Abstract
Background:
Methamphetamine use is a growing public health concern in the United States. Prior analyses with nationally representative data from 2015-2017 suggested that increases in methamphetamine use appeared largely selective to people using heroin. This analysis updated prior estimates to determine if trends are selectively persistent and how they compare to historical trends. We also evaluate sociodemographic risk factors associated with methamphetamine use among people using heroin.
Methods:
Data from the 2015-2019 National Surveys on Drug Use and Health (NSDUH) were analyzed. Data from the 2006-2014 NSDUH were summarized for historical trends. Past month and past year methamphetamine use prevalence was determined within populations using heroin as well as those using other drugs (e.g., cocaine, cannabis). Multivariable logistic models accounting for complex survey design evaluated predictors of methamphetamine use among people using heroin.
Results:
From 2015 to 2019, past month methamphetamine use increased from 9.0% to 44.0% within the population of people reporting past month heroin use. Similarly, past year methamphetamine use increased from 22.5% to 46.7% among those reporting past year heroin use. Risk factors for methamphetamine use among people using heroin included rurality, past year injection drug use, and serious mental illness.
Conclusions:
A rapid, selective, and sustained increase in methamphetamine use is evident among people using heroin. These findings combined with similar findings in treatment admission and overdose data emphasize the need for increased attention to a specific type of high-risk use pattern in the US, an issue that appears increasingly unlikely to naturally resolve.
Keywords: Injection, Opioid, Polydrug, Rural, Stimulant
1. Introduction
Regional and national data document mounting public health issues related to methamphetamine use among people who use heroin. Specifically, evidence suggests rising methamphetamine use prevalence among people using heroin (Palamar et al., 2020; Strickland et a., 2019), increasing stimulant-involved overdoses (Gladden et al., 2019; Lim et al., 2021), and more methamphetamine use reported among primary heroin treatment admissions (Cicero et al., 2020; Ellis et al., 2018; Jones et al., 2020b). From a supply-side perspective, such increases may relate to greater methamphetamine availability (U.S. Customs and Border Protection, 2021) and higher-potency, lower-cost product (DEA, 2020) combined with ongoing law enforcement and regulatory efforts targeting reductions in heroin and other opioid supply. Qualitative data have explored motives for co-use of methamphetamine and heroin, finding that people who use heroin are co-using methamphetamine to mitigate opioid withdrawal, as a cheaper substitute for heroin, to create synergistic highs, and as a perceived safer alternative following spikes in opioid overdose fatalities (Ellis et al., 2018; Lopez et al., 2021).
We previously analyzed nationally representative data from 2015-2017 to determine methamphetamine use prevalence rates within populations of people who use other drugs (Strickland et al., 2019). In those analyses, we found that increases in past month methamphetamine use were largely selective to people using opioids, with the largest of these increases in methamphetamine use for people using heroin. Trends in past year methamphetamine use in the general population and within specific subgroups were also recently analyzed from 2015-2018 by Palamar and colleagues (2020). Increases in past year methamphetamine use were observed for several populations reporting other past year drug use, including people reporting past year heroin use (22.5% to 37.4%) and past year LSD use (5.1% to 10.3%) with smaller, but significant, increases for people using ecstasy (6.1% to 10.8%), cocaine (8.4% to 11.8%), and non-medical prescription opioids (5.4% to 8.0%) in the past year. What is evident from these analyses is that methamphetamine use is increasing among a subgroup of Americans and among people that use heroin, in particular. However, it is unclear if increases in methamphetamine use prevalence have continued among people using heroin and if evidence of increases in other subgroups reflect emerging upward trends or more transient increases.
This Short Communication provides a timely update on prior analyses that documented increases in methamphetamine use among people using heroin from 2015-2017 (Strickland et al., 2019) as well as new analyses aimed at further characterizing this phenomenon. We sought to evaluate if trends in prevalence across past month and year use contexts were selectively persistent in more recent years or had plateaued, to assess similar trends in methamphetamine use historically, and to identify sociodemographic risk factors associated with methamphetamine use within the population of people using heroin.
2. Methods
Data from the 2015-2019 National Surveys on Drug Use and Health (NSDUH) were analyzed. The NSDUH population consists of non-institutionalized US residents, aged 12 years and older, with dwelling units including households, homeless shelters, and other non-institutional group quarters. We also used data from the 2006-2014 NSDUH for historical trends, although data were not directly compared with 2015-2019 given 2015 changes in NSDUH questions that make comparisons non-analogous (Substance Abuse and Mental Health Services Administration, 2015). All NSDUH protocols are approved by Institutional Review Boards and the Johns Hopkins University Institutional Review Boards considered this analysis of public data exempt.
