interventions (470) were made by pharmacists of which 32%, 11.7%, 4%, 2.6%, 2.1% were due to error in dosing regimens, drug duplication, missing drug information, drugs requiring prior authorization, and missing critical information, respectively; while 40.6% were due to medication shortage of which 40.3% were substituted with alternative medications. Based on the analysis of drugs involved in interventions, medication groups that were mainly associated with interventions included antibiotics (16.8%), electrolytes/minerals (11.7%) and vitamins (9.4%).
Conclusion
During health crises such as COVID-19 pandemic, the role of pharmacists in the ICU services becomes extremely crucial for providing better patients’ outcomes. Further studies should be conducted to follow up these findings in the context of COVID-19 pandemic.
Keywords: COVID-19, ICU patients, Pharmacist, Interventions
1. Introduction
Declaring Coronavirus 2019 (COVID-19) pandemic by the World Health Organization on March 11, 2020 (Tang et al., 2020, World Health Organization, xxxx), imposed a significant challenge on the global healthcare services and resources. During this crisis, there has been a huge demand for medications and unprecedented utilization of intensive care unit (ICU) services (World Health Organization, 2020), that has subsequently and profoundly impacted the quality of medical care provided to COVID-19 patients. Although respiratory distress and failure caused by SARS-CoV-2 is known to jeopardize the patients’ lives, medication errors (MEs) and adverse drug events (ADEs) represent additional life-threatening factors.
All ICU cases are complicated in the sense that they require more parameters monitoring, multiple high-risk medications administration and are subjected to more frequent changes in therapeutic plans (Cullen et al., 1997, Moyen et al., 2008, Klopotowska et al., 2010). However, with COVID-19 pandemic, the situation has become more complex that consequently made the critically ill COVID-19 patients more vulnerable to MEs and ADEs.
Medication errors (MEs) represent a major concern globally. Early studies have estimated that MEs account for 7000 deaths annually in the United States (Phillips et al., 1998, Phillips et al., 2001). Whereas recent reports have shown that the number is underestimated as MEs may account for up to 251,000 deaths a year in the U.S. (Makary and Daniel, 2016, Anderson and Abrahamson, 2017). Drug related mortality and morbidities have a major economic burden on the American health care system, as their cost was estimated to exceed $177 billion annually (Ernst and Grizzle, 2001). This underlines the significant role that pharmacists can play to provide the most economically saving therapies and more importantly ensure patients’ safety during the treatment process.
Pharmacists have a crucial role in emergency medical services (EMS), including the ICU, through participation in planning pharmacotherapies and decisions related to clinical parameters evaluation and drug monitoring (Kane et al., 2003). Their interventions represent the first line defense that prevents MEs and ADEs from occurring in the first place, ultimately improving the medication safety. Beyond this, their presence in the ICU and consultation with ICU physicians have shown to reduce the consumed quantities of drugs, which was correlated with a reduction in the cost of drug therapy (Aljbouri et al., 2013, Montazeri and Cook, 1994), and prevent inappropriate drug use or ADEs, thus avoiding their attributable cost (MacLaren et al., 2021, MacLaren and Devlin, 2019). More details regarding contribution of pharmacists in the ICU is discussed elsewhere (Preslaski et al., 2013).
Despite the wealth of literature with the role of ICU pharmacists in general, there is a paucity of research on the role of pharmacists on the ICU admitted COVID-19 patients. This study aimed to explore the role of pharmacists in the ICU services provided to the critically ill COVID-19 patients. The overall goal of the study was to highlight the major types of pharmacists’ interventions and MEs that pharmacists experience during caring for critically ill COVID-19 patients to draw the practitioners’ attention to areas where they need to be more vigilant to warrant patients’ safety during this pandemic.
2. Method
This retrospective study was conducted in Diriyah hospital in Riyadh, Saudi Arabia on all COVID-19 patients admitted to the ICU between June 27th and August 15th, 2020. Patients who were admitted before June 27th and after August 15th were excluded from the study. All patients’ cases had been followed between June 27th and August 15th, until patients were transferred out of the ICU, i.e. transferred to the medical ward, discharged, or died. Baseline characteristics including demographic data, medical and disease history as well as pharmacists’ interventions were collected by two on-duty pharmacists and two volunteering pharmacists with no need to informed consent from patients as the study was performed retrospectively. Ten out of twelve on-duty pharmacists provided therapeutic interventions during the study period. Pharmacist intervention in our study is defined as any action taken by the pharmacist on medications ordered to these patients that might have potential measurable impact on the quality of care provided to them during their stay in the ICU (Alderman and Farmer, 2001, Dooley et al., 2004, Mongaret et al., 2018). Following their collection, thery were counted and classified according to the predefined types of interventions built into the utilized software at the hospital. Medication groups or classes corresponded to these interventions were determined. A designed collection sheet was utilized to gather all required information. Data related to pharmacists’ interventions and medications would be reviewed by one junior and 2 senior pharmacists, to ensure interventions align with the type or class provided by the software. Data were analyzed using Microsoft Excel 2019.
