Abstract
Background: Treatment of proximal interphalangeal joint (PIPJ) fracture-dislocations is difficult given the potential long-term complications of the involved finger and entire hand. Several surgical methods have been utilized for management of these injuries, none of which have shown consistently favorable results. The purpose of this systematic review of the literature is to report the post-operative outcomes of multiple treatment modalities for PIPJ fracture-dislocations in various studies. Methods: A literature review of PubMed and EMBASE databases was performed for all articles on PIPJ fracture-dislocations. Outcomes of interest included PIPJ range of motion, grip strength (% of contralateral hand), and quick disabilities of arm, shoulder, hand (QuickDASH). Articles were distributed into 5 groups by surgical method: open reduction, percutaneous fixation, dynamic external fixation, extension-block pinning, and hemi-hamate arthroplasty. Results: Forty-eight of 1679 total screened articles were included. The weighted means of post-operative range of motion (ROM; degrees) at final follow-up were open reduction 84.7 (n = 146), percutaneous fixation 86.5 (n = 32), dynamic external fixation 81.7 (n = 389), extension-block pinning 83.6 (n = 85), and hemi-hamate arthroplasty 79.3 (n = 52). Dorsal fracture-dislocations, regardless of surgical method, had an average ROM of 83.2 (n = 321), grip strength 91% (n = 132), and QuickDASH of 6.6 (n = 59) while pilon injuries had an average ROM of 80.2 (n = 48), grip strength 100% (n = 13), and QuickDASH of 11.4 (n = 13). Conclusion: Percutaneous fixation yielded the highest post-operative ROM at final follow-up while extension-block pinning resulted in the greatest grip strength. While dorsal fracture-dislocations produced higher average ROM and lower QuickDASH score, pilon fractures produced a higher grip strength. No treatment method or fracture type yielded consistently better outcomes than another.
Keywords: digits, anatomy, finger, fracture/dislocation, diagnosis, hand therapy, specialty, surgery
Introduction
The proximal interphalangeal joint (PIPJ) accounts for approximately 85% of joint motion that enables grasping an object, 1 thus fracture-dislocations or fracture-subluxations can have an immense impact upon hand utility. PIPJ fracture-dislocations can result in significant digit range of motion (ROM) limitation and subsequent occupational disability. Furthermore, PIPJ fracture-dislocations with suboptimal treatment can present as chronic joint instability, pain, osteoarthritis, and intra-articular deformity. These potential complications result in a hand injury that has historically been difficult to treat. 2
Current treatment modalities are open reduction, percutaneous fixation, dynamic external fixation, extension block pinning, and hemi-hamate arthroplasty. The dynamic external fixator technique most commonly involved either a Suzuki frame, 3 Ligamentotaxor® device, or application of a pins and rubber bands system with Kirschner wires (K-wires). Although extensive methods of surgical management have been described, few studies provide direct comparison among techniques and there remains a lack of consensus on the best approach to fracture-dislocation treatment. The purposes of this study were to review current literature on PIPJ fracture-dislocation modes of surgical repair (open reduction, percutaneous fixation, dynamic external fixation, extension block pinning and hemi-hamate arthroplasty) and analyze validated surgical and functional outcomes to determine efficacy of the numerous techniques in an acute setting. We hypothesize that no significant difference in patient outcomes will exist between the varying surgical methodologies and that no one method will result in better patient outcomes across the board.
Materials and Methods
Study Selection
A literature search was performed on January 21, 2019 via the electronic databases PubMed and EMBASE utilizing the search terms “PIP fracture dislocation” OR “proximal interphalangeal fracture.” Articles in the literature searched ranged from 1946 through January 2019. All articles subsequently underwent a two-step review process by two independent reviewers: (1) article title and abstract were reviewed and (2) those articles meeting eligibility criteria underwent a full text review.
Eligibility Criteria
Inclusion criteria for articles included: (1) English-language articles; (2) levels of evidence I through IV; (3) specification of a fracture with dislocation injury with fracture type provided; (4) specification of the type of repair performed; (5) repairs that were treated in an acute phase (<6 weeks from injury to surgery); and (6) inclusion of clinical outcomes data. Exclusion criteria included: (1) non-English articles; (2) review articles; (3) case reports, (4) studies evaluating PIPJ arthroplasty; (5) studies evaluating newly implemented surgical procedures or technique guides; (6) outcome measures of chronic fracture injuries (>6 weeks to surgery); (7) provided fracture types without a dislocation; (7) not specifying the type of repair performed; (8) no reporting data separated by type of operative treatment, and finally; (9) not reporting patient-reported measures of functional outcomes.
Data Abstraction/Analysis
Two independent reviewers examined the selected full-text articles after abstract review for inclusion. Data including patient characteristics, repair methodology, repair metrics, and functional outcomes was extracted from the articles selected for inclusion. The outcomes most commonly reported were ROM, grip strength, and Disabilities of the Arm, Shoulder, and Hand (QuickDASH) score.
