Abstract
Both autogenous and alloplastic material have been used in management of temporomandibular joint (TMJ) ankylosis. Second surgical site, donor site morbidity, possibility of over/undergrowth, graft fracture or resorption and increased surgical time are the disadvantages of autogenous graft. Alloplastic total joint replacement (TJR) has become a promising technique in management of adult temporomandibular joint ankylosis (TMJA). This paper intends to present the role of alloplastic TJR in management of TMJA. There is significant current evidence of the role of alloplastic TJR in the management of TMJA. Results in TMJA are excellent with sustained improvement in pain free mouth opening, correction of facial asymmetry, reduction in recurrence and improved quality of life. TMJ TJR is becoming the gold standard of care in the management of TMJA, although costs can sometime preclude access to this mode of therapy.
Keywords: Temporomandibular joint ankylosis, Total joint replacement, Re-ankylosis, Alloplasts
1. Introduction
Temporomandibular joint ankylosis (TMJA) can lead to minimal or nil mouth opening,1 problems in mastication, speech, aesthetics and airway. Physical, psychological, social well-being and quality of life is affected in TMJA patients.2 There is a plethora of procedures explained in literature for the management of TMJA. These range from simple osteoarthrectomy to complex reconstruction procedures. Perpetual failure rates with re-ankylosis and inability to maintain long term mouth opening, has been a challenge in management of TMJA. TMJA can affect both children and adults. Trauma has been reported as most common etiology for TMJA.3, 4, 5 The problem in many developing countries is lack of adequate access to healthcare or unavailability of surgical expertise in poorly developed area, illiteracy that precludes patients to seek treatment when the ankylosis ensues or fear of pain leading to consequent prolonged non-functional joint which can lead to ankylosis.5 Reports from published literature show that patients seek treatment for ankylosis anywhere between immediate to many years after.4 This has major significance, as the ankylosis if developed during the childhood cause severe mandibular growth retardation. If, one joint is affected in childhood, it can lead to facial asymmetry. Involvement of both the joints can lead to marked mandibular undergrowth and subsequent obstructive sleep apnea (OSA) secondary to bilateral growth centre arrest.
The alternative managements of TMJA are discussed elsewhere in this issue. Reconstruction of temporomandibular joint (TMJ) can be performed by autogenous as well as alloplastic material, both having advantages and disadvantages. Second surgical site, donor site morbidity, possibility of over/undergrowth, graft fracture or resorption and increased surgical time are disadvantages of autogenous grafts. Whilst alloplastic TJR have been used in the management of trauma, degenerative disease and for multiple failed surgeries, its use in ankylosis surgery has become increasingly indicated.
The goals of management in surgery are resection, reconstruction and rehabilitation and this similarly applies to TMJA. The goals of TMJ reconstruction are to; provide pain-free, adequate maximal incisal opening (MIO), prevent re-ankylosis, achieve satisfactory occlusion, maintain ramal height, maintain adequate facial symmetry, improve OSA if any, and to improve overall quality of life of patients. In children along with these there is an added need for maintenance of catch-up of growth.
Modern orthopaedic surgery would be unthinkable without the utilisation of alloplastic replacement. The TMJ is a joint like any other and there is ample evidence of the success of alloplastic replacement over the last 25 years to justify its routine use for ankylosis reconstruction and rehabilitation whilst preventing recurrence and restoring facial form and function and improving quality of life.6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27 With the available evidence and distinct advantages of TMJR, it appears to have become the gold standard of care specially in adults. Management of TMJA with TJR can be done using stock or custom joints. Custom joints can adapt easily and are made for available bone with its contours. The stock joint is cost-effective with less turnaround time but the bone has to be prepared to adapt to joint. This paper will provide a brief about history, presurgical consideration, advantages and disadvantages, preoperative planning, surgical technique and discussion on TMJR.
1.1. Historical consideration
Christensen designed the first of the modern prostheses in 1965.
This device has two components, a ramal/condylar component which articulates with a metal fossa. The condylar head component was made up of polymethylmethacrylate (PMMA) with cast vitallium ramal component fitting into it as a post and extending down the lateral ramus. The condylar head was changed to metal leading to a metal on metal articulation in the late 90s with disastrous consequences. According to Sidebottom et al. the issues with the metal on metal was early metal wear debris causing a lymphocyte type rejection and foreign body response.28 TMJ Concepts prosthesis commenced clinical trials in the early 90s and was approved in 99. The Biomet (formerly Lorenz) prosthesis started at a similar time. Unfortunately only the Biomet stock is FDA approved with the TMJC being the only custom prosthesis FDA approved. The Biomet stock prosthesis has 3 fossa baseplate sizes and 5 different ramus components and also an offset ramus variant in all 5 sizes. The fossa itself is the same size and shape to match the condylar head.
PRE-SURGICAL CONSIDERATION- One stage/two stage and stock/custom made prosthesis.
One stage or two stage approaches can be used for the replacement of TMJ with TMJ TJR. One stage approach is more acceptable to the patient as it reduces the number of hospital admissions, cumulative operative and anesthetic risk. One stage approach is straight forward and avoids nerve injury compared to two stage approach. One stage approach has been used by Haq et al.,29 Gerbino et al.12 and Brown et al.30 with successful outcome. Two stage approach however has the advantage of confirming successful arthroplasty with no heterotopic bone formation. This also allows for orthodontic preparation for concomitant TMJ TJR and orthognathic surgery. In two-stage protocol, in first stage osteoarthrectomy can be performed with or without distraction osteogenesis (specially in case of bilateral TMJA patients) or interposition of medical grade silastic as spacer. In literature, two-stage total prosthetic reconstruction of TMJ has been performed in severe and recurrent ankylosis by Egemen et al.31
The manufacture of the custom made prosthesis requires a significant amount of planning with the technical team, however this significantly saves intraoperative bone adjustments to get a non-custom joint to fit the patient. Wolford et al. compared the amount of MIO after stock and custom made prosthesis. MIO increased from 27.4 to 30.1 mm and from 27.4 to 37.3 mm postoperatively for stock and custom made prosthesis respectively.32 Both type of prosthesis provides adequate MIO. If, ankylosis has occurred after growth completion then stock joint is appropriate. Because after growth completion, ramal height is maintained and warping of mandible is seldom present. If the ankylosis is before growth completion then custom joint is appropriate as the ramus shows decreased height and warping.33 After deciding about one stage/two stage and stock/custom made prosthesis, preoperative planning should be followed.
1.2. Preoperative planning
Preoperative computed tomography (CT) should have interslice thickness of 1 mm. The CT should not be older than 3 months. Import the CT DICOM (Digital Imaging and Communications in Medicine) data of the patient into Mimics Materialize 22.0 (Belgium) and the dimensions of ankylotic mass can be measured and 3D reconstruction of skull base can be done. Superior cut should be parallel to Frankfort Horizontal (FH) plane such that a minimum of 8 mm thick bone stock is available from skull base. Measure total ramal length available for prostheses placement (superior cut to gonion), which should be followed by virtual gap creation of 1.5–2 cm. Fossa component should be almost parallel to FH plane with the posterior wing kept at a distance such that it is not encroaching the external auditory canal. In case of stock prosthesis, previously scanned and saved stereo lithography (STL) files of standard Zimmer Biomet® mandibular prosthesis 45, 50, 55 mm and fossa component including small, medium, large size should be imported to assess for a virtual fit and feasibility of the stock TMJ TJR. The imported STL file of the mandibular component should be virtually implanted such that it is parallel to posterior border of ramus; in maximum contact with ramus of mandible and at least five fixation screws not violating the neurovascular bundle. The virtual image can be rotated and viewed from all angles to see for superior-inferior, medio-lateral fit. The areas, which would require intraoperative lateral ramus surface reshaping should be noted. The criteria for fit should be checked from all angles.
