Abstract
Background
Long-term implant durability is a key concern when considering total hip arthroplasty (THA) in young patients. The ideal bearing surface used in these patients remains unknown. The purpose of this study was to analyze trends in THA bearing surface use from 2006 to 2016 using a large, pediatric national database.
Methods
This was a retrospective review from January 1, 2006, to December 31, 2016, using the Kids’ Inpatient Database. International Classification of Diseases, 9th revision and 10th revision codes were used to identify patients who underwent THA and create cohorts based on bearing surfaces: metal-on-metal, metal-on-polyethylene, ceramic-on-polyethylene (CoP), and ceramic-on-ceramic (CoC). Annual utilization of each bearing surface and associated patient and hospital demographics were analyzed.
Results
A total of 1004 THAs were identified during the 11-year study period. The annual number of THAs performed increased by 169% from 2006 to 2016. The mean patient age was 17.1 years. The most prevalent bearing surface used in 2006 was CoC (37.3%), metal-on-metal (31.8%) in 2009, and CoP in 2012 and 2016 (50.6% and 64.8%, respectively). From 2006 to 2016, utilization of CoP increased from 5.0% to 64.8%, representing a 1196% increase over the study period.
Conclusions
The number of THAs performed in pediatric patients is increasing significantly. Although CoC was previously the most commonly used bearing surface in this patient population, CoP is currently the most common. Further investigation is needed to determine whether bearing longevity and clinical outcomes with CoP are superior to other bearing surfaces.
Keywords: Total hip arthroplasty, Pediatric, Bearing surface trends
Introduction
Over the past few decades, total hip arthroplasty (THA) has become one of the most commonly performed orthopedic procedures in the United States [1]. As THA is performed more frequently in young, active patients, concerns about wear-related premature failure become ever more significant. Traditionally, the consensus was that younger patients would benefit from hard-on-hard surface bearings—metal-on-metal (MoM) and ceramic-on-ceramic (CoC)—as these would improve durability and avoid the complications associated with polyethylene wear and associated osteolysis. However, the use of MoM bearings has fallen precipitously over the last decade because of early failures associated with metal wear debris aseptic lymphocyte-dominant vasculitis-associated lesions [2]. CoC bearing couplings remain a viable option; however, they are associated with noise and, rarely, with implant fracture, which can be a devastating complication [3]. At the same time, the wear characteristics of hard-on-soft bearing couplings such as ceramic-on-polyethylene (CoP) and metal-on-polyethylene (MoP) have improved significantly with the advent and widespread use of highly cross-linked polyethylene [4].
Considerations relating to implant longevity are especially important in the extremely young (<21 years) patient population. The most common indications for THA in pediatric patients and young adults include undertreated developmental dysplasia of the hip, femoral acetabular impingement, Legg-Calve-Perthes disease, slipped capital femoral epiphysis, avascular necrosis (AVN), inflammatory arthritis, and posttraumatic arthritis [5]. While several reconstructive procedures exist (including femoral and pelvic osteotomies for dysplasia and femoral head decompression for AVN), increasing evidence of the long-term durability of hip arthroplasty in adult populations has likely contributed to the rise of THA in pediatric patients in whom reconstructive procedures are inadequate—including femoral head collapse with AVN and Stulberg IV/V hips in Legg-Calve-Perthes [5]. But even as the number of THAs performed in the extremely young patient population increases, it is not known which bearing couplings are most frequently used and result in superior outcomes in this patient population.
The purpose of this study is to perform an epidemiological analysis of bearing surface utilization in THA in the extremely young (<21 years) patient population using a national administrative database. We hypothesize that over the course of the study period, there will be a decrease in the use of MoM bearings along with an increase in CoC and CoP.
Material and methods
The study cohort was identified using the Kids’ Inpatient Database (KID) over an 11-year period (2006-2016), with data available for the years 2006, 2009, 2012, and 2016. The KID is a nationally representative database developed from all hospitals in the United States participating in the Healthcare Cost and Utilization Project (HCUP) and validated through a federal-state-industry partnership sponsored by the Agency for Healthcare Research and Quality (AHRQ). The KID contains inpatient data for patients younger than 21 years from 46 states plus the District of Columbia, covering approximately 80% of all pediatric discharges and 10% of uncomplicated hospital births from US hospitals, excluding rehabilitation and long-term acute care hospitals. The large sample size from the KID allows analysis of rare conditions. A stratified algorithm based on discharge weights reported by statewide HCUP contributors was designed to allow an estimation of nationally representative statistics. Available variables include demographic data, diagnoses, procedures, hospital characteristics, length of stay, and cost. As the KID is sufficiently deidentified of any personal health information or identifiers, this study was deemed exempt by the institutional review board at our institution.
Patients younger than 21 years who were admitted for THA were included in the study cohort. Patients were selected using the International Classification of Diseases, 9th Revision (ICD-9) and 10th Revision (ICD-10), procedure codes for THA. Patients were divided based on the type of bearing surfaces used for THA, identified using ICD-9 and ICD-10 codes for MoM, CoC, CoP, and MoP (Appendix Table 1). Annual incidence of each bearing surface type was calculated and used to generate trend lines for the study period. Individual hospitalization cost was calculated using diagnosis-related group codes multiplied by hospital-specific cost-to-charge ratios provided by the AHRQ. HCUP indices of the diagnosis-related group were then used to account for differences in severity of illness. Costs were then standardized for inflation using the yearly gross domestic product. Patients with missing data for any of the primary outcomes of interest were excluded.
All result sample sizes represented national annual estimates derived from individual discharge-level weights from the KID's random sampling design, using Stata’s survey data commands. Descriptive analysis was used to describe both baseline characteristics and outcome parameters within each comparison group. Categorical variables were presented as adjusted odds ratios and compared using the Chi-square statistic, except when there were less than 10 individuals, in which case the Fisher exact test was used. Continuous variables were reported using mean, 95% confidence interval, and P value. Analysis was completed using analysis of variance two-tailed Student’s t-test after ensuring normal distributions. For skewed distributions, continuous variables are presented as median (interquartile range) and analyzed using the Wilcoxon rank-sum test. Chi-square goodness of fit test was performed within each variable category. All statistical analyses were carried out comparing pediatric THA patients for each outcome of interest. Data were analyzed using Stata 15.0 (StataCorp LLC, College Station, TX). All tests were unpaired, and significance level was defined at P < .05.
Results
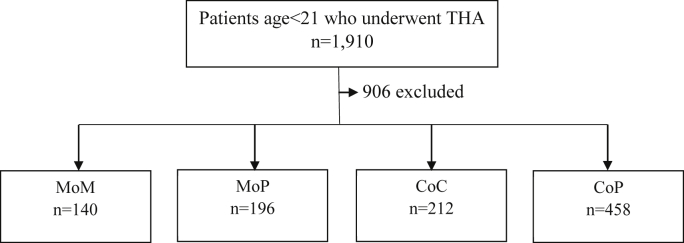
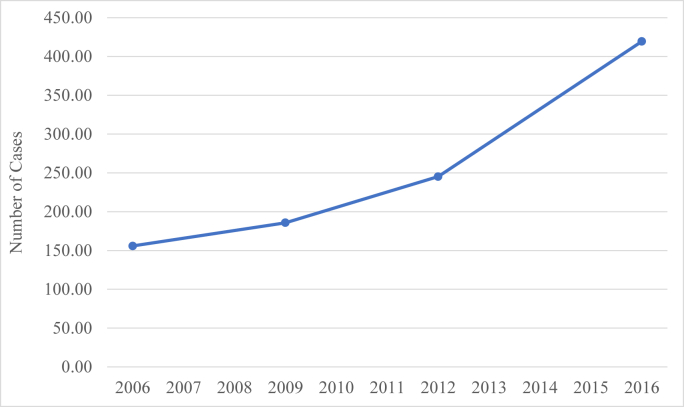
A total of 1910 THAs were identified during the study period (Fig. 1). Bearing type used was available for 1004 (52.6%) of these THAs and were included for analysis. The annual number of THAs performed increased by 169%, from 156 in 2006 to 420 in 2016, which represented a statistically significant increase (P < .05) (Fig. 2). The mean patient age at implantation across the combined cohort was 17.2 years and did not significantly change over the study period (P = .4). The mean comorbidity score measured by the Elixhauser Comorbidity Index was 0.87, and there was no significant difference based on bearing type (P = .21). Average cost of hospitalization was $22,080.93. Mean index hospitalization costs were highest for MoP at $22,747.71 and lowest for CoP at $19,682.64 (P = .0082). From 2006 to 2016, length of stay decreased from 4.85 days to 3.19 days (P = .0007); there was no significant difference between age and Elixhauser Comorbidity Index or cost across the study period.
Figure 1.
Flowchart of patient study population. Patients aged <21 years who underwent THA were separated into groups based on bearing types. Patients without bearing type designation were excluded.
Figure 2.
Incidence of pediatric total hip arthroplasty 2006-2016. There was an overall 169% increase in the number of pediatric THA cases. The increase was statistically significant if P < .05 using the Cochran-Armitage trend test.
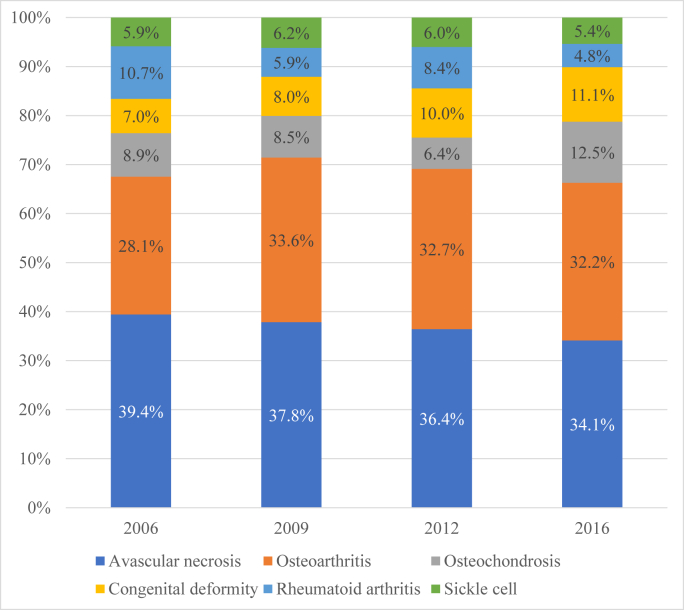
Patient demographics are included in Table 1. THA were most likely to be performed at urban teaching hospitals (82%) and in the Southern region (38.5%) of the United States (Table 1). The most common indications for THA included AVN (36.6%), osteoarthritis (31.9%), and congenital hip deformity (9.3%). Figure 3 is a graphical representation of the breakdown of THAs performed each year of the study period by indication.
Table 1.
Patient demographic characteristics.
| Characteristics | MoM (%) | MoP (%) | CoC (%) | CoP (%) | P value |
|---|---|---|---|---|---|
| Sex | |||||
| Male | 95 (67.6) | 93 (48.3) | 105 (49.3) | 210 (46.1) | - |
| Female | 45 (32.4) | 99 (51.7) | 108 (50.7) | 246 (53.9) | .0059 |
| Race | |||||
| White | 62 (43.9) | 96 (49.2) | 104 (49.2) | 234 (51.0) | .7228 |
| Black | 25 (18.0) | 28 (14.6) | 48 (22.5) | 81 (17.6) | .4049 |
| Hispanic | 16 (11.1) | 18 (9.1) | 16 (7.4) | 55 (12.1) | .4873 |
| Asian | 2 (1.1) | 4 (2.1) | 3 (7.4) | 15 (3.3) | .4367 |
| Other | 7 (5.0) | 12 (6.3) | 8 (3.6) | 27 (5.9) | .7673 |
| Insurance | |||||
| Medicare | 0 (0) | 4 (2.2) | 5 (2.4) | 11 (3.1) | .5447 |
| Medicaid | 38 (26.9) | 61 (31.2) | 75 (35.5) | 148 (32.2) | .6122 |
| Private | 94 (66.7) | 109 (55.6) | 110 (51.6) | 270 (59.0) | .1669 |
| Self | 3 (2.4) | 9 (4.5) | 4 (2.0) | 8 (1.8) | .5778 |
| Hospital type | |||||
| Rural | 4 (3.0) | 4 (2.1) | 2 (0.7) | 3 (0.7) | .2576 |
| Urban nonteaching | 21 (15.3) | 23 (11.5) | 39 (18.4) | 59 (12.9) | .392 |
| Urban teaching | 112 (79.6) | 166 (84.7) | 172 (80.8) | 393 (85.8) | .4331 |
| Hospital region | |||||
| Northeast | 24 (17.4) | 48 (24.8) | 27 (12.9) | 78 (17.0) | .1505 |
| Midwest | 33 (23.7) | 55 (28.4) | 44 (20.9) | 97 (21.3) | .5092 |
| South | 52 (37.4) | 46 (23.7) | 97 (45.5) | 176 (38.4) | .0159 |
| West | 30 (21.4) | 45 (23.2) | 44 (20.8) | 107 (23.3) | .9479 |
| Hospital size | |||||
| Small bed | 29 (20.7) | 24 (12.5) | 33 (15.8) | 81 (17.6) | .4615 |
| Medium bed | 20 (14.6) | 46 (23.8) | 45 (21.0) | 69 (15.1) | .1724 |
| Large bed | 88 (62.6) | 121 (62.1) | 134 (63.2) | 305 (66.7) | .8147 |
| Income | |||||
| 0-25th Percentile | 52 (37.4) | 45 (23.1) | 60 (28.5) | 124 (27.1) | .1198 |
| 25-50th Percentile | 31 (21.9) | 39 (19.9) | 50 (23.7) | 96 (20.9) | .8734 |
| 50-75th Percentile | 26 (18.8) | 51 (26.3) | 51 (22.9) | 101 (27.5) | .6084 |
| 75-100th Percentile | 29 (20.9) | 51 (26.3) | 49 (22.9) | 126 (27.5) | .5364 |
Figure 3.
Indications over time for pediatric total hip arthroplasty: Avascular necrosis and osteoarthritis were the primary 2 causes for pediatric total hip arthroplasty. There was a decreased rate of avascular necrosis as reason for surgery over the study period.
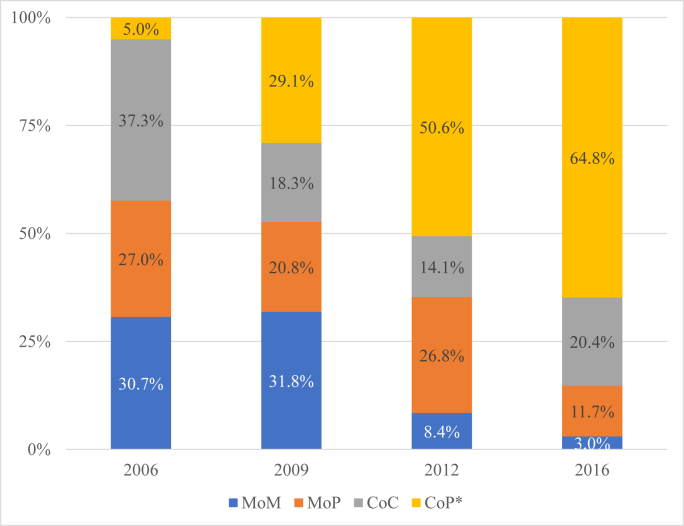
Of the 1004 patients included for analysis, 140 (14.0%) were MoM, 196 (19.6%) MoP, 212 (21.1%) CoC, and 458 (45.6%) CoP (Fig. 1). From 2006 to 2016, utilization of CoP increased from 8 (5.0%) to 272 (64.8%), respectively, which represents a 1196% increase (Fig. 4). The most prevalent bearing surface in 2006 was CoC (37.3%), MoM (31.8%) in 2009, and CoP in 2012 and 2016 (50.6% and 64.8%, respectively).
Figure 4.
Ratio of bearing type in pediatric total hip arthroplasty from 2006 to 2016. There was a 57% decrease in rate of MoP used as well as a 90% decrease in the rate of MoM used. There was a 1196% increase in the rate of CoP used. ∗Statistically significant if P < .05 using Cochran-Armitage trend test.
Discussion
To our knowledge, this is the first study to use a pediatric national administrative database to report on the indications for and bearing surface material utilization in THA performed in patients aged <21 years in the United States. We found a nearly 50% increase in THA nationally with a 1196% increase in CoP bearing surfaces between 2006 and 2016. Previously published results by Rajaee et al. on the trends of THA bearing surfaces in patients aged ≤30 years between 2009 and 2012 found that hard-on-hard bearing usage decreased from 2009 to 2012, whereas hard-on-soft bearing surface usage (MoP and CoP) increased [6]. However, the mean age in this cohort was 24 years, likely representing a different patient population.
The ideal bearing surface for THA in very young patients remains an important but unanswered question. Historically, it was felt that hard-on-hard bearings (ie, MoM and CoC) were advantageous for their increased longevity [7], but these surfaces have fallen out of favor in the ensuing years, as is made clear with this report.
The use of MoM bearings has declined sharply in all patient populations because of concerns associated with metal ion release leading to adverse reactions to metal debris [2,8,9]. MoP bearings with associated trunnionosis have also been linked with a higher risk for similar adverse reactions and reduced implant survival [10,11]. The decrease in the use of CoC bearings may have resulted from concerns over noise and the small but catastrophic risk of implant fracture [12,13]. The reported incidence of audible squeaking varies depending on head size and the brand of components studied; one study of large-diameter heads in CoC bearings found an increase in the incidence of squeaking after THA from 7.3% at 2 years to 17.4% at 5 years [14]. Examination of the Norwegian Arthroplasty Register between 1997 and 2017 including 31,479 CoP and 5790 CoC articulations found that the survivorship free from revision for ceramic fracture for CoC bearings was 99.8% at 10 years, but the hazard ratio for ceramic head fracture was 3.6 (95% confidence interval, 1.7 to 7.6) for CoC compared with CoP [15]. These results may have tempered interest in the use of CoC in the pediatric population. In addition, the improved wear characteristics and standardization of highly cross-linked polyethylene have further improved hard-on-soft articulations and may be contributing to the changes in national trends reported here [16,17].
This study has several limitations. The bearing surface used was not available for all THAs in the KID as this information is not required for compensation, which raises the possibility of selection bias. In addition, the database did not provide granular information on bearing types such head size, which generation of components were used, or the type of polyethylene used which limits our ability to draw bearing-specific conclusions. Clinical information was derived from a national administrative database populated with ICD-9 and ICD-10 codes, which are entered by hand and therefore subject to human error. However, physician and hospital compensation is based on these codes and therefore is generally highly accurate. Despite the general limitations associated with the use of a national administrative registry, the KID is validated through a federal-state-industry partnership sponsored by the AHRQ and is widely recognized as a reliable source of clinical information that has produced many peer-reviewed publications across a variety of specialties [[18], [19], [20]].
Conclusions
The data presented strongly suggest that the incidence of THAs performed in patients aged <21 years is increasing and that CoP is increasingly popular among arthroplasty surgeons for this age group. Further investigation is warranted to determine if bearing longevity and clinical outcomes with CoP are superior to previously popular bearing surfaces in this particular patient population.
Conflicts of interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: M. Silva has stocks or stock options in Imagen Technologiesand is in the medical/orthopaedic publications editorial/governing board of Journal of Haemophilia and Journal of Children Orthopaedics. E. Zeegen is a paid consultant for Zimmer Biomet and Smith & Nephew; has stock or stock options in Radlink, Inc.; received research support from Zimmer Biomet; is in the medical/orthopaedic publications editorial/governing board of Journal of Arthroplasty and Arthroplasty Today; and is a member of the Evidence Based Medicine Committee of American Association of Hip and Knee Surgeons. R. Thompson is a committee member of Pediatric Orthopaedic Society of North America and American Academy of Cerebral Palsy and Developmental Medicine.
Appendix A. Supplementary data
Appendix
Appendix Table 1.
Identifying patients of interest with International Classification of Diseases, 9th Revision and 10th Revision.
| Procedures | ICD-9 | ICD-10 |
|---|---|---|
| THA | 81.51 | -a |
| MoM | 00.75 | 0SR9019, 0SR901A, 0SR901Z, 0SRB019, 0SRB01A, 0SRB01Z |
| MoP | 00.74 | 0SR9029, 0SR902A, 0SR902Z, 0SRB029, 0SRB02A, 0SRB02Z |
| CoC | 00.76 | 0SR9039, 0SR903A, 0SR903Z, 0SRB039, 0SRB03A, 0SRB03Z |
| COP | 00.77 | 0SR9049, 0SR904A, 0SR904Z, 0SRB049, 0SRB04A, 0SRB04Z |
| Reason for surgery | ||
| Avascular necrosis | 733.40, 733,42, 733.49 | M87.9, M87.00, M87.08, M87.09, M87.10, M87.19, M87.20, M87.28, M87.29, M87.30, M87.38, M87.39, M87.80, M87.88, M87.89, T38.0X5, M87.188, M87.050, M87.051, M87.052, M87.059, M87.150, M87.151, M87.152, M87.159, M87.250, M87.251, M87.252, M87.256, M87.350, M87.351, M87.352, M87.353, M87.850, M87.851, M87.852, M87.859 |
| Osteoarthritis | 715.15, 715.25, 715.35, 715.95, 715.10, 715.20, 715.30, 715.00, 715.80, 715.90 | M1255, M16.0, M16.10, M16.11, M16.12, M16.4, M16.50, M16.51, M16.52, M16.6, M16.7, M16.9 |
| Rheumatoid arthritis | 714.30, 714.31, 714.32, 714.33, 714.0 | M0505, M0515, M0525, M0535, M0545, M0555, M0565, M0575, M0585, M0765, M0805, M0825, M0845, M0885, M0895, M1205, M1215, M1225, M1235, M1245, M1285, M1315, M1385, M1465, M1485, M0500, M0510, M0520, M0530, M0540, M0550, M0560, M0570, M0580, M0760, M0800, M0820, M0840, M0880, M0890, M1200, M1210, M1220, M1230, M1240, M1280, M1310, M1380, M1460, M1480, M0509, M0519, M0529, M0539, M0549, M0559, M0569, M0579, M0589, M0769, M0809, M0829, M0849, M0889, M0899, M1209, M1219, M1229, M1239, M1249, M1289, M1319, M1389, M1469, M1489, M05.9, M08.3, M12.9, M13.0 |
| Congenital deformity | 755.63, 755.69 | Q65.00, Q65.01, Q65.02, Q65.1, Q65.2, Q65.30, Q65.31, Q65.32, Q65.4, Q65.5, Q65.6, Q65.81, Q65.82, Q65.89, Q65.9, M16.2, M16.30, M16.31, M16.32 |
| Osteochondrosis | 732.1, 732.2, 732.6, 732.7, 732.9 | M91.0, M91.10, M91.11, M91.12, M91.20, M91.21, M91.22, M91.30, M91.31, M91.32, M91.40, M91.41, M91.42, M91.80, M91.81, M91.82, M91.90, M91.91, M91.92, M93.001, M93.002, M93.003, M93.011, M93.012, M93.013, M93.021, M93.022, M93.023, M93.031, M93.032, M93.033, M93.80, M93.811, M93.812, M93.819, M93.821, M93.822, M93.829, M93.831, M93.832, M93.839, M93.841, M93.842, M93.849, M93.851, M93.852, M93.859, M93.861, M93.862, M93.869, M93.871, M93.872, M93.879, M93.88, M93.89, M94.1, M94.9, M93.20, M93.251, M93.252, M93.259, M93.28, M93.29, M93.90, M94.251, M94.252, M94.259, M94.351, M94.352, M94.359 |
| Sickle cell | 282.60, 282.61, 282.62, 282.63, 282.64, 282.68, 282.69 | D57.00, D57.01, D57.02, D57.03, D57.09, D57.1, D57.20, D57.211, D57.212, D57.213, D57.218, D57.219, D57.3, D57.40, D57.411, D57.412, D57.413, D57.418, D57.419, D57.42, D57.431, D57.432, D57.433, D57.438, D57.439, D57.44, D57.451, D57.452, D57.453, D57.458, D57.459, D57.80, D57.811, D57.812, D57.813, D57.818, D57.819 |
ICD-9, International Classification of Diseases, 9th Revision; ICD-10, International Classification of Diseases, 10th Revision.
ICD-10 schema integrates THA and bearing type with each procedure.
References
- 1.Kurtz S., Ong K., Lau E., Mowat F., Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007 doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 2.Fabi D., Levine B., Paprosky W. Metal-on-metal total hip arthroplasty: causes and high incidence of early failure. Orthopedics. 2012 doi: 10.3928/01477447-20120621-12. [DOI] [PubMed] [Google Scholar]
- 3.Kim S.-C., Lim Y.-W., Jo W.-L. Fourth-generation ceramic-on-ceramic THA results in improvements in midterm outcomes compared to third-generation THA but does not resolve noise problems: a cohort study of a single-hip system. BMC Musculoskelet Disord. 2019;20(1):263. doi: 10.1186/s12891-019-2641-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Devane P.A., Horne J.G., Ashmore A., Mutimer J., Kim W., Stanley J. Highly cross-linked polyethylene reduces wear and revision rates in total hip arthroplasty: a 10-year double-blinded randomized controlled trial. J Bone Joint Surg Am. 2017;99(20):1703. doi: 10.2106/JBJS.16.00878. [DOI] [PubMed] [Google Scholar]
- 5.Shrader M.W. Total hip arthroplasty and hip resurfacing arthroplasty in the very young patient. Orthop Clin North Am. 2012;43(3):359. doi: 10.1016/j.ocl.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 6.Rajaee S.S., Theriault R.V., Pevear M.E., Smith E.L. National trends in primary total hip arthroplasty in extremely young patients: a focus on bearing surface usage from 2009 to 2012. J Arthroplasty. 2016 doi: 10.1016/j.arth.2016.01.061. [DOI] [PubMed] [Google Scholar]
- 7.D’Antonio J.A., Sutton K. Ceramic materials as bearing surfaces for total hip arthroplasty. J Am Acad Orthop Surg. 2009 [PubMed] [Google Scholar]
- 8.Kovochich M., Finley B.L., Novick R. Understanding outcomes and toxicological aspects of second generation metal-on-metal hip implants: a state-of-the-art review. Crit Rev Toxicol. 2018;48(10):853. doi: 10.1080/10408444.2018.1563048. [DOI] [PubMed] [Google Scholar]
- 9.Kim C.-H., Ryu J.J., Jeong M.Y., Kim J.W., Chang J.S., Yoon P.W. Serum metal ion levels in cementless metal-on-metal total hip arthroplasty: long-term follow-up trends. J Arthroplasty. 2019;34(3):534. doi: 10.1016/j.arth.2018.11.023. [DOI] [PubMed] [Google Scholar]
- 10.Waterson H.B., Whitehouse M.R., Greidanus N.V., Garbuz D.S., Masri B.A., Duncan C.P. Revision for adverse local tissue reaction following metal-on-polyethylene total hip arthroplasty is associated with a high risk of early major complications. Bone Joint J. 2018;100-B(6):720. doi: 10.1302/0301-620X.100B6.BJJ-2017-1466.R1. [DOI] [PubMed] [Google Scholar]
- 11.Metcalfe D., Peterson N., Wilkinson J.M., Perry D.C. Temporal trends and survivorship of total hip arthroplasty in very young patients: a study using the national joint registry data set. Bone Joint J. 2018 doi: 10.1302/0301-620X.100B10.BJJ-2017-1441.R2. [DOI] [PubMed] [Google Scholar]
- 12.Su E.P. Ceramic-ceramic bearing: too unpredictable to use it regularly. HSS J. 2012 doi: 10.1007/s11420-012-9289-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Traina F., De Fine M., Di Martino A., Faldini C. Fracture of ceramic bearing surfaces following total hip replacement: a systematic review. Biomed Res Int. 2013 doi: 10.1155/2013/157247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goldhofer M.I., Munir S., Levy Y.D., Walter W.K., Zicat B., Walter W.L. Increase in benign squeaking rate at five-year follow-up: results of a large diameter ceramic-on-ceramic bearing in total hip arthroplasty. J Arthroplasty. 2018;33(4):1210. doi: 10.1016/j.arth.2017.11.044. [DOI] [PubMed] [Google Scholar]
- 15.Hallan G., Fenstad A.M., Furnes O. What is the frequency of fracture of ceramic components in THA? Results from the Norwegian arthroplasty register from 1997 to 2017. Clin Orthop Relat Res. 2020;478(6):1254. doi: 10.1097/CORR.0000000000001272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Babovic N., Trousdale R.T. Total hip arthroplasty using highly cross-linked polyethylene in patients younger than 50years with minimum 10-year follow-up. J Arthroplasty. 2013 doi: 10.1016/j.arth.2012.12.005. [DOI] [PubMed] [Google Scholar]
- 17.Ayers D.C., Greene M., Snyder B., Aubin M., Drew J., Bragdon C. Radiostereometric analysis study of tantalum compared with titanium acetabular cups and highly cross-linked compared with conventional liners in young patients undergoing total hip replacement. J Bone Joint Surg Am. 2015;97(8):627. doi: 10.2106/JBJS.N.00605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sánchez Fernández I., Stephen C., Loddenkemper T. Disparities in epilepsy surgery in the United States of America. J Neurol. 2017;264(8):1735. doi: 10.1007/s00415-017-8560-6. [DOI] [PubMed] [Google Scholar]
- 19.Safdieh G., Silberman J., Nguyen J. Pediatric septic arthritis and osteomyelitis in the USA: a national KID database analysis. HSS J. 2019;15(2):159. doi: 10.1007/s11420-018-9644-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rumalla K., Smith K.A., Letchuman V., Gandham M., Kombathula R., Arnold P.M. Nationwide incidence and risk factors for posttraumatic seizures in children with traumatic brain injury. J Neurosurg Pediatr. 2018;22(6):684. doi: 10.3171/2018.6.PEDS1813. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.