Abstract
Background: Upper extremity injuries represent one of the most common pediatric conditions presenting to emergency departments (EDs) in the United States. We aim to describe the epidemiology, trends, and costs of pediatric patients who present to US EDs with upper extremity injuries. Methods: Using the National Emergency Department Sample, we identified all ED encounters by patients aged <18 years associated with a primary diagnosis involving the upper extremity from 2008 to 2012. Patients were divided into 4 groups by age (≤5 years, 6-9 years, 10-13 years, and 14-17 years) and a trauma subgroup. Primary outcomes were prevalence, etiology, and associated charges. Results: In total, 11.7 million ED encounters were identified, and 89.8% had a primary diagnosis involving the upper extremity. Fracture was the most common injury type (28.2%). Dislocations were common in the youngest group (17.7%) but rare in the other 3 (range = 0.8%-1.6%). There were 73.2% of trauma-related visits, most commonly due to falls (29.9%); 96.9% of trauma patients were discharged home from the ED. There were bimodal peaks of incidence in the spring and fall and a nadir in the winter. Emergency department charges of $21.2 billion were generated during the 4 years studied. While volume of visits decreased during the study, associated charges rose by 1.21%. Conclusions: Pediatric upper extremity injuries place burden on the economy of the US health care system. Types of injuries and anticipated payers vary among age groups, and while total yearly visits have decreased over the study period, the average cost of visits has risen.
Keywords: emergency department, injuries, epidemiology, research and health outcomes, HCUP, NEDS, health care, hand, anatomy, trauma, diagnosis, pediatric
Introduction
Hand and upper extremity injuries represent one of the most common pediatric conditions presenting to emergency departments (EDs) in the United States. Second only to the head, the hand is the most commonly injured body part in children.1,2 Fractures of the upper extremity are among one of the most common injuries in children. 3 Current literature on the epidemiology of pediatric upper extremity injuries primarily considers fractures and other very specific injuries but do not provide a comprehensive analysis of pediatric hand conditions presenting to the ED.4-8 In particular, data on the magnitude and types of upper extremity–related pediatric ED visits, especially information inclusive of nonfracture and soft-tissue conditions, are lacking.
The Nationwide Emergency Department Sample (NEDS), which includes data from 31 states, is currently the largest ED database in the United States, inclusive of all payer types. By combining data from 2 hospital-based ED databases, the State Inpatient Databases and the State Emergency Department Databases, the NEDS serves to provide national estimates of ED care. The key data elements provided by the NEDS include International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis codes; Current Procedural Terminology codes; information on mechanism, intent, and severity of injury; admission status; and patient demographic information. With demand for pediatric hand and orthopedic care in the ED setting, it is important for providers and hospitals to understand the volume, nature, and trends in pediatric hand and upper extremity injuries presenting to the ED.9-11 Using data available through NEDS, we describe the frequency and types of pediatric upper extremity conditions presenting to US EDs, elucidate patterns in visit volume and diagnosis, and describe trends in health care utilization as a result of these visits over a 4-year period.
Materials and Methods
We conducted a cross-sectional study of pediatric upper extremity–related ED visits in the United States between 2008 and 2012 using the NEDS, which is made available through the Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project (HCUP). 12 Years 2008-2012 were selected because they represent a time period prior to the implementation of the Affordable Care Act, which could potentially confound the data, particularly regarding payer mix.
ED Visit Selection
We identified all ED encounters by patients aged younger than 18 years that were associated with an upper extremity diagnosis between January 1, 2008, and December 31, 2012. We defined hand and upper extremity conditions as any injury distal to the shoulder using ICD-9-CM codes. As numerous ICD-9-CM codes can exist for each condition, diagnostic codes were grouped into the following categories: amputation, open wounds, arthropathy, burns, frostbite, contusions, neuropathy, fractures, dislocations, sprains, arterial injuries, superficial wounds (ie, abrasions or blisters), crush injuries, peripheral nerve injuries, tendon injuries, infections, and joint pain (see Supplemental Appendix).
Health Care Utilization
Measures of health care utilization included total number of visits per diagnosis category, average ED charges per visit with a hand or upper extremity condition as the primary diagnosis, and percentage of patients requiring inpatient admission. Patients directly discharged from the ED generated ED charges only; however, patients admitted to the same hospital after the initial ED visit generated charges for both the ED and inpatient care, adding to the estimation of incurred ED charges. All cost data obtained through HCUP were inflation-adjusted to 2018 US dollars.
Demographic, Injury-Related, and Disposition Data
Patient age, sex, anticipated primary payer (Medicare, Medicaid, Private, or Other), initial presentation, trauma score, and pediatric comorbidity were described in our study. Data on initial presentation included whether the primary diagnosis involved the upper extremity and whether the primary diagnosis was trauma-related. Within the trauma subgroup, mechanism of injury, intent of injury, and disposition were noted. The HCUP database further categorized mechanism and intent of injury into several broad categories. Mechanism of injury within the trauma subgroup was categorized into the following 12 groups of diagnoses related to the visit for upper extremity injury: cutting or piercing, drowning, falling, fire, firearm, machinery, motor vehicle, natural or environmental, poison, struck by or against something, suffocation, and multiple. Intent of injury was categorized into 3 groups: unintentional, assault, and self-harm. Disposition data included home discharge, admission, transfer, or death in the ED. 12 Trauma subgroup data were limited to the 2009-2012 period due to availability of trauma-specific variables.