ROM was reported as the arc of flexion-extension in degrees. The grip strength was reported as a percentage of injured hand strength to contralateral uninjured extremity. The QuickDASH is a patient-reported questionnaire composed of 11 questions pertaining to disability and severity of symptoms totaling to a maximum score of 100 with higher scores correlating to increased disability and symptoms. 4 Weighted averages were calculated using studies that provided one or more of the above metrics. A meta-analysis could not be performed due to the heterogeneity of literature collected.
Results
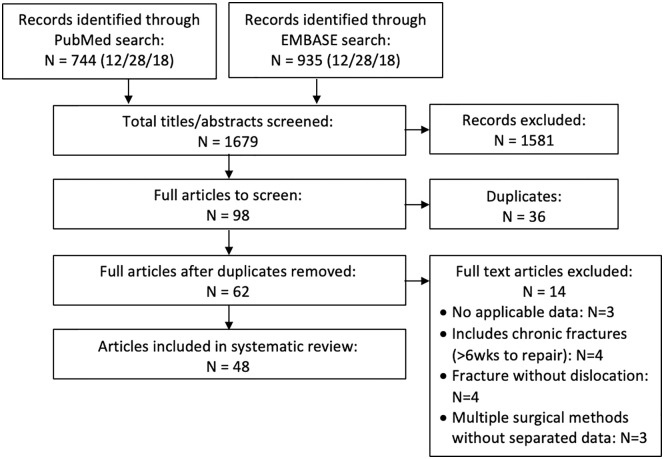
A total of 1936 articles were identified (Figure 1) with 98 articles identified that met eligibility requirements in the first review of abstract titles and abstracts. A total of 36 duplicate articles were removed. Full text review was performed on 62 articles, and 14 articles were excluded.
Figure 1.
Literature search process.
A total of 48 articles were included in the final review,5-52 25 of which reported data on dynamic external fixation, 12 on open reduction, 6 on hemi-hamate arthroplasty, 4 on extension block pinning, and 3 on percutaneous fixation. Two studies reported data on more than one group.17,48 Additionally, of the 48 articles included in the final review, 29 articles provided identification of fracture type. Of these 29 articles that underwent final review and identified fracture type, 26 reported data on dorsal fracture-dislocations, 5 reported data on pilon fracture-dislocations, and 1 on volar fracture-dislocations, with 1 article reporting two fracture types, 10 and 1 article reporting data on all three fracture types. 18
Patient Characteristics
Appendix A lists patient and study characteristics in more detail. Of the 48 articles included, data were available for 746 hands from 735 patients. In the open reduction internal fixation group (144 patients; 146 hands), 27% of patients were female and the average age for all patients was 32.2 years. In articles reporting involved finger, 42% of injuries involved the ring finger, 26% the middle finger, 25% the pinky finger, and 7% the index finger. Average time to surgery was 8.3 days, and average time for follow-up was 37.4 months. In the percutaneous fixation group (31 patients; 32 hands), 40% of patients were female; average age was 28.8 years. The ring finger accounted for 41% of the injuries, the pinky finger accounted for 31%, the middle finger 18.8%, and the index finger 9.4%. Average time to surgery was 4.6 days with an average follow-up of 74.7 months. In the dynamic external fixation group (427 patients; 431 hands), 30% of patients were female; average age was 36.1 years. In articles reporting involved finger, 38% were ring finger injuries, 34% pinky finger injuries, 17.7% middle finger injuries, and 10.6% were to the index finger. Articles with data for dynamic external fixation reported an average of 7.8 days with an average follow-up of 16.1 months. In the extension block pinning group (81 patients; 85 hands), 40% of patients were female; average age was 34.3 years. Thirty-eight percent of injuries involved the ring finger, 24.7% the middle finger, 18% the pinky finger, and 20% the index finger. Average time to surgery was 8.4 days with a mean follow-up of 42.4 months. In the hemi-hamate arthroplasty group (52 patients; 52 hands), 50% were female with an average age of 37.8 years. Articles reporting which finger was injured resulted in 53% ring finger, 25% middle finger, 13.9% index finger, and 8% pinky finger. Average time to surgery was 18.9 days for articles which reported this metric, and average length of follow-up was 25 months.