3. Results:
3.1. Baseline characteristics
During the study period, one hundred and nine patients were considered, of which thirty were excluded [9 admitted to the medical ward; 16 with inaccessible files since their transfer to Diriyah hospital was cancelled; 3 with inaccessible clinical notes; 2 patients with missing medication lists] that resulted in 79 patients to be included in the study. The mean age of patients was 58.8 years (±12.98 SD), with age of >64 years in approximately 37%, as shown in Table 1. Male patients represented 84.8% and all were non-Saudis. Diabetes and hypertension were the most prevalent comorbidities which were diagnosed in 59.5% and 58% of the patients, respectively. Obesity existed in 38% of the patients, while 29% of patients were classified as overweight. Most of the patients were sedated and mechanically ventilated (87% and 90%, respectively). Further details on baseline characteristics are provided in Table 1.
Table 1.
Clinical baseline characteristics of participants (N = 79).
| Characteristic | Number (%) | ||
|---|---|---|---|
| Age [28 to 86; years] | |||
| < 55 | 34 (43.0) | ||
| 55-64 | 16 (20.3) | ||
| > 64 | 29 (36.7) | ||
| Gender | |||
| Male | 67 (84.8) | ||
| Female | 11 (13.9) | ||
| NA | 1 (1.3) | ||
| Nationality | |||
| Saudi | 0 | ||
| Non-Saudi | 79 (100) | ||
| BMI | |||
| Underweight (< 18.5) | 0 | ||
| Normal (18.5 ≤ to < 25) | 15 (19) | ||
| Overweight (25 ≤ to < 30) | 23 (29.1) | ||
| Obese | 30 (38) | ||
| Class I (30 ≤ to < 35) | 17 (56.7) | ||
| Class II (35 ≤ to < 40) | 8 (26.7) | ||
| Class III (> 40) | 5 (16.6) | ||
| NA | 11 (13.9) | ||
| Medical history | Yes | No | NA |
| Diabetes | 47 | 29 | 3 |
| Hypertension | 46 | 31 | 2 |
| Anemia* | 12 | 41 | 26 |
| IHD | 8 | 46 | 25 |
| A-fib | 3 | 52 | 24 |
| CHF | 1 | 52 | 26 |
| Dyslipidemia | 5 | 47 | 27 |
| Chronic Kidney failure (CKD) | 5 | 72 | 2 |
| Asthma | 2 | 36 | 41 |
| COPD | 2 | 37 | 40 |
| Lung mass (Cancer or TB) | 1 | 78 | 0 |
| Peptic ulcer | 1 | 12 | 66 |
| Schizophrenia | 1 | 78 | 0 |
| Inflammatory bowel syndrome | 1 | 59 | 19 |
| Hypothyroidism | 2 | 77 | 0 |
| Pulmonary embolism | 2 | 77 | 0 |
| stroke | 1 | 78 | 0 |
| Acute renal failure | 2 | 77 | 0 |
| Hyperthyroidism | 1 | 78 | 0 |
| Mechanical ventilation | |||
| Yes | 71 (89.9) | ||
| No | 7 (8.8) | ||
| NA | 1 (1.3) | ||
| Sedation | |||
| Yes | 69 (87.3) | ||
| No | 9 (11.4) | ||
| NA | 1 (1.3) | ||
NA: data is not available for this number of patients.
History of PRBCs transfusion in 8 patients (6 NA; 2 Yes).
3.2. Classification of pharmacists’ interventions based on their types
Four hundred and seventy interventions were made by pharmacists, as shown in Table 2. Of these interventions and based on the predefined types built into the software, 11.7%, 4%, 32%, 2.1% and 2.6% were due to drug duplication, drug information, error in dosing regimen, missing critical information about the patients and absence of prescriber’s privilege, respectively. In addition, 40.6% of the interventions were related to medication shortage as they were out of stock or being nonformulary drugs, of which pharmacists suggested alternatives for 40%, while 60% were left without suggestions due absence of alternative medications, yet they were requested and supplied by the Saudi Ministry of Health (MOH) or other governmental hospitals falling under MOH umbrella. Interventions related to drug order rejection represented only 2%. Further analysis of the interventions under error in dosing regimens type revealed that 53% and 21% were associated to dose and frequency adjustments, respectively. Additional information related the types of interventions, corresponding number of recipients and example for each intervention are provided in Table 2.
Table 2.