Analysis
Patients were divided into 4 groups by age (≤5 years, 6-9 years, 10-13 years, and 14-17 years) and a trauma subgroup. Age groups were divided by transition points in schooling (ie, preschool to elementary school) and therefore transitions in environment and risk factors for injury. All analyses were weighted to account for complex sampling design and to provide national estimates.
Results
Demographics and Volume of Pediatric Hand-Related Visits
Between 2008 and 2012, 11.7 million ED encounters in the United States were associated with a common upper extremity condition (M = 2.3 million/year), with 89.8% having a hand or upper extremity diagnosis as the primary diagnosis (Table 1). Children aged 6 to 9 and 10 to 13 years were the most likely to have a hand or upper extremity malady as their primary diagnosis (92.1%), whereas those aged 14 to 17 years were the least likely (85.1%). Most patients were males (58.9%), and most encounters were trauma-related (73.2%). The oldest age group (14-17 years) accounted for the largest number of ED visits (3.6 million, 31%), whereas patients aged 6 to 9 years had the lowest number of ED visits (2.1 million, 18%). Apart from the youngest age group (≤5 years), the number of hand-related and upper extremity–related ED visits decreased by 1% in every age group over 4 years. Conversely, the youngest age group saw 1% growth over the same period. Overall, there was a small net 1% decrease in the number of pediatric upper extremity–related ED visits annually over the years from 1.2 million in 2008 to 1.1 million in 2012.
Table 1.
Discharges Associated With Common Pediatric Hand and Upper Extremity Maladies Seen in US Emergency Departments, 2008-2012.
| Overall |
≤5 y |
6-9 y |
10-13 y |
14-17 y |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Demographic Characteristics | No. | % | No. | % | No. | % | No. | % | No. | % |
| Discharges | 11 731 073 | 100.0 | 2 751 137 | 100.0 | 2 153 060 | 100.0 | 3 238 947 | 100.0 | 3 587 929 | 100.0 |
| Hand malady as primary diagnosis | 10 530 237 | 89.8 | 2 534 678 | 92.1 | 1 982 482 | 92.1 | 2 959 976 | 91.4 | 3 053 101 | 85.1 |
| Trauma-related | 8 589 333 | 73.2 | 2 023 645 | 73.6 | 1 594 455 | 74.1 | 2 412 958 | 74.5 | 2 558 274 | 71.3 |
| Male | 6 905 834 | 58.9 | 1 441 808 | 52.4 | 1 173 591 | 54.5 | 1 969 049 | 60.8 | 2 321 385 | 64.7 |
| Anticipated primary payer | ||||||||||
| Medicare | 42 281 | 0.4 | 9473 | 0.3 | 8093 | 0.4 | 11 806 | 0.4 | 12 910 | 0.4 |
| Medicaid | 4 818 231 | 41.1 | 1 338 541 | 48.7 | 892 778 | 41.5 | 1 252 081 | 38.7 | 1 334 831 | 37.2 |
| Private | 5 451 777 | 46.5 | 1 090 171 | 39.6 | 1 009 486 | 46.9 | 1 611 625 | 49.8 | 1 740 495 | 48.5 |
| Other | 1 418 785 | 12.1 | 312 953 | 11.4 | 242 703 | 11.3 | 363 435 | 11.2 | 499 694 | 13.9 |
| Pediatric comorbidity | ||||||||||
| No conditions | 11 354 046 | 96.8 | 2 699 393 | 98.1 | 2 085 743 | 96.9 | 3 139 843 | 96.9 | 3 429 067 | 95.6 |
| 1 condition | 308 021 | 2.6 | 41 814 | 1.5 | 54 511 | 2.5 | 82 426 | 2.5 | 129 271 | 3.6 |
| 2+ conditions | 69 007 | 0.6 | 9930 | 0.4 | 12 806 | 0.6 | 16 678 | 0.5 | 29 592 | 0.8 |
| Elixhauser medical comorbidity | ||||||||||
| No conditions | 11 141 373 | 95.0 | 2 676 101 | 97.3 | 2 063 299 | 95.8 | 3 077 070 | 95.0 | 3 324 904 | 92.7 |
| 1 condition | 540 859 | 4.6 | 72 208 | 2.6 | 86 604 | 4.0 | 153 161 | 4.7 | 228 887.0 | 6.4 |
| 2+ conditions | 48 841 | 0.4 | 2829 | 0.1 | 3158 | 0.1 | 8716 | 0.3 | 34 139.0 | 1.0 |
The Nature of Pediatric Hand Conditions Presenting to US EDs
Fractures accounted for the highest percentage of all pediatric hand and upper extremity maladies (28.2%), followed by contusions (18.8%), open wounds (17%), and sprains (15.4%) (Table 2). Except for the oldest age group (14-17 years), who suffered most frequently from contusions (22.5%), fractures were the most common upper extremity condition in all other age groups and second most common in the oldest age group (21.1%). Compared with all other age groups, children aged 10 to 13 years were more likely to suffer from sprains (21.4% vs 5.2%-19.3%) and the youngest age group (<5 years) from dislocations (17.7% vs 0.8%-1.6%), burns (7.1% vs 1.1%-1.8%), and crush injuries (2.1% vs 0.6%-1.3%). Alternatively, the youngest age group was less than half as likely to be diagnosed with sprains (5.2%) compared with the older age groups (range = 12.7%-21.4%). Upper extremity amputations were rare in our study, comprising only 0.3% of hand-related injuries over the 4-year period.