Categorizing studies upon fracture type, in the dorsal fracture-dislocation group (340 patients; 347 hands) 30% of reported patients were female with an average age of 33.5 years. Reported injuries by finger involved the ring finger in 44% of patients, middle finger in 24.5%, pinky finger in 20%, and index finger in 12%. Average time to surgery was 11.3 days (with average follow up of 35.6 months). For pilon fracture-dislocations (59 patients; 61 hands), 30% of patients were female; average age was 37 years. Fifty-two percent of fractures involved the pinky finger, 37% the ring finger, 8.7% middle finger, and 2.2% the index finger. Average time to surgery was 4.7 days, while average follow-up was 19.4 months. Finally, only 1 study reported a volar fracture-dislocation (3 patients; 3 hands) with 66.7% of patients being female. Average age was 45 years with all fractures involving the pinky digit and no time to surgery or follow-up was provided. Data on volar fracture-dislocations were not included in Table 2 due to lack of patients compared to other fracture type groups.
Table 2.
Surgical Outcome Data by Fracture-Dislocation Type.
| Fracture-dislocation type | n = | Avg. ROM (degrees) | n = | Avg. grip strength (%) | n = | Avg. QuickDASH |
|---|---|---|---|---|---|---|
| Dorsal | 321 | 83.2 | 132 | 91 | 59 | 6.6 |
| Pilon | 48 | 80.2 | 13 | 100 | 13 | 11.4 |
Note. ROM = range of motion.
Clinical Outcomes
The full list of outcomes can be seen in Tables 1 and 2. The ROM (in degrees) was reported in all open reduction studies (n = 14; 146 hands), all percutaneous fixation studies (n = 3; 32 hands), 27 dynamic external fixation studies (389 hands), all extension block pinning studies (n = 4; 85 hands), and all hemi-hamate arthroplasty studies (n = 6; 52 hands). Preoperative scores were not provided for the ROM metric, however, postoperative weighted average ranges were 84.7°, 86.5°, 81.7°, 83.6°, and 79.3°, respectively.
Table 1.
Surgical Outcome Data by Repair Method.
| Repair type | n = | Avg. ROM | n = | Avg. grip strength (%) |
|---|---|---|---|---|
| Open reduction internal fixation | 146 | 84.7 | 13 | 85 |
| Percutaneous fixation | 32 | 86.5 | 0 | n/a |
| Dynamic external fixation | 389 | 81.7 | 102 | 89 |
| Extension block pinning | 85 | 83.6 | 53 | 95 |
| Hemi-hamate arthroplasty | 52 | 79.3 | 41 | 85 |
Note. ROM = range of motion.
Grip strength was reported in one open reduction studies (13 hands), 8 dynamic external fixation studies (102 hands), 3 extension block pinning studies (53 hands), and 4 hemi-hamate arthroplasty studies (41 hands). Preoperative scores were not provided for grip strength. Postoperative weighted average grip strengths compared to contralateral hand were 85%, 89%, 95%, and 85%, respectively. Grip strength was not provided in any percutaneous fixation studies.
The QuickDASH was not reported in a high enough quantity in surgical subtypes for continuous weighted average measures. The ROM (in degrees) was reported in 29 patient populations that had dorsal fracture dislocations (321 hands) and 5 pilon fracture-dislocation patient populations (48 hands). ROM was not reported in the article with data on volar fracture dislocations. Preoperative scores were not provided for ROM metric; postoperative weighted scores were 83.2° and 80.2°, respectively.
Grip strength was reported in 8 patient populations that had dorsal fracture dislocations (132 hands), 1 pilon fracture dislocation patient population (13 hands) and in the only study with data on volar fracture dislocations (3 hands). Preoperative scores were not provided for grip strength metric; postoperative weighted scores were 91°, 100°, and 76°, respectively. The QuickDASH was reported in 4 studies on dorsal fracture dislocations (59 hands), 1 study reporting on pilon fracture dislocations (13 hands), and in 1 study on volar fracture dislocations (3 hands). Preoperative scores were not provided for QuickDASH metric; post-operative weighted scores were 6.6, 11.4, and 9.1, respectively.
Discussion
This study provides an extensive literature review of surgical management approaches in the acute setting of PIPJ fracture-dislocation care. We found that no surgical treatment method yielded consistently greater average outcome data to others across different outcome measures. Percutaneous fixation yielded the greatest average ROM of the PIPJ postoperatively followed by open reduction. Hemi-hamate arthroplasty yielded the lowest average post-operative ROM. Extension-block pinning methods resulted in the greatest grip strength at final follow up compared to the contralateral hand.
Additionally, this study analyzed post-operative outcomes among fracture-dislocation types. Cause of injury through direct blow, hyperflexion, or axial loading are common causes that can result in proximal, dorsal, and pilon fracture-dislocations, respectively. 1 When analyzing the fracture-dislocation type, dorsal and pilon fracture-dislocations had similar post-operative ROM, although the average QuickDASH score was higher when patients presented with pilon fracture-dislocations. Average grip strength was greater post-operatively among pilon fracture-dislocations in comparison to dorsal fracture-dislocations.