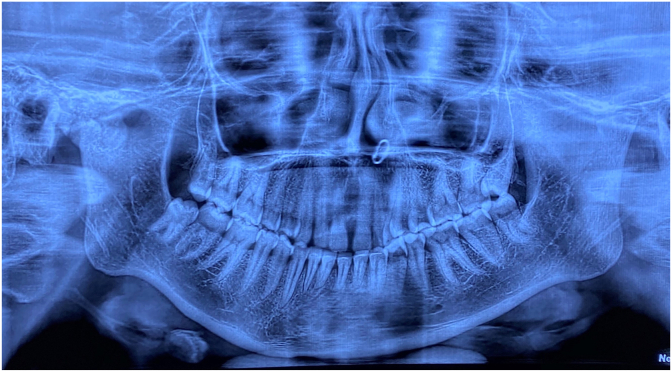
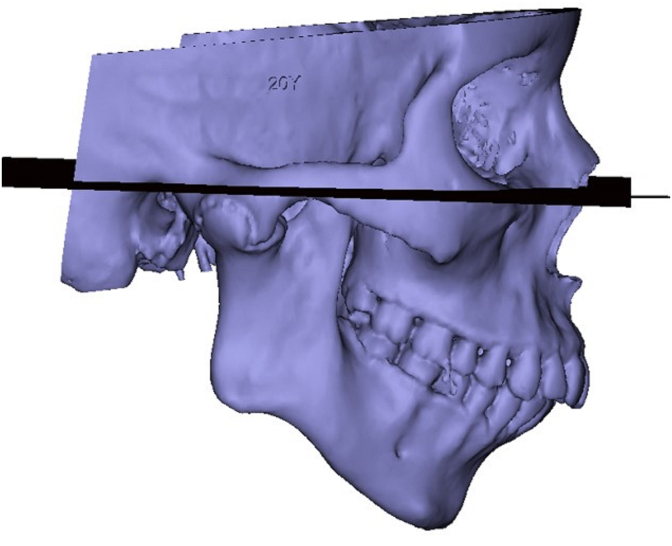
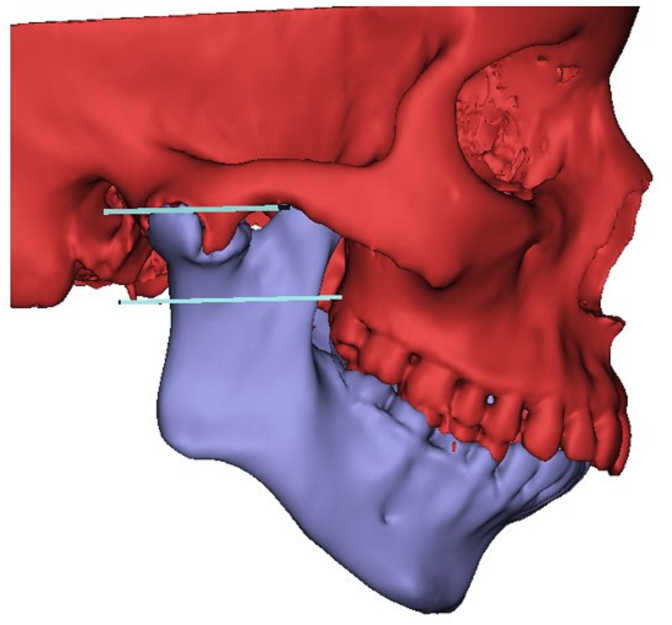
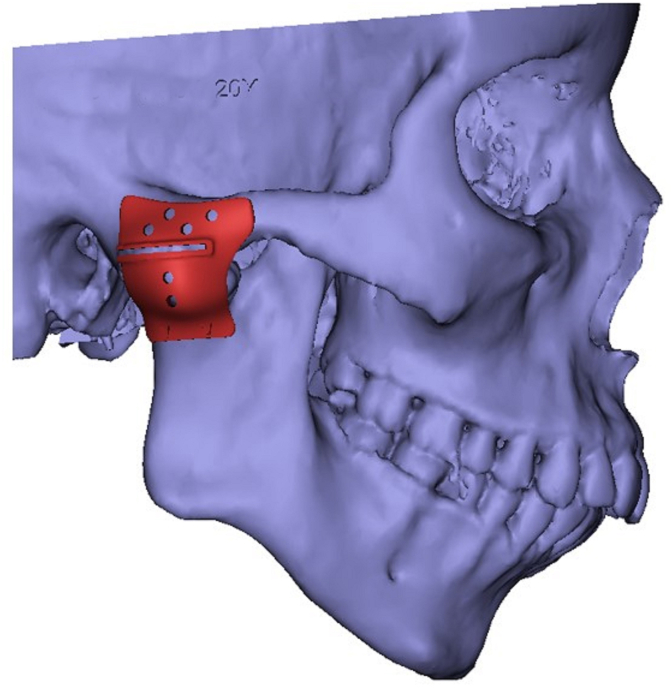
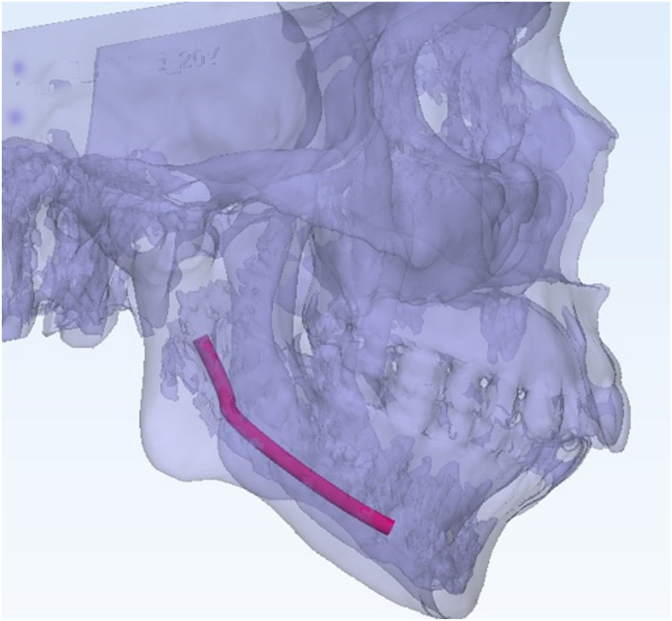
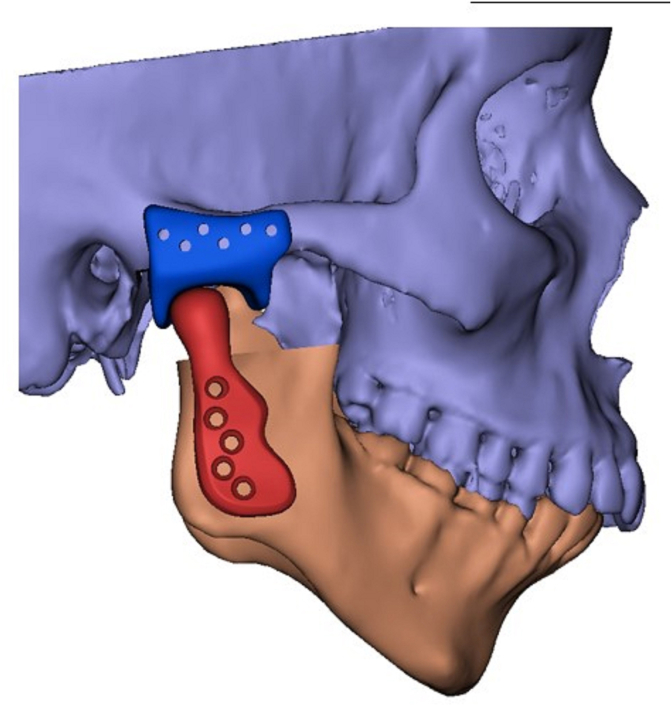
For custom made prosthesis, time taken for fabrication of custom implants is compensated by a quick fit in intraoperative time. Custom devices are made to fit the patient's mandible and fossa. For planning of custom devices, the workflow starts from preoperative virtual planning of the surgical procedure. A complete case of custom total joint replacement is shown (Fig. 1, Fig. 2, Fig. 3, Fig. 4, Fig. 5, Fig. 6, Fig. 7A, Fig. 7B, Fig. 8, Fig. 9, Fig. 10, Fig. 11, Fig. 12, Fig. 13). Preoperative maximal incisal opening (Fig. 1) and orthopantomogram showing right TMJA with morphological changes in left side (Fig. 2). For preoperative virtual surgical planning, the DICOM of CT data fed into the Mimics materialize 22.0 (Belgium) software. After segmentation, Frankfort-horizontal plane should be drawn (Fig. 3). Superior and inferior osteotomy cut are planned and cut are placed virtually (Fig. 4). During planning of superior osteotomy, the osteotomy should be parallel to FH plane away from auditory canal with at-least 8 mm of bone should be present at skull base. During inferior osteotomy, inferior alveolar canal and neurovascular bundle should be preserved. The inferior osteotomy cut should be below the level of ankylotic mass. With both stock and custom alloplasts, we can lengthen the ramus by releasing the pterygomasseteric sling thus widening the gap generated and reducing the need for excessive resection of the pre-existing ramus. This technique has a disadvantage of creating ipsilateral open bite and relying on subsequent eruption of teeth to close the open bite.
