Abstract
Background:
Chronic pain is challenging and costly to treat. Depression and anxiety co-occur with chronic pain. Identifying psychosocial mechanisms contributing to emotional outcomes among chronic pain patients can inform future iterations of this intervention.
Methods:
We examined explanatory mechanisms of change in emotional distress following a mind-body and activity intervention among 82 participants (21 – 79 years old, 65.85% female, 80.48% White). With depression and anxiety as outcomes, potential mediators were hypothesized to be change in pain catastrophizing, mindfulness, and pain resilience. Mixed-effects modeling were used to assess the indirect effects of time on each outcome variables through hypothesized mediators in a simultaneous model.
Results:
Improvements in depression from baseline to post-treatment were most explained by pain catastrophizing, (b = −2.53, CI = [−3.82, −1.43]), followed by mindfulness, (b = −1.21, CI = [−2.15, −0.46]), and pain resilience, (b = −0.76, CI = [−1.54, −1.66]). Improvements in anxiety from baseline to post-treatment were most explained by pain catastrophizing, (b = −2.16, CI = [−3.45, −1.08]) and mindfulness, (b = −1.51, CI = [−2.60, −0.65]), but not by pain resilience, (b = −0.47, CI = [−1.26, 0.17]).
Limitations:
Findings are limited by lack of a control group, relatively small sample, and two timepoints. However, findings can guide future mind-body intervention efficacy testing trials.
Conclusions:
Pain catastrophizing and mindfulness appear to be important intervention targets to enhance emotional functioning for chronic pain patients, and should be considered simultaneously in interventions for chronic pain.
Keywords: chronic pain, depression, anxiety, pain catastrophizing, mindfulness, pain resilience
Introduction
Chronic pain, or pain that persists for more than three months, affects up to 100 million adults in the U.S. and totals about $600 billion in costs annually (Institute of Medicine, 2011; Treede et al., 2015). Up to 72% of chronic pain patients experience clinically significant levels of depression and anxiety (Rayner et al., 2016). Depression and anxiety are closely linked to worse long-term physical functioning among chronic pain patients, and although modifiable, they are insufficiently addressed in treatment (Tseli et al., 2019). Biomedical treatments for chronic pain, such as surgery and medication are costly, only partially effective, and often include serious side effects which can worsen emotional distress (Domenichiello & Ramsdan, 2019). Despite the relationships among pain, depression, and anxiety, most randomized controlled trials (RCTs) focus on pain intensity and pain-related disability, as opposed to emotional distress (Barke et al., 2019). Among psychosocial interventions for chronic pain – cognitive-behavioral therapy (CBT), acceptance and commitment therapy (ACT), mindfulness – that are cost-effective and pose low risk for patients have exhibited small-to-moderate effects in managing pain and decreasing emotional distress (Eyer & Thorn, 2016; Veehod et al., 2016). We have previously shown that a mind-body activity program with two RCT arms (GetActive; GetActive-Fitbit) developed iteratively with feedback from patients, has high feasibility, acceptability, and is associated with improvements in depression and anxiety among patients with heterogenous musculoskeletal chronic pain (Greenberg et al., 2019, 2020). Given the importance of identifying mechanisms (i.e., process variables) prior to RCT efficacy testing (Nielsen et al., 2018), the present secondary analysis sought to test whether the mechanisms targeted within this program contributed to improved depression and anxiety.
Few interventions have merged conceptual models (Meints & Edwards, 2018) and examined multiple mediators of change that uniquely contribute to emotional outcomes among those with chronic pain (Trompetter et al., 2015). Our mind-body activity program is based on a conceptual biopsychosocial model (Relaxation Response Resiliency Program (3RP); Park et al., 2013) and integrates elements from the fear-avoidance model of pain (Crombez et al., 2012), cognitive model of pain (Turk & Okifuji, 2002), acceptance and commitment therapy for chronic pain (McCracken et al., 2004), mindfulness for pain (Grabovac et al., 2011), and positive psychology (Fredrickson, 2001) to promote resilience and willingness to engage in physical activity. Based on these conceptual models and current literature, hypothesized mechanisms of change included pain catastrophizing (fear-avoidance and cognitive models), mindfulness (ACT and mindfulness models), and pain resilience (ACT and positive psychology models).
Pain catastrophizing, or negative beliefs about pain, has been identified as a vulnerability factor that helps to explain patient improvement within CBT RCTs for chronic pain (Trompetter et al., 2015). Decreases in pain catastrophizing mediate the relationship between pain and depressed mood (e.g., Cheng et al., 2018; Wood et al., 2016). Recently, Dong and colleagues (2020) reported a significant relationship between catastrophizing and anxiety. However, interventions that specifically target pain catastrophizing tend to exhibit small-to-moderate effect sizes on pain, disability, and mood (Vlaeyen & Linton, 2012). Chronic pain interventions that target multiple psychological factors, such as pain acceptance or resilience, may help to increase effect sizes and enhance efficacy (Dong et al., 2020).
Interventions that promote resilience, positive activities, and acceptance of chronic pain (e.g., ACT, positive psychology, mindfulness) provide insights into additional potential mechanisms of change that informed our program (Hassett & Finan, 2016; Lumlet & Schubiner, 2020). Mindfulness, or nonjudgmental awareness of the present moment, skills have been successful for improving emotional functioning in chronic pain (Baer, 2003). However, few studies have examined mindfulness as a process of change (McCracken & Vowles, 2014). Curtin and Norris (2017) reported that mindfulness practice was associated with reduced anxiety among individuals with chronic pain, suggesting that it may be an important target for intervention. Further, although pain resilience remains understudied, several researchers have hypothesized that increased self-efficacy may increase resilience to stay active while coping with chronic pain (Akerbolm et al., 2015; Cheng et al., 2019; Radat et al., 2010). Together, findings suggest that pain catastrophizing, mindfulness, and pain resilience are important targets of intervention for improving emotional outcomes among patients with chronic pain.
The Current Study
We conducted a secondary analysis of data from an RCT testing a mind-body activity program using mixed-effects modeling to determine whether the hypothesized mechanisms of change – pain catastrophizing, mindfulness, pain resilience – helped to explain the effect of the intervention on depression and anxiety (baseline to post-treatment) among patients with chronic pain. Our goal was to determine the extent to which these psychological processes explained the effect of the treatment on the emotional outcomes, over and above the effects of each other, by simultaneously including in one overarching model. We hypothesized that improvement in pain catastrophizing, mindfulness, and pain resilience would each uniquely explain improvements in depression and anxiety within a mind-body activity intervention across both RCT arms (GetActive; GetActive-Fitbit). Given that both arms utilized an active intervention, we assessed mediators of change across groups and controlled for any group differences in analyses. Findings regarding mechanisms of change for emotional outcomes will inform future fully powered efficacy trials of the intervention.