Few studies examine post-operative results among PIPJ fracture-dislocation management strategies. Stern et al 48 evaluated both skeletal traction and open reduction. Neither surgical approach resulted in superior post-operative measures; both approaches reported mild reduction in PIPJ motion. Barksfield et al 17 assessed hemi-hamate arthroplasty outcomes compared to trans-articular K-wire fixation. Between these two surgical methods, the authors concluded that both techniques were equivalent in post-surgical measurements. Variations in patient injury acuity, post-operative follow-up period and individual study assessments limits direct comparison ability among surgical literature.
The goal of surgery for PIPJ fracture-dislocations is reduction of the middle phalanx onto the condyles of the proximal phalanx. Indications for surgical treatment of these injuries include >40% of the joint involved in an unstable fracture or failure of closed reduction. Percutaneous fixation is often used for large fragments with lack of comminution and involves fixation of fragments using K-wires. Open reduction internal fixation is indicated for large fragments without comminution when adequate reduction cannot be provided by percutaneous fixation. Dynamic external fixation is indicated for highly comminuted pilon fractures. Extension block splinting can be used for stable and unstable dorsal fracture-dislocations. Hemi-hamate arthroplasty is used for comminuted fractures involving the palmar lip or lateral plateau of the middle phalanx or for salvage after failure of other surgical methods. While each method has general indications as noted above, there is great variability for each fracture-dislocation based on the fracture characteristics and surgeon preference and experience. Post-operative rehabilitation after PIPJ fracture-dislocation also varies greatly by surgeon and institution; however, general mainstays of treatment include early passive ROM exercises as allowed by stability of the fixation construct. Disparity in post-operative rehabilitation is a potential source of variation in the results of this review.
This literature review has several constraints. Although only validated data were included, the heterogeneous composition of articles reviewed made direct comparisons challenging. Particularly, the reported measures differed between articles, making it difficult to perform a meta-analysis. Lack of standardized outcome measures not only resulted in reporting variability, but also in presentation of reported information (i.e. grip strength reported as a percentage of the contralateral hand versus in kilograms). Additionally, fracture-dislocation subtype was not specified in certain studies, which, if reported consistently, could have further enhanced this review, notably with the QuickDASH score. This review is also limited to a literature body of predominately case series, and therefore control studies are required to assess beyond correlation.
In this review, we report that no surgical approach to PIPJ fracture-dislocation management yielded consistently higher average post-operative function data through a literature evaluation of post-operative outcomes. Treatment of this hinge joint requires delicate decision-making that ultimately is based upon fracture type, area of affected joint space and size of fracture. We recommend standardization of reported outcomes such as average ROM, average grip strength, and average QuickDASH. Randomized trials are ultimately the gold standard to methodically compare surgical modalities and could help determine the standard of care in PIPJ fracture-dislocation treatment. The lack of universal and widely accepted outcome results as well as injury classification systems and relatively small incidence of PIPJ fracture-dislocations makes it difficult for outcome-based studies with controls to be performed. A multi-institutional study involving a standardized patient reported outcome system would provide strong evidence as to which surgical method yields greater patient outcomes.
