Abstract
Non-homeostatic, or hedonic eating can be detrimental to weight control efforts, yet the effect of exercise on hedonic eating is unclear.
Purpose:
This efficacy trial tests the hypothesis that exercise training favorably impacts hedonic eating (i.e., overeating, stress-induced overeating, disinhibited eating, eating when tempted), in a sample of women who are overweight or obese.
Methods:
Participants were inactive at baseline, self-identified as ‘stress eaters’, and were randomized to 12 weeks of moderate-intensity exercise training (EX; combination of supervised and objectively-confirmed unsupervised sessions) or to a no-exercise control condition (CON). EX participants were given an exercise goal of 200 min/week. No dietary instructions or weight control strategies were provided. Assessments occurred at baseline and 12 weeks. Overeating episodes, stress-induced overeating, and dietary temptations were measured over 14 days at each assessment using ecological momentary assessment (EMA). Disinhibition and dietary restraint were assessed via questionnaire.
Results:
49 participants (age: 40.4±10.8 years, BMI: 32.4±4.1 kg/m2) enrolled, and 39 completed this study. Adherence to the exercise intervention was high (99.4% of all prescribed exercise). At week 12, the proportion of eating episodes that were characterized as overeating episodes was lower in EX vs. CON (21.98% in EX vs. 26.62% in control; p=.001). Disinhibition decreased in EX, but not CON (p=.02), and was driven by internal factors. There was a trend, such that CON was more likely to give into dietary temptations (p=0.08). Stress-induced overeating was low, and did not differ between conditions (p=0.61).
Conclusion:
Exercise training reduced the likelihood of overeating, and eating in response to internal cues, in women who self-identified as stress eaters. This may be one pathway by which exercise impacts body weight.
Keywords: Weight control, Overeating, Exercise, Eating behaviors, physical activity, ecological momentary assessment (EMA)
1. INTRODUCTION
Eating behaviors are controlled by both homeostatic (i.e., eating to restore energy balance) and hedonic pathways (i.e., reward-based and pleasure seeking) (1). Hedonic regulation of food intake often overrides homeostatic cues (2) and can be detrimental for weight control (3, 4). Further, stress, negative emotions and aversive mood states can also lead to overeating and excess energy intake, hindering weight control efforts (5, 6). Currently, it is unclear whether exercise can buffer against these effects.
Exposure to highly palatable foods, or thoughts of these foods, can produce strong emotional states (e.g., feelings of deprivation if the food is not eaten, internal discomfort, and cravings and urges to eat) (1, 7–10). Conversely, the consumption of highly palatable foods can induce feelings of pleasure and reward, making this a common coping mechanism when experiencing food cravings and aversive mood states (1, 11–13). Further, stress and negative emotions can intensify the hedonic drive to eat and result in overeating or disinhibited eating (i.e., tendency to overeat in response to cognitive or emotional cues). Increased food cravings, an inability to resist dietary temptations, disinhibited eating, and frequent overeating of this nature could contribute to weight gain over time. Thus, from a clinical perspective, it is important to investigate factors which could help combat these aversive mood states and hedonic urges to eat.
One factor which may help buffer against the effect of stress and negative mood states on overeating is exercise. Previous research indicates that high levels of exercise are associated with less weight gain over time (14), yet these mechanisms are poorly understood. The traditional view is that exercise is important from a weight control perspective given that it results in an increase in energy expenditure. While this is certainly one pathway through which exercise can directly influence body weight, it is also possible that exercise indirectly impacts body weight through its effect on psychological or behavioral constructs implicated in eating behaviors. For example, in the addiction field, exercise has been shown to improve abstinence rates and cravings for drugs and alcohol via mechanisms unrelated to energy expenditure (15–17). These psychosocial mechanisms warrant further consideration in the weight control field.
Prior studies, including randomized trials, indicate that exercise training or regular physical activity improves mood (18, 19), reduces anxiety, depression, and stress (18, 20), (21–24), and improves one’s ability to cope with stress (21). A separate body of literature suggests that greater stress, exposure to stress, or daily hassles is associated with unhealthy food choices, increased snacking, overeating, wanting for unhealthy foods, and weight gain over time (25–29)(30, 31). However, despite findings that stress and anxiety lead to overeating and poor dietary choices (28, 30–32), and a separate body of literature demonstrating that exercise reduces stress and anxiety (18, 20, 21), it is unclear whether exercise training can reduce dietary temptations, food cravings, and overeating episodes. A greater understanding of the effect of exercise on disinhibited eating and overeating may be particularly important for individuals with overweight or obesity, as they are more prone to hedonic-driven eating (30).
This randomized trial uses ecological momentary assessment (EMA) to test the primary hypotheses that relative to a no exercise control condition, 12 weeks of moderate-intensity exercise will reduce overeating episodes and stress-induced overeating among a sample of inactive women, with overweight or obesity, who endorsed stress eating. Further, secondary hypotheses were that exercise training would reduce food cravings, dietary temptations, and dietary disinhibition, and improve eating-related self-control (i.e., the ability to resist eating the food when exposed to a dietary temptation).
2. METHODS
2.1. Participants
To be eligible for this study, individuals needed to be female, between the ages of 18-60, have a BMI of 25-40 kg/m2, own a smartphone, and be inactive, defined as self-reported moderate-intensity exercise <60 minutes/week over the past 6 months. Further, participants had to endorse some degree of stress-induced overeating, and thus were only eligible if they reported eating ‘more than usual’ or ‘much more than usual’ when they experienced moderate or extreme levels of stress, as assessed via phone screen. This study was limited to women, given that stress-induced eating is more likely to occur in women, compared to men (33, 34). Individuals with a limited ability to exercise, recent weight loss, current enrollment in a weight loss program, recent pregnancy, history of heart disease or diabetes, recent cancer diagnosis or treatment, those taking beta-blockers, or those with other factors that would likely limit their ability to participate in the study (e.g., severe psychiatric conditions, terminal illness, orthopedic conditions that would limit exercise, and plans to move out of the area during the study period) were excluded from this study. Further, prior to randomization, participants had to be willing to get a gym membership (for which they were reimbursed), if they did not already have one before enrolling in the study.
2.2. Study design
All eligible participants were instructed to wear an objective physical activity monitor (Sensewear Armband, Body Media, Inc, Pittsburgh, PA) for 14 days, while simultaneously completing the EMA protocol described below. To be eligible, participants were required to demonstrate compliance to wearing the armband (≥5 days and ≥10 hours/day) and completing the EMA surveys (≥80% of all surveys). Assessments of height, weight, fitness, and various questionnaire measures were also completed at baseline. Participants were matched on BMI and randomized to a 12-week exercise condition (EX) or delayed exercise condition, which served as the control comparison group (CON). Neither EX nor CON participants were provided with any instructions regarding their diet. All baseline measures were also completed at 12 weeks. Informed consent was obtained from all participants prior to enrollment and all study procedures were approved by The Miriam Hospital’s Institutional Review Board.