Methods
Information regarding sample, recruitment, intervention groups, and assessments relevant to this secondary analysis are described below. Additional details about intervention screening, randomization, intervention components, and effects of interventions on measured variables are reported in previous manuscripts (Greenberg et al., 2019; Greenberg et al., 2020).
Participants
Eighty-two participants with heterogenous musculoskeletal chronic pain were enrolled in this study between July 2018 and September 2019 at Massachusetts General Hospital Pain Clinic. Participant ages ranged from 21 to 79 (M = 51.77, SD = 14.53). Table 1 presents additional socio-demographics for the sample. Table 2 displays clinical characteristics, including medical diagnoses, mental health history, and current medications.
Table 1.
Participant Socio-Demographics Variables
| Total (N = 82) | |
|---|---|
| Sex/Gender | n (%) |
| Female | 54 (65.85%) |
| Male | 28 (34.15%) |
| Racial background | |
| White | 66 (80.48%) |
| Black or African-American | 7 (8.54%) |
| Bi/multiracial | 4 (4.87%) |
| Asian | 3 (3.66%) |
| American Indian or Alaska Native | 2 (2.44%) |
| Ethnicity | |
| Non-Hispanic or Latino/Latina | 72 (87.80%) |
| Hispanic or Latino/Latina | 8 (9.75%) |
| Not reported | 2 (2.44%) |
| Marital Status | |
| Single, never married | 28 (34.15%) |
| Married | 23 (28.05%) |
| Separated/Divorced | 16 (19.51%) |
| Living with significant other | 11 (13.41%) |
| Widowed | 4 (4.87%) |
| Annual Household Income | |
| Less than $10,000 | 18 (21.95%) |
| $10,000 – less than $20,000 | 14 (17.07%) |
| $20,000 – less than $35,000 | 12 (14.63%) |
| $35,000 – less than $50,000 | 9 (10.97%) |
| $50,000 – less than $75,000 | 7 (8.54%) |
| $75,000 or greater | 17 (20.73%) |
| Not reported | 5 (6.10%) |
| Education | |
| High school graduate or GED | 11 (13.41%) |
| Some college/Associate degree | 26 (31.71%) |
| Completed 4 years of college | 17 (20.73%) |
| Graduate/professional degree | 28 (34.15%) |
| Employment | |
| Employed full-time | 17 (20.73%) |
| Employed part-time | 11 (13.41%) |
| Student (full-time or part-time) | 3 (3.70%) |
| Self-employed | 1 (1.22%) |
| Retired | 18 (21.95%) |
| Unemployed | 18 (21.95%) |
| Disability | 12 (14.63%) |
| Worker’s Compensation | 2 (2.44%) |
Table 2.
Participant Medical and Mental Health History
| Total (N = 82) | |
|---|---|
| Medical diagnosis present | n (%) |
| Yes | 56 (68.29%) |
| No | 22 (26.83%) |
| History of mental health diagnosis1 | |
| None | 41 (50.00%) |
| Depression | 32 (39.02%) |
| Anxiety | 31 (37.80%) |
| PTSD | 11 (13.41%) |
| Bipolar | 1 (1.22%) |
| Panic Disorder | 1 (1.22%) |
| Current mental health d.agnosis | |
| None | 49 (59.76%) |
| Depression | 23 (28.05%) |
| Anxiety | 24 (29.27%) |
| PTSD | 10 (12.20%) |
| Bipolar | 2 (2.44%) |
| Panic Disorder | 1 (1.22%) |
| Current psychiatric medication | |
| Yes | 36 (43.90%) |
| No | 43 (52.44%) |
| Current pain medication | |
| Yes | 59 (71.95%) |
| No | 21 (25.61%) |
Participants checked all mental health diagnoses that applied, therefore co-morbidities are included in the frequencies for each diagnosis.
Patients were referred directly from their medical providers or indirectly through flyers and hospital-wide emails. Participants included in the study were: (1) adults (at least 18 years old), (2) experienced nonmalignant chronic pain for more than 3 months, (3) able to walk without assistance for 6 minutes, (4) had mobile device with Bluetooth (for Fitbit), (5) had no psychotropic or pain medications changes for past 3 months, and (6) medically cleared by a physician to participate. Participants were excluded if they had: (1) physical illness that is expected to decline in next 6 months, (2) serious psychiatric illness not currently treated or actively suicidal, (3) substance abuse disorder present and not treated, (4) engaged in mediation, yoga, or relaxation skills for more than 45 minutes per week over the past 6 months, (5) Fitbit regularly used over last 6 months, and (6) regularly exercise for more than 30 minutes each day.
Procedure
The Massachusetts General Hospital Institutional Review Board approved all study procedures. Participants were screened by phone for eligibility. Those who met inclusion criteria were provided information about the study and randomly assigned to one of two 10-week 90-minute groups that focus on increasing walking using time goals (GetActive, n = 41) or step-count reinforced via Fitbit (GetActiv-eFitbit, n = 41). The two programs are identical except one group received a Fitbit (GetActive-Fitbit), while the other group self-managed walking goals without the aid of Fitbit. After providing written informed consent and randomization, participants completed baseline assessments, including the self-report measures of emotional functioning, pain catastrophizing, pain resilience, and mindfulness behaviors described in the Measures section below (see Greenberg et al., 2020). One week following baseline assessments, participants started the 10-week program (90-minute weekly sessions). Participants repeated the assessments one-week post-intervention and were compensated $30 at each assessment.
Intervention
Details on the intervention development process and content have been published (Greenberg 2019;2020). Briefly, the 10-week GetActive and GetActive-Fitbit programs (90 minutes/week) were developed based on a conceptual theoretical model (Relaxation Response Resiliency Program (3RP); Park et al., 2013). The 3RP model is based on principles from stress management, cognitive-behavioral therapy, and positive psychology (Park et al., 2013). The 3RP aims to enhance adaptive responses to stress though increased awareness and engagement in strategies that help individuals move from the stress response to the relaxation response (Benson et al., 1974). Our GetActive and GetActive-Fitbit programs retain core skills of the 3RP and include new pain specific skills. Specifically, these programs teach mind-body skills focused on eliciting the relaxation response (e.g., diaphragmatic breathing, body scan) and mindfulness skills (guided meditations), pain-specific cognitive behavioral skills (e.g., behavioral activation techniques, adaptive restructuring of pain-related misconceptions such as catastrophizing and avoidance of fear), and physical restoration skills (e.g., quota-based pacing noncontingent on pain).
