Abstract
Background:
Little scientific evidence is available regarding the effect of knee joint line obliquity (JLO) before and after coronal realignment osteotomy.
Hypotheses:
Higher JLO would lead to abnormal relative position of the femur on the tibia, a shift of the joint contact areas, and elevated joint contact pressures.
Study Design:
Descriptive laboratory study.
Methods:
10 fresh-frozen human cadaveric knees (age, 59 ± 5 years) were axially loaded to 1500 N in a materials testing machine with the joint line tilted 0°, 4°, 8°, and 12° varus (“downhill” medially) and valgus, at 0° and 20° of knee flexion. The mechanical compression axis was aligned to the center of the tibial plateau. Contact pressure and contact area were recorded by pressure sensors inserted between the tibia and femur below the menisci. Changes in relative femoral and tibial position in the coronal plane were obtained by an optical tracking system.
Results:
Both medial and lateral JLO caused significant tibiofemoral subluxation and pressure distribution changes. Medial (varus) JLO caused the femur to subluxate medially down the coronal slope of the tibial plateau, and vice versa for lateral (valgus) downslopes (P < .01), giving a 6-mm range of subluxation. The areas of peak pressure moved 12 mm and 8 mm across the medial and lateral condyles, onto the downhill meniscus and the “uphill” tibial spine. Changes in JLO had only small effects on maximum contact pressures.
Conclusion:
A 4° change of JLO during load bearing caused significant mediolateral tibiofemoral subluxation. The femur slid down the slope of the tibial plateau to abut the tibial eminence and also to rest on the downhill meniscus. This caused large movements of the tibiofemoral contact pressures across each compartment.
Clinical Relevance:
These results provide important information for understanding the consequences of creating coronal JLO and for clinical practice in terms of osteotomy planning regarding the effect on JLO. This information provides guidance regarding the choice of single- or double-level osteotomy. Excessive JLO alteration may cause abnormal tibiofemoral joint articulation and chondral or meniscal loading.
Keywords: knee osteotomy, biomechanics, cartilage contact pressure, joint line obliquity, coronal slope, meniscus loading, tibiofemoral subluxation
Bony alignment of the knee joint is an important factor in normal function, different pathologies, and load distribution.37,38 Osteotomies are performed to alter alignment to unload cartilage, 1 menisci, and ligaments, and these procedures lead to good clinical results when performed accurately and in appropriately selected patients.9,10,12,15,29,32,34 The magnitude of sagittal tibial slope has been shown to affect knee biomechanics during the stance phase of gait and cruciate ligament loads. 8 In contrast to the sagittal slope, however, data are lacking on joint line obliquity (JLO) in the coronal plane, especially in the setting of osteotomy, in relation to biomechanical parameters such as articular contact stresses.19,28
A straight leg, aligned so that the mechanical tibiofemoral axis passes through the middle of the knee, has a medial (varus) slope (ie, where the medial edge of the plateau is distal, or inferior, to the lateral edge of the plateau) of the proximal tibia of 3° on average. 18 This gives a medial proximal tibial angle, between the long axis of the tibia and the tibial joint line, of 87°. This is matched by the lateral distal femoral angle also being 87° and provides a horizontal knee joint line—so that the JLO is zero—when the leg is adducted during the stance phase of gait. 3 However, such ideal lower limb alignment is not present in all individuals. 20 Realignment osteotomies are most commonly used in the treatment of osteoarthritis, to shift the weightbearing axis from a diseased articular surface to healthy areas. Osteotomies are also a good option to correct bony deformities and normalize biomechanical properties, such as reduction of locally elevated contact forces, of the knee in patients with congenital or postfracture deformity1,39 or after ligament reconstruction, meniscal transplant, or chondral resurfacing surgery in adversely aligned lower limbs.
Historically, a JLO of up to 10° was accepted, 11 although limited clinical evidence was available to support this level of obliquity. However, Babis et al5,6 were concerned that large JLO would cause excessive medial-lateral (ML) shear forces across the knee, and so they developed a method of double-level (femoral and tibial) osteotomy planning that could realign the leg and also aim to keep the JLO <4°. Using this JLO among their alignment criteria, Babis et al 5 reported that a small group of their osteotomy patients (n = 10) had no severe pain at 10-year follow-up. In recent years, other groups have advocated double-level osteotomies to prevent excessive JLO.27,33 Even though such large operations achieve better anatomic outcome, they increase morbidity and complications. To date, only scant evidence is available regarding how coronal JLO affects joint pressure and movement when the knee is weightbearing,19,25,28 and no clearly accepted upper limit of acceptable JLO has been established.
The purpose of this study was to investigate the effect of JLO on joint contact pressures, changes in position of the center of force within the knee, and the relative femoral and tibial movement in the coronal plane during joint loading. It was hypothesized that higher JLO would lead to an increased femoral ML displacement on the tibia in the coronal plane with a significant increase of articular contact pressure and consequent shift of the joint contact areas.