2.3. Treatment conditions
2.3.1. Exercise condition.
Participants randomized to EX received a 12-week exercise training program which consisted of both supervised exercise sessions and home-based (unsupervised) exercise. The exercise prescription started at 100 minutes/week of moderate-intensity exercise (Week 1) and quickly progressed to 200 minutes/week (Weeks 3-12). Given that this was an efficacy trial, it was important that participants achieved levels of exercise consistent with national guidelines (≥150 min/week of moderate-intensity exercise); thus an exercise prescription above this recommended threshold was chosen to better ensure this magnitude of exercise was achieved, even if participants fell short of the prescribed exercise goal. During the first 4 weeks, participants attended two supervised exercise visits/week (Weeks 1-2: 30 min/visit; Weeks 3-4: 40 min/visit) and during weeks 5-12, they attended one supervised exercise visit per week (50 minutes/visit). Supervised sessions were performed on an individual basis (i.e., not group-based). During these sessions, participants had the option to use the treadmill or elliptical trainer. They also wore a Sensewear armband (which provides minute-by-minute MET values) and HR was assessed throughout the exercise session to ensure that they remained within the targeted heart rate range (64-75% of age-predicted maximal heart rate). The remaining exercise was performed on their own, and participants kept activity logs and wore an armband to assess exercise duration and intensity during all home-based exercise sessions. Participants could choose any mode of exercise, as long as it was similar in intensity as that practiced during supervised sessions and they were encouraged to spread the exercise over 4-5 days each week. Moreover, they were not provided with any behavioral strategies for increasing exercise and were simply instructed to exercise at an intensity that was a similar intensity to that of supervised exercise sessions. They could use heart rate or the ratings of perceived exertion scale to gauge exercise intensity on their own. Self-reported exercise minutes and intensity were verified weekly using the armband data and participants were compensated for achieving their prescribed exercise minute goal. They were provided $10 in cash for each week that they met their goal and were given a $50 bonus (in the form of a gift card) if they averaged ≥180 min/week over the 12-week period as verified via the armband. To further facilitate achievement of the exercise minute goal, participants were required to have a gym membership and were reimbursed up to $40/month for this expense.
2.3.2. Delayed exercise condition:
Participants randomized to the delayed exercise condition (i.e., control condition; CON) were instructed not to change their exercise habits over the 12-week period. However, to assist with retention, they were provided with the option to participate in the exercise intervention following the completion of their 12-week assessment visit. Compensation was only provided for assessment measures during the initial 12-week period, but CON participants were compensated in a similar manner as EX participants if they choose to participate in the exercise intervention following completion of the 12-week assessment visit.
2.4. Assessment measures
2.4.1. Height, weight and fitness.
Height was assessed at baseline and measured to the nearest millimeter using a stadiometer. Weight was assessed at baseline and 12 weeks, and measured to the nearest 0.1kg using a digital scale. A graded exercise test (GXT) to 75% of age-predicted maximal heart rate (220-age) was conducted at baseline and 12 weeks. Participants walked on a treadmill at 3.0 mph and the incline of the treadmill increased every three minutes until the subject’s HR reached 75% of their age-predicted maximum. Total time on the treadmill was used to compare changes in fitness between treatment conditions.
2.4.2. Objective assessment of physical activity.
All participants wore a Sensewear armband for 14 consecutive days at baseline and 12 weeks (to coincide with the EMA monitoring period). This device was worn on the upper arm and has been shown to provide valid and reliable estimates of exercise intensity and energy expenditure via a unique combination of sensors (accelerometer, galvanic skin response, heat flux, and skin temperature)(35, 36). Moderate-to-vigorous PA (MVPA) bouts were calculated as follows: ≥10 minutes of activity ≥3 metabolic equivalents. As a fidelity check, treatment groups were compared on 12-week changes in bout-related MVPA.
2.4.3. EMA protocol:
Ecological momentary assessment was used to capture feeling states and eating behaviors in real time, overcoming known biases related to retrospective self-report and improving ecological validity (37). All participants were asked to respond to surveys via their smartphone for 14 days at baseline and 14 days at the end of the 12-week period. Surveys were in the form of 5 semi-random prompts (i.e., occurring every 2-3 hours) delivered between 8:00am and 10:00pm via text message. Participants were instructed to respond to the survey as soon as possible upon receiving the text message, but they had 45 minutes to respond before it was considered a missed survey. At each prompt, participants were asked to respond to questions which asked about their stress and anxiety levels, dietary temptations, and eating and overeating episodes (see Table 1 for list of questions). This EMA protocol followed standard procedures for assessing a combination of discrete (e.g., overeating) and continuous experiences (e.g., stress, anxiety, dietary temptation, etc.) by using prompts delivered throughout waking hours to ensure coverage of overeating, while sampling the cognitive and emotional factors. Semi-random prompts were used, as opposed to participant-initiated event-contingent reporting to minimize reactivity (38).
Table 1:
Summary of EMA variables
| Variable | Statement/Question | Response options or coding |
|---|---|---|
| Stress | Right now I feel stressed. | Likert scale: 1=not at all, 7=very much so |
| Anxiety | Right now I feel anxious. | Likert scale: 1=not at all, 7=very much so |
| Food craving | Right now I am craving food. | Likert scale: 1=strongly disagree, 7=strongly agree |
| Dietary temptation | Since the last prompt, a) I was tempted to overeat, b) I had a sudden urge to eat a tempting or forbidden food, c) I was exposed to tempting foods or beverages, or d) None of the above (check all that apply). | If response was a,b,or c, it was classified as a ‘dietary temptation’. |
| Intensity of temptation | What was the intensity of the temptation? | Likert scale: 1=not strong at all, 10=extremely strong |
| Self-control | Did you eat the tempting food? (only asked when a dietary temptation was reported) | If response was ‘no’ this was coded as ‘self-control exhibited’ |
| Eating episode | Have you eaten since the last prompt?* | Response options: ‘yes’ or ‘no’. |
| Overeating episode | If an eating episode occurred, participants were asked to check all that apply: a) I ate past the point of feeling full, b) I ate more than usual, c) I had unplanned eating (i.e., consumed food when I don’t usually eat and was not making up for a missed meal, or d) None of the above. | If response was a, b, or c, it was classified as an ‘overeating episode’ |
| Stress-induced overeating episode | Any eating episode classified as ‘overeating’ in which the participant reported a ‘high’ stress score (≥ 5 on 1-7 Likert scale) on the previous prompt. | |
| Anxiety-driven overeating episode | Any eating episode classified as ‘overeating’ in which the participant reported a ‘high’ anxiety score (≥ 5 on 1–7 Likert scale) on the previous prompt. | |
Participants were not given explicit instructions for what constituted an eating episode. This was open to their discretion.
2.4.4. Questionnaire measures.
At baseline and 12 weeks, participants completed the Three-Factor Eating Questionnaires (TFEQ)(39).The TFEQ is a 51-item questionnaire developed to measure cognitive and behavioral components of eating behaviors. It has three subscales: dietary restraint (cognitive control over food intake), disinhibition (overeating in response to internal or external cues), and hunger (subjective feelings of hunger and food cravings). The restraint subscale can be further divided into rigid (dichotomous or ‘all-or-nothing’ approach to eating) and flexible control (less strict approach to eating where foods are allowed in limited quantities without feeling guilt) and the disinhibition subscale is further divided into external (the tendency to overeat in response to environmental cues) and internal disinhibition (tendency to overeat in response to negative emotional or cognitive cues)(40).
