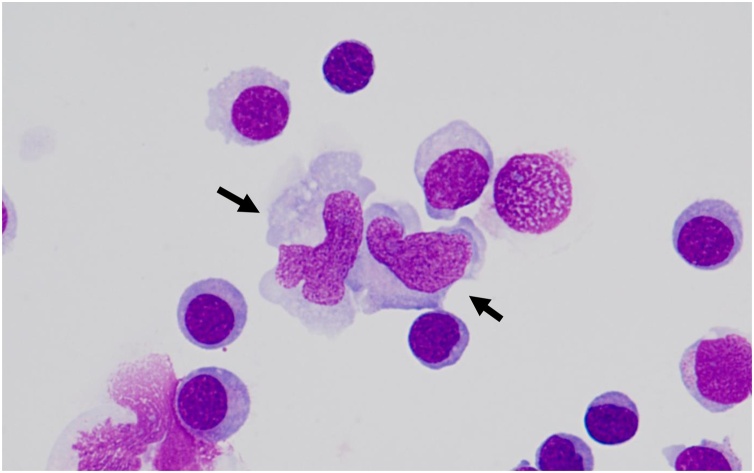
A 62-year-old man presented with a 5-day history of headache and nausea. He underwent an unrelated allogeneic stem cell transplantation (allo-SCT) for de novo blast phase chronic myeloid leukemia that achieved and maintained complete molecular response two years ago. He had been taking low-dose tacrolimus and prednisolone for chronic graft-versus-host disease and oral acyclovir at 200 mg daily for herpes virus prophylaxis. On admission, the patient was fully conscious and had no nuchal rigidity or neurological deficits. Brain magnetic resonance imaging without contrast medium showed normal findings. Cytology of cerebrospinal fluid (CSF) revealed a hypercellularity with pleocytosis. Some of these cells in the CSF were large monocytes harboring footprint-shaped nucleus, also known as “Mollaret cells” (May–Grünwald–Giemsa stain, × 1,000 objective, black arrows) [1] (Fig. 1). Comprehensive viral testing was performed and detected the herpes simplex virus-2 (HSV-2) DNA in the CSF specimen. Therefore, he was diagnosed as HSV-2 meningitis after an allo-SCT. His symptoms rapidly improved after an intravenous administration of 15 mg/kg acyclovir. Thereafter, he has no recurrent meningitis within two years. Recurrent meningitis associated with HSV-2 is also known as Mollaret’s meningitis in the narrow sense, and the presence of Mollaret’s cells is the hallmark characteristic of the early-stage disease [2].
Fig. 1.
Large monocytes harboring footprint-shaped nucleus.
Funding
This work was supported by JSPS KAKENHI Grant Number 19K17868 from the Ministry of Education, Culture, Sports, Science, and Technology of Japan.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Ethical approval
No ethical approval was required for this publication.
Author contribution
S. Tabata and T.M. planned this study and wrote this manuscript. T.H. and R.I. were involved with the treatment and the diagnostic procedure. S. Tamura and T.S. supervised the study.
Declaration of Competing Interest
The authors report no declarations of interest.
Acknowledgement
The authors would like to thank Enago (www.enago.jp) for the English language review.
References
- 1.Chan T.Y., Parwani A.V., Levi A.W., Ali S.Z. Mollaret’s meningitis: cytopathologic analysis of fourteen cases. Diagn Cytopathol. 2003;28:227–231. doi: 10.1002/dc.10261. [DOI] [PubMed] [Google Scholar]
- 2.Shalabi M., Whitley R.J. Recurrent benign lymphocytic meningitis. Clin Infect Dis. 2006;43:1194–1197. doi: 10.1086/508281. [DOI] [PubMed] [Google Scholar]