Classification of pharmacists’ interventions during ICU admission of COVID-19 patients.
| Interventions | Number of patients with this intervention | Example | Total number of interventions (%) |
|---|---|---|---|
| Drug class duplicate | 33 | Patient is on Vancomycin and prescribed Linezolid | 55 (11.7) |
|
Drug information Missing drug information, direction of use, indication |
14 | Patient is prescribed metronidazole without clear indication; Patient is prescribed phenytoin IV without choosing appropriate diluent |
19 (4.0) |
| Error in dosing regimen | 60 | 151 (32.13) | |
| Dose adjustment | 38 | Propofol was prescribed 500 mg/hr and maximum dose is 390 mg/hr (5 mg/kg/hr) for COVID19 Favipiravir was prescribed 850 mg BID and corrected by pharmacist to 800 mg BID |
80 |
| Frequency adjustment | 23 | Vancomycin was prescribed 1 gm daily, but corrected by pharmacist to BID | 31 |
| Duration adjustment | 4 | Enoxaparin was prescribed for 1 day only but extended by pharmacist for 3 days to be aptt after that. | 4 |
| Infusion rate adjustment | 5 | Potassium chloride is prescribed 80 mg over 6 hrs. However, potassium level was 3.35 WNR and based on hospital protocol it should be on 20 meq /200 ml over 2 hrs. Albumin 20% 100 ml was prescribed to infuse over 30 mins but adjusted by pharmacist to be over 4 hrs |
6 |
| Route of administration Adjustment | 6 | Metoprolol 12.5 mg BID was requested as IV but adjusted by pharmacist to Oral form. | 6 |
| Dose and frequency adjustment | 5 | Colistin was prescribed 3 million units daily but based on Crcl (29.5 ml/min) dose should be 2.5 mu every 12 hrs as suggested by pharmacist Apixaban was prescribed 5 mg daily but patient had PE, so dose was adjusted by pharmacist to 10 mg Bid for 7 days then decreased to 5 mg BID |
8 |
| Dose and infusion rate adjustment | 1 | MgSO4 50% dose and infusion rate were suggested by pharmacist 20 mg/ml (2000 mg/100 ml) or 50 ml (40 mg/ml) over 4 hrs | 1 |
| Infusion rate adjustment and missing diluents | 1 | Phenytoin 1 gm IV was prescribed and suggested by pharmacist to be in 100 ml D5W over 45 mins | 1 |
| Missing dose | 7 | Lactulose prescribed with no dose and 11 ml (11 gm prn) was recommended by pharmacist | 8 |
| Missing frequency | 1 | Dexamethasone prescribed without frequency | 1 |
| Missing infusion rate | 2 | Tranexamic acid 500 mg/5ml qid was prescribed without infusion rate | 2 |
| Missing dose and infusion rate | 1 | Magnesium sulfate was prescribed without dose and frequency and based on Mg level pharmacist recommended 2 gm\100 ml over 4 h | 1 |
| Missing route of administration | 2 | Sodium nitroprusside 50 mg prescribed without route of administration | 2 |
| Medication is not available | 69 | 191 (40.6) | |
| Medication is Not Available either out of stock or not in Formulary with no alternative suggestion | 54 | Beta-Sitosterol 0.25% ointment | 114 |
| Medication is Not Available either out of stock or not in Formulary but alternative suggested | 39 | Meropenem was not available and imipenem was recommended as an alternative | 77 |
|
Other: missing date, Time .. etc Missing patient data, lab values |
9 | Potassium chloride is prescribed, and K level was missed Calcium gluconate was prescribed, and Ca level was missed Amikacin was prescribed, and patient weight was missed |
10 (2.1) |
| Reject drug order | 6 | 9 (1.9) | |
| Reject drug order with justification | 5 | Acetazolamide 500 mg BID was rejected as based on pt. lab results no need to take this medication since bicarbonate and PH were within normal range | 7 |
| Reject drug order without justification | 1 | Cefotaxime was rejected by pharmacist with no clarification | 2 |
| Re-Order Requested | 10 | 17 (3.62) | |
| System error | 10 | – | 14 |
| Order entered by other-registered person | 1 | – | 3 |
| Non-privileged prescriber | 7 | Narcotics and few antibiotics | 12 (2.6) |
| None | 6 | 6 (1.3) | |
| Intervention description not entered | 3 | – | 3 |
| No intervention done during ICU stay | 3 | – | 3 |
3.3. Classification of pharmacists’ intervention based on the pharmacological category of involved medications and their numbers
Many pharmacological groups were associated with the interventions. However, antibiotics (16.8%), electrolytes/minerals (11.7%) and vitamins (9.4%) are considered the most involved categories. Further details are provided in Table 3.
Table 3.