2.5. Power and statistical analyses
2.5.1. Power analysis.
Power estimates for this trial were based upon a sample size of n=48 and an estimated attrition rate of 15%. Based upon our previous pilot work, we conservatively estimated that there would be a minimum of 10 “overeating” episodes at baseline. Thus, we would have 80% power to detect a ≥20% reduction in the number of eating episodes characterized as “overeating” at Week 12 (e.g., 10 “overeating” episodes at baseline to 8 “overeating” episodes at Week 12). We anticipated that this would be equivalent to approximately a 400 kcal reduction over 10 days or 1200 kcal in one month, which would likely be clinically significant. Similarly, if 60% of “overeating” episodes were classified as “stress-induced overeating”, we would have 80% power to detect a ≥20% reduction in “stress-induced overeating” (e.g., 6 episodes at baseline to 4.8 episodes at Week 12). The study ended up recruiting more than the anticipated sample size (n=49) but saw attrition rates greater than anticipated (20%). Furthermore, at baseline, there was an average of 8.5 overeating episodes (compared to the 10 anticipated), only 1 of which was stress-induced. These differences amounted to a modest reduction in power (71% for stress-eating outcome and 78% for overeating outcome).
2.5.2. Statistical analysis plan.
Between group differences in baseline demographics, weight, physical activity levels and EMA compliance were compared using chi-squared tests (for categorical variables), t-tests (for continuous variables) and non-parametric methods as appropriate, and were reported as means ± standard deviation. Similar methods were used to assess differences between study completers and non-completers. For each of the outcome models, potential confounders were identified using correlation analysis; any variables correlated with both the predictor (e.g., Group) and outcome (e.g., stress) at a model p<.10 level were included as covariates in the subsequent analyses.
Overall compliance rates to the supervised exercise sessions were calculated, along with mean minutes/week of self-reported and objectively measured min/week of MVPA. Between-group differences in armband compliance (mean number of days armband was worn for ≥10 hours/day during each monitoring period) were calculated and compared using t-tests. Repeated measures ANOVAs were used to assess between group differences in exercise and fitness outcomes at follow-up controlling for baseline.
Treatment effects on stress, overeating episodes and anxiety were examined using a series of longitudinal mixed effects models (for continuous outcomes) and Generalized Estimating Equations (GEE’s) with robust standard errors (for binary outcomes). Mixed effects models included random intercepts (to account for repeated measures within participant over time) and assess both linear and non-linear effects of time. Models adjusted standard errors for clustering of responses within participant within day within monitoring period. Models specified a logit link function. Models included specifications of time (a time-varying indicator of day, indexed by monitoring period).
Finally, moderators (e.g., BMI, stress, anxiety) of treatment effect (for each of the primary and secondary outcomes), were assessed using a parallel modeling strategy to that described above (Mixed Effects Models and GEE’s as appropriate). Models included main effects of both group and the potential moderator, as well as the interaction between them.
All analyses were run on the intent to treat sample with all randomized participants included in the analysis. Model used a likelihood-based approach to estimation and thus made use of all observed data without directly imputing missing outcomes. Significance level was set at .05 a priori and analysis was conducted using SPSS 24.0 and SAS 9.3.
3.1. RESULTS
Of the 49 participants randomized (EX: n=25, CON: n=24), 39 completed the study (EX: n=19, CON: n=20; see CONSORT in Figure 1). As shown in Table 2, EX and CON participants did not differ on any variables at baseline. However, those who completed the study had a lower weight (83.8±12.0 vs. 95.9±10.0 kg; p=0.005) and BMI (31.6±3.9 vs. 35.5±3.5; p=0.007) at baseline, compared to those who did not complete the study. There were no differences between EX and CON completers.
Figure 1. CONSORT Diagram.
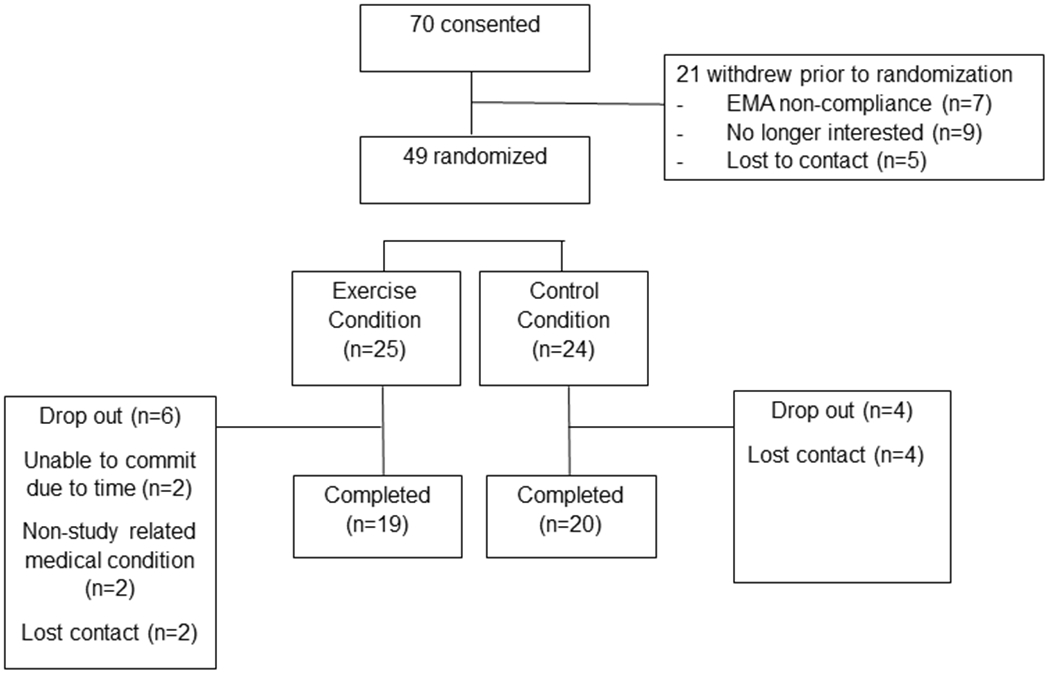
Table 2:
Baseline characteristics of randomized participants
| Exercise (n=25) |
Control (n=24) |
p-value for difference between groups | |
|---|---|---|---|
| Age (years) | 39.9±11.7 | 41.0±10.0 | 0.72 |
| BMI (kg/m2) | 32.5±4.0 | 32.2±4.3 | 0.88 |
| Weight (kg) | 86.5±12.9 | 86.1±12.3 | 0.92 |
| % Caucasian | 80.0% | 66.7% | 0.29 |
| EMA compliance (%) | 89.3±7.8 | 92.0±5.2 | 0.16 |
| Bout-related MVPA (min/day) | 9.7±9.1 | 7.9±7.2 | 0.45 |
| Sub-maximal fitness (sec) | 351.4±201.8 | 377.6±272.8 | 0.71 |
3.1.1. Compliance to the exercise intervention
Among participants randomized to EX, compliance to the exercise intervention was high. Participants attended an average of 15.5±1.1 out of 16 prescribed, supervised exercise sessions. Given the gradual progression of the prescribed exercise minutes, 100% compliance would equate to an average of 188 min/week of moderate-intensity PA over the 12-week intervention period. On average, participants in this study self-reported 189.0±26.6 min/week of bout-related MVPA and 186.8±28.4 min/week were objectively confirmed via the armband (99.4% of the prescribed exercise). All participants achieved at least 75% of the prescribed exercise minutes and the average MET value of all exercise performed was 4.5±0.4 METs. Further, on average, participants engaged in 4.0±0.8 exercise bouts per week, which included supervised sessions and objectively-confirmed unsupervised sessions that were at least 10 minutes in duration.