Measures
Emotional Functioning Outcomes
We assessed depression and anxiety with the PROMIS Short-Form Depression (v.1.0, 8b; Outcomes Measurement Information System, 2015) and Anxiety (v.10, 8a; Outcomes Measurement Information System, 2015) inventories. Depression items focus on negative mood and negative views of self and anxiety items address fear, hyperarousal, and somatic symptoms (Cella et al., 2010). Example items include, “In the past 7 days, I felt like a failure,” “In the past 7 days, I felt nervous.” Both measures are 8-items with responses ranging from 1 (Never) to 5 (Always), and higher scores indicating greater distress. Scores are reported on T-score metric (M = 50; SD = 10) centered on the general U.S. population (Reeve et al., 2007). T-scores of greater than 55 indicate clinically significant levels of distress (Reeve et al., 2007). Internal reliability for the PROMIS depression and anxiety scales in this sample were strong (Cronbach’s α = .95 – .96) and consistent with previously reported values (Cronbach’s α = .95; Marrie et al., 2018). Validity of PROMIS instruments has been confirmed in general and U.S. sample populations, including those with chronic pain (Amtmann et al., 2010; Pilkonis et al., 2011).
Pain Catastrophizing
We assessed pain catastrophizing with the Pain Catastrophizing Scale (PCS; Sullivan et al., 1995). It is a 13-item measure that focuses on helplessness, magnification, and rumination about pain. Participants responses range from 0 (Not at all) to 4 (All the time), with total scores ranging from 0 to 52 (higher scores mean greater pain catastrophizing). An example item includes, “I keep thinking about how badly I want the pain to stop.” Internal consistency was excellent within the sample (Cronbach’s α = .94), and in line with previous work (Cronbach’s α = .87) (Osman et al., 2000). PCS has been well-validated and is correlated with negative pain-related thoughts, greater emotional distress, and greater pain intensity (Sullivan et al., 1995).
Mindfulness
We measured mindfulness with the Cognitive and Affective Mindfulness Scale - Revised (CAMS-R; Feldman et al., 2007). This 12-item self-report inventory addresses the frequency of mindfulness behaviors (1 = Rarely/Not at all; 4 = Almost always). Scores range from 12 to 48 with higher scores indicate greater endorsement of mindfulness in everyday life (i.e., regulation of attention, orientation to present, awareness of experience, and acceptance/non-judgment towards experience). An example item includes, “I try to notice my thoughts without judging them.” Internal consistency within the sample was adequate (Cronbach’s α = .77), which is similar to current literature (Cronbach’s α = .74 – .77) (Schmertz et al., 2009). CAMS-R has strong validity as it has been highly correlated with existing measures of mindfulness as well as measures of distress, well-being, and emotion regulation (Feldman et al., 2007).
Pain Resilience
We used the Pain Resilience Scale (PRS; Slepian et al., 2016) to measure pain resilience, or the ability to maintain positive functioning despite physical or psychological adversity. This 14-item assessment asks participants to report responses on a scale of 0 (not at all) to 4 (to a great degree). Example items include, “I like to stay active,” or “I keep a hopeful attitude.” Scores are summed and range from 0 to 56, with higher scores indicating greater level of resilience to pain. The PRS is well-validated and exhibited strong internal reliability in the current sample (Cronbach’s α = .94), which is in line with previous work (Cronbach’s α = .72 – .94) (Slepian et al., 2016).
Data Analytic Plan
We analyzed data using multilevel linear modeling (MLM) through linear mixed-effects models (MIXED) procedure in SPSS, version 26.0 (IBM, 2017). Mixed-effects modeling accommodates interindividual differences in baseline levels of participants (i.e., random intercepts) and allows retention of all available data for analyses thereby increasing power (Chakraborty & Gu, 2009). Prior to modeling, we examined assumptions and descriptive statistics and mean centered all variables. The estimation method within the mixed-effects models were based on the restricted maximum-likelihood estimation. The models included two levels, where repeated assessments across time (Level 1; variables included time, hypothesized mediators) were nested within participants (Level 2).
Two separate multiple mediation models were run for each outcome (i.e., depression and anxiety). Each model examined the unique mediator role of changes in the three hypothesized mechanisms of change (pain catastrophizing, mindfulness, and pain resilience) for changes in either depression or anxiety between baseline and post-treatment. In each multiple mediation model, Time was the predictor, the three hypothesized mechanisms of change (in a simultaneous analytic model) were the mediators, and depression or anxiety symptoms were the outcome. Given that the focus was on identifying mechanisms of change across both groups, we adjusted for treatment group by including it as a fixed effect in the mediation models. We present findings for each step of mediation (path a, path b, path c, path c’, and path a*b). The indirect effect, from the predictor variable, through the hypothesized mediator, to the outcome variable, is the only requirement necessary to demonstrate mediation (Preacher & Hayes, 2008; Zhao et al., 2010).
First, changes in pain catastrophizing, mindfulness, and pain resilience were regressed on Time in separate models (path a). Then, either change in depression or change in anxiety (in separate models) were regressed on changes in pain catastrophizing, mindfulness, and pain resilience (as well as the treatment group variable) were simultaneously entered as fixed effects in the model (path b). We used Monte Carlo Method run by RMediation package (Tofighi & MacKinnon, 2011) to calculate the confidence interval (CI) of the indirect effects for each hypothesized mediator (path a*b). The 95% confidence intervals not containing zero indicate a significant indirect effect (i.e., mediation) (Preacher & Selig, 2012). The value of the direct effects (changes in depression or anxiety regressed on time) (path c), as well as the attenuation of the direct effects after inclusion of the hypothesized mediators (path c’) also were reported for descriptive purposes. Effect sizes of the significant indirect effects were calculated using “completely standardized indirect effects” (CSIE) with small, medium and large effect size estimates to be about .01, .09, .25, respectively (Preacher & Kelley, 2011).
Results
Preliminary Analyses
Descriptive Statistics
Table 3 displays descriptive statistics for outcome variables (i.e., depression and anxiety) and hypothesized mediators (i.e., pain catastrophizing, mindfulness, and pain resilience) across both timepoints. Baseline means of pain catastrophizing (M = 20.99, SD = 11.96), mindfulness (M = 31.21, SD = 6.74), and pain resilience (M = 35.10, SD = 10.06) fell into expected ranges based on measures and current literature among adults with chronic pain (e.g., Dong et al., 2020; Feldman et al., 2007; Slepian et al., 2016; Sullivan et al., 1995; Vowles et al., 2014). Forty-eight participants (58.54%) in our sample endorsed clinically significant levels of depression at baseline (T-scores > 55), and 53 participants (64.63%) endorsed clinically significant levels of anxiety at baseline (T scores > 55, which is in line with rates of emotional distress among chronic pain patients (Rayner et al., 2016). Separate bivariate correlations revealed that higher levels of depression and anxiety were associated with greater pain catastrophizing (r = .74, p < .001; r = .65, p < .001), less mindfulness (r = .74, p < .001; r = −.64, p < .001), and lower pain resilience (r = −.53, p < .001; r = −.48, p < .001), respectively.
Table 3.
Total Scores for Primary Variables
| Variable, Measure, and Possibl Range | M ± SD | Sample Range |
|---|---|---|
|
Emotional Distress (Outcomes) | ||
| Depression T-scores (PROMIS v1.0 8b) (37.1 – 81.1) | 54.07 ± 10.05 | 37.1 – 80.9 |
| Anxiety T-scores (PROMIS v1.0 8a) (37.1 – 83.1) | 55.07 ± 9.73 | 37.1 – 76.9 |
|
Hypothesized Mediators | ||
| Pain Catastrophizing Scale (0 – 52) | 17.33 ± 11.70 | 0 – 48 |
| Cognitive and Affective Mindfulness Scale, Revised (12 – 48) | 32.83 ± 6.83 | 19 – 48 |
| Pain Resilience Scale (0 – 56) | 37.33 ± 10.78 | 9 – 56 |
Note. Higher depression and anxiety scores indicate more symptoms. Higher pain catastrophizing scores indicate more catastrophizing. Higher pain resilience scores mean greater resilience to pain. Higher mindfulness scores indicate more engagement in mindful behaviors.
Multiple Mediation Analyses
Depression.
The a paths revealed that the three hypothesized mechanisms of change improved from baseline to post-intervention as reported in Greenberg et al., 2020. Pain catastrophizing significantly decreased, (b = −7.44, SE = 1.40, p < .001, CI = [−10.23, −4.65]), mindfulness significantly increased, (b = 3.35, SE = 0.73, p < .001, CI = [1.89, 4.80]), and pain resilience significantly increased, (b = 4.73, SE = 1.23, p < .001, CI = [2.28, 7.18]) from baseline to post-treatment among the sample overall. Regarding b Paths, when simultaneously included in one model, decreases in pain catastrophizing, b = 0.34, SE = 0.05, p < .001, increases in mindfulness, (b = −0.36, SE = 0.10, p < .001), and increases in pain resilience, (b = −0.16, SE = 0.06, p < .01) each accounted for a significant and unique variance in depression from baseline to post-treatment (see Table 4). Further, the path c (depressive symptoms regressed on time) was significant, (b = −3.54, SE = .91, p < .001, CI = [−5.36, −1.73]) indicating that depression decreased significantly from baseline to post-treatment (direct effects), which is in line with pervious work (Greenberg et al., 2020).
Table 4.
Mixed-Effects Models for Depression and Anxiety
|
Outcome: Depression |
b | Std. Error | t | p | Lower CI | Upper CI |
| Time | 0.84 | 0.77 | 1.09 | .279 | −0.69 | 2.36 |
| Group | 2.97 | 1.26 | 2.36 | .021 | 0.46 | 5.47 |
| Pain Catastrophizing | 0.34 | 0.05 | 6.52 | .000 | 0.24 | 0.45 |
| Mindfulness | −0.36 | 0.10 | −3.61 | .000 | −0.56 | −0.05 |
| Pain Resilience | −0.16 | 0.06 | −2.90 | .004 | −0.27 | −0.05 |
|
Outcome: Anxiety |
b | Std. Error | t | p | Lower CI | Upper CI |
| Time | 1.49 | 1.00 | 1.48 | .142 | −0.51 | 3.48 |
| Group | 2.54 | 1.31 | 1.94 | .056 | −0.07 | 5.15 |
| Pain Catastrophizing | 0.29 | 0.06 | 4.65 | .000 | 0.17 | 0.41 |
| Mindfulness | −0.45 | 0.11 | −3.86 | .000 | −0.67 | −0.22 |
| Pain Resilience | −0.10 | 0.07 | −1.58 | .116 | −0.23 | 0.03 |
Note. AIC = 979.96 for Depression mode; AIC 1026.80 for Anxiety model.
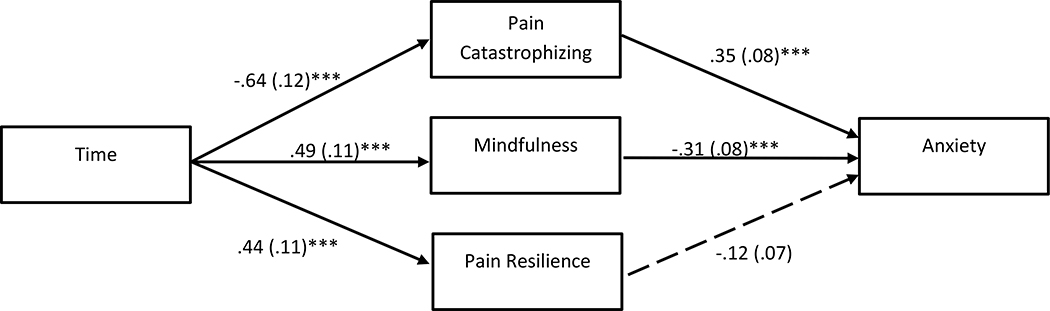
When hypothesized mechanisms of change were included in the model, the relationship between time and depression (path c’) was no longer significant, (b = 0.84, SE = 0.77, p = .279), indicating that hypothesized mechanisms fully mediated depression changes baseline to post-treatment. The indirect effects (path a*b) of time on improvements in depression through pain catastrophizing, (b = −2.53, SE = 0.61, CI = [−3.82, −1.43] (CSIE = −0.26)), mindfulness, (b = −1.21, SE = 0.43, CI = [−2.15, −0.46] (CSIE = −0.12), and pain resilience, (b = −0.76, SE = 0.35, CI = [−1.54, −1.66] (CSIE = −0.07)), were all significant (see Figure 1). In other words, time had the largest effect on depression through pain catastrophizing, followed by mindfulness, and then pain resilience.
Figure 1.
Mediation model testing the effect of hypothesized mechanisms of change on depression
Note. Paths specificy level-1 mixed linear modeling (MLM) equations with standardized values, *p < .05; ** p <.01; ***p <.001, path c’ = ß = −0.08 (.08). Solid lines represent significant pathways.