Appendix
Appendix A.
| Author | Year | Number of Hands | M/F | Avg. Age (years) | Avg. time to surgery (days) | Avg. follow up time (mo.) | PIPJ ROM (°) | Grip Strength (%) | Quick DASH |
|---|---|---|---|---|---|---|---|---|---|
| Open Reduction (n=14) | |||||||||
| 17 Barksfield | 2015 | 12 | 9/3 | 40 | 3 | 56 | |||
| 20 Lee | 2013 | 9 | 8/1 | 31 | 9 | 93.2 | |||
| 22 Cheah | 2012 | 13 | 11/2 | 33 | 7 | 25 | 75 | 85 | 4 |
| 31 Hamilton | 2006 | 9 | 7/2 | 35 | 17 | 42 | 70 | ||
| 32 Lee | 2006 | 12 | 8/2 | 30 | 9.2 | 8 | 85 | ||
| 33 Grant | 2005 | 14 | 13/1 | 30 | 21 | 39 | 94 | ||
| 34 Aladin | 2005 | 8 | 8/0 | 33 | 84 | 82 | |||
| 34 Aladin | 2005 | 6 | 5/1 | 42 | 84 | 84 | |||
| 34 Aladin | 2005 | 5 | 4/1 | 32 | 84 | 80 | |||
| 36 Khan | 2004 | 3 | 3/0 | 24.7 | 7.33 | 61 | 100 | ||
| 43 Weiss | 1996 | 12 | 10/2 | 27.3 | 6 | 25.2 | 89 | ||
| 46 Eglseder | 1992 | 6 | 36 | 3.5 | 5.5 | 93 | |||
| 48 Stern | 1991 | 9 | 7/2 | 32 | 1 | 27 | 70 | ||
| 52 Larsen | 2000 | 28 | 16/12 | 25 | 3 | 27 | 100 | ||
| Percutaneous Fixation (n=3) | |||||||||
| 24 Vitale | 2011 | 6 | 3/3 | 32 | 4 | 18 | 93 | ||
| 27 Ikeda | 2009 | 15 | 10/5 | 25.5 | 5.1 | 14.2 | 84.9 | ||
| 42 Newington | 2001 | 11 | 9/1 | 192 | 85 | ||||
| Dynamic External Fixation (n=30) | |||||||||
| 7 Kodama | 2018 | 9 | 7/2 | 22.6 | 4.7 | 11.1 | 94.6 | ||
| 5 Awad | 2018 | 12 | 8/4 | 36 | 4 | 6 | 90.8 | 78 | 12.3 |
| 8 Kostoris | 2017 | 4 | 3/1 | 49.5 | 6.5 | 6 | 60 | 21 | |
| 10 Abou Elatta | 2017 | 21 | 37 | 12 | 90 | ||||
| 10 Abou Elatta | 2017 | 15 | 37 | 12 | 83 | ||||
| 14 Pelissier | 2015 | 88 | 69/17 | 38.8 | 15.2 | 70 | 15.7 | ||
| 13 MacFarlane | 2015 | 28 | 19/9 | 33.9 | 7 | 22 | 85 | 20.3 | |
| 12 Shen | 2015 | 10 | 3/7 | 48 | 27.5 | 23.7 | 83.9 | ||
| 16 Colegate-Stone | 2015 | 12 | 12/0 | 29 | 10 | 3.5 | 65 | 9.1 | |
| 18 Nilsson | 2014 | 26 | 19/7 | 29 | 92 | 4.5 | |||
| 18 Nilsson | 2014 | 3 | 1/2 | 45 | 76 | 9.1 | |||
| 18 Nilsson | 2014 | 13 | 7/6 | 45 | 100 | 11.4 | |||
| 6 Hirth | 2013 | 5 | 4/1 | 43 | 9.2 | 7 | 96.6 | ||
| 26 Korting | 2009 | 15 | 8/7 | 47.3 | 2.7 | 10 | 76.3 | 86 | |
| 28 Ruland | 2008 | 34 | 27/7 | 30 | 16 | 93 | |||
| 29 Ellis | 2007 | 8 | 8/0 | 27 | 5.8 | 26 | 88 | 92 | |
| 29 Ellis | 2007 | 6 | 5/1 | 39 | 8 | 6 | 69 | ||
| 30 Theivendran | 2007 | 11 | 10/1 | 35.9 | 7.6 | 23.5 | 62.2 | 86 | |
| 35 Badia | 2005 | 6 | 4/2 | 27 | 6 | 24 | 84 | ||
| 37 Deshmukh | 2004 | 14 | 11/3 | 37 | 4.5 | 34 | 85 | 92 | |
| 39 Duteille | 2003 | 20 | 18/2 | 30.1 | 3.3 | 18 | 92.2 | ||
| 40 Syed | 2003 | 9 | 6/2 | 43 | 6 | 26.4 | 79 | ||
| 41 De Smet | 2002 | 8 | 7/1 | 35.4 | 23.5 | 16.5 | 91.3 | ||
| 44 Morgan | 1995 | 14 | 8/6 | 35 | 4 | 24 | 89 | ||
| 45 Inanami | 1993 | 4 | 4/0 | 32 | 5 | 17 | 95 | ||
| 48 Stern | 1991 | 7 | 7/0 | 29 | 1 | 24 | 80 | ||
| 49 Kubitskiy | 2014 | 10 | 8/2 | 34 | 6 | 83.5 | |||
| 50 Keramidas | 2007 | 6 | 19.8 | 96 | |||||
| 50 Keramidas | 2007 | 5 | 16.5 | 87.5 | |||||
| 51 Hynes | 2001 | 8 | 6/1 | 36 | 10.7 | 7.71 | 88 | ||
| Extension Block Pinning (n=4) | |||||||||
| 11 Waris | 2016 | 41 | 24/15 | 44 | 9 | 62 | 80 | 93 | |
| 15 Bear | 2015 | 12 | 7/5 | 30 | 7.5 | 35.5 | 84 | 100 | 5.7 |
| 23 Waris | 2010 | 18 | 12/4 | 36 | 9 | 58 | 83 | ||
| 47 Inoue | 1991 | 14 | 13/1 | 27 | 8 | 14.2 | 94.4 | ||
| Hemi-Hamate Arthroplasty (n=6) | |||||||||
| 9 Burnier | 2017 | 9 | 39 | 24 | 86 | 76 | 7 | ||
| 17 Barksfield | 2015 | 7 | 7/0 | 39 | 4 | 65 | |||
| 19 Yang | 2014 | 11 | 8/3 | 30 | 4 | 38.1 | 85.4 | 95 | |
| 21 Lindenblatt | 2013 | 4 | 4/0 | 41 | 4.5 | 8 | 78.8 | ||
| 25 Afendras | 2010 | 8 | 5/3 | 49 | 22 | 60 | 67 | 90 | 19 |
| 38 Williams | 2003 | 13 | 4/9 | 29 | 45 | 16 | 85 | 80 | |
Note. PIPJ = proximal interphalangeal joint; ROM = range of motion.