3.1.2. Between group changes in physical activity, fitness, and weight at 12 weeks
Compliance to wearing the armband was high at baseline (13.2±1.7 days of ≥10 hours/day and 13.8±1.2 hours/day) and 12 weeks (11.3±2.7 days and 13.9±1.2 hours/day) and did not differ between treatment groups (p’s >0.35). As expected, the EX condition significantly increased bout-related MVPA from baseline to 12 weeks (78.0±66.9 to 231.4±112.0 min/wk; p<0.001), whereas there was no change in MVPA among CON participants (53.8±48.8 to 52.6±88.5 min/wk; p=0.92). Similarly, there was a significant time by treatment interaction such that those in the CON condition experienced no change in fitness (change: 0.00±96.7 sec) while those in the EX condition increased fitness by 125.2±122.7 seconds at 12 weeks (p=0.001). Further, weight change among EX participants was −1.1±3.5% of initial body weight at 12 weeks whereas CON gained +0.4±2.0% (p=0.11). The effects of condition on fitness or percent weight change were not moderated by BMI (p’s>0.31).
3.1.3. Dietary restraint and disinhibition
Baseline to 12-week changes in dietary restraint and disinhibition are shown in Figure 2. There was a significant difference in mean disinhibition scores at 12 weeks, with EX having lower mean scores, compared to CON, after controlling for baseline (p=.01). Parallel models suggest this pattern of findings held for internal but not external disinhibition (in which there were no significant effects). Moreover, results suggest significant (p=.01) effects of condition on dietary restraint and rigid control (p=.04) but not for flexible control (p=.07). In all measures of restraint, data indicated higher scores at 12 weeks for EX vs. CON after controlling for baseline. BMI was not a significant moderator of the effect of condition on restraint or disinhibition (p’s>0.18).
Figure 2. Mean change in dietary restraint and disinhibition from baseline to 12 weeks.
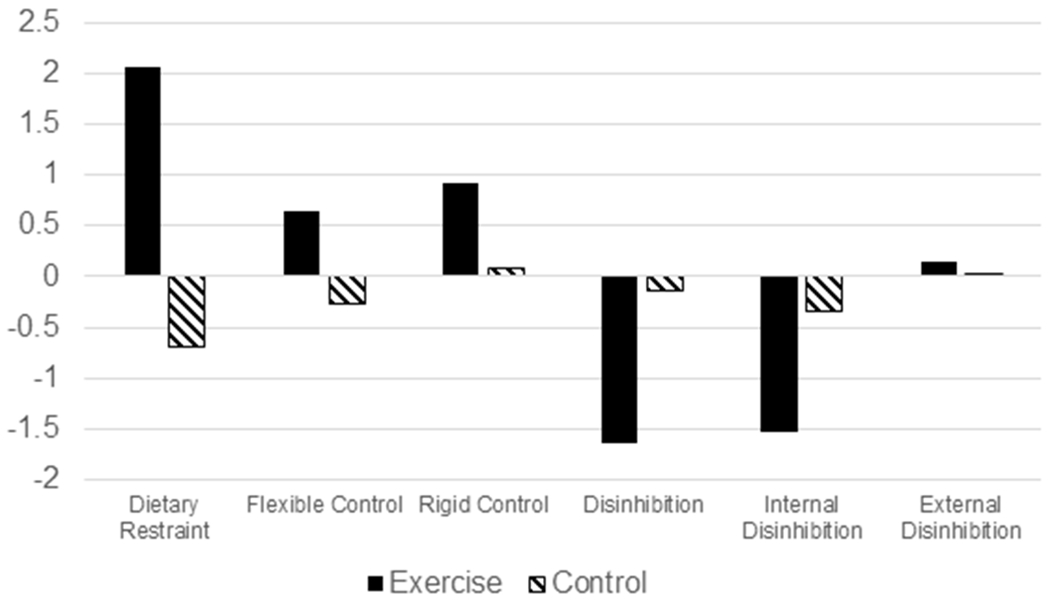
Change score calculated as 12-week minus baseline. * indicates EX and CON significant different from one another at p<0.05 in models adjusting for baseline value and random intercept. Results are for the intent-to-treat sample, with all available data included in the analysis.
3.1.4. Measures assessed via EMA
Participants responded to 91.8±6.6% of all EMA surveys at baseline and 83.7±12.9% of surveys at 12 weeks. On average it took participants 3.17±2.74 minutes to answer a survey and the average time between prompt delivery and response was 8.38±10.16 minutes. Table 3 displays baseline descriptive measures of all EMA variables aggregated over the 14-day monitoring period and stratified by condition. On average, participants reported approximately 31 eating episodes, 8 overeating episodes, 1 stress-induced overeating episode, and 1 anxiety-induced overeating episode over the 14-day period. A little over 30% of the time, participants reported exhibiting self-control and not eating a tempting food when one was present. Mean stress and anxiety ratings were low (range 2.17 – 2.75 on 1-7 Likert scale) and stress or anxiety was reported to be ‘high’ (≥5 on 1 to 7 Likert scale) on only 14%-19% of answered prompts.