Fig. 1.
Preoperative maximal incisal opening in a case of right temporomandibular joint ankylosis.
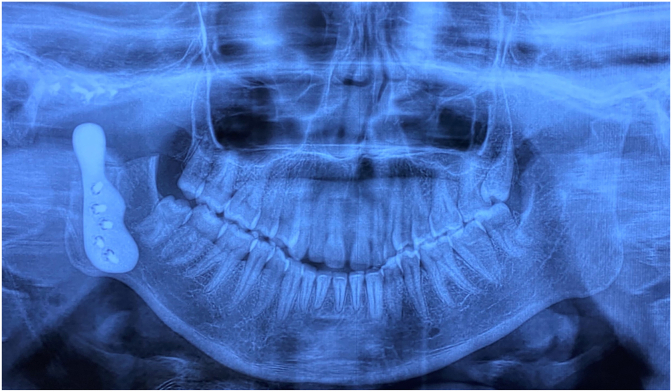
Fig. 2.
Orthopantomogram showing right side temporomandibular joint ankylosis with morphological changes in left side.
Fig. 3.
Segmentation of CT data and drawing Frankfort horizontal plane.
Fig. 4.
Superior and inferior osteotomy, superior osteotomy parallel to Frankfort-horizontal plane.
Fig. 5.
Cutting guide for superior and inferior osteotomy, superior horizontal slot for superior osteotomy and inferior horizontal part for inferior osteotomy.
Fig. 6.
Nerve mapping to preserve neurovascular bundle.
Fig. 7A.
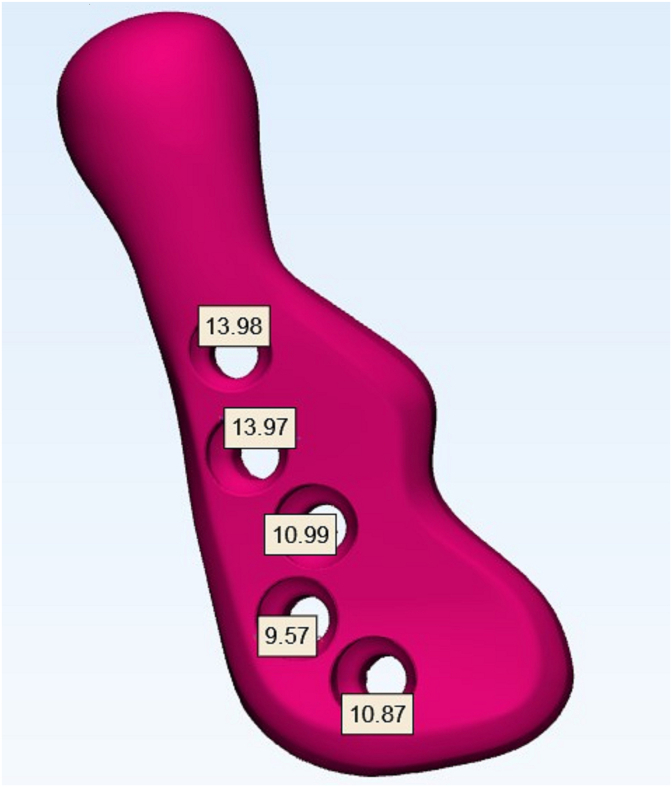
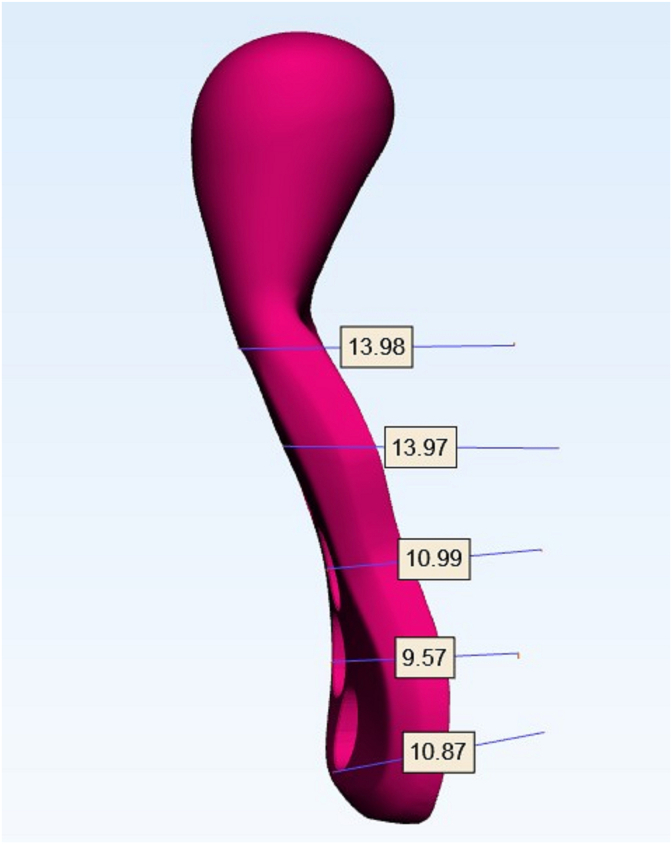
Screw hole positioning to avoid injury to inferior alveolar neurovascular bundle.
Fig. 7B.
screw mapping to know the length of the screw required.
Fig. 8.
The check of fit and accuracy of fossa and mandibular component on the 3D virtual model. (This can be rotated 360° to check fit accuracy).
Fig. 9.