Anxiety.
The a paths are the same across mediation models for both outcomes (see above). In terms of b Paths, when simultaneously entered in one model, decreases in pain catastrophizing, (b = 0.29, SE = 0.06, p < .001), and increases in mindfulness, (b = −0.45, SE = 0.11, p < .000) significantly accounted for unique variance in anxiety from baseline to post-treatment (path b) (see Table 4). Path b for pain resilience was not significant, (b = −0.10, SE = 0.07, p = .116) (see Table 4). Further, the path c (anxiety symptoms regressed on time) was significant, (b = −2.56, SE = 1.04, p < .05, CI = [−4.64, −.49]) indicating a significant decrease from baseline to post-treatment (direct effects) as reported in Greenberg et al., 2020.
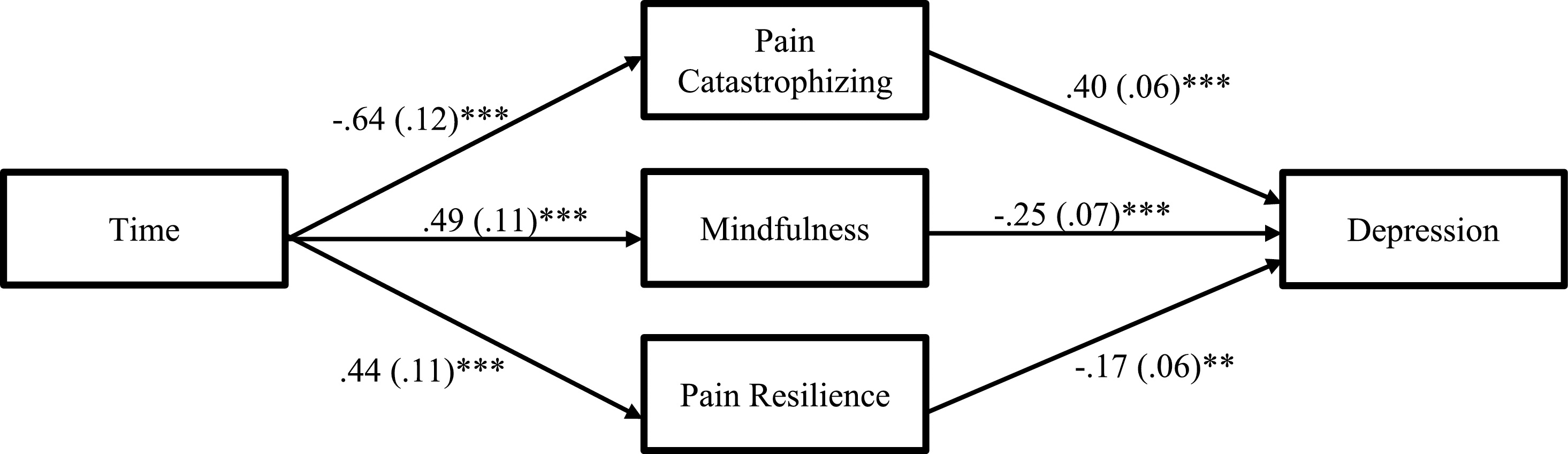
When the three hypothesized mechanisms of change were included in the model, the relationship between time and depression (path c’’) was no longer significant, (b = 1.49, SE = 1.00, p = .142), indicating that hypothesized mechanisms fully mediated anxiety changes baseline to post-treatment. The indirect effects (path a*b) of time on improvements in anxiety through pain catastrophizing, (b = −2.16, SE = 0.06, CI = [−3.45, −1.08] (CSIE = −0.22)), and mindfulness, (b = −1.51, SE = 0.50, CI = [−2.60, −0.65] (CSIE = −0.15)), were both significant (see Figure 2). There was no significant indirect effect of time on improvements in anxiety through pain resilience, (b = −0.47, SE = 0.36, CI = [−1.26, 0.17]). Similar to depression, time had the largest effect on anxiety through pain catastrophizing, followed by mindfulness.
Figure 2.
Mediation model testing the effect of hypothesized mechanisms of change on anxiety
Note. Paths specificy level-1 mixed linear modeling (MLM) equations with standardized values, *p < .05; ** p <.01; ***p <.001, path c’ = ß = 0.15 (.10). Solid lines represent significant pathways and dashed line represents non-significant pathway.
Discussion
Among psychosocial interventions for chronic pain, few have integrated conceptual models and examined multiple psychosocial processes that contribute to depression and anxiety outcomes (Barke et al., 2019; Meints & Edwards, 2018). We addressed this gap by examining the extent to which multiple mediators explained changes in emotional outcomes in response to a recently developed mind-body activity that incorporated elements of CBT, ACT, and mindfulness (Greenberg et al., 2019, 2020). We hypothesized that pain catastrophizing, mindfulness, and pain resilience would each uniquely explain improvements in depression and anxiety from baseline to post-treatment. Consistent with our hypothesis, pain catastrophizing, mindfulness, and pain resilience uniquely and fully mediated depression from baseline to post-treatment. Further, pain catastrophizing and mindfulness, but not pain resilience, uniquely and fully mediated anxiety from baseline to post-treatment. We discuss the implications of findings below for each hypothesized mediator of change.
Pain Catastrophizing and Emotional Outcomes
Decreases in pain catastrophizing explained a large portion of variance in depression and anxiety improvements (CSIEs = −0.26 and −.22) (Preacher & Kelley, 2011). In fact, pain catastrophizing explained more than twice the magnitude explained by mindfulness and more than three times the magnitude explained by pain resilience in emotional outcomes, when all included in the same models. Findings are consistent with previous literature that pain catastrophizing is a mediator of depression and associated with anxiety among people experiencing chronic pain (Dong et al., 2020; Wood et al., 2016). This analysis highlights the value of addressing negative cognitions surrounding pain and provides evidence for the fear-avoidance model given that pain catastrophizing can perpetuate depression (e.g., Crombez et al., 2012). Our mind-body activity program directly addressed the disability spiral by restructuring of pain-related misconceptions or pain-related thoughts, which may explain why pain catastrophizing was the largest mediator of change in emotional outcomes. In other words, restructuring beliefs about pain seems to serve as a useful mechanism for developing a more adaptive perspective on pain, which may help increase engagement in activities and thereby decrease anxious and depressive symptoms (Cheng et al., 2018). Although restructuring cognitions about pain, appeared to be an effective technique in our program, other researchers have identified psychological flexibility as a potential tool to decrease negative pain-related thoughts, suggesting that other interventions techniques also may be useful to address pain catastrophizing (Vowles & McCracken, 2008).