Footnotes
Ethical Approval: This study was a systemtic review using data published by other authors in publically available literature and thus did not require approval by an institutional review board.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: Informed consent was obtained when necessary.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Cory Demino  https://orcid.org/0000-0002-5066-0790
https://orcid.org/0000-0002-5066-0790
References
- 1. Blazar PE, Steinberg DR. Fractures of the proximal interphalangeal joint. J Am Acad Orthop Surg. 2000;8:383-390. [DOI] [PubMed] [Google Scholar]
- 2. Giugale JM, Wang J, Kaufmann RA, et al. Mid-term outcomes after open reduction internal fixation of proximal interphalangeal joint dorsal fracture-dislocations through a volar, shotgun approach and a review of the literature. Open Orthop J. 2017;11:1073-1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Suzuki Y, Matsunaga T, Sato S, Yokoi T. The pins and rubbers traction system for treatment of comminuted intraarticular fractures and fracture-dislocations in the hand. J Hand Surg Br. 1994;19(1):98-107. [DOI] [PubMed] [Google Scholar]
- 4. Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (Disabilities of the Arm, Shoulder and Hand). Am J Ind Med. 1996;29(6):602-608. [DOI] [PubMed] [Google Scholar]
- 5. Awad GA, Everton F, Downs M, et al. Outcomes of the use of Ligamentotaxor® for proximal interphalangeal fractures of the hand: North Bristol hand centre experience. Eur J Plast Surg. 2018;41(5):613-616. [Google Scholar]
- 6. Hirth MJ, Jacobs DJ, Sleep K. Hand-based swing traction splinting for intra-articular proximal interphalangeal joint fractures. Hand Ther. 2013;18(2):42-56. [Google Scholar]
- 7. Kodama A, Sunagawa T, Nakashima Y, et al. Joint distraction and early mobilization using a new dynamic external finger fixator for the treatment of fracture-dislocations of the proximal interphalangeal joint. J Orthop Sci. 2018;23(6):959-966. [DOI] [PubMed] [Google Scholar]
- 8. Kostoris F, Canton G, Longo E, et al. Treatment of dorsal fracture-dislocation of the proximal interphalangeal joint using the Ligamentotaxor device: clinical and radiographic preliminary results. Acta Biomed. 2017;88(suppl 4):90-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Burnier M, Awada T, Marin Braun F, et al. Treatment of unstable proximal interphalangeal joint fractures with hemi-hamate osteochondral autografts. J Hand Surg Eur Vol. 2017;42(2):188-193. [DOI] [PubMed] [Google Scholar]
- 10. Abou Elatta MM, Assal F, Basheer HM, et al. The use of dynamic external fixation in the treatment of dorsal fracture subluxations and pilon fractures of finger proximal interphalangeal joints. J Hand Surg Eur Vol. 2017;42(2):182-187. [DOI] [PubMed] [Google Scholar]
- 11. Waris E, Mattila S, Sillat T, et al. Extension block pinning for unstable proximal interphalangeal joint dorsal fracture dislocations. J Hand Surg Am. 2016;41(2):196-202. [DOI] [PubMed] [Google Scholar]
- 12. Shen XF, Mi JY, Rui YJ, et al. Delayed treatment of unstable proximal interphalangeal joint fracture-dislocations with a dynamic external fixator. Injury. 2015;46(10):1938-1944. [DOI] [PubMed] [Google Scholar]
- 13. MacFarlane RJ, Gillespie S, Cashin F, et al. Treatment of fracture subluxations of the proximal interphalangeal joint using a ligamentotaxis device: a multidisciplinary approach. J Hand Surg Eur Vol. 2015;40(8):825-831. [DOI] [PubMed] [Google Scholar]
- 14. Pelissier P, Gobel F, Choughri H, et al. Proximal interphalangeal joint fractures treated with a dynamic external fixator: a multicenter and retrospective study of 88 cases. Chir Main. 2015;34(5):245-250. [DOI] [PubMed] [Google Scholar]
- 15. Bear DM, Weichbrodt MT, Huang C, et al. Unstable dorsal proximal interphalangeal joint fracture-dislocations treated with extension-block pinning. Am J Orthop (Belle Mead NJ). 2015;44(3):122-126. [PubMed] [Google Scholar]