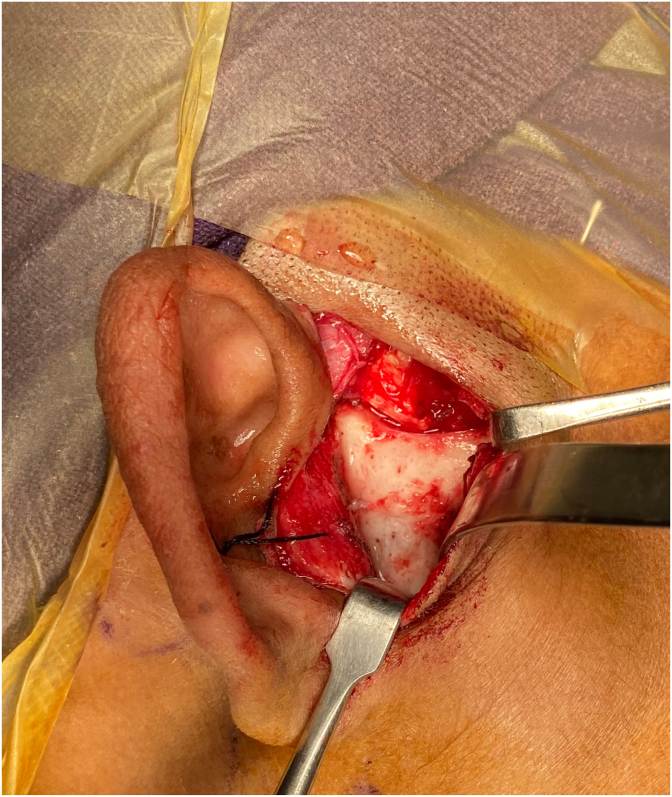
Endaural incision for osteoarthrectomy.
Fig. 10.
Retromandibular incision to expose ramus and for placing ramal component.
Fig. 11.
Position of condylar component in posterior most position in fossa.
Fig. 12.
Follow-up orthopantomogram showing TJR components in situ.
Fig. 13.
Follow-up mouth opening (32 mm).
As the fossa and mandibular component are fabricated after virtual surgery, it is important to transfer exact osteotomy cut in intraoperative time period. Cutting guides or positioning guides have been used in literature which help to transfer virtual planning to operating room, more accurately and precisely.12,29,30,34, 35, 36, 37, 38, 39, 40, 41 A surgical guide for fossa is very important and mandatory for accurate cutting in TMJA patients. Most of the cutting guides used in literature are with predrilled holes (Fig. 5). The holes in cutting guide should coincide with final fossa position. These guides also help in predrilling of fixation holes in the mandible to minimize errors in final prostheses positioning. A horizontal slot for superior osteotomy and a lower-end of the cutting guide corresponds to the inferior cut (Fig. 5). The cutting guide are 3D printed by selective laser melting in titanium alloy. Its precise adaptability should be ensured on stereolithographic model (Fig. 5). A cutting guide will help to safely perform the osteotomy according to the plan and will help to save important vital structures. Guides have been used for both custom-fitted and stock joint. The cutting guide allow the subcondylar bone-cut to be performed according to the exact shape and size of the planned prostheses. Xu et al. used surgical guide only for the ramus component which is useful for the inset of the stock prostheses.36
When planning of joint, screw hole should be away from inferior alveolar canal. To avoid this nerve mapping should be done (Fig. 6). Finite element analysis should be performed in every case to know the area of stress and strain. Screw mapping is important (to know the required length of the screw at each position and to avoid injury to neurovascular bundle) (Fig. 7A, Fig. 7B). Fit of the implant should be evaluated on the virtual 3-D model (Fig. 8). After checking accuracy of implant the metal joint should be printed with screw mapping. Fossa and screws are fabricated by CNC. The implants are sterilized and packed aseptically.
1.3. Surgical technique
Classical preauricular, endaural incision with or without extended temporal surgical incision is used for osteoarthrectomy and fossa component fit. Endaural incision can provide improved cosmesis (Fig. 9). Retromandibular/Submandibular incision is used to expose the lateral ramus for the fixation of mandibular component (Fig. 10). For osteoarthrectomy, piezoelectric saw should be used as it results in a flat temporal surface where the fossa can be fitted without much reshaping to reduce the rocking and use of piezo help to reduce chances of re-ankylosis.42 Osteoarthrectomy should be performed perpendicular to cortical bone. The superior and inferior cut should be parallel and medial tapering of cut should be avoided and all edges of osteotomy should be rounded. There is often a need to do coronoidectomy due to forward positioning of the coronoid causing impingement on the posterior maxilla and restricting mouth opening. Ipsilateral coronoidectomy should be performed if passive MIO after osteoarthrectomy is < 30 mm. Contralateral coronoidectomy should be performed only if the passive mouth opening of <30 mm after ipsilateral coronoidectomy as per Kaban's protocol.43 For stable fossa placement, tripod stability is must. The fossa component should be parallel to FH plane. The anterior portion should be slightly inferior to the posterior to avoid anterior dislocation of prosthesis. Fossa should be secured with 2.0 mm screw at zygomatic bone and at least 3, preferably 4 bicortical screws should be used. The head of the condyle should be posterior in fossa so that some amount of pseudotranslation can happen (Fig. 11). Also, anterior positioning of condyle in fossa can lead to anterior dislocation of condyle during mouth opening. In case of too lateral position of condyle in fossa, we can reshape bone from superior edge of ramus to allow a central-medial position of condyle, although this may be due to inadequate resection of ramal height. In case of more medial position of condyle, offset ramal component should be used to position condyle in a central-lateral position. The lateral surface of the ramus however requires reshaping, as a long-standing ankylosis sometimes causes warping of the lateral ramus. Care should be exercised to have best possible fit of ramus component after reshaping the lateral ramus. The ramus component requires fixation with at least 5 bicortical screws, the most important being the most proximal screw adjacent to the ramal osteotomy. Standard precautions should be taken for reduction of periprosthetic joint infection (PJI) (Table 1). Fat grafting should be performed by mobilizing the nearby available buccal fat pad or free abdominal fat. All the patients should follow a rigorous postoperative mouth opening exercise protocol. All the patients should be followed up preferably for periods more than 5 years for MIO and yearly radiographs to monitor any signs of re-ankylosis and condition of implants (Fig. 12, Fig. 13). Simultaneous orthognathic surgery can be done, if required. This however requires additional planning. The fabrication of splint is not possible due to closed mouth. Splint-less orthognathic surgery with 3D printed plates is performed when single stage concomitant TJR and orthognathic correction is planned.
Table 1.
Preventive measures to control periprosthetic joint infection (PJI).4
| Serial number | Preventive measures for PJI |
|---|---|
| 1 | Ceftriaxone 1g + 600 mg clindamycin 1 h before procedure |
| 2 | Vancomycin-soaked gauze in ear |
| 3 | Isolation of eyes, mouth and nares (apply Tegaderm) |
| 4 | Meticulous iodine preparation of oral cavity, if concomitant TJR and orthognathic surgery is planned |
| 5 | Surgeons scrub changed every time the intraoral/extraoral area approached |
| 6 | Soaking of implants in antibiotic solution |
Abbreviation: PJI- periprosthetic joint infection; TJR-total joint replacement.