Table 3:
Summary of EMA-assessed variables over the 14-day monitoring period at baseline
| Exercise | Control | P-value | |
|---|---|---|---|
| # eating episodes | 33.46±11.58 32.16±13.58 |
28.98±16.50 38.60±9.11 |
0.18 0.09 |
| Baseline 12w | |||
| # overeating episodes | 8.21±6.92 6.10 ±5.93 |
8.59±6.80 9.55±8.68 |
0.83 0.16 |
| Baseline 12w | |||
| # stress-induced overeating episodes | 1.11±1.99 0.74±1.56 |
1.05±2.05 0.55±1.00 |
0.90 0.66 |
| Baseline 12w | |||
| # anxiety-induced overeating episodes | 1.25±3.17 0.68±1.45 |
1.26±3.00 1.35±2.52 |
0.99 0.32 |
| Baseline 12w | |||
| # anxiety-induced overeating episodes | 1.25±3.17 0.68±1.45 |
1.26±3.00 1.35±2.52 |
0.99 0.32 |
| Baseline 12w | |||
| Mean anxiety rating | 2.17±1.14 2.04±1.03 |
2.30±1.42 2.12±1.26 |
0.65 0.81 |
| Baseline 12w | |||
| Proportion of instances where stress was ‘high’ | 0.15±.19 0.19±.26 |
0.19±.28 0.09±.12 |
0.94 0.15 |
| Baseline 12w | |||
| Proportion of instances where anxiety was ‘high’ | 0.15±.20 0.11±.21 |
0.14±.24 0.11±.20 |
0.94 0.96 |
| Baseline 12w | |||
| Proportion of instances where anxiety was ‘high’ | 0.15±.20 0.11±.21 |
0.14±.24 0.11±.20 |
0.94 0.96 |
| Baseline 12w | |||
| Proportion of instances where participant did not eat tempting food (self-control) | 0.36±0.31 0.33±0.29 |
0.32±0.28 0.15±0.14 |
0.57 0.03 |
| Baseline 12w |
P-value for between-group difference. Mean±SD, ‘high’ stress or anxiety defined as ≥5 on 1–7 Likert scale. Results are for the intent-to-treat sample, with all available data included in the analysis.
3.1.5. Overeating.
There was a significant between-group difference in the unadjusted proportion of eating episodes that were characterized as ‘overeating episodes’ in EX (21.98%) vs. CON at 12 weeks (26.62%; p=.001). The odds of having an overeating episode among EX participants was 0.58 times lower than CON’s at 12 weeks (condition*time=−.005, SE=.002, p=.01). Further investigation of the response options that were used to classify an eating episode as overeating (eating past feeling full, eating more than usual, unplanned eating) suggested that EX participants were reporting significantly less unplanned eating versus CON (condition*time=−.01, SE=.002, p=.04). There were no significant effects of condition on ‘eating past point of being full’ or ‘eating more than usual’. Finally, BMI was a significant moderator (p=.02) of the effect of exercise on overeating. Specifically, among those with higher BMI, there was less of an effect of exercise on the odds of overeating episodes; in other words, exercise training was more likely to reduce overeating among those with lower BMI.
3.1.6. Stress and anxiety.
Mixed effects models did not suggest differences between conditions over time on stress (when considered as a continuous outcome). However, models examining the effect of treatment group on high stress (scores >=5) vs. low stress (scores<5) suggested significant effects of group (p=.03). Specifically, the odds of a high stress score were significantly higher among EX participants versus CON at 12 weeks (OR=1.34, 95% CI:1.08-1.81). Conversely, a significant effect of treatment group on anxiety was found, with anxiety decreasing over time more in the EX condition vs. CON (p=.02). In addition, a GEE model suggested a lower odds of having a ‘high’ anxiety score (>=5) among EX participants vs CON at 12 weeks (OR=0.71, 95% CI: −0.46–0.99). Finally, BMI was not a significant moderator of the intervention effect on stress (scores>=5). However, it was a significant moderator of the exercise effect on anxiety outcomes (odds of scores>=5; p=.002). That is, the effects of exercise on reducing ‘high’ anxiety episodes was greater among those with a lower BMI. It should be noted, that a similar pattern of findings resulted when high stress/anxiety was coded as scores more than 1 standard deviation from the participant-level mean.
3.1.7. Anxiety or stress-induced overeating.
Results did not suggest significant effects of the intervention on stress-induced overeating (p=.61) or anxiety-induced overeating (p=.81). Moderators of potential effects were explored (BMI, stress, anxiety) but none reached statistical significance (p’s>.40).
3.1.8. Food cravings, dietary temptations, and self-control when tempted.
Longitudinal models showed a significant effect of treatment group on the temptation to overeat, with a lower odds of temptation among EX vs. CON (p=.002). However, although the odds of a temptation was lower in EX vs. CON, the mean intensity of the dietary temptations was higher among EX participants (p<.001). Further, although not significant (p=0.08), EX participants were more likely to exhibit self-control (i.e., not eat the tempting food; OR=2.02). These associations were not moderated by BMI, stress or anxiety (p’s>.45). Finally, food cravings over the 14-day EMA period were no different between EX and CON (p=0.79).
4.1. DISCUSSION
This randomized trial sought to examine the effect of 12 weeks of exercise training on eating behaviors among women who self-identified as eating more than usual in response to stress at baseline. Throughout the study, compliance to the exercise prescription was excellent and at 12 weeks EX participants experienced an increase in dietary restraint and a reduction in disinhibited eating (driven by internal disinhibition) when compared to a no-exercise control condition. Exercise participants were also less likely to overeat and there was a trend suggesting that they were more likely to exhibit self-control when faced with tempting foods (i.e., not eat the tempting food), despite the fact that no dietary instructions were provided throughout the trial. Overall these findings suggest that the effect of exercise on weight control may extend beyond the energy expenditure of the exercise itself, and may in part be due to favorable changes in eating-related constructs which are known to be associated with successful weight control efforts.
Maladaptive eating behaviors that are observed in response to emotional states (e.g., stress-induced overeating or disinhibited eating), can be detrimental to weight control efforts, particularly among women who are overweight or obese (40, 41). The current study found that 12 weeks of exercise training reduced disinhibited eating in EX, but not CON, suggesting an increased ability to resist urges to eat in response to stimuli, despite satiation. Specifically, this difference was driven by internal disinhibition, which represents the tendency to eat in response to negative thoughts, feelings, or sensations, which has been shown to be more strongly correlated with treatment response within weight loss programs, as compared to external disinhibition (40). The magnitude of reduction in internal disinhibition observed via 3 months of exercise training is approximately half of that which was observed in a 6-month, acceptance-based behavioral weight loss program, which specifically targeted individuals with high baseline levels of internal disinhibition and produced a mean weight loss of 8.7% (42). Interestingly, in the current study, this improvement in internal disinhibition was observed despite no dietary recommendations being provided and a much smaller observed weight loss (1.1% of initial body weight).
In contrast to disinhibition, dietary restraint represents the conscious restriction of food intake in an effort to manage weight. In today’s society, powerful environmental and social stimuli, and the presence of highly palatable foods can trigger hedonic eating; thus restrained eating may be important for weight control efforts. Previous research indicates that dietary restraint increases throughout a behavioral weight loss program and that higher restraint is associated with improved short and long-term weight loss success (43). While the magnitude of increase in dietary restraint that was observed as a result of 12 weeks of exercise is less than that which is typically observed in behavioral weight loss programs that include both diet and exercise instruction (44), the current findings provide additional evidence for the favorable effect of exercise on this important weight-related eating behavior.