Primary dependent measures were past month and past year methamphetamine use. We evaluated methamphetamine use prevalence as predicted by use of other drugs and classes (i.e., heroin, cocaine, cannabis, LSD, and non-medical use of prescription opioids, stimulants, tranquilizers, and sedatives). Year-specific prevalence estimates of methamphetamine use and corresponding 95% confidence intervals for proportions were determined within each of these populations of people reporting other drug use (e.g., methamphetamine use among people who use heroin, methamphetamine use among people who use cannabis). Temporal trends were analyzed with the predictor of other drug use (e.g., heroin use) interacting with time wherein significant interactions reflected different temporal trends in methamphetamine use prevalence within populations using the predictor drug compared to those not endorsing use. Multivariable logistic regression was then used to determine the association of sociodemographic factors with methamphetamine use among people reporting past year heroin use, collapsing 2015-2019 cohorts (1,063 respondents). We analyzed past year heroin use given lower power in the past month heroin use cohort (500 respondents). Data analysis was conducted in R using the survey package for sampling weights and design-based variance estimation (Lumley, 2011). Code to replicate analyses is available at https://osf.io/ga5en/?view_only=617f62a084c54bfd8280109cf78cc458.
3. Results
3.1. Methamphetamine Prevalence Estimates
Figure 1 highlights a rapid and sustained increase in methamphetamine use from 2015-2019 among people using heroin (Supplemental Materials for point estimates and 95% confidence intervals). From 2015-2019, within the population of people using heroin in the past year, past month methamphetamine use increased from 8.2% to 34.2% and past year methamphetamine use increased from 22.5% to 46.7%. Similar patterns were observed within the past month heroin use population, with past month methamphetamine use increasing from 9.0% to 44.0% and past year methamphetamine use increasing from 17.8% to 49.2%. Importantly, within the population of people using heroin, no appreciable increases in use of other drug classes were observed indicating that changes were specific to increased methamphetamine use (Supplemental Figure 3 and Supplemental Table 5).
Figure 1. Prevalence of Methamphetamine Use within Populations Who Use Other Drugs.
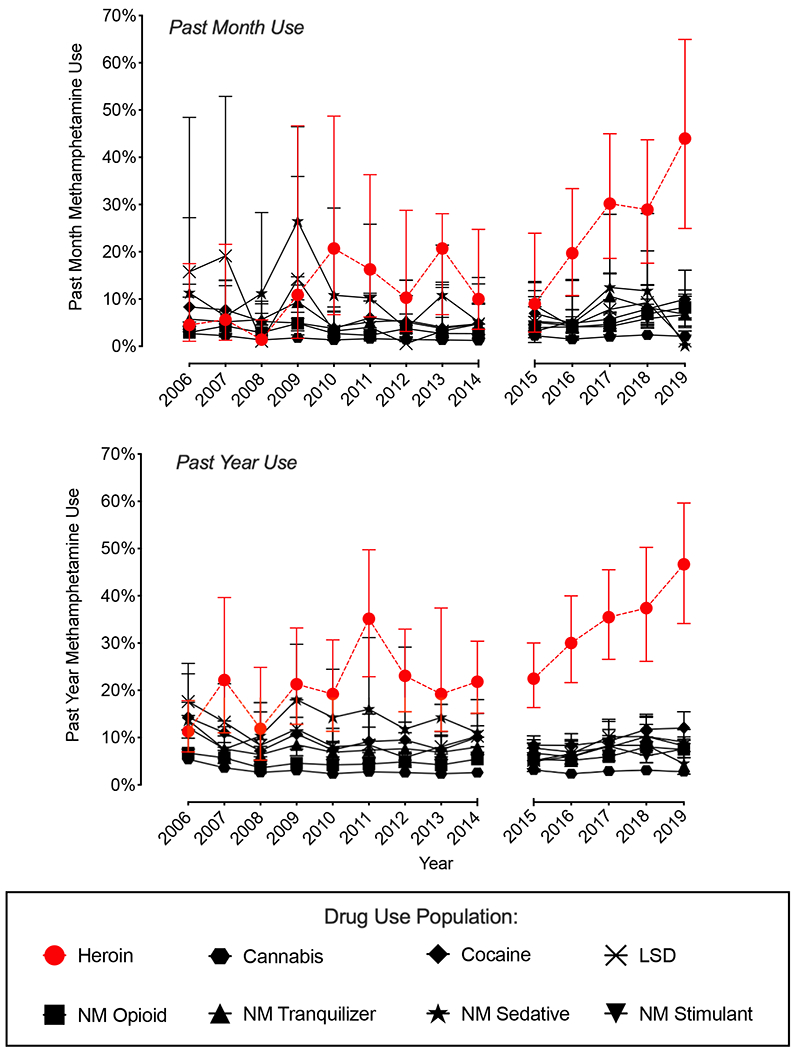
Plotted are prevalence estimates and 95% confidence intervals for past month (top) and past year (bottom) methamphetamine use for the population of people who used other drugs and classes in the past month (top) or past year (bottom). Estimates of methamphetamine use are plotted for the population of people reporting heroin use (red dotted lines/circles) as well as use of other drug types (black lines/other symbols). Data are demarcated into 2006-2014 and 2015-2019 blocks due to question changes that preclude direct comparison. NM = non-medical use.
Figure 1 also emphasizes how increasing trends in methamphetamine use prevalence were not readily apparent outside of the population of people using heroin. Lower and generally stable past month and year methamphetamine use prevalence were observed in populations reporting other drug use during this period (e.g., stability in past month methamphetamine use among people who used cannabis; Supplemental Tables 1–4).
Prevalence of past month methamphetamine use by people who did not use non-medical opioids (prescription opioids or heroin) was 0.25% [95% CI: 0.20-0.31%] in 2015 and 0.31% [0.25-0.39%] in 2019 while past year methamphetamine use was 0.38% [0.31-0.46%] in 2015 and 0.44% [0.36-0.53%] in 2019. Similar estimates of methamphetamine use were observed when sub-setting to the population of people without heroin use (Supplemental Table 6).
3.2. Temporal Trend Tests
Use by time interactions predicting methamphetamine use prevalence treating time as a continuous variable were statistically significant for the population of people reporting past month heroin use, p = .01, and past year heroin use, p = .003. This interaction reflected greater yearly increases in past month and past year methamphetamine use prevalence in those groups, respectively, compared to respondents that did not report heroin use. Use by linear time interactions for all other drug use populations evaluated were not statistically significant, p > .08. Generally consistent results were observed treating time as a categorical variable (Supplemental Tables 1–4). Although some significant individual year differences were observed for other drugs (e.g., greater past year methamphetamine use in 2017 and 2018 for people who used LSD in the past year), these yearly trends were not consistent over time (e.g., increases in methamphetamine use in the past year LSD use population were not present in 2019 and were not observed for in the past LSD month use population). In the no opioid use population, no differences were observed when treating time categorically. A slightly positive and significant linear trend was observed for past month, OR = 1.11, p = 004, and past year, OR = 1.07, p = .03, use reflecting small increases over time in methamphetamine use prevalence among people who did not report non-medical opioid use.
3.3. Sociodemographic Correlates
Multivariable logistic models evaluated the association of sociodemographic variables with past year methamphetamine use within the population of people reporting past year heroin use (Table 1). Rurality, past year injection drug use, past year serious mental illness, and identifying as White were associated with greater odds of past year methamphetamine use, whereas past year drug-specific treatment was associated with a lower odds of past year methamphetamine use. Similar results were observed when predicting past month methamphetamine use with the exception that the race association was not significant (Supplemental Table 7).
Table 1.
Sociodemographic Correlates of Methamphetamine Use Among People Who Use Heroin
| Past Year Methamphetamine Use | |||
|---|---|---|---|
| Not in Group | In Group | AOR (95% CI) | |
| Female | 32.0% | 38.1% | 0.95 (0.55, 1.65) |
| Young (< 26 years old) | 32.9% | 37.9% | 1.26 (0.78, 2.02) |
| White | 23.0% | 38.0% | 2.15 (1.25, 3.69)** |
| Sexual Minority | 33.2% | 40.6% | 1.24 (0.65, 2.35) |
| High School Graduate | 29.8% | 35.0% | 1.20 (0.70, 2.05) |
| Employed | 35.8% | 32.1% | 0.85 (0.55, 1.32) |
| Below Poverty Line | 31.3% | 39.3% | 1.50 (0.99, 2.28) |
| Rural | 33.1% | 53.7% | 2.31 (1.08, 4.95)* |
| Past Year Injection Drug Use | 26.9% | 40.3% | 1.85 (1.23, 2.77)** |
| Serious Mental Illness | 29.0% | 48.7% | 2.12 (1.32, 3.42)** |
| Past Year Drug-Specific Treatment | 35.2% | 30.1% | 0.61 (0.39, 0.98)* |
Note. Not in Group/In Group estimates reflect percentage of people who endorsed past year methamphetamine use who did not (Not in Group) or did (In Group) belong to the row variable category. AOR = adjusted odds ratio. Rural refers to regions not in a Core Based Statistical Area (CBSA).
p < .05
p < .01
p < .001
4. Discussion
This analysis provides an update on national methamphetamine use trends in the United States among populations of people who use other drugs and further emphasizes a selective and sustained increase in methamphetamine use among people using heroin. Past month methamphetamine use increased approximately five-fold from 2015-2019 within the population of people using heroin in the past month. Prevalence of methamphetamine use for populations not reporting non-medical opioid use remained low. Similarly, temporal trends in methamphetamine use for populations reporting other drug use were not consistent (e.g., people reporting past year LSD use showed a large proportional increase in methamphetamine use in 2017 and 2018, but downward trend in 2019). Together, these findings emphasize increases in methamphetamine use among people who use heroin that are striking and consistent, with key implications for use-related harms and treatment efforts.
These results identified concerning sociodemographic factors and health characteristics closely associated with methamphetamine use among people who use heroin – namely, rurality, injection drug use, and serious mental illness. These risk factors are consistent with those predictive of methamphetamine use more generally (Jones et al., 2020a) and are factors commonly associated with more complicated substance use disorder and psychiatric treatment trajectories. Co-occurring substance use that includes both methamphetamine and heroin, the latter increasingly adulterated with fentanyl, and which is also associated with injection drug use, has the potential to further strain health systems by contributing to increased morbidities and mortalities among an already vulnerable population of rural-dwelling adults with serious mental illness (Mattson et al. 2021). That methamphetamine and heroin supply will likely not decrease in coming years, and that among people using heroin those without recent treatment involvement had a greater odds of methamphetamine use, emphasizes the urgency of this public health crisis and commensurate urgency in addressing barriers to substance use disorder and psychiatric care. In fact, previously identified motives for co-occurring methamphetamine and heroin use in qualitative work directly relate to unaddressed treatment needs, including methamphetamine use for mitigation of opioid withdrawal and for overdose avoidance (Lopez et al., 2021). Targeted expansion of treatment programs that can address these needs (e.g., access to medications to alleviate opioid withdrawal) or community-based harm reduction services (e.g., drug checking) may be beneficial in developing comprehensive, scientifically informed prevention and intervention systems. Identifying and implementing the prevention and treatment pathways is essential given the lack of effective interventions for methamphetamine use among people using opioids (Chan et al., 2020) and the high health risks associated with such co-occurring use (Howell et al., 2021).
Limitations of this analysis include the use of cross-sectional data constrained to the NSDUH population, which does not include institutionalized people. Offsetting this limitation is that these analyses possibly underestimate the growth trajectory given the lack of data on institutionalized populations that may show disproportionately higher rates of substance use, such as criminal-justice involved groups. Our sociodemographic analyses were also restricted to the past year heroin use cohort. This strategy was selected to improve power given the smaller sample in the past month cohort, even when combining across five years of data. The nature of NSDUH data also means we cannot evaluate the temporal proximity of co-use and distinguish between simultaneous use (i.e., co-administration of methamphetamine and heroin) and concurrent use (i.e., use of both drugs over a given period, although not necessarily simultaneously). This limitation emphasizes the need for future data collected in person-context (e.g., ecological momentary assessment) that can better establish the temporal patterns of use underlying this emergent trend.
These findings emphasize a consistent increase in methamphetamine use among people who use heroin in the United States from 2015-2019, uniqueness of use changes when considered with 2006-2014, and general selectivity of this increase to both the population of people using heroin compared to people who use other drugs and to methamphetamine use within this heroin use population. Each of these findings highlight the need for continued attention to a specific type of high-risk use pattern in the United States, an issue that appears increasingly unlikely to naturally resolve.
Supplementary Material
Highlights.
We evaluate methamphetamine use by people who use heroin from 2015 to 2019
Past month methamphetamine use increased from 9.0% to 44.0%
Past year methamphetamine use increased from 22.5% to 46.7%
Risk factors were rurality, past year injection drug use, & serious mental illness
Acknowledgments
Role of Funding Source
Support for JCS was provided by NIDA T32DA07209. JRH was supported by NIDA R01DA033862. Support for KES was provided by the Intramural Research Program of the NIH NIDA. In the past 3 years, KED has served as a consultant for Beckley-Canopy Therapeutics, Canopy Corporation, and Grünenthal, Inc. All other authors report no financial disclosures.
Footnotes
Conflict of Interest
The authors have no conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Chan B, Freeman M, Ayers C, Korthuis PT, Paynter R, Kondo K, Kansagara D, 2020. A systematic review and meta-analysis of medications for stimulant use disorders in patients with co-occurring opioid use disorders. Drug Alcohol Depend. 216, 108193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicero TJ, Ellis MS, Kasper ZA, 2020. Polysubstance use: A broader understanding of substance use during the opioid crisis. Am. J. Public Health. 110, 244–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drug Enforcement Administration, 2020. 2019 National Drug Threat Assessment. U.S. Department of Justice, https://www.dea.gov/documents/2020/01/30/2019-national-drug-threat-assessment Accessed February 28, 2011. [Google Scholar]
- Ellis MS, Kasper ZA, Cicero TJ, 2018. Twin epidemics: The surging rise of methamphetamine use in chronic opioid users. Drug Alcohol Depend. 193, 14–20. [DOI] [PubMed] [Google Scholar]
- Gladden RM, O’Donnell J, Mattson CL, Seth P, 2019. Changes in opioid-involved overdose deaths by opioid type and presence of benzodiazepines, cocaine, and methamphetamine—25 states, July–December 2017 to January–June 2018. Morb. Mortal. Wkly. Rep. 68(34), 737–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howell BA, Bart G, Wang EA, Winkelman TN, 2021. Service involvement across multiple sectors among people who use opioids, methamphetamine, or both, United States—2015–2018. Med. Care. 59, 238–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CM, Compton WM, Mustaquim D 2020a, Patterns and characteristics of methamphetamine use among adults—United States, 2015–2018. Morb. Mortal. Wkly. Rep. 69, 317–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CM, Underwood N, Compton WM, 2020. Increases in methamphetamine use among heroin treatment admissions in the United States, 2008–17. Addiction. 115, 347–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim JK, Earlywine JJ, Bagley SM, Marshall BD, Hadland SE, 2021. Polysubstance involvement in opioid overdose deaths in adolescents and young adults, 1999-2018. JAMA Pediatr. 175, 194–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez AM, Dhatt Z, Howe M, Al-Nassir M, Billing A, Artigiani E, Wish ED, 2021. Co-use of methamphetamine and opioids among people in treatment in Oregon: A qualitative examination of interrelated structural, community, and individual-level factors. Int. J. Drug Policy, 91, 103098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumley T Complex surveys: a guide to analysis using R. John Wiley & Sons; 2011. [Google Scholar]
- Mattson CL, Tanz LJ, Quinn K, Kariisa M, Patel P, & Davis NL, 2021. Trends and geographic patterns in drug and synthetic opioid overdose deaths—United States, 2013–2019. Morb. Mortal. Wkly. Rep, 70(6), 202–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar JJ, Han BH, Keyes KM, 2020. Trends in characteristics of individuals who use methamphetamine in the United States, 2015-2018. Drug Alcohol Depend. 213, 108089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strickland JC, Havens JR, Stoops WW, 2019. A nationally representative analysis of “twin epidemics”: Rising rates of methamphetamine use among persons who use opioids. Drug Alcohol Depend. 204, 107592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration, 2015. National Survey on Drug Use and Health: 2014 and 2015 Redesign Changes. Substance Abuse and Mental Health Services Administration, Rockville, MD. [PubMed] [Google Scholar]
- U.S. Customs and Border Protection, 2020. CBP Enforcement Statistics FY2020. U.S. Department of Homeland Security. Washington DC. https://www.cbp.gov/newsroom/stats/cbp-enforcement-statistics-fy2020. Accessed February 28, 2021. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