Mindfulness and Emotional Outcomes
Increases in mindfulness explained a medium to large portion of the variance in depression and anxiety (CSIEs = −.12 and −0.15) improvements from baseline to post-treatment (Preacher & Kelley, 2011). These findings are consistent with reports that mindfulness practice has been effective for improving emotional functioning patients with chronic pain (e.g., Baer, 2003; Curtin & Norris, 2017). The present results, which suggest that mindfulness is an important mechanism of change, address limitations of previous studies which have overlooked it as a process variable in emotional function outcomes (McCracken & Vowles, 2014; Shen et al., 2020). The fact that mindfulness explained unique change in emotional outcomes, above and beyond pain catastrophizing, emphasizes its value for chronic pain interventions. Mindfulness has been negatively associated with ruminative anxiety and may disrupt the cycle of chronic pain and emotional distress by decreasing negative pain-related cognitions (Curtin & Norris, 2017). Mindfulness also has been associated with neurobiological changes, lower perceived stress, fewer appraisals of everyday events as hassles, less self-blame, and less escape-avoidance behaviors, which can decrease depressive symptoms (Shen et al., 2020; Moskowitz et al., 2015). Within our program, relaxation response skills (e.g., mindfulness mediation, body scan) likely helped participants increase awareness of their internal experiences (e.g., negative pain-related thoughts, body sensations), thereby enhancing adaptive coping and decreasing emotional distress.
Pain Resilience and Emotional Outcomes
Changes in pain resilience explained a small to medium portion of the variance in depression (CSIE = −0.07), but not variance in anxiety following participation in our mind-body activity program (Preacher & Kelley, 2011). Findings regarding pain resilience and depression confirm previous reports that resilience helps to attenuate depression and maintain physical activity (Akerbolm et al., 2015; Radat et al., 2010). Willingness to engage in activities with pain may be more relevant for improving mood, but not anxiety, which is consistent with literature on the value of behavioral activation for mood among patients with chronic pain (Kim et al., 2017). It is possible that items on the Pain Resilience Scale (e.g., “I still find joy in my life”) are more sensitive to mood.
It is important to note that the significant effect for pain resilience on depression was small when compared with contributions of pain catastrophizing and mindfulness. This finding may be because the program indirectly targeted resilience by focusing on physical activity, mind-body skills, and correcting negative pain-related thoughts; therefore, less change was evident in pain resilience. Future iterations of this intervention or adapted interventions could consider the inclusion of acceptance and/or positive psychology skills which may more directly address pain resilience (Dong et al., 2020). Further, pain catastrophizing and mindfulness may have shared variance with pain resilience, making it more conceptually difficult to tease apart their unique contributions.
Strengths and Limitations
The current analysis has several strengths. First, the present study utilized a rigorous methodological design in the implementation of a novel pilot mind-body activity RCT. Our program incorporated strong conceptual foundations (e.g., biopsychosocial 3RP model, fear-avoidance-model, CBT, ACT), well-established measures, and randomization. This methodology sets the stage to effectively assess mechanisms of change, which is an important step prior to RCT efficacy testing (Nielsen et al., 2018). Second, we examined multiple mediators simultaneously to extend the current literature regarding psychosocial processes that may explain emotional outcomes. Few researchers have examined more than two mediators to understand emotional outcomes among patients with chronic pain, despite the evidence that enhanced outcomes involved multiple processes (Dong et al., 2020; Wongpakaran et al., 2016). To our knowledge, this is the first study to merge several evidence-based conceptual models and test multiple mediators in the context of a novel intervention. Each of our hypothesized mediators represented core processes in the conceptual underpinnings of this intervention (i.e., negative cognitions about pain, nonjudgmental awareness of pain-related beliefs, and willingness to function with pain). In addition, our analytical approach allowed us to: (1) assess unique explanatory role of multiple psychosocial processes for depression and anxiety; (2) adjust for individual differences at baseline; (3) control for group effects; and (4) include all available data to increase power.
Study limitations also should be considered. First, the study did not include a control condition and, therefore, data between two treatment groups (GetActive, GetActive-Fitbit) were merged to determine processes that may explain outcomes to inform to future efficacy testing (Aklin et al., 2020). Without a control condition, we cannot rule out that participants’ improvement in processes and outcomes may have been a function of time or other factors. Second, although the analytical approach was the most appropriate for the data, mediation analyses were limited by two time points and a small sample size. Further, causality and directionality cannot be assumed without more time points and control conditions. Previous literature has highlighted a reciprocal relationship between pain catastrophizing and depression, which emphasizes the complex nature of directionality and should be addressed in future studies with more timepoints and control groups (Wongpakaran et al., 2016). Future studies can address these limitations by including more timepoints, control conditions, and larger samples.
Clinical Implications and Future Directions
This work provides evidence for treatment mechanisms that are important to consider in the development and implementation of psychosocial interventions targeting emotional distress among patients with chronic pain. Pain catastrophizing, mindfulness, and pain resilience mediated improvements in depression and/or anxiety, which highlights that these processes are important to target in future iterations of our mind-body activity program. Our finding that pain catastrophizing exhibited a large effect on emotional outcomes suggests that patients with chronic pain would benefit from addressing negative pain-related thoughts and pain misconceptions in psychotherapy. The result that mindfulness explained medium to large effects on emotional outcomes emphasizes that clinicians should consider incorporating mindfulness and/or mind-body skills into treatment to enhance functioning. Future RCT trials of this intervention should attempt to replicate and test directionality of these mechanisms of change with a larger sample, increased power, and including a control condition.
The findings that multiple psychological processes – pain catastrophizing, mindfulness, and pain resilience –explain unique portions and different magnitudes of variance in emotional outcomes highlight the value of targeting all processes given that they fully accounted for changes in depression and anxiety across time. Interventions should consider utilizing several techniques to address negative pain-related cognitions, increase nonjudgmental awareness, and increase willingness or acceptance of pain to enhance functioning. Further work examining how these processes may interact is warranted. This would help clarify how these skills should be presented and taught to patients in psychosocial interventions. Merging mechanisms of change across a variety of psychosocial interventions (e.g., ACT, mindfulness, CBT) may reveal the most effective treatments for chronic pain patients. Future interventions that consider the value of multiple theoretical models might elucidate psychosocial processes involved in managing emotional distress associated with chronic pain.