Classification of pharmacists’ interventions based on the pharmacological category of involved medications.
| Interventions in Drugs categories | Total number of medications | Number of involved cases (%) |
|---|---|---|
| Antibiotic | 19 | 79 (16.8) |
| Electrolytes & Minerals | 8 | 55 (11.7) |
| Vitamin | 5 | 44 (9.4) |
| Laxative | 10 | 26 (5.5) |
| Antihypertensive | 10 | 21 (4.5) |
| Antipsychotic | 3 | 19 (4.0) |
| Anticoagulant | 4 | 18 (3.8) |
| Antifungal | 8 | 16 (3.4) |
| Antiulcer | 2 | 15 (3.2) |
| Analgesic | 6 | 11 (2.3) |
| Wound healing drop/ointment | 3 | 10 (2.1) |
| Antiplatelet | 2 | 7 (1.5) |
| Colloid | 1 | 7 (1.5) |
| Vasopressor | 3 | 7 (1.5) |
| Antiepileptic | 3 | 6 (1.3) |
| Antidiabetic | 2 | 5 (1.1) |
| Antihemorrhagic | 2 | 5 (1.1) |
| Antiviral | 1 | 5 (1.1) |
| Steroid | 3 | 5 (1.1) |
| Diuretic | 3 | 4 (0.9) |
| Sedative and anxiolytic | 3 | 4 (0.9) |
| Antiasthmatic | 1 | 3 (0.6) |
| Antiasthmatic-COPD | 1 | 3 (0.6) |
| Hemostatic agent | 1 | 3 (0.6) |
| Antiallergic | 2 | 2 (0.4) |
| Antidote | 2 | 2 (0.4) |
| Antiseptic | 1 | 2 (0.4) |
| Sedative and analgesic | 1 | 2 (0.4) |
| Antiarrhythmic | 1 | 1 (0.2) |
| Antibiotic/Steroid | 1 | 1 (0.2) |
| Antidepressant | 1 | 1 (0.2) |
| Antihyperthyroidism | 1 | 1 (0.2) |
| Lubricant | 1 | 1 (0.2) |
| Neuromuscular blocker | 1 | 1 (0.2) |
| Sedative and anesthetic | 1 | 1 (0.2) |
| Vasodilator | 1 | 1 (0.2) |
| Others | - | 76 (16.2) |
Regarding the number of interventions per patient, it ranged between none in 3 patients to 22 interventions in 1 patient, while many had 3 to 4 interventions, as shown in Table 4.
Table 4.
Patients classification based on the number of interventions implemented by pharmacists.
| Interventions | Number of patients |
|---|---|
| 0 intervention | 3 (3.8) |
| 1 intervention | 8 (10.1) |
| 2 interventions | 4 (5.1) |
| 3 interventions | 11 (13.9) |
| 4 interventions | 14 (17.7) |
| 5 interventions | 5 (6.3) |
| 6 interventions | 5 (6.3) |
| 7 interventions | 8 (10.1) |
| 8 interventions | 5 (6.3) |
| 9 interventions | 3 (3.8) |
| 10 interventions | 3 (3.8) |
| 11 interventions | 2 (2.5) |
| 13 interventions | 1 (1.3) |
| 14 interventions | 2 (2.5) |
| 16 interventions | 2 (2.5) |
| 18 interventions | 1 (1.3) |
| 19 interventions | 1 (1.3) |
| 22 interventions | 1 (1.3) |
3.4. Health complications in COVID-19 patients during ICU stay and patients’ survival
Cardiovascular and respiratory complications were found the most common in this cohort (25.5% and 26%, respectively), as shown in Table 5.
Table 5.
Medical complications in patients during their ICU admission.
| Complications | Number of patients with each complication | Total number of cases (%) |
|---|---|---|
| Cardiovascular system | 139 (25.5) | |
| Tachycardia | 21 | |
| Bradycardia | 22 | |
| Hypertension | 13 | |
| Hypotension | 30 | |
| Septic shock | 22 | |
| Others | 31 | |
| Respiratory system | 142 (26%) | |
| Tachypnea | 14 | |
| Pneumonia | 32 | |
| ARDS | 23 | |
| Others | 73 | |
| Urinary system | 53 (9.7) | |
| Oliguria | 20 | |
| Acute Kidney injury | 16 | |
| Others | 17 | |
| Gastrointestinal system | 26 | 26 (4.8) |
| Central nervous system | 37 | 37 (6.8) |
| Dermatological system | 18 (3.3) | |
| Bed sore or skin ulcers | 15 | |
| Other | 3 | |
| Others | 131 (24%) | |
| Fever | 12 | |
| Hyperkalemia | 24 | |
| Hypernatremia | 12 | |
| Hypomagnesemia | 11 | |
| Other | 72 | |
| No complications | 2 | 2 (0.35) |
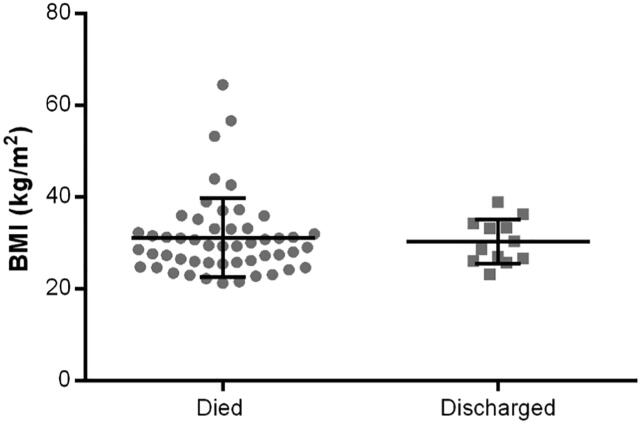
Patients were also categorized based on their survival. Unfortunately, 74.7% (59 patients) died, while only 20.3% (16 patients) survived at the end of the study. Interestingly, when BMI was compared between patients who survived and discharge (12 patients) vs. those who died (51 patients), no significant difference was observed (mean BMI 30.30 kg/m2 vs. 31.2 kg/m2, respectively), as provided in Fig. 1. It is worth to mention that a total of 16 patients from the cohort were excluded from this analysis because of missing BMI and/or survival data (4 patients), missing BMI data only (10 patients) or being transferred to another hospital where survival data could not be obtained (2 patients).