- 16. Colegate-Stone T, Marenah K, Compson J, et al. Functional outcomes following pilon fractures of the middle phalanx managed with the ligamentotaxor external fixator. Hand Surg. 2015;20(2):285-289. [DOI] [PubMed] [Google Scholar]
- 17. Barksfield RC, Bowden B, Chojnowski AJ. Hemi-hamate arthroplasty versus transarticular Kirschner wire fixation for unstable dorsal fracture-dislocation of the proximal interphalangeal joint in the hand. Hand Surg. 2015;20(1):115-119. [DOI] [PubMed] [Google Scholar]
- 18. Nilsson JA, Rosberg HE. Treatment of proximal interphalangeal joint fractures by the pins and rubbers traction system: a follow-up. J Plast Surg Hand Surg. 2014;48(4):259-264. [DOI] [PubMed] [Google Scholar]
- 19. Yang DS, Lee SK, Kim KJ, et al. Modified hemihamate arthroplasty technique for treatment of acute proximal interphalangeal joint fracture-dislocations. Ann Plast Surg. 2014;72(4):411-416. [DOI] [PubMed] [Google Scholar]
- 20. Lee JJ, Park HJ, Choi HG, et al. Open reduction of proximal interphalangeal fracture-dislocation through a midlateral incision using absorbable suture materials. Arch Plast Surg. 2013;40(4):397-402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lindenblatt N, Biraima A, Tami I, et al. Hemi-hamate autograft arthroplasty for acute and chronic PIP joint fracture dislocations. Handchir Mikrochir Plast Chir. 2013;45(1):13-19. [DOI] [PubMed] [Google Scholar]
- 22. Cheah AE, Tan DM, Chong AK, et al. Volar plating for unstable proximal interphalangeal joint dorsal fracture-dislocations. J Hand Surg Am. 2012;37(1):28-33. [DOI] [PubMed] [Google Scholar]
- 23. Waris E, Alanen V. Percutaneous, intramedullary fracture reduction and extension block pinning for dorsal proximal interphalangeal fracture-dislocations. J Hand Surg Am. 2010;35(12):2046-2052. [DOI] [PubMed] [Google Scholar]
- 24. Vitale MA, White NJ, Strauch RJ. A percutaneous technique to treat unstable dorsal fracture-dislocations of the proximal interphalangeal joint. J Hand Surg Am. 2011;36(9):1453-1459. [DOI] [PubMed] [Google Scholar]
- 25. Afendras G, Abramo A, Mrkonjic A, et al. Hemi-hamate osteochondral transplantation in proximal interphalangeal dorsal fracture dislocations: a minimum 4 year follow-up in eight patients. J Hand Surg Eur Vol. 2010;35(8):627-631. [DOI] [PubMed] [Google Scholar]
- 26. Korting O, Facca S, Diaconu M, et al. Treatment of complex proximal interphalangeal joint fractures using a new dynamic external fixator: 15 cases. Chir Main. 2009;28(3):153-157. [DOI] [PubMed] [Google Scholar]
- 27. Ikeda M, Ishii T, Kobayashi Y, et al. Percutaneous pinning of the displaced volar plate avulsion fracture of the PIP joint. Hand Surg. 2009;14(2-3):113-119. [DOI] [PubMed] [Google Scholar]
- 28. Ruland RT, Hogan CJ, Cannon DL, et al. Use of dynamic distraction external fixation for unstable fracture-dislocations of the proximal interphalangeal joint. J Hand Surg Am. 2008;33(1):19-25. [DOI] [PubMed] [Google Scholar]
- 29. Ellis SJ, Cheng R, Prokopis P, et al. Treatment of proximal interphalangeal dorsal fracture-dislocation injuries with dynamic external fixation: a pins and rubber band system. J Hand Surg Am. 2007;32(8):1242-1250. [DOI] [PubMed] [Google Scholar]
- 30. Theivendran K, Pollock J, Rajaratnam V. Proximal interphalangeal joint fractures of the hand: treatment with an external dynamic traction device. Ann Plast Surg. 2007;58(6):625-629. [DOI] [PubMed] [Google Scholar]
- 31. Hamilton SC, Stern PJ, Fassler PR, et al. Mini-screw fixation for the treatment of proximal interphalangeal joint dorsal fracture–dislocations. J Hand Surg Am. 2006;31(8):1349-1354. [DOI] [PubMed] [Google Scholar]
- 32. Lee JY, Teoh LC. Dorsal fracture dislocations of the proximal interphalangeal joint treated by open reduction and interfragmentary screw fixation: indications, approaches and results. J Hand Surg Br. 2006;31(2):138-146. [DOI] [PubMed] [Google Scholar]
- 33. Grant I, Berger AC, Tham SK. Internal fixation of unstable fracture dislocations of the proximal interphalangeal joint. J Hand Surg Br. 2005;30(5):492-498. [DOI] [PubMed] [Google Scholar]