Table 2.
Nature of Pediatric Hand and Upper Extremity Maladies Stratified by Age Group.
| Overall |
≤5 y |
6-9 y |
10-13 y |
14-17 y |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Injury Type | No. | % | No. | % | No. | % | No. | % | No. | % |
| Discharges | 11 731 073 | 100.0 | 2 751 137 | 100.0 | 2 153 060 | 100.0 | 3 238 947 | 100.0 | 3 587 929 | 100.0 |
| Open wounds | 1 994 528 | 17.0 | 477 095 | 17.3 | 350 462 | 16.3 | 452 972 | 14.0 | 713 999 | 19.9 |
| Fractures | 3 310 656 | 28.2 | 667 540 | 24.3 | 826 507 | 38.4 | 1 060 299 | 32.7 | 756 310 | 21.1 |
| Contusion | 2 204 678 | 18.8 | 346 699 | 12.6 | 380 049 | 17.7 | 671 804 | 20.7 | 806 126 | 22.5 |
| Sprains | 1 801 666 | 15.4 | 142 020 | 5.2 | 272 373 | 12.7 | 694 277 | 21.4 | 692 995 | 19.3 |
| Joint pain | 691 575 | 5.9 | 113 443 | 4.1 | 109 913 | 5.1 | 207 477 | 6.4 | 260 743 | 7.3 |
| Infections | 630 639 | 5.4 | 188 017 | 6.8 | 115 401 | 5.4 | 118 841 | 3.7 | 208 380 | 5.8 |
| Superficial wounds (ie, abrasions, blisters, etc) | 944 584 | 8.1 | 247 308 | 9.0 | 174 622 | 8.1 | 210 647 | 6.5 | 312 007 | 8.7 |
| Burns | 327 929 | 2.8 | 196 221 | 7.1 | 38 972 | 1.8 | 35 453 | 1.1 | 57 284 | 1.6 |
| Arthropathy | 69 718 | 0.6 | 17 879 | 0.6 | 15 729 | 0.7 | 18 581 | 0.6 | 17 529 | 0.5 |
| Dislocations | 589 183 | 5.0 | 486 657 | 17.7 | 19 252 | 0.9 | 27 210 | 0.8 | 56 064 | 1.6 |
| Neuropathy | 8806 | 0.1 | 418 | 0.0 | 807 | 0.0 | 1641 | 0.1 | 5940 | 0.2 |
| Tendon injuries | 41 318 | 0.4 | 4440 | 0.2 | 4784 | 0.2 | 9510 | 0.3 | 22 584 | 0.6 |
| Crush injuries | 129 466 | 1.1 | 56 427 | 2.1 | 27 639 | 1.3 | 22 322 | 0.7 | 23 078 | 0.6 |
| Amputation | 40 053 | 0.3 | 20 793 | 0.8 | 6735 | 0.3 | 5619 | 0.2 | 6906 | 0.2 |
| Peripheral nerve injuries | 10 880 | 0.1 | 1143 | 0.0 | 1454 | 0.1 | 2373 | 0.1 | 5910 | 0.2 |
| Arterial injuries | 5129 | 0.0 | 748 | 0.0 | 638 | 0.0 | 823 | 0.0 | 2919 | 0.1 |
| Frostbite | 1054 | 0.0 | 216 | 0.0 | 129 | 0.0 | 241 | 0.0 | 468 | 0.0 |
Trauma-Related Injuries in Children Presenting to US EDs
Trauma-related visits were the majority, making up 73.2% of total ED visits over a 4-year period. Most patients had a single mechanism of injury, with only 0.7% having multiple mechanisms of injury. Children in the 10- to 13-year age group were the most likely to suffer from trauma to the upper extremity, albeit by a narrow margin (74.5%) (Table 1). Mechanisms of injury related to pediatric upper extremity maladies are classified in Table 3, which shows that falls (29.9%) were the most common injury overall, followed by strikes (17.9%) and cuts (10.4%). Except the oldest age group, falls were the most common mechanism of injury (30.5%-41.9%). Strikes, defined by the HCUP database as blunt force injury by or against a person or object, were the most common injury in the oldest age group (26.7%), followed by falls (19.2%) and cuts (14%). This age group also displayed the sharpest increase in the percentage of motor vehicle–related injuries, 7.1%, up from 2.7% in patients aged 10 to 13 years. Other than falls, children in the 10- to 13-year age group were most likely to suffer from strikes (22.7%), which accounted for a disproportionately higher percentage of trauma-related injuries compared with the younger age groups (range: 5.5%-12.1%). The next youngest age group (6-9 years) experienced the highest percentage of falls (41.9% vs 19.2%-30.5%). Compared with all older age groups, the youngest age group (≤5 years) suffered more commonly from fire (6.7% vs 1.0%-1.6%) and nature (7.0% vs 2.8%-5.4%), which is defined by the HCUP database as injury involving environmental causes, including bites and stings. 12 Most trauma-related hand conditions (96.9%) were discharged from the ED without admission for inpatient care; only 3.0% of patients were admitted to the hospital or transferred to another facility. Rates of discharge, admission, transfer, and death were similar for all age groups.