Fig. 1.
Body mass index (BMI) comparison between deceased and survived critically ill COVID-19 patients.
4. Discussion
Many studies have been conducted investigating the essential services delivered by pharmacists during COVID-19 pandemic. Pharmacists had the likely to show a superior role during this pandemic in multiple aspects, such as providing drug information for healthcare providers (Dhahri et al., 2020, Louiselle et al., 2020), patients counseling (Meng et al., 2020), suggestion alternative therapy (Ong et al., 2020), therapeutic drug monitoring (Mongaret et al., 2018), drug supply administration (Ong et al., 2020, Tan et al., 2020) and safety measures for infection control (Ong et al., 2020, Zuckerman et al., 2020). This study sheds light on the services provided by pharmacists to the critically ill COVID-19 patients in Riyadh, Saudi Arabia.
Since the beginning of this pandemic, researchers all over the world started searching different aspects of this novel disease. As the available peer reviewed literature regarding the services of pharmacists provided to COVID-19 patients in the ICU setting has been scarce, it has become of our interest to assess that during the pandemic. Understanding how pharmacists have contributed in providing services to the critically ill COVID-19 patients would highlight their achievements and more importantly expose any gap in their practice giving ample opportunity for future improvements.
Only one study conducted on 22 ICU-admitted COVID-19 patients in China investigating this topic and was published recently by Wang et al. (2021). Wang et al. (2021) have shown that drug discontinuation was the most common recommendation (31.5%; 35 out of 111) while dose adjustment accounted for 15.3%. Despite the slight difference in type of interventions at drug level compared to our study, most of the recommendation based on their observation were related antibiotics (57.7%) which aligns with the current reported results (16.8%; 79 of 470) in spite of the lower rate. As studies discussing this matter are rarely reported (Wang et al., 2021), it becomes challenging to compare our findings to additional studies. Nevertheless, a quick glance on types of interventions made by pharmacists on the critically ill COVID-19 patients reveled some similarities with their interventions at different critical care units. For instance, a study focused on the impact of pharmacists’ interventions with respect to drug-related problems (DRPs) in the ICU has shown 28.9% and 14.3% were related to wrong dosing regimen and no indication for drug use, respectively (Al-Jazairi et al., 2008). Additional study assessing the role of clinical pharmacy services in the oncology ward showed that 26.6%, 21.5% and 10.3% of pharmacist’s interventions were related to drug discontinuation, drug dosing adjustments, and therapeutic drug monitoring (Delpeuch et al., 2015). Further findings from the oncology ward revealed 27.1%, 20.0%, 6.2%, 5.1% of the pharmacist interventions were secondary to drug dosing modifications, therapy discontinuations, recall of the treatment, and replacement of a drug with another one, respectively (Moukafih et al., 2021). Another study conducted by Faqeer and colleagues on identifying DRPs in the oncology ward, showed that addition of medications (38.7%), then discontinuation of medications (25%) were the most common types of interventions followed by dose adjustment secondary to wrong dose (3.7%) (Faqeer et al., 2021). In the internal medical ward, Abunahlah and colleagues showed that inappropriate drug use (44.79%), inappropriate dose (27.61%), and inappropriate medication treatment procedures (21.47%) were the most common interventions identified by the clinical pharmacists (Abunahlah et al., 2018). Although Molino and colleagues’ study was conducted in the outpatients’ setting, they reported similar rate of our interventions related to drug duplication (11.29%), and lower rate of those associated to dose adjustment (20.05%) (Molino Cde et al., 2014).
Comparing with the current literature, our results are in agreement with the type of ICU pharmacists’ interventions seen in the current pharmacy practice in hospitals, reiterating the notion that more attention should be directed towards errors in the prescribed regimens that are mainly attributed to wrong dose and/or frequencies. Our results also showed approximately 60% of the interventions associated to medication shortage were left with no alternative suggestions (117 of 191). Despite that, these medications were requested and supplied by MOH, either directly or via other MOH-operated hospitals.