A strength of this study was the assessment of participants over a 14-day period, in real-time, and under free living conditions. On average study participants engaged in approximately eight overeating episodes during the baseline monitoring period (26% of all reported eating episodes) and when faced with a tempting food, they only exhibited self-control approximately one-third of the time (i.e., did not eat the tempting food); both of which indicate the presence of maladaptive eating behaviors in the studied sample. However, following 12 weeks of exercise training, the proportion of eating episodes that were characterized as ‘overeating’ was significantly lower among EX relative to CON, and there was a trend such that EX was also more likely to exhibit self-control. These findings are promising and indicate that among women with overweight or obesity, regular exercise may have a favorable impact on eating patterns that can be detrimental to weight control efforts. Interestingly, the effect of EX on overeating was primarily driven by ‘unplanned’ eating, which is not surprising given that exercise training also increased dietary restraint. It is possible that exercise improved appetite regulation, making one less susceptible to non-appetitive internal (e.g., emotional) or external (i.e., environmental) cues that could trigger unplanned eating episodes. However, additional research is warranted to better understand why regular exercise may reduce unplanned eating and the potential impact that this may have on body weight. Future studies should seek to better understand why in the current study, the effect of exercise training on overeating was primarily observed among those with a lower BMI (<35 kg/m2). One possible explanation is that those with a higher BMI may experience more negative affective responses to an exercise bout (45). Given that affect can influence eating behaviors, future studies should examine affective responses to exercise as one contributing factor. Finally, it is unclear whether similar findings would be observed with a different dose or intensity of exercise or within the context of a behavioral weight control intervention; additional research in this area is warranted.
While weight change was not a primary outcome measure in the current study, it is still important to note that on average EX lost 1.3 kg more than CON, which was not statistically significant. Previous research indicates that the impact of exercise on body weight is typically only 2-3 kg (46). Moreover, based upon the energy expenditure of the objectively-confirmed exercise in the current study, a mean weight loss of 2.0 kg would have been expected, suggesting that a small degree of energy compensation may have occurred in response to the exercise training. This is somewhat surprising given exercise training reduced overeating episodes, improved disinhibited eating, and led to participants giving into fewer dietary temptations. However, it is possible that exercise led to an increase in total energy intake, which could have been driven an increase in hunger or other factors not assessed in the current study (e.g., increased portion sizes at meals, more frequent snacking, or changes in the macronutrient composition of meals). Future studies could consider comparing EMA methods used in the current study to dietary self-monitoring records to better understand potential associations with portion sizes, meal timing, and frequency. Also, given that exercise has been shown to exhibit a greater effect during weight loss maintenance (47), future studies should assess the impact of exercise-related improvements in disinhibited eating and overeating on long-term weight control.
Despite the abovementioned effects of exercise training on important eating behaviors, there were also several findings that were contrary to our hypotheses. First, was the lack effect of exercise training on stress, as assessed via EMA ratings. Results indicate no difference in stress over time as a result of condition, but EX was more likely to have a ‘high’ stress score at 12 weeks, relative to CON. Given that previous research clearly indicates that high levels of exercise are associated with lower stress, and that exercise training can reduce stress (18, 48), it is uncertain why these findings were not in the hypothesized direction. This is especially surprising given that exercise training lowered anxiety and reduced the probability of having a ‘high’ anxiety score in the current sample, which is in the direction of that hypothesized for stress. One possibility for these discordant findings is that the act of striving to achieve the exercise goals to appease the research staff, may have induced stress, thereby negating the positive effect that exercise typically has on stress. Another possibility could be attributed to the low levels of stress observed at baseline, thereby allowing little room for improvement in stress as a result of exercise training. These low levels of reported stress and few instances of ‘high stress’ (15% at baseline) also made it difficult to examine whether exercise could reduce stress-induced overeating. On average, there was only one stress-induced overeating episode observed per person at baseline, thereby making it difficult to ascertain whether exercise training could buffer against this effect. This is surprising given that all study participants were women (a subgroup more likely to endorse stress-eating compared to men (33, 34), and that all women endorsed overeating in response to stress on the eligibility screener. Nonetheless, this is a limitation of the current research. Future studies seeking to examine the effect of exercise on stress-induced overeating should not only recruit individuals who endorse eating more in response to stress, but they should also consider only recruiting individuals with high stress, or utilizing data collection methods which would capture additional moments of ‘high’ stress (e.g., real-time assessment of heart rate variability, as this has been shown to be associated with autonomic nervous system activity associated with stress (49)).
While there are many strengths to the current study, including the use of ecological momentary assessment methodology, supervised exercise training with objectively confirmed exercise adherence to unsupervised visits, and the use of a population at greatest risk for stress-induced overeating, there are additional limitations. First, this study was limited to women and it is therefore unclear whether findings would be replicated in men, particularly those who endorse stress-eating. Second, due to higher than anticipated attrition rates, and fewer overeating episodes and stress-induced overeating episodes at baseline, this study was slightly underpowered for these primary outcomes (78% and 71% power respectively). Third, while the dose of exercise training was above national PA recommendations for improved health (≥150 min/week), it was below that recommended for weight control (≥250 min/week (50); thus future studies should examine whether similar findings are observed with higher doses of exercise. Alternatively, investigators could also consider matching participants on energy expenditure, rather than total exercise minutes, as energy expenditure in this study likely varied between participants. However, prescribing exercise based on energy expenditure would limit translatability of findings (i.e., exercise is typically prescribed in minutes per week and not calories expended per week), thus the pros and cons of this approach should first be considered. In addition, given that this was an efficacy trial (not an effectiveness trial), participants were compensated for exercise compliance. While we believe that the provision of compensation aided in our excellent adherence to the exercise prescription, it is also possible that compensation was a motivating factor for participants, potentially impacting study findings. Future effectiveness trials are warranted. Finally, this study is limited in that menstrual cycle was not assessed as part of the current protocol, precluding the examination of hormonal influence (e.g., progesterone) on hedonic eating in this sample of women. Changes in menstrual function resulting from the 12-week exercise program, or differences in menstrual cycle phase during EMA assessment periods may have also impacted study findings. Future studies should consider assessing and controlling for hormonal and menstrual cycle.
In conclusion, this randomized trial assessed the effects of 12 weeks of exercise training on eating behaviors, in a population at increased risk of hedonic eating. Compliance to the exercise prescription was excellent, and CON participants were equally compliant, not altering their PA, thereby creating a necessary and significance difference in PA between groups to adequately address the proposed research questions. Findings reveal that exercise training had a favorable effect on internal disinhibition, dietary restraint, and overeating episodes, all of which have been shown to be important for weight control. These findings add to the existing literature and suggest that chronic exercise may indirectly influence energy balance via effects on eating behaviors among women who are overweight or obese.
Acknowledgements
This study was supported by a grant awarded to Dr. Unick by the National Institute of Diabetes and Digestive Diseases (K01DK100498-01). The authors declare that they have no competing interests. The results of this study are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation. Further, the results of this study do not constitute endorsement by ACSM.
Footnotes
Trial registration: clinicaltrials.gov (NCT02936076); registered on 10/13/2016 https://clinicaltrials.gov/ct2/show/NCT02936076?term=NCT02936076&draw=2&rank=1
References
- 1.Lowe MR, Butryn ML. Hedonic hunger: a new dimension of appetite? Physiol Behav. 2007;91(4):432–9. Epub 2007/05/29. doi: 10.1016/j.physbeh.2007.04.006.. [DOI] [PubMed] [Google Scholar]
- 2.Woods SC. The eating paradox: how we tolerate food. Psychol Rev. 1991;98(4):488–505. Epub 1991/10/01. doi: 10.1037/0033-295x.98.4.488.. [DOI] [PubMed] [Google Scholar]
- 3.French SA, Epstein LH, Jeffery RW, Blundell JE, Wardle J. Eating behavior dimensions. Associations with energy intake and body weight. A review. Appetite. 2012;59(2):541–9. Epub 2012/07/17. doi: 10.1016/j.appet.2012.07.001.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Elfhag K, Rossner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev. 2005;6(1):67–85. Epub 2005/01/19. doi: OBR170 [pii] 10.1111/j.1467-789X.2005.00170.x.. [DOI] [PubMed] [Google Scholar]
- 5.Groesz LM, McCoy S, Carl J, Saslow L, Stewart J, Adler N, et al. What is eating you? Stress and the drive to eat. Appetite. 2012;58(2):717–21. doi: 10.1016/j.appet.2011.11.028.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Macht M How emotions affect eating: a five-way model. Appetite. 2008;50(1):1–11. doi: 10.1016/j.appet.2007.07.002.. [DOI] [PubMed] [Google Scholar]
- 7.Forman EM, Butryn ML. A new look at the science of weight control: how acceptance and commitment strategies can address the challenge of self-regulation. Appetite. 2015;84:171–80. doi: 10.1016/j.appet.2014.10.004. ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.DiLeone RJ, Taylor JR, Picciotto MR. The drive to eat: comparisons and distinctions between mechanisms of food reward and drug addiction. Nat Neurosci. 2012;15(10):1330–5. doi: 10.1038/nn.3202.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nederkoorn C, Smulders FT, Jansen A. Cephalic phase responses, craving and food intake in normal subjects. Appetite. 2000;35(1):45–55. doi: 10.1006/appe.2000.0328.. [DOI] [PubMed] [Google Scholar]
- 10.Sobik L, Hutchison K, Craighead L. Cue-elicited craving for food: a fresh approach to the study of binge eating. Appetite. 2005;44(3):253–61. doi: 10.1016/j.appet.2004.12.001.. [DOI] [PubMed] [Google Scholar]
- 11.Berridge KC. Food reward: brain substrates of wanting and liking. Neurosci Biobehav Rev. 1996;20(1):1–25.. [DOI] [PubMed] [Google Scholar]
- 12.Gosnell BA, Levine AS. Reward systems and food intake: role of opioids. Int J Obes (Lond). 2009;33 Suppl 2:S54–8. doi: 10.1038/ijo.2009.73.. [DOI] [PubMed] [Google Scholar]
- 13.Lowe MR, Levine AS. Eating motives and the controversy over dieting: eating less than needed versus less than wanted. Obes Res. 2005;13(5):797–806. doi: 10.1038/oby.2005.90.. [DOI] [PubMed] [Google Scholar]
- 14.Jakicic JM, Powell KE, Campbell WW, Dipietro L, Pate RR, Pescatello LS, et al. Physical Activity and the Prevention of Weight Gain in Adults: A Systematic Review. Med Sci Sports Exerc. 2019;51(6):1262–9. Epub 2019/05/17. doi: 10.1249/MSS.0000000000001938.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smith MA, Lynch WJ. Exercise as a potential treatment for drug abuse: evidence from preclinical studies. Front Psychiatry. 2012;2:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Prochaska JJ, Hall SM, Humfleet G, Munoz RF, Reus V, Gorecki J, et al. Physical activity as a strategy for maintaining tobacco abstinence: A randomized trial. Prev Med. 2008;47(2):215–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brown RA, Abrantes AM, Read JP, Marcus BH, Jakicic J, Strong DR, et al. Aerobic exercise for alcohol recovery: rationale, program description, and preliminary findings. Behav Modif. 2009;33(2):220–49. Epub 2008/12/19. doi: 0145445508329112 [pii] 10.1177/0145445508329112. ;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Starkweather AR. The effects of exercise on perceived stress and IL-6 levels among older adults. Biol Res Nurs. 2007;8(3):186–94. Epub 2006/12/19. doi: 10.1177/1099800406295990.. [DOI] [PubMed] [Google Scholar]
- 19.Steptoe A, Edwards S, Moses J, Mathews A. The effects of exercise training on mood and perceived coping ability in anxious adults from the general population. J Psychosom Res. 1989;33(5):537–47. Epub 1989/01/01. doi: 0022–3999(89)90061–5 [pii].. [DOI] [PubMed] [Google Scholar]
- 20.Norris R, Carroll D, Cochrane R. The effects of physical activity and exercise training on psychological stress and well-being in an adolescent population. J Psychosom Res. 1992;36(1):55–65. Epub 1992/01/01. doi: 0022–3999(92)90114-H [pii].. [DOI] [PubMed] [Google Scholar]
- 21.Steptoe A, Moses J, Edwards S, Mathews A. Exercise and responsivity to mental stress: Discrepancies between the subjective and phsyiological effects of aerobic training. Int J Sport Psychol. 1993;24:110–29. [Google Scholar]
- 22.LaPerriere AR, Antoni MH, Schneiderman N, Ironson G, Klimas N, Caralis P, et al. Exercise intervention attenuates emotional distress and natural killer cell decrements following notification of positive serologic status for HIV-1. Biofeedback Self Regul. 1990;15(3):229–42. Epub 1990/09/01.. [DOI] [PubMed] [Google Scholar]
- 23.Cramer SR, Nieman DC, Lee JW. The effects of moderate exercise training on psychological well-being and mood state in women. J Psychosom Res. 1991;35(4–5):437–49. Epub 1991/01/01.. [DOI] [PubMed] [Google Scholar]
- 24.Roth DL, Holmes DS. Influence of aerobic exercise training and relaxation training on physical and psychologic health following stressful life events. Psychosom Med. 1987;49(4):355–65. Epub 1987/07/01.. [DOI] [PubMed] [Google Scholar]
- 25.Block JP, He Y, Zaslavsky AM, Ding L, Ayanian JZ. Psychosocial stress and change in weight among US adults. Am J Epidemiol. 2009;170(2):181–92. Epub 2009/05/26. doi: kwp104 [pii] 10.1093/aje/kwp104.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kivimaki M, Head J, Ferrie JE, Shipley MJ, Brunner E, Vahtera J, et al. Work stress, weight gain and weight loss: evidence for bidirectional effects of job strain on body mass index in the Whitehall II study. Int J Obes (Lond). 2006;30(6):982–7. Epub 2006/01/19. doi: 0803229 [pii] 10.1038/sj.ijo.0803229. [DOI] [PubMed] [Google Scholar]
- 27.Newman E, O'Connor DB, Conner M. Daily hassles and eating behaviour: the role of cortisol reactivity status. Psychoneuroendocrinology. 2007;32(2):125–32. Epub 2007/01/03. doi: 10.1016/j.psyneuen.2006.11.006.. [DOI] [PubMed] [Google Scholar]
- 28.Oliver G, Wardle J, Gibson EL. Stress and food choice: a laboratory study. Psychosom Med. 2000;62(6):853–65. Epub 2001/01/04.. [DOI] [PubMed] [Google Scholar]
- 29.Zellner DA, Loaiza S, Gonzalez Z, Pita J, Morales J, Pecora D, et al. Food selection changes under stress. Physiol Behav. 2006;87(4):789–93. Epub 2006/03/08. doi: 10.1016/j.physbeh.2006.01.014.. [DOI] [PubMed] [Google Scholar]
- 30.Lemmens SG, Rutters F, Born JM, Westerterp-Plantenga MS. Stress augments food 'wanting' and energy intake in visceral overweight subjects in the absence of hunger. Physiol Behav. 2011;103(2):157–63. Epub 2011/01/19. doi: S0031–9384(11)00024–2 [pii] 10.1016/j.physbeh.2011.01.009.. [DOI] [PubMed] [Google Scholar]
- 31.Roemmich JN, Lambiase MJ, Lobarinas CL, Balantekin KN. Interactive effects of dietary restraint and adiposity on stress-induced eating and the food choice of children. Eat Behav. 2011;12(4):309–12. Epub 2011/11/05. doi: S1471–0153(11)00064-X [pii] 10.1016/j.eatbeh.2011.07.003.. [DOI] [PubMed] [Google Scholar]
- 32.O'Connor DB, Jones F, Conner M, McMillan B, Ferguson E. Effects of daily hassles and eating style on eating behavior. Health Psychol. 2008;27(1 Suppl):S20–31. Epub 2008/03/08. doi: 2008–00684-004 [pii] 10.1037/0278-6133.27.1.S20.. [DOI] [PubMed] [Google Scholar]
- 33.Provencher V, Drapeau V, Tremblay A, Despres JP, Lemieux S. Eating behaviors and indexes of body composition in men and women from the Quebec family study. Obes Res. 2003;11(6):783–92. Epub 2003/06/14. doi: 10.1038/oby.2003.109.. [DOI] [PubMed] [Google Scholar]
- 34.Greeno CG, Wing RR. Stress-induced eating. Psychol Bull. 1994;115(3):444–64. Epub 1994/05/01.. [DOI] [PubMed] [Google Scholar]
- 35.Jakicic JM, Marcus M, Gallagher KI, Randall C, Thomas E, Goss FL, et al. Evaluation of the SenseWear Pro Armband to assess energy expenditure during exercise. Med Sci Sports Exerc. 2004;36(5):897–904. Epub 2004/05/06. doi: 00005768–200405000-00024 [pii].. [DOI] [PubMed] [Google Scholar]
- 36.St-Onge M, Mignault D, Allison DB, Rabasa-Lhoret R. Evaluation of a portable device to measure daily energy expenditure in free-living adults. Am J Clin Nutr. 2007;85(3):742–9. Epub 2007/03/09. doi: 85/3/742 [pii].. [DOI] [PubMed] [Google Scholar]
- 37.Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4:1–32. Epub 2008/05/30. doi: 10.1146/annurev.clinpsy.3.022806.091415.. [DOI] [PubMed] [Google Scholar]
- 38.Shiffman S Designing protocols for ecological momentary assessment. In: Stone AA, Shiffman S, Atienza AA, Nebeling L, editors. The science of REAL-TIME data capture. New York: Oxford University Press; 2007. p. 27–53. [Google Scholar]
- 39.Stunkard AJ, Messick S. The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J Psychosom Res. 1985;29(1):71–83. Epub 1985/01/01.. [DOI] [PubMed] [Google Scholar]
- 40.Niemeier HM, Phelan S, Fava JL, Wing RR. Internal disinhibition predicts weight regain following weight loss and weight loss maintenance. Obesity (Silver Spring). 2007;15(10):2485–94. Epub 2007/10/11. doi: 15/10/2485 [pii] 10.1038/oby.2007.295.. [DOI] [PubMed] [Google Scholar]
- 41.Hays NP, Roberts SB. Aspects of eating behaviors "disinhibition" and "restraint" are related to weight gain and BMI in women. Obesity (Silver Spring). 2008;16(1):52–8. Epub 2008/01/29. doi: 10.1038/oby.2007.12.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lillis J, Niemeier HM, Thomas JG, Unick J, Ross KM, Leahey TM, et al. A randomized trial of an acceptance-based behavioral intervention for weight loss in people with high internal disinhibition. Obesity (Silver Spring). 2016;24(12):2509–14. doi: 10.1002/oby.21680.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Thomas JG, Bond DS, Phelan S, Hill JO, Wing RR. Weight-loss maintenance for 10 years in the National Weight Control Registry. Am J Prev Med. 2014;46(1):17–23. Epub 2013/12/21. doi: 10.1016/j.amepre.2013.08.019.. [DOI] [PubMed] [Google Scholar]
- 44.Teixeira PJ, Silva MN, Coutinho SR, Palmeira AL, Mata J, Vieira PN, et al. Mediators of weight loss and weight loss maintenance in middle-aged women. Obesity (Silver Spring). 2010;18(4):725–35. Epub 2009/08/22. doi: 10.1038/oby.2009.281.. [DOI] [PubMed] [Google Scholar]
- 45.Ekkekakis P, Lind E, Vazou S. Affective Responses to Increasing Levels of Exercise Intensity in Normal-weight, Overweight, and Obese Middle-aged Women. Obesity (Silver Spring). 2010;18(1):79–85. Epub 2009/06/27. doi: oby2009204 [pii] 10.1038/oby.2009.204.. [DOI] [PubMed] [Google Scholar]
- 46.Garrow JS, Summerbell CD. Meta-analysis: effect of exercise, with or without dieting, on the body composition of overweight subjects. Eur J Clin Nutr. 1995;49(1):1–10. Epub 1995/01/01.. [PubMed] [Google Scholar]
- 47.Donnelly JE, Blair SN, Jakicic JM, Manore MM, Rankin JW, Smith BK. American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc. 2009;41(2):459–71. Epub 2009/01/08. doi: 10.1249/MSS.0b013e3181949333.. [DOI] [PubMed] [Google Scholar]
- 48.Schnohr P, Kristensen TS, Prescott E, Scharling H. Stress and life dissatisfaction are inversely associated with jogging and other types of physical activity in leisure time--The Copenhagen City Heart Study. Scand J Med Sci Sports. 2005;15(2):107–12. Epub 2005/03/19. doi: 10.1111/j.1600-0838.2004.00394.x.. [DOI] [PubMed] [Google Scholar]
- 49.Kim HG, Cheon EJ, Bai DS, Lee YH, Koo BH. Stress and Heart Rate Variability: A Meta-Analysis and Review of the Literature. Psychiatry Investig. 2018;15(3):235–45. Epub 2018/02/28. doi: 10.30773/pi.2017.08.17.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.U.S. Department of Health and Human Services. Physical activity guidelines for Americans, 2nd edition. Washington DC: U.S. Department of health and Human Services; 2018. [Google Scholar]