- 34. Aladin A, Davis TR. Dorsal fracture–dislocation of the proximal interphalangeal joint: a comparative study of percutaneous kirschner wire fixation versus open reduction and internal fixation. J Hand Surg Br. 2005;30(2):120-128. [DOI] [PubMed] [Google Scholar]
- 35. Badia A, Riano F, Ravikoff J, et al. Dynamic intradigital external fixation for proximal interphalangeal joint fracture dislocations. J Hand Surg Am. 2005;30(1):154-160. [DOI] [PubMed] [Google Scholar]
- 36. Khan W, Agarwal M, Muir L. Management of intra-articular fractures of the proximal interphalangeal joint by internal fixation and bone grafting. Arch Orthop Trauma Surg. 2004;124(10):688-691. [DOI] [PubMed] [Google Scholar]
- 37. Deshmukh SC, Kumar D, Mathur K, et al. Complex fracture-dislocation of the proximal interphalangeal joint of the hand. J Bone Joint Surg Br. 2004;86(3):406-412. [DOI] [PubMed] [Google Scholar]
- 38. Williams RM, Kiefhaber TR, Sommerkamp T, et al. Treat-ment of unstable dorsal proximal interphalangeal fracture/dislocations using a hemi-hamate autograft. J Hand Surg Am. 2003;28(5):856-865. [DOI] [PubMed] [Google Scholar]
- 39. Duteille F, Pasquier P, Lim A, et al. Treatment of complex interphalangeal joint fractures with dynamic external traction: a series of 20 cases. Plast Reconstr Surg. 2003;111(5):1623-1629. [DOI] [PubMed] [Google Scholar]
- 40. Syed AA, Agarwal M, Boome R. Dynamic external fixator for pilon fractures of the proximal interphalangeal joints: a simple fixator for a complex fracture. J Hand Surg Br. 2003;28(2):137-141. [DOI] [PubMed] [Google Scholar]
- 41. De Smet L, Boone P. Treatment of fracture–dislocation of the proximal interphalangeal joint using the suzuki external fixator. J Orthop Trauma. 2002;16(9):668-671. [DOI] [PubMed] [Google Scholar]
- 42. Newington DP, Davis TR, Barton NJ. The treatment of dorsal fracture-dislocation of the proximal interphalangeal joint by closed reduction and Kirschner wire fixation: a 16-year follow up. J Hand Surg Br. 2001;26(6):537-540. [DOI] [PubMed] [Google Scholar]
- 43. Weiss A. Cerclage fixation for fracture dislocation of the proximal interphalangeal joint. Clin Orthop Relat Res. 1996;327:21-28. [DOI] [PubMed] [Google Scholar]
- 44. Morgan JP, Gordon DA, Klug MS, et al. Dynamic digital traction for unstable comminuted intra-articular fracture-dislocations of the proximal interphalangeal joint. J Hand Surg Am. 1995;20(4):565-573. [DOI] [PubMed] [Google Scholar]
- 45. Inanami H, Ninomiya S, Okutsu I, et al. Dynamic external finger fixator for fracture dislocation of the proximal interphalangeal joint. J Hand Surg Am. 1993;18(1):160-164. [DOI] [PubMed] [Google Scholar]
- 46. Eglseder WA, Jeter EC. Open reduction and internal fixation of proximal interphalangeal joint fracture-subluxations. Cont Ortho. 1991;24(1):45-50. [PubMed] [Google Scholar]
- 47. Inoue G, Tamura Y. Treatment of fracture-dislocation of the proximal interphalangeal joint using extension-block Kirschner wire. Ann Chir Main Memb Super. 1991;10(6):564-568. [DOI] [PubMed] [Google Scholar]
- 48. Stern PJ, Roman RJ, Kiefhaber TR, et al. Pilon fractures of the proximal interphalangeal joint. J Hand Surg Am. 1991;16(5):844-850. [DOI] [PubMed] [Google Scholar]
- 49. Kubitskiy A, Soliman BAB, Dowd MB, et al. External fixation of the hand: a simple approach to comminuted proximal interphalangeal joint fractures. Hand Surg. 2014;19(1):85-89. [DOI] [PubMed] [Google Scholar]
- 50. Keramidas E, Solomos M, Page RE, et al. The Suzuki frame for complex intra-articular fractures of the proximal interphalangeal joint of the fingers. Ann Plast Surg. 2007;58(5):484-488. [DOI] [PubMed] [Google Scholar]
- 51. Hynes MC, Giddins GE. Dynamic external fixation for pilon fractures of the interphalangeal joints. J Hand Surg Am. 2001;26(2):122-124. [DOI] [PubMed] [Google Scholar]
- 52. Larsen MS, Leicht P, Lassen E. Osteosynthesis of intra-articular fractures in the proximal interphalangeal joint with Kirschner wires. Scand J Plast Reconstr Surg Hand Surg. 2000;34(2):149-153. [DOI] [PubMed] [Google Scholar]