Conclusions
Few chronic pain interventions include depression and anxiety as outcomes and assess multiple mediators of change within interventions. Our work highlights core elements of treatment that can enhance emotional functioning. Pain catastrophizing and mindfulness helped to explain improvements in depression and anxiety following a pilot mind-body activity RCT for chronic pain. Pain resilience contributed to a small portion of change in depression and did not contribute to anxiety. Within this program, negative pain-related beliefs and mind-body skills likely contributed to improved pain catastrophizing and mindfulness and better emotional outcomes. Future iterations of our program could include techniques that target resilience (e.g., acceptance) to further enhance emotional functioning. Next steps include testing the efficacy of a fully powered RCT of determine core mechanisms of change that improve functioning among patients with chronic pain. Current findings provide valuable information to clinicians and researchers as to important processes – pain catastrophizing and mindfulness – to consider for treatment and intervention development.
Highlights.
Need to understand mechanisms that address depression and anxiety in chronic pain interventions
Pain catastrophizing and mindfulness mediated depression and anxiety improvements
Pain resilience mediated depression improvements, but not anxiety
Mechanisms of change inform efficacy trials of this mind-body activity intervention
Funding Acknowledgements
This study was funded by an R34 grant from the National Center for Complementary and Integrative Health (NCCIH; IR34AT009356-01A1) to the senior author and K23 grant from NCCIH (1K23AT01065301A1) to the fourth author.
Footnotes
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aklin WM, Stoeckel LE, Green PA, Keller C, King JW, Nielsen L, & Hunter C (2020). Commentary: National Institutes of Health (NIH) Science of Behavior Change (SOBC). Health Psychology Review, 14(1), 193–198. [DOI] [PubMed] [Google Scholar]
- Amtmann D, Cook KF, Jensen MP, Chen W-H, Choi S, Revicki D, Cella D, Rothrock N, Keefe F, Callahan L, & Lai J(2010). Development of a PROMIS item bank to measure pain interference. Pain, 150(1), 173–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baer RA (2003). Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology: Science and Practice, 10(2), 125–143. [Google Scholar]
- Barke A, Koechlin H, Korwisi B, & Locher C (2020). Emotional distress: Specifying a neglected part of chronic pain. European Journal of Pain, 24(3), 477–480. [DOI] [PubMed] [Google Scholar]
- Benson H, Beary JF, & Carol MP (1974). The relaxation response. Psychiatry, 37(1), 37–46. [DOI] [PubMed] [Google Scholar]
- Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, Amtmann D, Bode R, Buysse D, Choi S, Cook K, DeVellis R, DeWalt D, Fries JF., Gershon R, Hahn EA, Lai J, Pilkonis P, Revicki D, Rose M, Weinfurt K, & Hays R (2010). The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. Journal of Clinical Epidemiology, 63(11), 1179–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakraborty H, & Gu H (2009). A mixed model approach for intent-to-treat analysis in longitudinal clinical trials with missing values. RTI Press Publication No. MR-0009–0903. Research Triangle Park, NC: RTI Press. 10.3768/rtipress.2009.mr.0009.0903 [DOI] [PubMed] [Google Scholar]
- Cheng S-T, Leung CM, Chan KL, Chen PP, Chow YF, Chung JW, Law AC, Lee J.s., Leung EM, & Tam CW (2018). The relationship of self-efficacy to catastrophizing and depressive symptoms in community-dwelling older adults with chronic pain: a moderated mediation model. PloS One, 13(9), e0203964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crombez G, Eccleston C, Van Damme S, Vlaeyen JW, & Karoly P (2012). Fear-avoidance model of chronic pain: the next generation. The Clinical Journal of Pain, 28(6), 475–483. [DOI] [PubMed] [Google Scholar]
- Curtin KB, & Norris D (2017). The relationship between chronic musculoskeletal pain, anxiety and mindfulness: Adjustments to the Fear-Avoidance Model of Chronic Pain. Scandinavian Journal of Pain, 17, 156–166. [DOI] [PubMed] [Google Scholar]
- Domenichiello AF, & Ramsden CE (2019). The silent epidemic of chronic pain in older adults. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 93, 284–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong H-J, Gerdle B, Bernfort L, Levin L-Å, & Dragioti E (2020). Pain Catastrophizing in Older Adults with Chronic Pain: The Mediator Effect of Mood Using a Path Analysis Approach. Journal of Clinical Medicine, 9(7), 2073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldman G, Hayes A, Kumar S, Greeson J, & Laurenceau J-P (2007). Mindfulness and emotion regulation: The development and initial validation of the Cognitive and Affective Mindfulness Scale-Revised (CAMS-R). Journal of Psychopathology and Behavioral Assessment, 29(3), 177. [Google Scholar]
- Fredrickson BL (2001). The role of positive emotions in positive psychology: The broaden-and-build theory of positive emotions. American Psychologist, 56(3), 218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg J, Lin A, Zale EL, Kulich RJ, James P, Millstein RA, Shapiro H, Schatman ME, Edwards RR, & Vranceanu AM (2019). Development and early feasibility testing of a mind-body physical activity program for patients with heterogeneous chronic pain; the GetActive study. Journal of Pain Research, 12, 3279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg J, Popok PJ, Lin A, Kulich RJ, James P, Macklin EA, Millstein RA, Edwards RR, & Vranceanu AM (2020). A Mind-Body Physical Activity Program for Chronic Pain With or Without a Digital Monitoring Device: Proof-of-Concept Feasibility Randomized Controlled Trial. JMIR Formative Research, 4(6), e18703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grabovac AD, Lau MA, & Willett BR (2011). Mechanisms of mindfulness: A Buddhist psychological model. Mindfulness, 2(3), 154–166. \ [Google Scholar]
- Hassett AL, & Finan PH (2016). The role of resilience in the clinical management of chronic pain. Current Pain and Headache Reports, 20(6), 39. [DOI] [PubMed] [Google Scholar]
- IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp. [Google Scholar]
- Institute of Medicine. (2011). Relieving pain in America: A blueprint for transforming prevention, care, education, and research. Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- Kim EH, Crouch TB, & Olatunji BO (2017). Adaptation of behavioral activation in the treatment of chronic pain. Psychotherapy, 54(3), 237. [DOI] [PubMed] [Google Scholar]
- Marrie RA, Zhang L, Lix LM, Graff LA, Walker JR, Fisk JD, Patten SB, Hitchon CA, Bolton JM, Sareen J, El-Gabalawy R, Mariott JJ,. & Bernstein CN (2018). The validity and reliability of screening measures for depression and anxiety disorders in multiple sclerosis. Multiple Sclerosis and Related Disorders, 20, 9–15. [DOI] [PubMed] [Google Scholar]
- McCracken LM, & Vowles KE (2014). Acceptance and commitment therapy and mindfulness for chronic pain: Model, process, and progress. American Psychologist, 69(2), 178. [DOI] [PubMed] [Google Scholar]
- McCracken LM, Carson JW, Eccleston C, & Keefe FJ (2004). Acceptance and change in the context of chronic pain. Pain, 109(1), 4–7. [DOI] [PubMed] [Google Scholar]
- Meints SM, & Edwards RR (2018). Evaluating psychosocial contributions to chronic pain outcomes. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 87, 168–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moskowitz JT, Duncan LG, Moran PJ, Acree M, Epel ES, Kemeny ME, Hecht FM, & Folkman S (2015). Dispositional mindfulness in people with HIV: associations with psychological and physical health. Personality and Individual Differences, 86, 88–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen L, Riddle M, King JW, Aklin WM, Chen W, Clark D, Collier E, Czajkowski S, Esposito L, Ferrer R, Green P, Hunter C, Kehll K, King R, Onken L, Simmons JM, Stoeckel L, Stoney C, Tully L, & Weber W (2018). The NIH Science of Behavior Change Program: Transforming the science through a focus on mechanisms of change. Behaviour Research and Therapy, 101, 3–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Outcomes Measurement Information System. 2015. A Brief Guide to the PROMIS Anxiety Instruments URL: http://www.healthmeasures.net/images/PROMIS/manuals/PROMIS_Anxiety_Scoring_Manual.pdf [accessed 2018-10-29]
- Outcomes Measurement Information System. 2015. A Brief Guide to the PROMIS Anxiety Instruments URL: http://www.healthmeasures.net/images/PROMIS/manuals/PROMIS_Anxiety_Scoring_Manual.pdf [accessed 2018-10-29]
- Osman A, Barrios FX, Gutierrez PM, Kopper BA, Merrifield T, & Grittmann L (2000). The Pain Catastrophizing Scale: further psychometric evaluation with adult samples. Journal of Behavioral Medicine, 23(4), 351–365. [DOI] [PubMed] [Google Scholar]
- Park ER, Traeger L, Vranceanu A-M, Scult M, Lerner JA, Benson H, Denninger J, & Fricchione GL (2013). The development of a patient-centered program based on the relaxation response: the Relaxation Response Resiliency Program (3RP). Psychosomatics, 54(2), 165–174. [DOI] [PubMed] [Google Scholar]
- Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, Cella D, & Group PC (2011). Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS®): depression, anxiety, and anger. Assessment, 18(3), 263–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radat F, & Koleck M (2011). Pain and depression: cognitive and behavioural mediators of a frequent association. L’Encephale, 37(3), 172–179. [DOI] [PubMed] [Google Scholar]
- Rayner L, Hotopf M, Petkova H, Matcham F, Simpson A, & McCracken LM (2016). Depression in patients with chronic pain attending a specialised pain treatment centre: prevalence and impact on health care costs. Pain, 157(7), 1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reeve BB, Hays RD, Bjorner JB, Cook KF, Crane PK, Teresi JA., Thissen D, Revicki DA, Weiss DJ, Hambleton RK, Liu H, Gershon R, Reise SP, Lai J, & Cella D (2007). Psychometric evaluation and calibration of health-related quality of life item banks: plans for the Patient-Reported Outcomes Measurement Information System (PROMIS). Medical Care, S22–S31. [DOI] [PubMed] [Google Scholar]
- Schmertz SK, Anderson PL, & Robins DL (2009). The relation between self-report mindfulness and performance on tasks of sustained attention. Journal of Psychopathology and Behavioral Assessment, 31(1), 60–66. [Google Scholar]
- Shen H, Chen M, & Cui D (2020). Biological mechanism study of meditation and its application in mental disorders. General Psychiatry, 33(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slepian PM, Ankawi B, Himawan LK, & France CR (2016). Development and initial validation of the pain resilience scale. The Journal of Pain, 17(4), 462–472. [DOI] [PubMed] [Google Scholar]
- Sullivan MJ, Bishop SR, & Pivik J (1995). The pain catastrophizing scale: Development and validation. Psychological Assessment, 7(4), 524. [Google Scholar]
- Tofighi D, & MacKinnon DP (2011). RMediation: an R package for mediation analysis confidence intervals. Behavior Research Methods, 43(3), 692–700. doi: 10.3758/s13428-011-0076-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trompetter HR, Bohlmeijer ET, Fox JP, & Schreurs KM (2015). Psychological flexibility and catastrophizing as associated change mechanisms during online Acceptance & Commitment Therapy for chronic pain. Behaviour Research and Therapy, 74, 50–59. [DOI] [PubMed] [Google Scholar]
- Tseli E, Boersma K, Stålnacke BM, Enthoven P, Gerdle B, Äng BO, & Grooten WJ (2019). Prognostic factors for physical functioning after multidisciplinary rehabilitation in patients with chronic musculoskeletal pain: A systematic review and meta-analysis. The Clinical Journal of Pain, 35(2), 148–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turk DC, & Okifuji A (2002). Psychological factors in chronic pain: Evolution and revolution. Journal of Consulting and Clinical Psychology, 70(3), 678. [DOI] [PubMed] [Google Scholar]
- Vlaeyen JW, & Linton SJ (2012). Fear-avoidance model of chronic musculoskeletal pain: 12 years on. Pain, 153(6), 1144–1147. [DOI] [PubMed] [Google Scholar]
- Vowles KE, Witkiewitz K, Sowden G, & Ashworth J (2014). Acceptance and commitment therapy for chronic pain: evidence of mediation and clinically significant change following an abbreviated interdisciplinary program of rehabilitation. The Journal of Pain, 15(1), 101–113. [DOI] [PubMed] [Google Scholar]
- Wongpakaran T, Wongpakaran N, Tanchakvaranont S, Bookkamana P, Pinyopornpanish M, Wannarit K, Satthapisit S, Nakawiro D, Hiranyatheb T, & Thongpibul K (2016). Depression and pain: testing of serial multiple mediators. Neuropsychiatric Disease and Treatment, 12, 1849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood BM, Nicholas MK, Blyth F, Asghari A, & Gibson S (2016). The mediating role of catastrophizing in the relationship between pain intensity and depressed mood in older adults with persistent pain: A longitudinal analysis. Scandinavian Journal of Pain, 11, 157–162. [DOI] [PubMed] [Google Scholar]
- Zhao X, Lynch JG Jr, & Chen Q (2010). Reconsidering Baron and Kenny: Myths and truths about mediation analysis. Journal of Consumer Research, 37(2), 197–206. [Google Scholar]