2. Discussion
Alloplastic TMJ TJR is now considered as definitive treatment protocol in adult TMJA. Reports are available for the use of TJR in TMJA patients over 20 years. The major advantage of alloplastic TJR is its resemblance to TMJ anatomy. TMJ TJR provides biomechanical rather than biological solution for TMJ reconstruction.44 Wolford and Mercuri in 2014 used alloplastic TJR in 56 patients and reported no failure.45 It allows immediate physiotherapy and markedly reduced chances of recurrence. Complications of second surgical site can be avoided as in case of autogenous graft. In a review article, CCG and alloplastic TJR have been compared and alloplastic total joint replacement was considered more effective than CCG.46 On contrary to this, Dimitroulis has suggested the use of total TMJ prosthesis in re-ankylosis cases only.47
Autogenous grafts in patients with multiple surgical procedure have reported with poorer outcome compared with fresh cases. Multiple surgical procedure lead to formation of scar tissue, loss of surgical plane and reduced or interrupted blood supply. These changes can lead to degradation of bony and soft tissue around the joints. Marx reported that capillaries can penetrate a maximum thickness of 180–220 μm, whereas Mercuri reported that the average thickness of scar tissue around TMJ is 440 μm in multiply operated cases.48 This may be the reason for failure of autogenous graft in multiply operated cases. Adequate mouth opening is important outcome factor after TMJ replacement. Roychoudhury, Sidebottom, Wolford and Mercuri et al. reported adequate mouth opening after use of alloplastic joint replacement in TMJA patients.4,13,19,23,32,45
In orthopaedic literature, alloplastic joints have been used in skeletally immature patients. Outcome has been reported as successful in some small case series. Bessette et al. performed alloplastic TJR in 12 patients (16 hips) in skeletally immature patients and found satisfactory results in 67% joints even at follow-up of 13.6 years.49 Wroblewski et al. found excellent result in 28 patients (39 joints) at maximum follow-up of 34 years.50 With advancement in current diagnostic facility and improved equipment, instruments and planning, it may be worthwhile to extend the TJR in skeletally immature patients. The concern of growth of mandible in such patients remains a challenge. The use of alloplastic TJR may hamper the growth of mandible in growing patients, this may require revision surgery in future. Mercuri and Swift used alloplastic TJR in a TMJA in a growing patient and demonstrated successful outcome in terms of mandibular range of motion and occlusion without any sign of recurrence after a follow-up of 5.5 year.51 Keyser et al. in 2020 in a pilot survey concluded that TMJ TJR can be a useful modality in skeletally immature patients.52 Sidebottom et al. reviewed both autogenous tissue and alloplastic TMJR. The author referred the use of TJR in children specially in cases where autogenous tissue has previously failed.53 Form follows function theory by Moss states that soft tissue controls the growth of bone.54 Interplay between soft tissue and bone regulates growth. This theory may explain the continued growth seen in pediatric patients with TMJ TJR. Further evidence with large sample size and longer follow-up is necessary for definitive answer to the use of alloplastic TMJ TJR in pediatric patients.
In patients, where ankylosis develop prior to growth cessation, facial asymmetry with or without cant (unilateral involvement) will be present depending on duration of ankylosis and in case of involvement of both the joints, marked mandibular undergrowth and subsequent OSA may be present secondary to bilateral growth centre arrest. In these patient, correction of facial asymmetry and OSA are the additional goals to achieve. Ramus-condyle unit reconstruction should be the aim to correct pre-existing facial asymmetry and to improve OSA status or prevent worsening of OSA. In cases where ankylosis has ensued before the growth cessation and if the ankylosis is long-standing, there are chances of warping and shortening of vertical ramus. Thus, making the fit feasibility and ideal positioning of stock joint questionable. In a long-standing bilateral ankylosis, which would require a large amount of advancement and counter-clockwise movement of mandible for correction of retrognathia and possible OSA, use of stock joint may not be feasible due to the ramal bowing and the length of the stock prosthesis being too long for the ramus.33 In both such situations, it is advisable to use custom-fitted joint.
TJR also allows the fulfilment of another goal of TMJA management in form of facial deformity correction as it allows concomitant orthognathic surgery. In patients with minimal maxillomandibular deformity, alloplastic TJR can be a major indication as we can perform concomitant orthognathic procedure.4,55 This can be done as single stage or two stage procedure. Facial deformity with TMJA can be treated in a single stage allowing significant decrease in treatment time and better outcome.4 The two-stage TMJ-TJR and orthognathic surgery allows time for presurgical orthodontics and confirmation of no heterotopic bone formation after osteoarthrectomy. More technical and surgical expertise is required for concomitant orthognathic surgery and TJR. When planning the concomitant maxillary surgery and alloplastic TMJ replacement the mandibular position should be determined first as the prosthesis cannot be adjusted to fit with the maxilla once that is moved, whereas minor adjustments of the maxilla is possible once the prosthesis is in situ.
Recurrence of TMJA is one of the most devasting outcome. In literature, heterotopic bone formation has been reported in 50% of cases.56 Autogenous fat graft either pedicled buccal fat pad or abdominal fat pad have been used around the reconstructed joint. The autogenous fat helps in reduction of heterotopic bone formation. Wolford et al. and Mercuri et al. have stated that abdominal fat pad around the joints helps to prevent postoperative incidence of fibrosis around joints and ultimately heterotopic/reactive bone formation.19,57,58 Wolford observed that patients with fat packing around the joints have better outcome than patients without fat packing. Buccal fat pad has been used with equal success rate. Roychoudhury et al. compared of buccal fat pad and abdominal fat pad with abdominal fat pad giving better results than buccal fat pad in TMJA patients. They have also reported the benefits of fat grafting in TJR for TMJA.59
The use of piezoelectric scalpel to reduces heterotopic bone formation after osteoarthrectomy was first reported in 2014.60 Other methods includes complete removal of ankylotic mass, aggressive physiotherapy, low dose radiation, nonsteroidal anti-inflammatory drugs61 (Indomethacin) and copious irrigation with saline to remove all the bone chips/slurry to prevent the impregnation of bone morphogenetic protein (BMP) in surrounding tissue. Roychoudhury et al., in 2020 demonstrated that the use of piezoelectric scalpel for complete removal of ankylotic mass, copious irrigation with saline to remove all the bone chips, fat grafting around joints and aggressive physiotherapy prevent heterotopic bone formation in alloplastic TJR.4 They used this protocol in 41 patient (54 joints) without any recurrence over 6 years.
Pain is common in patients with inflammatory TMJ disease but not in TMJA due to trauma or infection. Wolford et al. used TMJ concept prosthesis in 35 patients (65 joints) and observed reduction in pain in 89% of patients.62 Thereafter, TMJ concept was approved by FDA as total TJR prosthesis. Mercuri et al., in 2007 reported significant reduction in pain and improvement in mandibular function over a follow-up of 14 years.63
Hypersensitivity to the alloplastic prosthesis can occur. It is more in case of metal to metal prosthesis and less in case of metal on UHMWPE.63 Wear of component of knee and hip TJR have been observed in the orthopaedic literature. This wear of component limits its use in knee and hip joints and revision surgery may be required because of this potential complication.25 Functional load on TMJ is less than knee and hip joint. This decrease in functional load may be the possible reason for less wear of component of TMJ TJR. During alloplastic TJR, lateral pterygoid and temporalis muscle are dis-inserted from TMJ that further decreases the load on TMJ.63 Theoretically, there are less chances or wear and particulation after TMJ TJR. Mercuri has reported in his publications, no evidence of polymer particulation failure in histology of intra-articular tissue after alloplastic TJR. Westermark et al. observed that modern TMJ prosthesis (with condyle made up of Co–Cr–Mo and fossa made up of UHMWPE) function without foreign body reaction.26
Potential complications of TMJ surgery can be encountered in patients. These includes haemorrhage, dislocation of prosthesis in intraoperative and postoperative period, neurological alterations (mostly temporal and marginal mandibular nerve branches of facial nerve), scar or heterotopic bone formation resulting in failure of prosthesis, PJI, pain and implant failure. Significant pain problems can be encountered related to fibrosis, calcifications, cervical neuropathy, immunological problems to alloplastic material in multiply operated patients. PJI, if encountered is most difficult task to be manage in alloplastic TJR. PJIs have been reported in literature after use of alloplastic TJR.12,64 Roychoudhury et al. reported no case of PJI after use of 54 stock alloplastic TJR in TMJA patients using the protocol (Table 1).4
Although rare, dislocation of condyle has been reported in intraoperative and postoperative period.16,17 Dislocation is common after TJR specially in case of unilateral or bilateral coronoidectomy.4 This dislocation should be managed with reduction under general anaesthesia and light guiding elastics.4 Mercuri suggests that potential for posterior dislocation exists in the stock and custom metal-on-metal fossa as they do not have a posterior stop. There is a requirement of a perfect alignment of the head of condyle in the centre of the fossa to minimize dislocation. This is of a particular concern in the concomitant TJR- orthognathic surgery case.65 Mustafa and Sidebottom in their article in 2013 studied risk factor for intraoperative dislocation of the TJR and advised to try to dislocate the joint at the time of placement and if dislocation occurs then place the patient in light elastics for one week to prevent dislocation. Mustafa and Sidebottom revealed that there is increased risk of dislocation where coronoidectomy has been performed. Relocation in postoperative period can usually be simply achieved with a little sedation and analgesia which is easier than a normal joint dislocating.66 RHB Jones observed dislocation in 2 patients (out of 7).25
From the studies available in literature, it can be proposed that: Donor site morbidity can be avoided in alloplastic TMJ TJR; alloplastic prosthesis have better outcome than autogenous tissue; fat grafting around the TMJ can improve outcomes of mouth opening, improved jaw functions and required number of re-surgery; alloplastic TMJ TJR with fat grafting can be considered as definitive protocol for adult TMJA management; concomitant orthognathic surgery can be performed with TJR; osseointegration of fossa and ramal component can occur and it provides long term stability; reported improvement in maximal incisal opening, TMJ pain, jaw functions and quality of life.