Table 3.
Summary of Diagnosis Codes Related to Trauma-Related Emergency Department Visits for Pediatric Hand and Upper Extremity Injuries During the Time Period 2009-2012 Due to Availability of Trauma-Specific Variables.
| Overall |
≤5 y |
6-9 y |
10-13 y |
14-17 y |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Injury Characteristics and Disposition | No. | % | No. | % | No. | % | No. | % | No. | % |
| Discharges | 8 589 333 | 100.0 | 2 023 645 | 100.0 | 1 594 455 | 100.0 | 2 412 958 | 100.0 | 2 558 274 | 100.0 |
| Mechanism of injury | ||||||||||
| Cut | 896 536 | 10.4 | 179 330 | 8.9 | 142 633 | 8.9 | 216 048 | 9.0 | 358 524 | 14.0 |
| Drown | 765 | 0.01 | 90 | 0.0 | 117 | 0.0 | 243 | 0.0 | 315 | 0.0 |
| Fall | 2 571 140 | 29.9 | 617 199 | 30.5 | 668 742 | 41.9 | 793 633 | 32.9 | 491 565 | 19.2 |
| Fire | 221 324 | 2.6 | 136 422 | 6.7 | 26 021 | 1.6 | 23 455 | 1.0 | 35 426 | 1.4 |
| Firearm | 7515 | 0.1 | 288 | 0.0 | 248 | 0.0 | 805 | 0.0 | 6173 | 0.2 |
| Machinery | 15 352 | 0.2 | 4110 | 0.2 | 1629 | 0.1 | 2448 | 0.1 | 7164 | 0.3 |
| Motor vehicle | 323 642 | 3.8 | 34 339 | 1.7 | 42 687 | 2.7 | 65 161 | 2.7 | 181 456 | 7.1 |
| Nature | 376 127 | 4.4 | 141 099 | 7.0 | 85 588 | 5.4 | 77 555 | 3.2 | 71 885 | 2.8 |
| Poison | 5051 | 0.1 | 943 | 0.0 | 543 | 0.0 | 920 | 0.0 | 2645 | 0.1 |
| Struck | 1 533 749 | 17.9 | 111 332 | 5.5 | 192 785 | 12.1 | 547 543 | 22.7 | 682 089 | 26.7 |
| Suffocation | 433 | 0.01 | 76 | 0.0 | 18 | 0.0 | 84 | 0.0 | 254 | 0.0 |
| Multiple | 59 245 | 0.7 | 13 852 | 0.7 | 11 197 | 0.7 | 13 642 | 0.6 | 20 554 | 0.8 |
| Intent of injury | ||||||||||
| Assault | 74 053 | 0.9 | 2 266 | 0.1 | 2 941 | 0.2 | 14 711 | 0.6 | 54 135 | 2.1 |
| Self-harm | 46 259 | 0.5 | 72 | 0.0 | 290 | 0.0 | 8095 | 0.3 | 37 802 | 1.5 |
| Unintentional | 7 871 783 | 91.6 | 1 905 013 | 94.1 | 1 505 388 | 94.4 | 2 235 910 | 92.7 | 2 225 471 | 87.0 |
| Multiple | 121 557 | 1.4 | 2771 | 0.1 | 3825 | 0.2 | 22 747 | 0.9 | 92 215 | 3.6 |
| Disposition | ||||||||||
| Home discharge | 8 319 175 | 96.9 | 1 945 614 | 96.1 | 1 537 429 | 96.4 | 2 359 888 | 97.8 | 2 476 244 | 96.8 |
| Admitted to same hospital | 141 897 | 1.7 | 38 357 | 1.9 | 27 284 | 1.7 | 26 187 | 1.1 | 50 069 | 2.0 |
| Transfer to another hospital | 112 838 | 1.3 | 36 084 | 1.8 | 26 943 | 1.7 | 23 182 | 1.0 | 26 629 | 1.0 |
| Died in the emergency department | 619 | 0.01 | 138 | 0.01 | 82 | 0.01 | 87 | 0.00 | 312 | 0.01 |
Note. The injury severity score is assigned using a publicly available Stata program for Injury Classification (International Classification of Diseases Program for Injury Categorization) which uses International Classification of Diseases, Ninth Revision, Clinical Modification diagnosis codes to assign a severity score (ranging from 1 to 75, with 75 being the most severe).
Trends in Pediatric Hand Maladies Within and Over Multiple Years
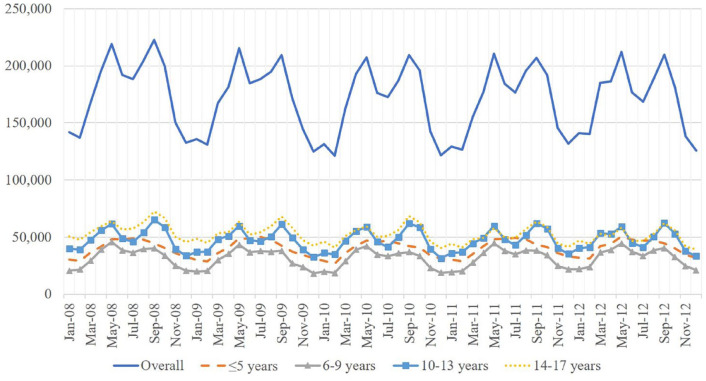
The volume of hand injuries in children presenting to US EDs showed a clear seasonal, cyclic pattern over the 4-year period of our study. When adjusted for the number of days in a month, the trend in yearly ED visits showed bimodal peaks in the summer and fall months (June and October, respectively) and a nadir in the winter (January) (Figure 1). This cyclic pattern was similar for all groups with the exception of the youngest (≤5 years) group.
Figure 1.
Time trend in emergency department discharges in the United States for common pediatric hand and upper extremity conditions, 2008-2012.
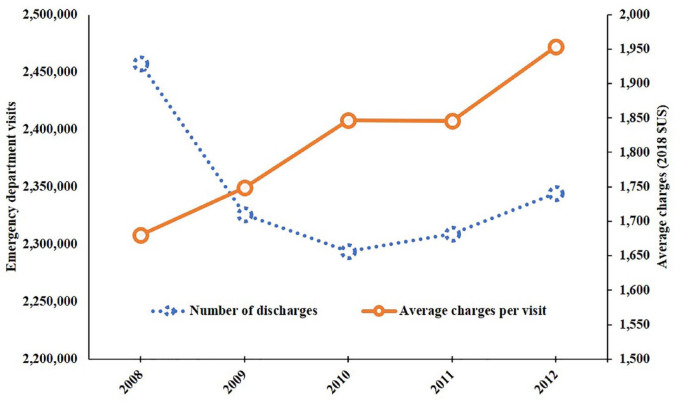
Health Care Costs of Pediatric Hand Maladies
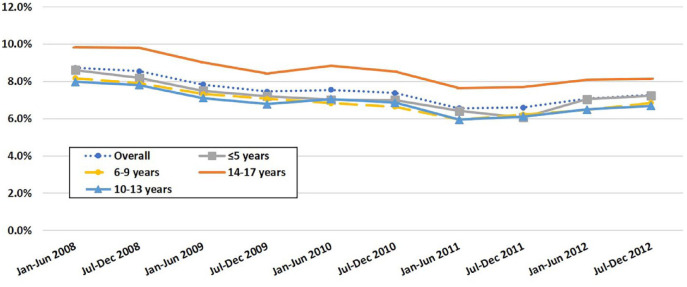
Overall ED charges were $21.2 billion during the study. Yearly visit volume decreased from 2.4 million in 2008 to 2.3 million in 2012 (net 1% decrease), but annual cost increased from $4.1 billion in 2008 to $4.5 billion in 2012, with the average ED charges per visit rising from $1654 in 2008 to $2000 over the same period (net 1.21% increase) (Table 4, Figure 2). Private insurance providers were the anticipated payer in 46.5% of visits overall; however, Medicaid paid for 48.7% of visits for patients aged <5 years (Table 1). The average number of uninsured discharges was 7.5%. The highest proportion of uninsured patients consisted of those aged 14 to 17 years (8.6%) (Figure 3).
Table 4.
Trend in the Number of Hand and Upper Extremity–Related ED Discharges and Associated Health Care Costs.
| Time Period | No. of discharges | Average ED charges per discharge with hand condition as primary diagnosis (2018 US dollars) |
|---|---|---|
| January-June 2008 | 1 204 768 | 1654 |
| July-December 2008 | 1 252 377 | 1705 |
| January-June 2009 | 1 152 631 | 1727 |
| July-December 2009 | 1 173 279 | 1771 |
| January-June 2010 | 1 123 951 | 1814 |
| July-December 2010 | 1 169 820 | 1879 |
| January-June 2011 | 1 116 328 | 1806 |
| July-December 2011 | 1 192 717 | 1885 |
| January-June 2012 | 1 187 460 | 1906 |
| July-December 2012 | 1 156 792 | 2000 |
| % Change | 0.96 | 1.21 |
Note. ED = emergency department.
Figure 2.
Trend in the number of US emergency department visits and associated health care costs (US dollars) for hand and upper extremity injuries among pediatric patients, 2008-2012.
Figure 3.
Percentage of uninsured patients between 2008 and 2012.
Discussion
We aimed to present a comprehensive overview of the volume and breakdown of pediatric hand-related and upper extremity–related conditions presenting to US EDs over a 4-year period and their associated health care costs. Overall, patients were mostly males and most commonly presented with trauma-related injuries, consistent with prior epidemiological studies.3,6,7,13,14 Whereas previous literature reported laceration as the most common pediatric hand injury, our study showed that fractures were the most common injury presenting to US EDs in nearly all age groups.13,15 Inclusion of more proximal upper extremity injuries likely accounts for the difference in our findings, as previous studies did not include conditions of the upper arm, forearm, and wrist, fractures of which are the most common upper extremity injuries in children overall.3,13,16 Furthermore, trauma accounts for most hand-related and upper extremity–related ED visits, the vast majority of which are amenable to treatment and discharge from the ED. 15 Nevertheless, the number of patients treated successfully in the ED is likely underestimated. One previous study found that a greater number of transfers occurred from institutions that could not admit children, regardless of hand coverage, and a large proportion of those transferred were discharged without a hospital admission. 17 Further research should be done to ensure appropriate emergency care to pediatric patients and whether transfers are initiated because of discomfort of caring for pediatric patients by the ED provider or poor accessibility to hand and upper extremity specialists who can care for children.
We show several age-related differences in the nature of presenting injury. First, the percentage of fractures saw a decrease in the oldest age group, supporting current trends reported in the literature.16,18,19 Decrease in skeletal growth rate in adolescence may have a positive effect on bone mineral density and therefore fracture susceptibility. 20 In addition, the same group also saw a spike in the percentage of motor vehicle–related injuries, which likely corresponds to the legal driving age in the United States (16 years of age). The youngest age group suffered dislocations more frequently than others, which may be partially explained by higher incidence of nursemaid’s elbow and age-related differences in soft-tissue laxity.21-23 In the youngest group, burns only accounted for 7.1% of injuries but represented 60% of all upper extremity burns sustained by children. Similarly, crush injuries in those aged ≤5 years account for 44% of crush injuries in all age groups. These findings, seen also in other papers,15,24,25 are likely due to the natural behavior of toddlers, who are more prone to manual exploration without awareness of the associated dangers. 6 Within the same age group (≤5 years), home-related falls may account for most falls in young children, as they tend to fall during exploration and as a result of immature motor development. Falls from playground equipment or bicycles and sports may account for the same in preadolescents. 26 Further investigation may elucidate age-related behavioral differences and guide age-specific safety interventions.
There was a clear seasonal pattern of ED visit volume observed in our study. With the exception of the youngest age group (≤5 years), our analysis shows a clear increase in ED visit volume in the summer and fall months with a nadir in the winter. The seasonality of injuries has been well reported in the literature.2,27,28 Increased outdoor activity in the summer and return to school and sports participation in the fall may account for increased ED visit volume. Similarly, decreased daylight hours and less outdoor activity in the winter months may correspond to less observed ED visits.28,29 This bimodal ED visitation pattern is not observed in children aged ≤5 years, perhaps due to variation in developmental stage–specific risk factors. For example, the epidemiological study of pediatric wrist fractures by Shah et al 30 showed beds/bed frames, stairs, and playgrounds were consumer products most commonly associated with wrist fractures in children aged 0 to 12 months, 13 to 36 months, and 3 to 5 years, respectively. This study highlights likely variability in risk factors within the youngest age group, warranting further risk factor analysis after substratification by year or perhaps developmental milestone/stage. Nevertheless, seasonal fluctuations in visit volume may help guide hand and orthopedic call staffing during the busier months, particularly in resource-limited hospitals or regions.
Annual ED visit volume decreased over the period of our study, which supports the findings of the large-scale epidemiologic study of pediatric hand conditions by Shah et al. 13 This may be partially attributed to continued efforts to improve the safety of consumer products and/or activities associated with hand injuries. Alternatively, Shah et al 13 found that a slightly younger population (aged 10-14 years) accounted for most ED visits (vs 14-17 years in our study). Analysis of different time periods, durations, and databases could account for the discrepancy. In addition, we included all injuries distal to the shoulder in our analysis, whereas the aforementioned study only included hand conditions distal to the wrist. Importantly, associated health care costs grossly increased despite decreased ED visit volume. This increase in cost is likely multifactorial; however, data from this study represent a time period of unpredictable health care policy changes. Therefore, our cost data should be considered as a reference point as health care policy continues to change. Unlike the adult population, there are no previous studies of the health care costs associated with pediatric hand and upper extremity maladies in the United States. Further economic analysis taking into account continually changing US health care policy is required to determine the exact factors contributing to the rise of emergency hand and upper extremity care.
Our study should be considered in the context of several limitations. The use of a national database of ED visits does not include patients seen in clinic, urgent care, or other health care settings, which underestimates the true burden of pediatric hand and upper extremity maladies. In addition, this database lacked information on the exact location of injury, which could have served as a point of comparison with previous studies that included location of injury in their analyses. The use of ICD-9-CM codes to identify patients is inherently subject to errors in coding and may not have comprehensively captured all pediatric upper extremity maladies. Therefore, our study likely underestimates the true burden of these pediatric conditions. Finally, the analyzed data only allow us to observe trends and identify correlative data; however, they do not allow us to conclude the underlying reasons between said trends and associations.
In adult patients, emergency medicine (EM) physicians and hand surgeons largely agree on which hand diagnoses are amenable to management by EM physicians. 31 Although these data are unavailable for pediatric patients, a lack of on-call hand specialists contributes to inappropriate interhospital transfers in both populations. 17 Because our data did not differentiate care provided by EM physicians, pediatric orthopedists, and hand surgeons, further investigation is warranted to determine the volume and scope of pediatric upper extremity care provided by different disciplines. Nevertheless, there is a definite role of EM physicians in caring for pediatric upper extremity injuries, justifying future efforts to determine and address contributors to underutilization and finding ways to expand the volume of hand and upper extremity care provided by EM physicians.
Conclusion
Between 2008 and 2012, EDs in the United States saw 11.7 million pediatric hand and upper extremity complaints. Emergency department visit volume peaks in the summer and fall with a nadir in the winter. Most visits were trauma-related, with falls and fractures being the most common mechanism and diagnosis overall, respectively. However, patients aged 14 to 17 were more likely to suffer from contusions than fractures, and patients aged ≤5 years were more likely than the older age groups to suffer from dislocations, burns, and crush injuries. Burns and crush injuries in the youngest age group accounted for a significant percentage of burns and crush injuries overall. Most trauma-related hand conditions were treated and discharged directly from the ED, with only a small percentage being admitted to the hospital or transferred to another facility.
Supplemental Material
Supplemental material, Appendix for Pediatric Hand and Upper Extremity Injuries Presenting to Emergency Departments in the United States: Epidemiology and Health Care–Associated Costs by Alfred Lee, David L. Colen, Justin P. Fox, Benjamin Chang and Ines C. Lin in HAND
Footnotes
Supplemental material is available in the online version of the article.
Authors’ Note: The views expressed in this article are those of the authors and do not reflect the official policy of the United States Air Force, Department of Defense, or the US Government Justin P. Fox is also affiliated to Surgical Operations Squadron, 88th Medical Group, Wright Patterson AFB, Ohio.
Ethical Approval: This study is exempt from the University of Pennsylvania institutional review board.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: Informed consent was obtained when necessary.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Alfred Lee  https://orcid.org/0000-0003-2693-7144
https://orcid.org/0000-0003-2693-7144
References
- 1. Hastings H, 2nd, Simmons BP. Hand fractures in children: a statistical analysis. Clin Orthop Relat Res. 1984;(188):120-130. [PubMed] [Google Scholar]
- 2. Ljungberg E, Rosberg HE, Dahlin LB. Hand injuries in young children. J Hand Surg Br. 2003;28(4):376-380. [DOI] [PubMed] [Google Scholar]
- 3. Naranje SM, Erali RA, Warner WC, Jret al. Epidemiology of pediatric fractures presenting to emergency departments in the United States. J Pediatr Orthop. 2016;36(4):e45-e48. doi: 10.1097/BPO.0000000000000595. [DOI] [PubMed] [Google Scholar]
- 4. Voth M, Lustenberger T, Frank Jet al. [Pediatric finger and hand injuries: an epidemiological study]. Chirurg. 2017;88(10):871-878. doi: 10.1007/s00104-017-0499-8. [DOI] [PubMed] [Google Scholar]
- 5. Voth M, Lustenberger T, Auner Bet al. What injuries should we expect in the emergency room? Injury. 2017;48(10):2119-2124. doi: 10.1016/j.injury.2017.07.027. [DOI] [PubMed] [Google Scholar]
- 6. Yorlets RR, Busa K, Eberlin KRet al. Fingertip injuries in children: epidemiology, financial burden, and implications for prevention. Hand (N Y). 2017;12(4):342-347. doi: 10.1177/1558944716670139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Vakhshori V, Bouz GJ, Mayfield CKet al. Trends in pediatric traumatic upper extremity amputations [published online ahead of print May 1, 2018]. Hand (N Y). doi: 10.1177/1558944718777865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Buncke GM, Buntic RF, Romeo O. Pediatric mutilating hand injuries. Hand Clin. 2003;19(1):121-131. [DOI] [PubMed] [Google Scholar]
- 9. Burt CW, McCaig LF. Staffing, capacity, and ambulance diversion in emergency departments: United States, 2003-04. Adv Data. 2006(376):1-23. [PubMed] [Google Scholar]
- 10. Smith BG, Kanel JS, Halsey MFet al. Emergency department on-call status for pediatric orthopaedics: a survey of the POSNA membership. J Pediatr Orthop. 2015;35(2):199-202. doi: 10.1097/BPO.0000000000000201. [DOI] [PubMed] [Google Scholar]
- 11. Whipple LA, Kelly T, Aliu Oet al. The crisis of deficiency in emergency coverage for hand and facial trauma: exploring the discrepancy between availability of elective and emergency surgical coverage. Ann Plast Surg. 2017;79(4):354-358. doi: 10.1097/SAP.0000000000001155. [DOI] [PubMed] [Google Scholar]
- 12. Healthcare Cost and Utilization Project (HCUP). Nationwide Emergency Department Sample. Rockville, MD: Agency for Healthcare Research and Quality; 2008-2012. [PubMed] [Google Scholar]
- 13. Shah SS, Rochette LM, Smith GA. Epidemiology of pediatric hand injuries presenting to United States emergency departments, 1990 to 2009. J Trauma Acute Care Surg. 2012;72(6):1688-1694. doi: 10.1097/TA.0b013e31824a4c5b. [DOI] [PubMed] [Google Scholar]
- 14. Vadivelu R, Dias JJ, Burke FDet al. Hand injuries in children: a prospective study. J Pediatr Orthop. 2006;26(1):29-35. doi: 10.1097/01.bpo.0000189970.37037.59. [DOI] [PubMed] [Google Scholar]
- 15. Bhende MS, Dandrea LA, Davis HW. Hand injuries in children presenting to a pediatric emergency department. Ann Emerg Med. 1993;22(10):1519-1523. [DOI] [PubMed] [Google Scholar]
- 16. Clark EM. The epidemiology of fractures in otherwise healthy children. Curr Osteoporos Rep. 2014;12(3):272-278. doi: 10.1007/s11914-014-0227-y. [DOI] [PubMed] [Google Scholar]
- 17. Gornitzky AL, Milby AH, Gunderson MAet al. Referral patterns of emergent pediatric hand injury transfers to a tertiary care center. Orthopedics. 2016;39(2):e333-e339. doi: 10.3928/01477447-20160222-06. [DOI] [PubMed] [Google Scholar]
- 18. Kopjar B, Wickizer TM. Fractures among children: incidence and impact on daily activities. Inj Prev. 1998;4(3):194-197. doi: 10.1136/ip.4.3.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Stracciolini A, Casciano R, Levey Friedman Het al. Pediatric sports injuries: a comparison of males versus females. Am J Sports Med. 2014;42(4):965-972. doi: 10.1177/0363546514522393. [DOI] [PubMed] [Google Scholar]
- 20. Faulkner RA, Davison KS, Bailey DAet al. Size-corrected BMD decreases during peak linear growth: implications for fracture incidence during adolescence. J Bone Miner Res. 2006;21(12):1864-1870. doi: 10.1359/jbmr.060907. [DOI] [PubMed] [Google Scholar]
- 21. Cheng JC, Chan PS, Hui PW. Joint laxity in children. J Pediatr Orthop. 1991;11(6):752-756. [DOI] [PubMed] [Google Scholar]
- 22. Jansson A, Saartok T, Werner Set al. General joint laxity in 1845 Swedish school children of different ages: age- and gender-specific distributions. Acta Paediatr. 2004;93(9):1202-1206. [DOI] [PubMed] [Google Scholar]
- 23. Vitello S, Dvorkin R, Sattler Set al. Epidemiology of nursemaid’s elbow. West J Emerg Med. 2014;15(4):554-557. doi: 10.5811/westjem.2014.1.20813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Jeon BJ, Lee JI, Roh SYet al. Analysis of 344 hand injuries in a pediatric population. Arch Plast Surg. 2016;43(1):71-76. doi: 10.5999/aps.2016.43.1.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Liu EH, Alqahtani S, Alsaaran RNet al. A prospective study of pediatric hand fractures and review of the literature. Pediatr Emerg Care. 2014;30(5):299-304. doi: 10.1097/PEC.0000000000000118. [DOI] [PubMed] [Google Scholar]
- 26. Hedström EM, Svensson O, Bergström Uet al. Epidemiology of fractures in children and adolescents. Acta Orthop. 2010;81(1):148-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Pierce B. Does the year-end decline in injury risk reflect reporting error. Am J Ind Med. 2015;58(5):519-527. doi: 10.1002/ajim.22440. [DOI] [PubMed] [Google Scholar]
- 28. Jespersen E, Holst R, Franz Cet al. Seasonal variation in musculoskeletal extremity injuries in school children aged 6-12 followed prospectively over 2.5 years: a cohort study. BMJ Open. 2014;4(1):e004165. doi: 10.1136/bmjopen-2013-004165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Wareham K, Johansen A, Stone MDet al. Seasonal variation in the incidence of wrist and forearm fractures, and its consequences. Injury. 2003;34(3):219-222. [DOI] [PubMed] [Google Scholar]
- 30. Shah NS, Buzas D, Zinberg EM. Epidemiologic dynamics contributing to pediatric wrist fractures in the United States. Hand (N Y). 2015;10(2):266-271. doi: 10.1007/s11552-014-9710-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Drolet BC, Lifchez SD, Jacoby SMet al. Perceptions of emergency medicine residency and hand surgery fellowship program directors in the appropriate disposition of upper extremity emergencies. J Hand Surg Am. 2015;40(12):2435-2439. doi: 10.1016/j.jhsa.2015.09.014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Appendix for Pediatric Hand and Upper Extremity Injuries Presenting to Emergency Departments in the United States: Epidemiology and Health Care–Associated Costs by Alfred Lee, David L. Colen, Justin P. Fox, Benjamin Chang and Ines C. Lin in HAND