Our results showed that antibiotics (16.8%) were the most common drug classes associated with interventions, which goes hand on hand with previous studies (Wang et al., 2021, Faqeer et al., 2021, Babelghaith et al., 2020, Hajjar et al., 2021). This was followed by electrolytes/minerals (11.7%) and vitamins (9.4%).
By looking at the complications that COVID-19 patients developed during ICU admission, respiratory complications were found to be the most prominent (26%) among which pneumonia, tachypnea, ARDS, hypoxia, and metabolic acidosis which were more frequent, followed by the cardiovascular complications (25.5%), which were mainly hypotension, septic shock and bradycardia/tachycardia. These results are in agreement with Hajjar et al study that was focused on the intensive care management of COVID-19 patients (Hajjar et al., 2021). Finally, and unexpectedly, when BMI was compared between the survived and deceased patients, there was no significant difference between the two groups.
5. Conclusion
Our findings highlight that pharmacist’s attention should be amplified towards errors in dosing regimens and drug duplications throughout caring of critically ill COVID-19 patients. In addition, with medication shortage that potentially occur during the pandemic, pharmacist as a medication expert should be proactive in providing information about drugs and their alternatives, if necessary, for healthcare providers. Studies focused on significance of pharmacists’ interventions on health outcomes of critically ill COVID-19 patients and their acceptance by physicians should be conducted to follow up these findings.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgment
The authors extend their appreciation to the Deputyship for Research & Innovation, "Ministry of Education" in Saudi Arabia for funding this research work through the project no. (IFKSURG-2020-148).
Funding
This study is funded by Deputyship for Research & Innovation, "Ministry of Education" in Saudi Arabia through the project no. (IFKSURG-2020-148).
Authors’ contributions
Conception and design: AW, AR, SO, and SA; Data collection, analysis, and interpretation: AW, AR, SO, SA and SW; Writing the manuscript: AW, AR, SO, SA, SW and SB. All authors reviewed the manuscript.
Footnotes
Peer review under responsibility of King Saud University.
Contributor Information
Abdulrahman Alwhaibi, Email: aalwhaibi@ksu.edu.sa.
Abdulmohsin Alrwaished, Email: alrwaisheda@pmah.med.sa.
Sawsan Alawwad, Email: salawwad@kfmc.med.sa.
Syed Wajid, Email: wali@ksu.edu.sa.
Salmeen Bablghaith, Email: sbabelghaith@ksu.edu.sa.
Sultan Alghadeer, Email: salghadeer@ksu.edu.sa.
Mohammed N Al Arifi, Email: malarifi@ksu.edu.sa.
References
- Abunahlah N., Elawaisi A., Velibeyoglu F.M., Sancar M. Drug related problems identified by clinical pharmacist at the Internal Medicine Ward in Turkey. Int. J. Clin. Pharm. 2018;40(2):360–367. doi: 10.1007/s11096-017-0585-5. Epub 2018 Jan 29 PMID: 29380236. [DOI] [PubMed] [Google Scholar]
- Alderman C.P., Farmer C. A brief analysis of clinical pharmacy interventions undertaken in an Australian teaching hospital. J. Quality Clin. Practice. 2001;21(4):99–103. doi: 10.1046/j.1440-1762.2001.00428.x. [DOI] [PubMed] [Google Scholar]
- Al-Jazairi A.S., Al-Agil A.A., Asiri Y.A., Al-Kholi T.A., Akhras N.S., Horanieh B.K. The impact of clinical pharmacist in a cardiac-surgery intensive care unit. Saudi Med. J. 2008;29(2):277–281. PMID: 18246241. [PubMed] [Google Scholar]
- Aljbouri T.M., Alkhawaldeh M.S., Abu-Rumman A.E.K., Hasan T.A., Khattar H.M., Abu-Oliem A.S. Impact of clinical pharmacist on cost of drug therapy in the ICU. Saudi Pharm. J. 2013;21(4):371–374. doi: 10.1016/j.jsps.2012.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson, J.G., Abrahamson, K., 2017. Your Health Care May Kill You: Medical Errors. InITCH 2017 Jan 1, pp. 13–17. [PubMed]
- Babelghaith S.D., Wajid S., Alrabiah Z., Othiq M.A.M., Alghadeer S., Alhossan A., Al-Arifi M., Attafi I.M. Drug-related problems and pharmacist intervention at a general hospital in the Jazan Region, Saudi Arabia. Risk Manag. Healthc. Policy. 2020;6(13):373–378. doi: 10.2147/RMHP.S247686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cullen D.J., Sweitzer B.J., Bates D.W., Burdick E., Edmondson A., Leape L.L. Preventable adverse drug events in hospitalized patients: a comparative study of intensive care and general care units. Crit. Care Med. 1997;25(8):1289–1297. doi: 10.1097/00003246-199708000-00014. PMID: 9267940. [DOI] [PubMed] [Google Scholar]
- Delpeuch A., Leveque D., Gourieux B., Herbrecht R. Impact of clinical pharmacy services in a hematology/oncology inpatient setting. Anticancer Res. 2015 Jan;35(1):457–460. PMID: 25550587. [PubMed] [Google Scholar]
- Dhahri A.A., Arain S.Y., Memon A.M., Rao A., Mian M.A., Khan M.M., Hafeez G., Dhahri M.A., Mustafa F.G., Malhi ShewaRam, Iqbal M.H., Ahmad R., Aziz I., Arain A.S., Nankani D., Hussain M.W., Kausar M.A., Saqlain M., Chawla S., Azhar H., Haneef H., Arain H.S., Arain S.F., Shahid M.S., Iqbal S., Mughal M., Awan S.A., Mehbub H., Qiam F., Abro J.G., Khattak T., Bhatti D.S., Choudhary A.M., Khan A.F.A., Baqai S., Afzal F., Dhahri S.A., Dhahri P.A., Ghufran S., Umbrin I., Shehdio W., Shaikh M., Dhahri M., Memon M., Yousufzai Y., Kumar J., Ilyas M., Chaudhary T., Nawaz S., Bilal H., Faraz N., Chawla R., Shaikh S. The psychological impact of COVID-19 on medical education of final year students in Pakistan: a cross-sectional study. Ann. Med. Surgery. 2020;60:445–450. doi: 10.1016/j.amsu.2020.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dooley M.J., Allen K.M., Doecke C.J., Galbraith K.J., Taylor G.R., Bright J., Carey D.L. A prospective multicentre study of pharmacist initiated changes to drug therapy and patient management in acute care government funded hospitals. British J. Clin. Pharmacol. 2004;57(4):513–521. doi: 10.1046/j.1365-2125.2003.02029.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ernst F.R., Grizzle A.J. Drug-related morbidity and mortality: updating the cost-of-illness model. J. Am. Pharm. Assoc. 2001;41(2):192–199. doi: 10.1016/s1086-5802(16)31229-3. [DOI] [PubMed] [Google Scholar]
- Faqeer N., Mustafa N., Abd Al-Jalil N., Quran T. Impact of clinical pharmacists in an inpatient medical oncology service: A prospective study at a comprehensive cancer center in Jordan. J. Oncol. Pharm. Pract. 2020 doi: 10.1177/1078155220943277. 1078155220943277. Epub ahead of print. PMID: 32703083. [DOI] [PubMed] [Google Scholar]
- Hajjar L.A., Costa I.B.S.D.S., Rizk S.I., Biselli B., Gomes B.R., Bittar C.S., De Oliveira G.Q., De Almeida J.P., De Oliveira Bello M.V., Garzillo C., Leme A.C., Elena M., Val F., De Almeida Lopes M., Lacerda M.V.G., Ramires J.A.F., Kalil Filho R., Teboul J.L., Landoni G. Intensive care management of patients with COVID-19: a practical approach. Ann. Intensive Care. 2021;11(1):36. doi: 10.1186/s13613-021-00820-w. PMID: 33604873; PMCID: PMC7891474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane S.L., Weber R.J., Dasta J.F. The impact of critical care pharmacists on enhancing patient outcomes. Intensive Care Med. 2003;29(5):691–698. doi: 10.1007/s00134-003-1705-3. Epub 2003 Mar 29 PMID: 12665997. [DOI] [PubMed] [Google Scholar]
- Klopotowska J.E., Kuiper R., van Kan H.J., de Pont A.C., Dijkgraaf M.G., Lie-A-Huen L., Vroom M.B., Smorenburg S.M. On-ward participation of a hospital pharmacist in a Dutch intensive care unit reduces prescribing errors and related patient harm: an intervention study. Critical Care. 2010;14(5):1. doi: 10.1186/cc9278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Louiselle K., Elson E.C., Oschman A., Duehlmeyer S. Impact of COVID-19 pandemic on pharmacy learners and preceptors. Am. J. Health-System Pharm. 2020;77(14):1097–1099. doi: 10.1093/ajhp/zxaa127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacLaren R., Devlin J.W. The bedside critical care pharmacist: a mandatory ICU team member essential for patient care. Critical Care Med. 2019;47(9):1276–1278. doi: 10.1097/CCM.0000000000003888. [DOI] [PubMed] [Google Scholar]
- MacLaren R., Roberts R.J., Dzierba A.L., Buckley M., Lat I., Lam S.W. Characterizing critical care pharmacy services across the United States. Critical Care Explor. 2021;3(1) doi: 10.1097/CCE.0000000000000323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makary M.A., Daniel M. Medical error—the third leading cause of death in the US. Bmj. 2016;3:353. doi: 10.1136/bmj.i2139. [DOI] [PubMed] [Google Scholar]
- Meng L., Qiu F., Sun S. Providing pharmacy services at cabin hospitals at the coronavirus epicenter in China. Int. J. Clin. Pharm. 2020;42(2):305–308. doi: 10.1007/s11096-020-01020-5. Epub 2020 Apr 2. PMID: 32240484; PMCID: PMC7113541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molino Cde G., Carnevale R.C., Rodrigues A.T., Visacri M.B., Moriel P., Mazzola P.G. Impact of pharmacist interventions on drug-related problems and laboratory markers in outpatients with human immunodeficiency virus infection. Ther. Clin. Risk Manag. 2014;7(10):631–639. doi: 10.2147/TCRM.S61821. PMID: 25120369; PMCID: PMC4130328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mongaret C., Quillet P., Vo T.H., Aubert L., Fourgeaud M., Michelet-Huot E., Bonnet M., Bedouch P., Slimano F., Gangloff S.C., Drame M. Predictive factors for clinically significant pharmacist interventions at hospital admission. Medicine. 2018;97(9) doi: 10.1097/MD.0000000000009865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montazeri Mitra, Cook Deborah J. Impact of a clinical pharmacist in a multidisciplinary intensive care unit. Critical Care Med. 1994;22(6):1044–1048. doi: 10.1097/00003246-199406000-00027. [DOI] [PubMed] [Google Scholar]
- Moukafih B., Abahssain H., Mrabti H., Errihani H., Rahali Y., Taoufik J., Chaibi A. Impact of clinical pharmacy services in a hematology/oncology ward in Morocco. J Oncol Pharm Pract. 2021;27(2):305–311. doi: 10.1177/1078155220919169. Epub 2020 Apr 23 PMID: 32326873. [DOI] [PubMed] [Google Scholar]
- Moyen E., Camiré E., Stelfox H.T. Clinical review: medication errors in critical care. Critical Care. 2008;12(2):1–7. doi: 10.1186/cc6813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ong S.W., Tan Y.K., Chia P.Y., Lee T.H., Ng O.T., Wong M.S., Marimuthu K. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. Jama. 2020;323(16):1610–1612. doi: 10.1001/jama.2020.3227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips J., Beam S., Brinker A., Holquist C., Honig P., Lee L.Y., Pamer C. Retrospective analysis of mortalities associated with medication errors. Am. J. Health-System Pharm. 2001;58(19):1835–1841. doi: 10.1093/ajhp/58.19.1835. [DOI] [PubMed] [Google Scholar]
- Phillips D.P., Christenfeld N., Glynn L.M. Increase in US medication-error deaths between 1983 and 1993. The Lancet. 1998;351(9103):643–644. doi: 10.1016/S0140-6736(98)24009-8. [DOI] [PubMed] [Google Scholar]
- Preslaski C.R., Lat I., MacLaren R., Poston J. Pharmacist contributions as members of the multidisciplinary ICU team. Chest. 2013;144(5):1687–1695. doi: 10.1378/chest.12-1615. [DOI] [PubMed] [Google Scholar]
- Tan S.L., Zhang B.K., Xu P. Chinese pharmacists' rapid response to the COVID-19 outbreak. Am. J. Health Syst. Pharm. 2020;77(14):1096–1097. doi: 10.1093/ajhp/zxaa120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang B., Bragazzi N.L., Li Q., Tang S., Xiao Y., Wu J. An updated estimation of the risk of transmission of the novel coronavirus (2019-nCov) Infectious Disease Modell. 2020;1(5):248–255. doi: 10.1016/j.idm.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang R., Kong L., Xu Q., Yang P., Wang X., Chen N., Li L., Jiang S., Lu X. On-ward participation of clinical pharmacists in a Chinese intensive care unit for patients with COVID-19: a retrospective, observational study. Res. Social Adm. Pharm. 2021;17(1):1853–1858. doi: 10.1016/j.sapharm.2020.06.005. Epub 2020 Jun 6. PMID: 33317764; PMCID: PMC7832950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization, 2020. Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected: interim guidance, 13 March 2020. World Health Organization.
- World Health Organization. WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020. Available at https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (last accessed on May 10, 2021).
- Zuckerman A.D., Patel P.C., Sullivan M., Potts A., Knostman M., Humphreys E., O'Neal M., Bryant A., Torr D.K., Lobo B., Peek G., Kelley T., Manfred J., Tomichek J., Crothers G., Catlin R., Brumagin H.E., Hughes L., Hayman J. From natural disaster to pandemic: a health-system pharmacy rises to the challenge. Am. J. Health Syst. Pharm. 2020;77(23):1986–1993. doi: 10.1093/ajhp/zxaa180. Epub ahead of print. PMID: 32417878; PMCID: PMC7239216. [DOI] [PMC free article] [PubMed] [Google Scholar]