3. Conclusion
The authors conclude that ample evidence, albeit only from large cohort studies, for the use of TJR with fat graft for successful management of TMJA not only in terms of maximal incisal opening but also other goals of TMJA management. The alloplastic TJR can provide adequate functional, aesthetic outcome and can improve quality of life in TMJA. Use of alloplastic TMJ TJR in skeletally immature patient require further research. With continuous advancements, these device can be more stable with long-term successful results.
References
- 1.el-Sheikh M.M., Medra A.M., Warda M.H. Bird face deformity secondary to bilateral temporomandibular joint ankylosis. J Cranio-Maxillo-Fac Surg. 1996;24(2):96–103. doi: 10.1016/s1010-5182(96)80020-5. [DOI] [PubMed] [Google Scholar]
- 2.Elgazzar R.F., Abdelhady A.I., Saad K.A. Treatment modalities of TMJ ankylosis: experience in Delta Nile, Egypt. Int J Oral Maxillofac Surg. 2010 Apr;39(4):333–342. doi: 10.1016/j.ijom.2010.01.005. [DOI] [PubMed] [Google Scholar]
- 3.Bhatt K., Roychoudhury A., Bhutia O., Pandey R.M. Functional outcomes of gap and interposition arthroplasty in the treatment of temporomandibular joint ankylosis. J Oral Maxillofac Surg. 2014;72:2434–2439. doi: 10.1016/j.joms.2014.08.012. [DOI] [PubMed] [Google Scholar]
- 4.Roychoudhury A., Yadav P., Alagarsamy R., Bhutia O., Goswami D. Outcome of stock total joint replacement with fat grafting in adult temporomandibular joint ankylosis patients. J Oral Maxillofac Surg. 2021 Jan;79(1):75–87. doi: 10.1016/j.joms.2020.07.214. [DOI] [PubMed] [Google Scholar]
- 5.Roychoudhury A., Parkash H., Trikha A. Functional restoration by gap arthroplasty in temporomandibular joint ankylosis: a report of 50 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999 Feb;87(2):166–169. doi: 10.1016/s1079-2104(99)70267-2. [DOI] [PubMed] [Google Scholar]
- 6.Granquist E.J., Bouloux G., Dattilo D. Outcomes and survivorship of biomet microfixation total joint replacement system: results from an FDA postmarket study. J Oral Maxillofac Surg. 2020 Sep;78(9):1499–1508. doi: 10.1016/j.joms.2020.04.021. [DOI] [PubMed] [Google Scholar]
- 7.Balon P., Vesnaver A., Kansky A., Kočar M., Prodnik L. Treatment of end stage temporomandibular joint disorder using a temporomandibular joint total prosthesis: the Slovenian experience. J Cranio-Maxillo-Fac Surg. 2019;47(1):60–65. doi: 10.1016/j.jcms.2018.10.022. [DOI] [PubMed] [Google Scholar]
- 8.Zou L., Zhao J., He D. Preliminary clinical study of Chinese standard alloplastic temporomandibular joint prosthesis. J Cranio-Maxillo-Fac Surg. 2019;47(4):602–606. doi: 10.1016/j.jcms.2019.01.045. [DOI] [PubMed] [Google Scholar]
- 9.Sahdev R., Wu B.W., Anderson N., Khawaja S.N., Kim S., Keith D.A. A retrospective study of patient outcomes after temporomandibular joint replacement with alloplastic total joint prosthesis at Massachusetts general hospital. J Oral Maxillofac Surg. 2019;77(2):280–288. doi: 10.1016/j.joms.2018.09.002. [DOI] [PubMed] [Google Scholar]
- 10.Zou L., Zhang L., He D., Yang C., Zhao J., Ellis E., 3rd Clinical and radiologic follow- up of zimmer biomet stock total temporomandibular joint replacement after surgical modifications. J Oral Maxillofac Surg. 2018;76(12):2518–2524. doi: 10.1016/j.joms.2018.06.013. [DOI] [PubMed] [Google Scholar]
- 11.Gerbino G., Zavattero E., Bosco G., Berrone S., Ramieri G. Temporomandibular joint reconstruction with stock and custom-made devices: indications and results of a 14- year experience. J Cranio-Maxillo-Fac Surg. 2017;45(10):1710–1715. doi: 10.1016/j.jcms.2017.07.011. [DOI] [PubMed] [Google Scholar]
- 12.Gerbino G., Zavattero E., Berrone S., Ramieri G. One stage treatment of temporomandibular joint complete bony ankylosis using total joint replacement. J Cranio-Maxillo-Fac Surg. 2016;44(4):487–492. doi: 10.1016/j.jcms.2016.01.003. [DOI] [PubMed] [Google Scholar]
- 13.Wolford L., Movahed R., Teschke M., Fimmers R., Havard D., Schneiderman E. Temporomandibular joint ankylosis can Be successfully treated with TMJ concepts patient-fitted total joint prosthesis and autogenous fat grafts. J Oral Maxillofac Surg. 2016;74(6):1215–1227. doi: 10.1016/j.joms.2016.01.017. [DOI] [PubMed] [Google Scholar]
- 14.Selbong U., Rashidi R., Sidebottom A. Management of recurrent heterotopic ossification around total alloplastic temporomandibular joint replacement. Int J Oral Maxillofac Surg. 2016;45(10):1234–1236. doi: 10.1016/j.ijom.2016.02.017. [DOI] [PubMed] [Google Scholar]
- 15.Kunjur J., Niziol R., Matthews N.S. Quality of life: patient-reported outcomes after total replacement of the temporomandibular joint. Br J Oral Maxillofac Surg. 2016;54(7):762–766. doi: 10.1016/j.bjoms.2016.04.022. [DOI] [PubMed] [Google Scholar]
- 16.Gruber E.A., McCullough J., Sidebottom A.J. Medium-term outcomes and complications after total replacement of the temporomandibular joint. Prospective outcome analysis after 3 and 5 years. Br J Oral Maxillofac Surg. 2015;53(5):412–415. doi: 10.1016/j.bjoms.2014.12.010. [DOI] [PubMed] [Google Scholar]
- 17.Murdoch B., Buchanan J., Cliff J. Temporomandibular joint replacement: a New Zealand perspective. Int J Oral Maxillofac Surg. 2014;43(5):595–599. doi: 10.1016/j.ijom.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 18.Leandro L.F., Ono H.Y., Loureiro C.C., Marinho K., Guevara H.A. A ten-year experience and follow-up of three hundred patients fitted with the Biomet/Lorenz Microfixation TMJ replacement system. Int J Oral Maxillofac Surg. 2013;42(8):1007–1013. doi: 10.1016/j.ijom.2013.04.018. [DOI] [PubMed] [Google Scholar]
- 19.Sidebottom A.J., Gruber E. One-year prospective outcome analysis and complications following total replacement of the temporomandibular joint with the TMJ Concepts system. Br J Oral Maxillofac Surg. 2013;51(7):620–624. doi: 10.1016/j.bjoms.2013.03.012. [DOI] [PubMed] [Google Scholar]
- 20.Idle M.R., Lowe D., Rogers S.N., Sidebottom A.J., Speculand B., Worrall S.F. UK temporomandibular joint replacement database: report on baseline data. Br J Oral Maxillofac Surg. 2014;52(3):203–207. doi: 10.1016/j.bjoms.2013.12.004. [DOI] [PubMed] [Google Scholar]