Methods
After ethical approval was granted by Imperial College London Healthcare Tissue Bank, 10 unpaired fresh-frozen human cadaveric knees with an average donor age of 59 years (range, 51-65 years) were tested (5 left- and 5 right-sided; 6 female and 4 male). A power analysis using G*Power 3.1.9.7 software 13 based on published cartilage contact pressures 1 showed that a change of 1 MPa could be identified with 95% power and alpha = .05 with 9 specimens. The specimens were stored at −20°C and were thawed 24 hours at room temperature before testing. All knees were free of osteoarthritis and had intact ligaments and menisci. This was confirmed by gross inspection and manual examination during the dissection process. The femur and tibia were cut 15 cm above and below the joint line level. The skin and subcutaneous tissue were removed, leaving the muscles, tendons, ligaments, patella, and capsule intact. The proximal 7 cm of the fibula was fixed to the tibia in an anatomic position using a tricortical bone screw. Each knee was tested in 1 day and was kept moist during the entire testing with a water spray.
The proximal femur and the distal tibia were skeletonized and cemented into 6-cm diameter cylindrical steel pots using poly-methyl methacrylate bone cement. The knees were aligned with the vertical tibial shaft positioned in the bone pot so that the compression axis of the testing machine was on the mechanical axis, passing through the center of the plateau between the tibial spines. The femur was then potted with the knee in 0° of flexion (when the tibial and femoral shafts were parallel in the sagittal plane) and with the 2 bone pots coaxial; thus, the femoral shaft was angled approximately 6° from vertical in the coronal plane, the difference between the anatomic and mechanical axes of the femur. After potting, digital photos were taken of the knees in full extension with pins inserted at the joint line medially and laterally, and the actual JLO of the specimen was measured. The tibial plateau had a mean medial downslope (JLO) of 3.3°± 2.0° (range, 0°-5.5°), which is the normal range in undeformed bones. 18 The results were corrected to the mean value of medial downslope across all knees and reported accordingly.
A motion tracking camera system (Polaris, Vega; Northern Digital Inc) was used to measure femoral motion relative to the tibia. Reflective markers (BrainLab) were rigidly secured to the femur and tibia with bicortical rods, which were then tracked during the experiment by a stereo infrared camera. The measurement procedure had been developed and described previously,21,24 with a translational accuracy of ±0.1 mm. The medial and lateral epicondyles, the proximal end of the femur, the most medial and lateral points of the tibial plateau, and the distal end of the tibia were marked with fiducial screws. These anatomic landmarks were digitized with a stylus to define the femoral and tibial coordinate systems. We defined 0° of flexion as when the tibial and femoral pots were parallel when viewed in the sagittal plane, and the 6 degrees of freedom tibiofemoral motion was then measured. Although the usual convention is to describe the motion of the tibia in relation to the femur, here we describe femoral motion across the stationary tibia, as though in the stance phase of walking.
A pressure sensor foil (K-Scan 4011; Tekscan Inc) was used to measure contact pressures and areas. The pressure-sensitive elements were covered with a thin film of self-adhesive tape to protect them against wear and moisture damage during testing. Before testing, as per the manufacturer’s guidelines, each sensor area was equilibrated to 2000 N to normalize the readings by compression between steel platens with a 3-mm rubber sheet interlayer, in a dual-axis servohydraulic materials testing machine (Model 8874; Instron), and a power-law calibration was performed at loads of 500 N and 1500 N. To insert the 2 pressure sensor sections into the medial and lateral compartments, horizontal incisions 20 mm long were made below the menisci in the anterior and posterior capsule. Structures such as the collateral and cruciate ligaments, meniscotibial ligaments (apart from the anterior incisions), and meniscus root attachments were carefully preserved while the sensor was inserted from the anterior incisions. After sensor positioning between the menisci and the tibial plateau, the non-pressure-sensitive boundary area of the foil was sutured to the anterior and posterior capsule to prevent displacement shifts during testing.
The materials testing machine was used for axial compression testing. The potted femur was mounted on a purpose-built fixture connected to the moving test machine actuator (Figure 1). This allowed the knee to be fixed at 0° to 20° of knee flexion to cover the range of motion during the stance phase of walking. 26 The femoral mounting fixture allowed the orientation of the knee to be rotated in the coronal plane about an anterior-posterior (AP) axis crossing the center of the tibial plateau. The femoral mounting used predrilled location holes to ensure that orientation accuracy and precision were within 1°. This caused changes of the JLO while keeping the joint compression force on a vertical mechanical axis through the center of the knee. The JLO was changed by 0°, 4°, 8°, and 12° medial (varus) or lateral (valgus) down-sloping away from the native 3° medial downslope, giving a range of 9° lateral to 15° medial slope. The potted tibia was mounted on a purpose-built pivoting rig on an XY rolling table on the test machine base, which allowed the tibia to freely translate in AP and ML directions and to rotate about the AP abduction-adduction axis under the applied loads. The free rotation of the tibia about the AP axis allowed the load balance between the medial and lateral condyles to be maintained even when the joint line was tilted and also when the medial and lateral compartments had differing compressive stiffness (Figure 1). The rotary axis of the test machine was used to adjust the knee in internal-external rotation to a neutral position where the torque was zero at each angle of knee flexion, thus allowing for the screw-home mechanism, and then locked when the knee was loaded. The knees were axially loaded, always in a vertical direction through the center of the tibial plateau regardless of knee position, to a compression load of 20 N as a starting measurement for the pressure sensor and optical tracking. The knees were then loaded axially at 25 N/s to a compression force of 1500 N, chosen because it is the mean knee contact force during the stance phase of walking. 36 At this load, the pressure sensor and optical tracking data were recorded.
Figure 1.
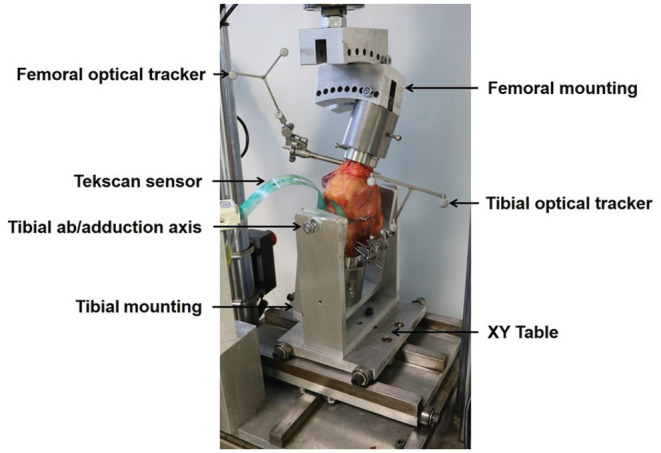
Experimental setup of a left knee at 9° lateral downslope and 20° of knee flexion. The femoral pot was secured to the fixture mounted on the materials testing machine actuator at the top of the picture. The tibial rig sits on the XY rolling table, which allowed free movement including free abduction and adduction about the AP pivot axis. Optical trackers were securely fixed to the femur and tibia to measure relative movements of the femur and tibia while axial force was applied. A foil pressure sensor was inserted underneath the medial and lateral menisci to obtain joint pressure readings.
The following contact pressure characteristics were calculated from the pressure sensors: mean and peak contact pressure (PCP) and center of pressure in each compartment, and the position of the resultant force across the knee joint. The PCP was the highest value in a sensel in the contact area, after we manually discarded erroneous readings, such as outside of the contact area. The contact pressure maps were also analyzed in respect to the peak pressure acting on each of the menisci and the tibial spine within each of the medial and lateral compartments, and these were plotted versus JLO. A preliminary guideline to this process was that if each tibial condyle was assumed to be semicircular, then the tibial spine was assumed to lie at the center of the semicircle and extend out to 50% of the outer radius. The remaining outer area was assumed to be the meniscal contact, and this was often shown clearly by the pressure sensor data with a semicircular contact track around the periphery of the tibial condyle. This guideline was moderated subjectively by reference to a photograph of the plateau with menisci in situ, to allow for the anatomic deviation from this simplified geometry in the frames when the contact area transitioned from the meniscus to the tibial spine.
Statistical Analysis
Data were analyzed using GraphPad Prism (Version 9 for Windows; GraphPad Software). The data for peak contact pressures and for ML translations passed the Shapiro-Wilk normality test, with alpha = .05 in all testing. Repeated-measures 1-way analyses of variance were used to examine the effect of variation of the JLO on the dependent variables: contact pressures and tibiofemoral movements. If significant effects were found, then paired t tests were used to compare values at 3° medial coronal slope (when the tibia was vertical) versus the values with different medial or lateral downslopes across ±12°, at 0° and 20° of knee flexion, with P < .0083 after Bonferroni correction.
Results
Tibiofemoral Medial-Lateral Translation
In full extension and with 3° medial JLO (vertical tibia), the femur moved medially with respect to the tibia when axial load was applied (Figure 2). The medial femoral translation increased 247% when the medial JLO was increased to 15° medial JLO (P < .001). In contrast, the femur did not translate significantly in the lateral direction with up to 9° lateral JLO in the extended knee (Figure 2).
Figure 2.
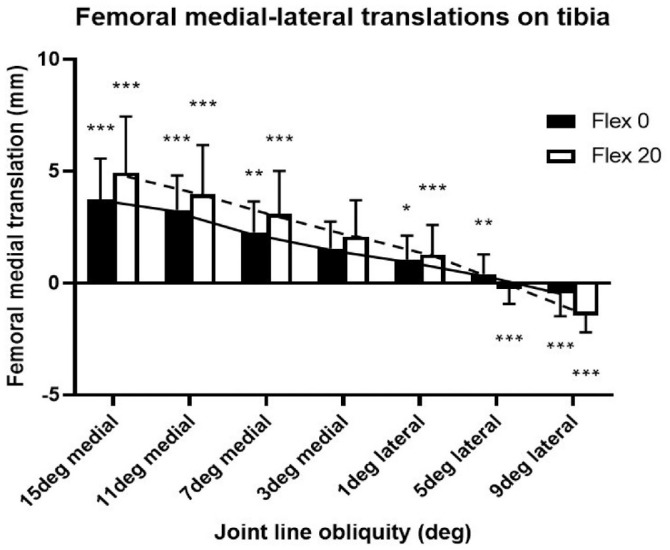
Medial-lateral translation of the femur in relation to the tibia when the knee was axially loaded to 1500 N at a range of coronal joint line obliquity. Values are shown as mean ± SD; n = 10. *P < .05, **P < .01, ***P < .001 versus the translation at 3° of medial joint line obliquity.
At 20° of knee flexion, the femoral ML translations followed the same pattern as at 0° of flexion, but with larger movements, so now the lateral translation was also significant with 9° lateral JLO (P < .001) (Figure 2).
Locations of the Peak Contact Pressures
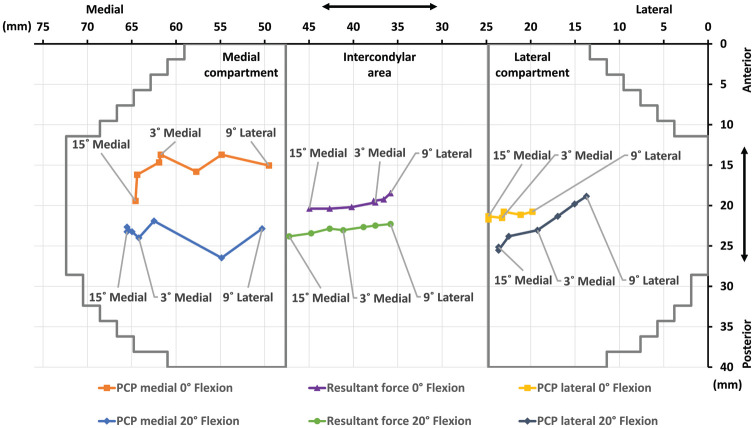
When the femur slid medially or laterally “downhill” as a result of the JLO, it caused the positions of the PCPs to move across each of the tibial condyles in the same direction (Figure 3). The movement of the PCP across each compartment was greater than the ML shifts of the femur, due to the joint surface conformity. In the medial compartment, the PCP moved mediolaterally by a mean of 15.2 mm at 0° of flexion and 16.1 mm at 20° in response to changing the JLO. In the lateral compartment, the PCP moved by a mean of 5.1 mm mediolaterally at 0° and 9.9 mm at 20°. These movements of the PCP caused the line of action of the resultant force acting on the joint also to move across the width of the tibial plateau, by approximately 12 mm.
Figure 3.
Schematic based on geometry of the pressure sensor to show movements of the mean positions of the peak contact pressure (PCP) across the medial and lateral compartments, as well as the resultant force near the center of the tibial plateau, in response to changes of joint line obliquity (JLO), at 0° and 20° of knee flexion. Medial refers to medial JLO; lateral refers to lateral JLO.
Peak Contact Pressure Variation With Joint Line Obliquity
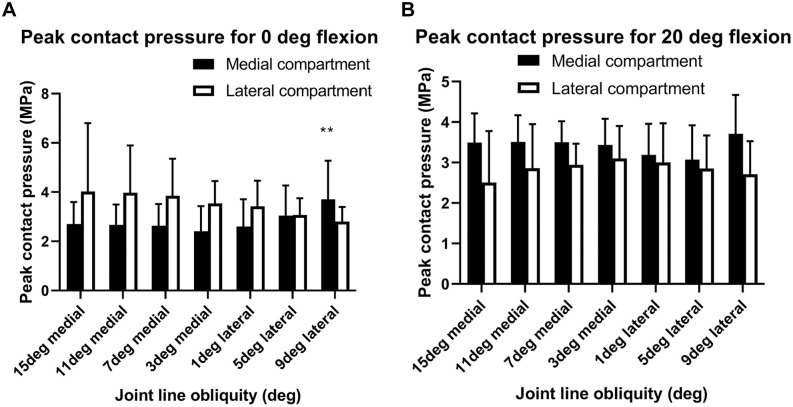
Although the position of the PCP moved considerably across each compartment in response to the femur shifting across the tibial plateau with changes of JLO, those movements were not followed by large changes of the magnitude of the PCP (Figure 4). We noted a significant effect of JLO on PCP in the medial compartment at 0° of flexion (P < .05) but not in the lateral compartment (P = .19). At 9° lateral JLO, the PCP had increased in the medial compartment at 0° of flexion.
Figure 4.
Peak contact pressure of the medial and lateral compartments at 0° and 20° of knee flexion. Medial and lateral axis values refer to medial downslope and lateral downslope, respectively. Values are shown as mean ± SD; n = 10. **P < .01 versus joint line obliquity at 3° of medial joint line obliquity.
Mean Contact Pressure Variation With Joint Line Obliquity
The mean contact pressures were in the range 1.0 to 1.3 MPa in both the medial and lateral compartments at both 0° and 20° of knee flexion across the range of JLO examined. An exception to this was that the mean contact pressures in the lateral compartment decreased with larger medial JLO, to 0.9 MPa (P < .05) and 0.7 MPa (P < .001) at 0° and 20° of flexion, respectively, at 15° medial JLO.
Articular and Meniscal Contact Pressures
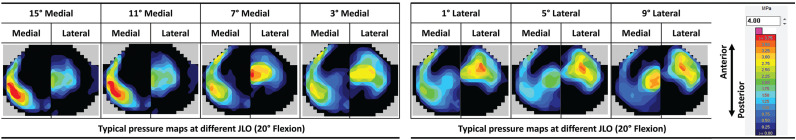
The pressure maps (Figure 5) show clearly how the contact stresses moved across the tibial plateau with changes of JLO. With medial JLO, the medial translation of the medial femoral condyle was resisted by the medial meniscus taking greatly increased load. At the same time, the lateral femoral condyle shifted medially and so the lateral compartment contact area shifted against the lateral intercondylar eminence (Figure 5).
Figure 5.
A typical set of pressure maps for one knee, showing the changes in pressure distribution of the medial and lateral compartments as a function of coronal tibial slope with the knee at 20° of flexion. When the medial downslope was increased, a higher pressure could be seen at the lateral part of the intercondylar eminence and on the medial meniscus. When the tibial slope was changed laterally, the areas of high pressure moved to the medial tibial intercondylar eminence and the lateral meniscus. JLO, joint line obliquity.
The opposite effects were seen with lateral JLO: The medial compartment contact area moved laterally against the medial tibial intercondylar eminence, whereas the movement of the lateral femoral condyle loaded the lateral meniscus (Figure 5).
Within each of the medial and lateral compartments, a clear reciprocal relationship was seen between the pressures acting on the meniscus and the tibial eminence (Figure 6). In the medial compartment, a medial JLO caused a high pressure on the medial meniscus and a low pressure where the femoral condyle moved away from the tibial eminence; a lateral JLO moved the medial condyle onto the medial eminence and off of the medial meniscus. The opposite trends were found in the lateral compartment (Figure 6).
Figure 6.
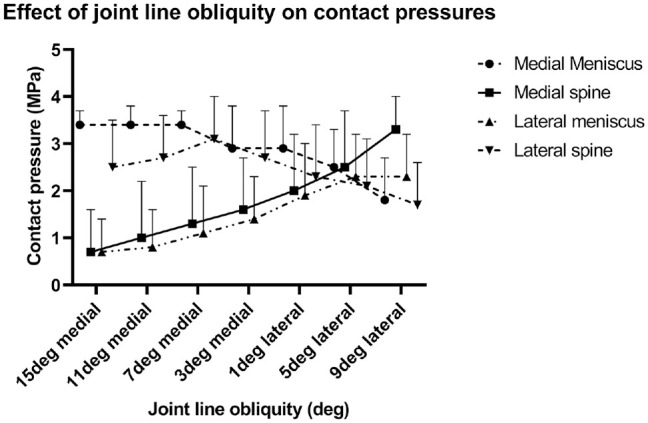
Variation of peak contact pressures on the meniscus and tibial eminence with joint line obliquity in the medial and lateral compartments of the knee. Values are shown as mean ± SD; n = 10.
Figure 6 reveals a synergy between the contact pressures on the medial meniscus and the lateral spine, and of the lateral meniscus with the medial spine, caused by the identical translations of the 2 femoral condyles across each of the compartments. All 4 variables converged at 4° lateral JLO.
Discussion
The most important finding of this study was that changing the slope of the knee joint line in the coronal plane (JLO) significantly affected the relative positions of the femur and tibia under load and the locations of the contact areas, as hypothesized. The ML subluxations caused elevated pressures on the menisci and the medial and lateral tibial intercondylar eminences. Contrary to the initial hypothesis, increased JLO did not directly increase contact pressures but rather moved the areas of high pressure mediolaterally across the condyles toward the menisci and intercondylar eminences. This is of considerable importance in understanding the effect of JLO on patients’ knees and, thus, in planning osteotomy.
Increasing JLO causes the femur to “slide downhill” across the tibial plateau, and this causes a shift in joint contact pressure locations, causing high stress at the intercondylar eminence of the tibia and the menisci. Although radiography shows that an ML translation of the femur causes impingement with the tibial eminence, the present study shows that it also causes the other (downhill) meniscus to act as a sling, resisting the shift of the femur by transmitting load back to the meniscotibial root attachments. This was confirmed in 1 loaded knee when the posterior root of the medial meniscus was transected, causing the femur to suddenly drop further into medial subluxation. It is also likely that the meniscofemoral ligaments attaching to the posterior horn of the lateral meniscus 17 were loaded when there was a lateral JLO. The positions of the highest pressure areas move far more than the bone-bone translations: For an ML translation of the femur of approximately 6 mm, the area of PCP moves 16 mm across the medial compartment and 8 mm across the lateral compartment. These findings have been observed clinically. Kim et al 22 reported that the femur subluxated medially across the tibia with varus deformity with medial compartment osteoarthritis and that this led to overcorrection into valgus after medial opening-wedge high tibial osteotomy (MOWHTO) as the joint line convergence angle reduced. Those investigators reported that the mechanism causing the ML subluxation was not well understood, and that is now clarified by the present study. Akamatsu et al 2 found that MOWHTO reduced femoral medial subluxation by 4 mm, but they did not report the JLO. In addition to these immediate mechanical changes, long-term outcomes may be influenced by the changes in articular contact conditions.
An abnormal JLO has been related to some aspects of inferior clinical outcomes at a mean of 2.5 years after surgery, 23 with high JLO most strongly related to higher medial proximal tibial angle due to the medial elevation after MOWHTO. A clinical review 30 found that JLO after surgery ranged from 9° lateral to 5° medial after a mean MOWHTO of 8°. In the present study, the range of JLO was from 9° lateral to 15° medial, causing significant changes of contact mechanics. Despite concerns about contact mechanics, a JLO of up to 10° was generally thought acceptable, 11 despite there being no biomechanical evidence to support that limit. Later work 6 developed double-level osteotomy to limit the JLO to a maximum of 4°, with good survival data. 5 Even though a normal medial proximal tibial angle is 87°, an angle of 95° has been used as the limit beyond which double-level osteotomy was implemented. 14
Two previous studies investigated the biomechanical consequences of tibiofemoral JLO. Hooper et al 19 studied 3 cadaveric knees and found increased contact pressure on the lateral tibial eminence with 10° medial JLO, which corresponds with the results of the present study. However, the ML femoral movement across the tibial plateau was only 3 mm when the JLO was varied 30°, compared with 6 mm in the present study when the JLO varied 24°. The larger ML subluxations in the present study were allowed by the low-friction XY table in the tibial mounting. Nakayama et al 28 used a computer model without menisci and predicted a higher contact pressure on the tibial spine with 10° lateral JLO. This also agrees with present findings, where the pressure at the medial tibial spine increased significantly at 9° lateral JLO. Nakayama et al estimated that the shear stress would increase significantly above 5° JLO.
The present study shows clearly that JLO potentially can be harmful because it leads to a nonphysiological pressure distribution pattern with high loads on the meniscus and tibial intercondylar eminence, due to femoral ML translation. These results need to be considered carefully in planning osteotomy including choice of bone to realign, degree of correction and consequent effect on JLO, and whether the correction should be shared between both femur and tibia (a double osteotomy) to maintain acceptable JLO. 14 It is not enough to simply plan the degree of correction for an osteotomy by measuring overall limb deformity alone; it is also critical to analyze the cause of the deformity. An appreciation of the shapes of the distal femur and proximal tibia is vitally important (as well as assessment of the convergence of joint surfaces; ie, the convergence angle); otherwise, JLO may occur.
Deviations of medial proximal tibial angle and/or lateral distal femoral angle can be seen in preoperative deformities or as an unavoidable consequence of single-level osteotomies.6,16,25,30 Several studies reported medial proximal tibial angle >95° after MOWHTO with a significant change in JLO.16,23,25,30 The change in JLO can be estimated as approximately 1° for each 2° of correction in the hip-knee-ankle (HKA) angle. 31 Double-level osteotomies should be considered, despite their greater morbidity rates, if tibial overcorrection and excessive JLO result.6,27,33 The question is, how much JLO is acceptable? Before the present experiment, we hypothesized that excessive JLO would cause higher contact stresses, leading to recommended limits of JLO. However, contrary to that hypothesis, changes of JLO caused large movements of the peak pressure across each of the medial and lateral compartments without causing large changes in the magnitudes of the contact pressures. Specific areas within each compartment—the menisci and the intercondylar eminences—are subjected to large changes of pressure as the JLO changes, so it is difficult to recommend a specific limit of JLO. It might be possible to relate the present findings to work showing that elevated contact pressure on a particular area of cartilage leads to degenerative changes 4 or to meniscal extrusion, for example. A further stage of this work could superimpose the JLO variations onto gait analysis, noting that JLO can vary while at a fixed HKA alignment and is (as far as we are aware) unreported in gait analyses of either patients with osteotomy or normal participants. This could be reported and would be interesting in the follow-up of HTO patients, showing the effect of JLO as well as HKA alignment.
This study has limitations and strengths. We acknowledge the limitations in transferring data gained from cadaveric specimens to knees in clinical situations, especially pertaining to the preparation and alignment of cadaveric specimens and the inability to translate normal physiological forces to the knee. The testing was performed at full extension and 20° of flexion because these parameters cover the load-bearing arc during the stance phase of gait. The 1500-N compressive load reproduced the mean force across the stance phase of gait 36 and could have been normalized to subject-specific weight, although cadavers are often subject to premortal changes of body weight and body mass index. However, the compressive load used did not reproduce the loads in sporting activity, which would have produced larger effects. Although the study findings are related to osteotomy, the experimental design did not involve osteotomy. This was because our intent was not to study osteotomy itself but rather to isolate the mechanical effect of alterations in JLO within the knee. This was achieved accurately by simply realigning the joint line relative to the mechanical axis; a similar design has been used previously. 19 This setup avoided inaccuracies with osteotomy arising from cutting the bones and reorientation and fixation of bone fragments outside of the knee, which should in any case have led to identical results within the knee as the method used in the present study. Also with cadaveric bone quality, osteotomy fixation might have been hard to maintain. This study of JLO did not include the effects of osteotomy on soft tissue tension, such as release of the superficial medial collateral ligament with MOWHTO, which affects joint contact pressures.1,35 Noting these points, however, we must keep in mind that changes of JLO are a byproduct of limb realignment osteotomy surgery. This work used normal knees that had not experienced loss of joint space and related ligament slackening, which might have increased the ML translations. In future work on HTO, it would be desirable to use knees with pathological cartilage loss in the medial compartment, corresponding to a varus HKA misalignment, or at least a loading setup that simulates this situation. Such a design would mix the effects of changes of JLO with changes of the knee adduction moment during gait and consequent shifting of the load axis across the width of the knee, with corresponding ML force redistribution. One of the strengths of the present study is that it has isolated the JLO effect from the clinical complexity described. The advantages of the design of the test rig included the tibial mounting that allowed free coupled ML and AP translations and free abduction and adduction rotations caused by joint compression loads. The pressure sensor in the joint space might have affected the behavior of the joint, being approximately 0.5 mm thick and requiring small incisions of the anterior and posterior capsular meniscotibial ligaments, which might have affected the motion of the menisci, although the root attachments were undisturbed. The pressure sensor could not fit the exact shapes and sizes of all the joints, nor could it take accurate readings from the sides of the tibial eminences, because the slope there would have caused shear stresses in the sensor, and it is not designed to resist or measure shearing. However, the experimental design allowed us to test the effects of a range of JLOs in each knee, allowing repeated-measures intraspecimen comparisons, thus largely eliminating interspecimen or other surgical effects. Finally, the purpose of this study was to discover the effect of altering JLO alone, with the joint force always imposed along a central axis. In clinical work, the JLO changes as a secondary byproduct of realigning the limb, and that, of course, is intended to move the joint force across the width of the knee. Thus, in clinical use, although the JLO affects the ML shearing of the tibiofemoral joint, the osteotomy superimposes an alteration of the ML load balance: The present study has shown how the resulting changes of JLO influence the knee, and their effects appear not to be negligible.
This work has shown clearly that JLO causes significant changes in knee joint mechanics, and these findings may be related to clinical procedures:
Medial JLO caused larger medial translation of the femur across the tibial plateau than the same lateral JLO caused lateral translation. Changing JLO by 4° in either direction changed the position of the loaded femur on the tibia significantly.
The ML translations of the femur caused the PCPs to move across the plateau further than the actual bone-bone movements, due to the articular geometry.
The articular PCP moved against the tibial eminence, which articulated with the adjacent femoral condyle.
The JLO caused the downhill femoral condyle to slide onto the meniscus, transmitting load to the rim of the tibial plateau. This will cause large tension in the meniscotibial root attachments, so meniscectomy may increase the mechanical changes resulting from JLO.
Contrary to the initial hypothesis of this study, changes of JLO did not cause large changes of PCP across the whole medial and lateral compartments.
Specific areas of the tibial plateau and meniscus were subjected to large changes of contact pressure. Moving the loads onto areas that are not adapted to bear them has been related to degenerative changes 4 ; loading the tibial eminence is the price of unloading the same compartment.
The ML movements of the contact pressures in each compartment caused the line of action of the resultant joint force to also move, by approximately 1 mm for each 2° change of JLO. This is negligible in the clinical context, where a change of tibial orientation of 1° can move the load axis at the knee by 8 mm, if the tibia is 450 mm long.
It is difficult to transfer these findings into recommendations for clinical work, not only because of the need to be circumspect in going from laboratory to clinic but also because of the lack of full data sets and long follow-ups in clinical studies that would support this. When Oh et al 30 corrected 6° varus to 3° valgus HKA by MOWHTO, unsurprisingly the medial elevation of the tibial plateau moved the JLO toward lateral but only by a mean of 2° (but with a large range, from 14° lateral to 5° medial), so the effect of osteotomy on JLO is not simple. If the mechanical axis from hip to ankle does not change, then a valgising high tibial osteotomy will lead to femoral adduction and, hence, a more lateral JLO. 7 However, these comments are not supported by data on the effects of specific tissue contact pressures on long-term degeneration that would validate clinical recommendations. It is desirable that long-term level 1 studies of osteotomy are conducted and that among many important factors, JLO should be measured to ascertain the clinical effect of this variable.
Although our results do not allow a recommendation of safe maximum medial and lateral JLO, the message is clear that the surgeon cannot afford to be casual with resultant JLO after osteotomy, because the consequences for the joint can be profound.
Conclusion
A 4° change of JLO in either valgus or varus caused significant mediolateral tibiofemoral subluxations, with large movements of the contact pressures across each of the medial and lateral compartments, as the femur slid downhill. A medial JLO caused the femur to translate medially, imposing high load onto the lateral tibial eminence and the medial meniscus, and vice versa for lateral JLO.
Footnotes
Submitted August 5, 2020; accepted February 19, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: Financial support for this work was paid by Fortius Research and Education Foundation, which was supported by DePuy Synthes Co. L.W. has received salary support from the German Foundation for Research. K.K.A. has received salary support from Smith & Nephew paid via the Imperial College London. A.W. is director of Innovation Orthopaedics Co and of Fortius Clinic London and has received speaking fees from Smith & Nephew Inc. A.A.A. is director of Orthonika Co and has received speaking fees from Smith & Nephew Inc. The Instron test machine was purchased with an equipment grant from Arthritis Research UK. The tissue specimens were provided by the MedCure tissue bank, Portland, Oregon, USA. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Agneskirchner JD, Hurschler C, Wrann CD, Lobenhoffer P. The effects of valgus medial opening wedge high tibial osteotomy on articular cartilage pressure of the knee: a biomechanical study. Arthroscopy. 2007;23(8):852-861. [DOI] [PubMed] [Google Scholar]
- 2. Akamatsu Y, Ohno S, Kobayashi H, Kusayama Y, Kumagai K, Saito T. Coronal subluxation of the proximal tibia relative to the distal femur after opening wedge high tibial osteotomy. Knee. 2017;24(1):70-75. [DOI] [PubMed] [Google Scholar]
- 3. Amis AA. Biomechanics of high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2013;21(1):197-205. [DOI] [PubMed] [Google Scholar]
- 4. Andriacchi TP, Mundermann A, Smith RL, Alexander EJ, Dyrby CO, Koo S. A framework for the in vivo pathomechanics of osteoarthritis at the knee. Ann Biomed Eng. 2004;32:447-457. [DOI] [PubMed] [Google Scholar]
- 5. Babis GC, An KN, Chao EY, Larson DR, Rand JA, Sim FH. Upper tibia osteotomy: long term results—realignment analysis using OASIS computer software. J Orthop Sci. 2008;13(4):328-334. [DOI] [PubMed] [Google Scholar]
- 6. Babis GC, An KN, Chao EY, Rand JA, Sim FH. Double level osteotomy of the knee: a method to retain joint-line obliquity: clinical results. J Bone Joint Surg Am. 2002;84(8):1380-1388. [DOI] [PubMed] [Google Scholar]
- 7. Bartholomeeusen S, van den Bempt M, van Beek N, Claes T, Claes S. Changes in knee joint line orientation after high tibial osteotomy are the results of adaptation of the lower limb to the new alignment. Knee. 2020;27(3):777-786. [DOI] [PubMed] [Google Scholar]
- 8. Bernhardson AS, Aman ZS, Dornan GJ, et al. Tibial slope and its effect on force in anterior cruciate ligament grafts: anterior cruciate ligament force increases linearly as posterior tibial slope increases. Am J Sports Med. 2019;47(2):296-302. [DOI] [PubMed] [Google Scholar]
- 9. Birmingham TB, Giffin JR, Chesworth BM, et al. Medial opening wedge high tibial osteotomy: a prospective cohort study of gait, radiographic, and patient-reported outcomes. Arthritis Rheum. 2009;61(5):648-657. [DOI] [PubMed] [Google Scholar]
- 10. Bonnin MP, Laurent JR, Zadegan F, Badet R, Pooler Archbold HA, Servien E. Can patients really participate in sport after high tibial osteotomy? Knee Surg Sports Traumatol Arthrosc. 2013;21(1):64-73. [DOI] [PubMed] [Google Scholar]
- 11. Coventry MB. Proximal tibial varus osteotomy for osteoarthritis of the lateral compartment of the knee. J Bone Joint Surg Am. 1987;69(1):32-38. [PubMed] [Google Scholar]
- 12. El-Azab HM, Morgenstern M, Ahrens P, Schuster T, Imhoff AB, Lorenz SG. Limb alignment after open-wedge high tibial osteotomy and its effect on the clinical outcome. Orthopedics. 2011;34(10):e622-628. [DOI] [PubMed] [Google Scholar]
- 13. Faul F, Erdfelder E, Lang A-G, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Meth. 2007;39:175-191. [DOI] [PubMed] [Google Scholar]
- 14. Feucht MJ, Winkler PW, Mehl J, et al. Isolated high tibial osteotomy is appropriate in less than two-thirds of varus knees if excessive overcorrection of the medial proximal tibial angle should be avoided. Knee Surg Sports Traumatol Arthrosc. Published online July 20, 2020. doi: 10.1007/s00167-020-06166-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Floerkemeier S, Staubli AE, Schroeter S, Goldhahn S, Lobenhoffer P. Outcome after high tibial open-wedge osteotomy: a retrospective evaluation of 533 patients. Knee Surg Sports Traumatol Arthrosc. 2013;21(1):170-180. [DOI] [PubMed] [Google Scholar]
- 16. Goshima K, Sawaguchi T, Shigemoto K, Iwai S, Fujita K, Yamamuro Y. Comparison of clinical and radiologic outcomes between normal and overcorrected medial proximal tibial angle groups after open-wedge high tibial osteotomy. Arthroscopy. 2019;35(10):2898-2908. [DOI] [PubMed] [Google Scholar]
- 17. Gupte CM, Bull AMJ, Thomas RD, Amis AA. A Review of the function and biomechanics of the meniscofemoral ligaments. Arthroscopy 2003;19:161-171. [DOI] [PubMed] [Google Scholar]
- 18. Hofmann S, Lobenhoffer P, