Abstract
Respiratory pathogens such as Chlamydia pneumoniae may activate osteoclast cells, thereby inducing bone resorption and joint inflammation. Herein is a case report of a young man with misdiagnosed persistent wrist pain without any major trauma. Investigation of the patient's medical history confirmed a recent systemic C. pneumoniae infection. Preoperative X-ray and magnetic resonance imaging (MRI) showed a substantial decrease in cancellous lunate bone compactness. A stepwise approach was undertaken considering the rapid onset of bone devascularisation and the clinical presentation. Wrist arthroscopy confirmed extensive joint inflammation associated with decreased osteochondral lunate solidity. Microbiological examination excluded joint infection. Histological analysis showed a diffuse inflammatory infiltration. Temporary mediocarpal K-wire stabilization and synovectomy were performed. Postoperative MRI confirmed lunate bone revascularization. At 6 and 12 months' follow-up the young man was pain-free and had good recovery of range of motion. In vitro and in vivo studies demonstrate that inflammatory conditions may promote osteoclast cell activity and induce bone resorption. Moreover, infection with C. pneumoniae could activate specific “osteoporotic” bone pathways. To the authors' knowledge, this is the first published case report of specific lunate bone loss induced by systemic C. pneumoniae infection. The authors proposed an etiologic explanation, and a stepwise approach was associated with good outcome.
Keywords: Lunate bone loss, Bone loss infection, Chlamydia pneumonia
Introduction
Bone is a living tissue under constant reconstruction through a balance between bone resorption and bone formation. Microorganisms such as Staphylococcus aureus, Salmonella, and Actinobacillus actinomycetemcomitans have been reported to increase the bone resorption activity of osteoclast cells [[1], [2], [3]].
Chlamydia pneumoniae is a respiratory pathogen that has been shown to disseminate through peripheral blood mononuclear cells and localize in extrapulmonary sites, such as synovial tissue and bone. Studies have demonstrated that C. pneumoniae infection is associated with the development of inflammatory joint disease [4,5]. Moreover, in 2012, Di Pietro et al. reported high rates of C. pneumoniae DNA in osteoporotic bone cells, with an increase in specific interleukins (IL-6, IL1β) [6]. To the authors' knowledge, this is the first published case report of specific bone loss at the wrist joint induced by systemic C. pneumoniae infection.
Case report
A 16-year-old male presented at our department with persistent pain of the dorsal right wrist, particularly in maximum extension, with pain localized between the scaphoid and lunate bone. He reported a minor wrist trauma in maximum extension had occurred four weeks previously. Wrist X-ray conducted immediately after this minor wrist trauma did not show any fracture, direct or indirect signs of ligament lesions or bone damage (Fig. 1). Another X-ray four weeks later, when the patient had been brought to our attention because of persistent wrist pain, showed lunate bone erosion associated with volar intercalated segment instability (VISI) (Fig. 2). MRI was performed to better investigate the wrist joint and vascular lunate supply. The results of MRI excluded any ligament-associated lesions and showed a decrease in cancellous lunate bone compactness similar to that seen with Kienböck disease (Fig. 3). The sudden onset of pain following a minor trauma, the young age of the patient, the absence of any previous type of pain or functional limitation at wrist level and the absence of any direct or indirect sign of lunate bone lesions on previous X-ray led us to further investigate the patient's medical history. Two days after the wrist trauma, the patient developed fever and arthralgia, with a serum white blood cell (WBC) count of 5920/μL and CRP (C-reactive protein) of 4.89 mg/L. He was initially discharged with a broad-spectrum antibiotic. Five days later the patient was hospitalized because of persistent and increasing fever. Blood tests showed increased WBC count (7480/μL) and CRP (27.3 mg/L). Chest X-ray and serum IgM level confirmed the diagnosis of pneumonia due to C. pneumoniae infection. Any other infections were ruled out. The patient was discharged after seven days of intravenous specific antibiotic therapy (clarithromycin) with complete remission of signs and symptoms except for persistent wrist pain.
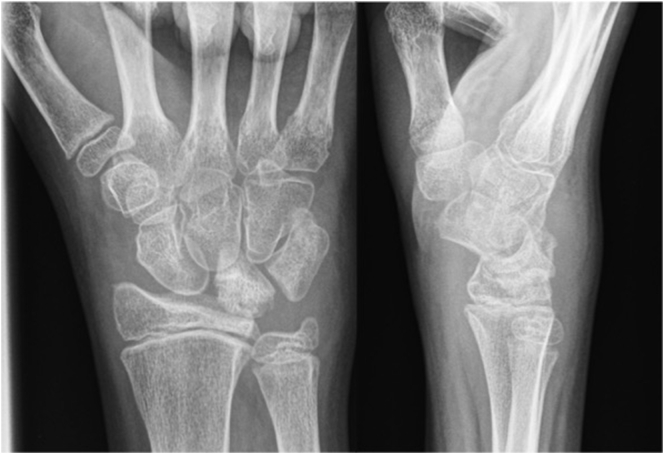
Fig. 1.
X-ray after the minor trauma shows no bone lesion or lunate vascular damage.
Fig. 2.
X-ray 4 weeks after the minor trauma shows lunate bone erosion associated with VISI deformity.
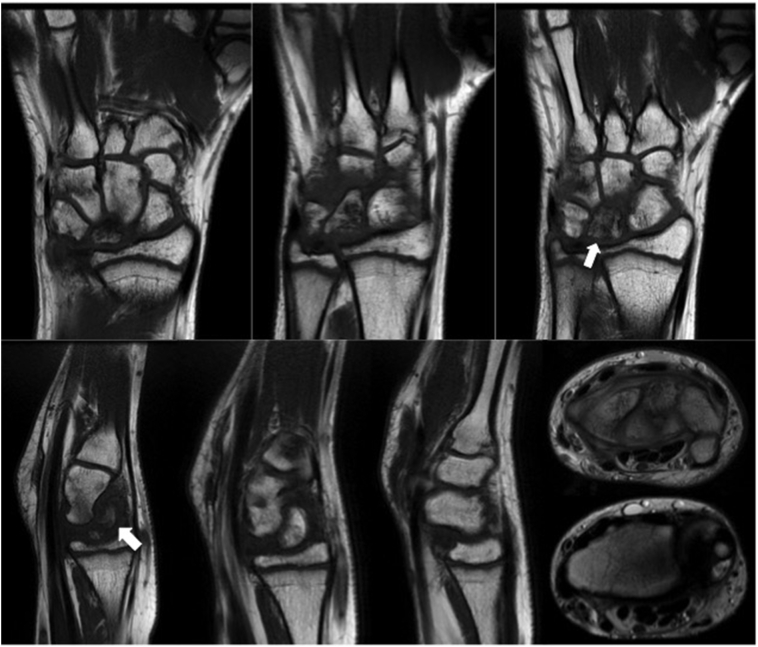
Fig. 3.
Preoperative MRI shows decrease in cancellous lunate bone compactness and vascularity (white arrows).
Considering the non-linear history of pain development, the young age of the patient and the aspect of the lunate bone on MRI, the authors decided to use a stepwise approach. Wrist arthroscopy was conducted using standard wrist portal 3–4/6 U and midcarpal ulnar/midcarpal radial portals (MCU/MCR) to check the quality of the bone, ligament and articular surface and to assess the general condition of the wrist joint. Extensive and diffuse inflammatory synovitis involving the soft tissue around the lunate bone was observed at the radiocarpal and midcarpal level. No associated ligament lesion was found. The radial joint surface was undamaged. The arthroscopic aspect of lunate cartilage was normal but there was extensive synovitis around the lunate surfaces. Decreased osteochondral lunate solidity was observed on assessment of the cartilage lunate surface using the probe. Moreover, the lunate cartilage surface was easily disrupted with the probe, indicating a significant decrease of lunate cancellous bone analogous to osteoporotic bone loss (Fig. 4). Arthroscopic histological and microbiological synovial samples were taken, and debridement of inflammatory synovial tissue and copious joint space washes were performed. The lunate was temporarily stabilized with a luno-triquetral K-wire and the pressure on the lunate bone surface was reduced by a temporary capitate-scaphoid K-wire. The wrist was immobilized for four weeks and then the K-wires were removed.
Fig. 4.
Arthroscopic radiocarpal view. The probe easily disrupts the lunate cartilage surface and a significant decrease in lunate cancellous bone is observed (asterisks).
The microbiological synovial examination was negative for joint infection. The histological sample showed a diffuse inflammatory infiltration with numerous macrophages and mononuclear cells. The patient underwent clinical checks at four weeks postoperatively (at which time the K-wire was removed) and then again at eight weeks. At six-months' follow-up, MRI confirmed the lunate revascularization with an initial asymptomatic VISI deformity (Fig. 5). The patient was pain-free and had complete range of motion (ROM) (Fig. 6) and returned to sport and daily life activities.
Fig. 5.
Postoperative MRI confirms lunate revascularization.
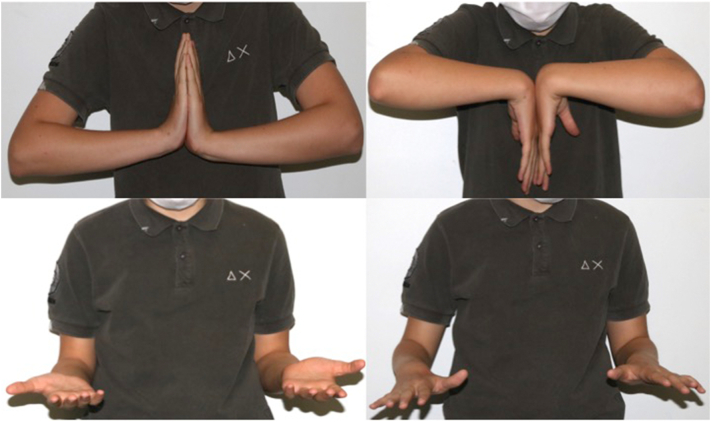
Fig. 6.
Six-months' follow-up. Complete ROM is observed.
Discussion
Chlamydia pneumoniae infection starts in the respiratory tract and usually disseminates in the blood via macrophages (a common reservoir) and peripheral blood mononuclear cells. This microorganism survives in macrophages and in tissues including synovial tissue and bone [4,5].
In vitro [7] and in vivo [6] studies demonstrate that an inflammatory condition may promote the recruitment of macrophages and peripheral blood mononuclear cells in synovial and bone tissues, stimulating the production of interleukins (IL-6, IL-1 and TNF-α). In these tissues, the inflammation induced by C. pneumoniae infection elicits a soluble receptor activator of nuclear factor (NF)-kB ligand (sRANKL)-pathway-mediated osteoclast activity. The osteoclasts could create an “osteoporotic” condition with decreased cancellous bone solidity [8,9]. Herein is reported the case of a young patient affected by pneumonia due to C. pneumoniae confirmed by blood serum test, chest X-ray and medical history. The patient reported persistent wrist pain following a minor wrist trauma that had no signs of fracture or damage on X-ray. MRI highlighted substantially decreased cancellous bone solidity of the lunate bone; however, Kienböck disease was excluded considering the sudden onset of the pain, the young age of the patient and the absence of any previous symptoms. Moreover, the wrist X-ray performed immediately after the minor trauma did not show any direct or indirect sign of advanced lunate avascular necrosis.
Considering the history of C. pneumoniae infection the authors presumed that the bone loss could be because of the effect of this microorganism at wrist level with a specific tropism for the lunate bone that was increased by the minor trauma. Diffuse inflammatory synovitis was observed on arthroscopic wrist evaluation and decreased cancellous lunate bone solidity was seen on MRI. Histological findings included numerous macrophages and peripheral blood mononuclear cells in synovial and bone tissues. The minor wrist trauma caused an inflammatory response at wrist level concomitant with C. pneumoniae infection. This microorganism, as reported in the literature, could increase and directly activate osteoclast bone activity leading to severe reduction of bone solidity [6,9].
To the authors' knowledge, this is the first published case report of specific lunate bone loss induced by systemic C. pneumoniae infection. Considering the non-linear pattern of presentation, a stepwise approach was recommended. First, the patient's medical history was investigated to ascertain whether a systemic condition could explain the wrist symptoms reported by the patient. Second, imaging investigations like MRI could be useful to provide information about the wrist joint and bone condition but the authors suggest a wrist arthroscopy approach to better understand and test the inflammatory condition and bone solidity. Histological and microbiological assessment could be useful to confirm the diagnosis. The authors proposed conservative treatment, including stabilizing and decreasing the load charging at the affected bone and synovial debridement. In this case, a stepwise approach led to a good outcome for the patient, including decreased pain and restoration of wrist ROM. Moreover, wrist arthroscopy decreased local inflammation, thereby reducing the risk of sustained bone resorption. Postoperative MRI confirmed a good outcome in terms of lunate bone revascularization, pain reduction and recovery of ROM. The initial VISI deformity and imperfect lunate shape require strict follow-up and possible further surgery should the patient become clinically symptomatic.
Contributor Information
Daniele Tosi, Email: tosi.da@gmail.com.
Giuseppe Caserta, Email: caserta.giuseppe@aou.mo.it.
Roberto Adani, Email: adani.roberto@aou.mo.it.
References
- 1.Marriott I. Osteoblast responses to bacterial pathogens: a previously unappreciated role for bone-forming cells in host defense and disease progression. Immunol. Res. 2004;30:291–308. doi: 10.1385/IR:30:3:291. [DOI] [PubMed] [Google Scholar]
- 2.Teng Y.T., Nguyen H., Gao X., Kong Y.Y., Gorczynski R.M., Singh B. Functional human T-cell immunity and osteoprotegerin ligand control alveolar bone destruction in periodontal infection. J. Clin. Invest. 2000;106:59–67. doi: 10.1172/jci10763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Henderson B., Nair S.P., Ward J.M., Wilson M. Molecular pathogenicity of the oral opportunistic pathogen Actinobacillus actinomycetemcomitans. Annu. Rev. Microbiol. 2003;57:29–55. doi: 10.1146/annurev.micro.57.030502.090908. [DOI] [PubMed] [Google Scholar]
- 4.Gracey E., Inman R.D. Chlamydia-induced ReA: immune imbalances and persistent pathogens. Nat. Rev. Rheumatol. 2011;8:55–59. doi: 10.1038/nrrheum.2011.173. [DOI] [PubMed] [Google Scholar]
- 5.Villareal C., Whittum-Hudson J.A., Hudson A.P. Persistent Chlamydiae and chronic arthritis. Arthritis Res. 2002;4:5–9. doi: 10.1186/ar382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Di Pietro M., Schiavoni G., Sessa V., Pallotta F., Costanzo G., Sessa R. Chlamydia pneumoniae and osteoporosis-associated bone loss: a new risk factor? Osteoporos. Int. 2013;24:1677–1682. doi: 10.1007/s00198-012-2217-1. [DOI] [PubMed] [Google Scholar]
- 7.Bailey L., Engström P., Nordström A., Bergström S., Waldenström A., Nordstöm P. Chlamydia pneumoniae infection results in generalized bone loss in mice. Microbes Infect. 2008;10:1175–1181. doi: 10.1016/j.micinf.2008.06.010. [DOI] [PubMed] [Google Scholar]
- 8.Lacey D.L., Timms E., Tan H.L., Kelley M.J., Dunstan C.R., Burgess T. Osteoprotegerin ligand is a cytokine that regulates osteoclast differentiation and activation. Cell. 1998;93:165–176. doi: 10.1016/s0092-8674(00)81569-x. [DOI] [PubMed] [Google Scholar]
- 9.Simonet W.S., Lacey D.L., Dunstan C.R., Kelley M., Chang M.S., Lüthy R. Osteoprotegerin: a novel secreted protein involved in the regulation of bone density. Cell. 1997;89:309–319. doi: 10.1016/s0092-8674(00)80209-3. [DOI] [PubMed] [Google Scholar]