- 21.Giannakopoulos H.E., Sinn D.P., Quinn P.D. Biomet microfixation temporomandibular joint replacement system: a 3-year follow-up study of patients treated during 1995 to 2005. J Oral Maxillofac Surg. 2012;70(4):787–796. doi: 10.1016/j.joms.2011.09.031. [DOI] [PubMed] [Google Scholar]
- 22.Machon V., Hirjak D., Beno M., Foltan R. Total alloplastic temporomandibular joint replacement: the Czech-Slovak initial experience. Int J Oral Maxillofac Surg. 2012;41(4):514–517. doi: 10.1016/j.ijom.2011.12.033. [DOI] [PubMed] [Google Scholar]
- 23.Mercuri L.G., Ali F.A., Woolson R. Outcomes of total alloplastic replacement with periarticular autogenous fat grafting for management of re-ankylosis of the temporomandibular joint. J Oral Maxillofac Surg. 2008;66(9):1794–1803. doi: 10.1016/j.joms.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 24.Linsen S.S., Reich R.H., Teschke M. Mandibular kinematics in patients with alloplastic total temporomandibular joint replacement--a prospective study. J Oral Maxillofac Surg. 2012;70(9):2057–2064. doi: 10.1016/j.joms.2012.05.026. [DOI] [PubMed] [Google Scholar]
- 25.Jones R.H. Temporomandibular joint reconstruction with total alloplastic joint replacement. Aust Dent J. 2011;56(1):85–91. doi: 10.1111/j.1834-7819.2010.01288.x. [DOI] [PubMed] [Google Scholar]
- 26.Westermark A. Total reconstruction of the temporomandibular joint. Up to 8 years of follow-up of patients treated with Biomet(®) total joint prostheses. Int J Oral Maxillofac Surg. 2010;39(10):951–955. doi: 10.1016/j.ijom.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 27.Pearce C.S., Cooper C., Speculand B. One stage management of ankylosis of the 50 temporomandibular joint with a custom-made total joint replacement system. Br J Oral Maxillofac Surg. 2009;47(7):530–534. doi: 10.1016/j.bjoms.2009.04.024. [DOI] [PubMed] [Google Scholar]
- 28.Sidebottom A.J., Speculand B., Hensher R. Foreign body response around total prosthetic metal-on-metal replacements of the temporomandibular joint in the UK. Br J Oral Maxillofac Surg. 2008 Jun;46(4):288–292. doi: 10.1016/j.bjoms.2007.12.003. [DOI] [PubMed] [Google Scholar]
- 29.Haq J., Patel N., Weimer K., Matthews N.S. Single stage treatment of ankylosis of the temporomandibular joint using patient-specific total joint replacement and virtual surgical planning. Br J Oral Maxillofac Surg. 2014;52(4):350–355. doi: 10.1016/j.bjoms.2014.01.004. [DOI] [PubMed] [Google Scholar]
- 30.Brown E., Wilson M.H., Revington P. Single-stage temporomandibular joint arthroplasty in a patient with complete bony ankylosis and previous extradural haematoma. BMJ Case Rep. 2016 Oct 8 doi: 10.1136/bcr-2015-213917. bcr2015213917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Egemen O., Ozkaya O., Filinte G.T., Uscetin I., Akan M. Two-stage total prosthetic reconstruction of temporomandibular joint in severe and recurrent ankylosis. J Craniofac Surg. 2012 Sep;23(5):e520–e524. doi: 10.1097/SCS.0b013e31825b5afd. [DOI] [PubMed] [Google Scholar]
- 32.Wolford L.M., Dingwerth D.J., Talwar R.M., Pitta M.C. Comparison of 2 temporomandibular joint total joint prosthesis systems. J Oral Maxillofac Surg. 2003 Jun;61(6):685–690. doi: 10.1053/joms.2003.50112. discussion 690. [DOI] [PubMed] [Google Scholar]
- 33.Alagarsamy R., Roychoudhury A., Bhutia O., Lal B., Yadav R., Bhalla A.S. Evaluation of fit feasibility of stock total joint replacement in temporomandibular joint ankylosis patients. Br J Oral Maxillofac Surg. 2020 doi: 10.1016/j.bjoms.2020.11.016. (in press) [DOI] [PubMed] [Google Scholar]
- 34.Kraeima J., Merema B.J., Witjes M.J.H., Spijkervet F.K.L. Development of a patient-specific temporomandibular joint prosthesis according to the Groningen principle through a cadaver test series. J Cranio-Maxillo-Fac Surg. 2018;46(5):779–784. doi: 10.1016/j.jcms.2018.03.004. [DOI] [PubMed] [Google Scholar]
- 35.Sembronio S., Tel A., Costa F., Isola M., Robiony M. Accuracy of custom-fitted temporomandibular joint alloplastic reconstruction and virtual surgical planning. Int J Oral Maxillofac Surg. 2019;48(8):1077–1083. doi: 10.1016/j.ijom.2019.01.024. [DOI] [PubMed] [Google Scholar]
- 36.Xu X., Ma H., Jin S. One-stage treatment of giant condylar osteoma: alloplastic total temporomandibular joint replacement aided by digital templates. J Craniofac Surg. 2018;29(3):636–639. doi: 10.1097/SCS.0000000000004097. [DOI] [PubMed] [Google Scholar]
- 37.Patel A., Otterburn D., Saadeh P., Levine J., Hirsch D.L. 3D Volume assessment techniques and computer-aided design and manufacturing for preoperative fabrication of implants in head and neck reconstruction Facial. Plast Surg Clin North Am. 2011;19(4):683–709. doi: 10.1016/j.fsc.2011.07.010. [DOI] [PubMed] [Google Scholar]
- 38.Jones R. The use of virtual planning and navigation in the treatment of temporomandibular joint ankylosis. Aust Dent J. 2013;58(3):358–367. doi: 10.1111/adj.12086. [DOI] [PubMed] [Google Scholar]
- 39.Bai G., He D., Yang C., Chen M., Yuan J., Wilson J.J. Application of digital templates to guide total alloplastic joint replacement surgery with biomet standard replacement system. J Oral Maxillofac Surg. 2014 Dec;72(12):2440–2452. doi: 10.1016/j.joms.2014.08.014. [DOI] [PubMed] [Google Scholar]
- 40.Bai G., Yang C., He D., Zhang X., Abdelrehem A. Application of fossa bone graft to stabilize stock total joint prosthesis in temporomandibular joint surgery. J Cranio-Maxillo-Fac Surg. 2015;43(8):1392–1397. doi: 10.1016/j.jcms.2015.06.048. [DOI] [PubMed] [Google Scholar]
- 41.Rhee S.H., Baek S.H., Park S.H., Kim J.C., Jeong C.G., Choi J.Y. Total joint reconstruction using computer-assisted surgery with stock prostheses for a patient with bilateral TMJ ankylosis. Maxillofac Plast Reconstr Surg. 2019 Oct 10;41(1):41. doi: 10.1186/s40902-019-0225-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yadav P & Roychoudhury A & Bhutia O. Strategies to reduce re-ankylosis in temporomandibular joint ankylosis patients. Br J Oral Maxillofac Surg. 10.1016/j.bjoms.2021.02.007. [DOI] [PubMed]
- 43.Kaban L.B., Bouchard C., Troulis M.J. A protocol for management of temporomandibular joint ankylosis in children. J Oral Maxillofac Surg. 2009 Sep;67(9):1966–1978. doi: 10.1016/j.joms.2009.03.071. [DOI] [PubMed] [Google Scholar]
- 44.Mercuri L.G. A rationale for total alloplastic temporomandibular joint reconstruction in the management of idiopathic/progressive condylar. J Oral Maxillofac Surg. 2007 Aug;65(8):1600–1609. doi: 10.1016/j.joms.2006.03.056. Erratum in: J Oral Maxillofac Surg. 2008 Jan;66(1):208. [DOI] [PubMed] [Google Scholar]
- 45.Wolford L.M., Mercuri L.G., Schneiderman E.D., Movahed R., Allen W. Twenty-year follow-up study on a patient-fitted temporomandibular joint prosthesis: the Techmedica/TMJ Concepts device. J Oral Maxillofac Surg. 2015 May;73(5):952–960. doi: 10.1016/j.joms.2014.10.032. [DOI] [PubMed] [Google Scholar]
- 46.Mercuri L.G. Costochondral graft versus total alloplastic joint for temporomandibular joint reconstruction. Oral Maxillofac Surg Clin North Am. 2018 Aug;30(3):335–342. doi: 10.1016/j.coms.2018.05.003. [DOI] [PubMed] [Google Scholar]
- 47.Dimitroulis G. Temporomandibular joint surgery: what does it mean to India? J Maxillofac Oral Surg. 2012;11(3):249–257. doi: 10.1007/s12663-012-0419-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mercuri L.G. Total joint reconstruction--autologous or alloplastic. Oral Maxillofac Surg Clin North Am. 2006 Aug;18(3):399–410. doi: 10.1016/j.coms.2006.03.003. vii. [DOI] [PubMed] [Google Scholar]
- 49.Bessette B.J., Fassier F., Tanzer M., Brooks C.E. Total hip arthroplasty in patients younger than 21 years: a minimum, 10-year follow- up. Can J Surg. 2003;46:257–262. [PMC free article] [PubMed] [Google Scholar]
- 50.Wroblewski B.M., Purbach B., Siney P.D., Fleming P.A. Charnley low-friction arthro- plasty in teenage patients: the ultimate challenge. J Bone Joint Surg Br. 2010;92:486–488. doi: 10.1302/0301-620X.92B4.23477. [DOI] [PubMed] [Google Scholar]
- 51.Mercuri L.G., Swift J.Q. Considerations for the use of alloplastic temporomandibular joint replacement in the growing patient. J Oral Maxillofac Surg. 2009 Sep;67(9):1979–1990. doi: 10.1016/j.joms.2009.05.430. [DOI] [PubMed] [Google Scholar]
- 52.Keyser B.R., Banda A.K., Mercuri L.G., Warburton G., Sullivan S.M. Alloplastic total temporomandibular joint replacement in skeletally immature patients: a pilot survey. Int J Oral Maxillofac Surg. 2020;49(9):1202–1209. doi: 10.1016/j.ijom.2020.02.001. [DOI] [PubMed] [Google Scholar]
- 53.Sidebottom A.J. Alloplastic or autogenous reconstruction of the TMJ. J Oral Biol Cra- niofac Res. 2013;3:135–139. doi: 10.1016/j.jobcr.2013.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Moss M.L., Salantijn L. The capsular matrix. Am J Orthod. 1969;56:474–490. doi: 10.1016/0002-9416(69)90209-7. [DOI] [PubMed] [Google Scholar]
- 55.Movahed R., Wolford L.M. Protocol for concomitant temporomandibular joint custom-fitted total joint reconstruction and orthognathic surgery using computer-assisted surgical simulation. Oral Maxillofac Surg Clin North Am. 2015 Feb;27(1):37–45. doi: 10.1016/j.coms.2014.09.004. [DOI] [PubMed] [Google Scholar]
- 56.Lindqvist C., Soderholm A.L., Hallikainen D., Sjövall L. Erosion and heterotopic bone formation after alloplastic temporomandibular joint reconstruction. J Oral Maxillofac Surg. 1992;50:942–950. doi: 10.1016/0278-2391(92)90051-z. [DOI] [PubMed] [Google Scholar]
- 57.Wolford L.M., Karras S.C. Autologous fat transplantation around temporomandibular joint total joint prostheses: preliminary treatment outcomes. J Oral Maxillofac Surg. 1997;55(3):245–252. doi: 10.1016/s0278-2391(97)90535-8. [DOI] [PubMed] [Google Scholar]
- 58.Wolford L.M., Morales-Ryan C.A., Morales P.G., Cassano D.S. Autologous fat grafts placed around temporomandibular joint total joint prostheses to prevent heterotopic bone formation. Proc (Bayl Univ Med Cent). 2008;21(3):248–254. doi: 10.1080/08998280.2008.11928404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Roychoudhury A., Acharya S., Bhutia O., Seith Bhalla A., Manchanda S., Pandey R.M. Is there a difference in volumetric change and effectiveness comparing pedicled buccal fat pad and abdominal fat when used as interpositional arthroplasty in the treatment of temporomandibular joint ankylosis? J Oral Maxillofac Surg. 2020;78(7):1100–1110. doi: 10.1016/j.joms.2020.03.006. [DOI] [PubMed] [Google Scholar]
- 60.Jose A., Nagori S.A., Virkhare A., Bhatt K., Bhutia O., Roychoudhury A. Piezoelectric osteoarthrectomy for management of ankylosis of the temporomandibular joint. Br J Oral Maxillofac Surg. 2014;52(7):624–628. doi: 10.1016/j.bjoms.2014.04.012. [DOI] [PubMed] [Google Scholar]
- 61.Bhatt K., Pandey S., Bhutia O., Roychoudhury A. Use of indomethacin as an adjuvant to surgery for recurrent temporomandibular joint ankylosis in adults. Natl J Maxillofac Surg. 2014 Jul-Dec;5(2):198–201. doi: 10.4103/0975-5950.154836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wolford L.M., Mehra P. Custom-made total joint prostheses for temporomandibular joint reconstruction. Proc (Bayl Univ Med Cent). 2000 Apr;13(2):135–138. doi: 10.1080/08998280.2000.11927656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mercuri L.G., Edibam N.R., Giobbie-Hurder A. Fourteen-year follow-up of a patient-fitted total temporomandibular joint reconstruction system. J Oral Maxillofac Surg. 2007 Jun;65(6):1140–1148. doi: 10.1016/j.joms.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 64.Mercuri L.G., Psutka D. Perioperative, postoperative, and prophylactic use of antibiotics in alloplastic total temporomandibular joint replacement surgery: a survey and preliminary guidelines. J Oral Maxillofac Surg. 2011;69(8):2106–2111. doi: 10.1016/j.joms.2011.01.006. [DOI] [PubMed] [Google Scholar]
- 65.Mercuri G.L. The role of custom-made prosthesis for temporomandibular joint replacement. Rev Española Cirugía Oral Maxilofac. 2013;35(1):1–10. [Google Scholar]
- 66.Mustafa el M., Sidebottom A. Risk factors for intraoperative dislocation of the total temporomandibular joint replacement and its management. Br J Oral Maxillofac Surg. 2014 Feb;52(2):190–192. doi: 10.1016/j.bjoms.2013.09.018. [DOI] [PubMed] [Google Scholar]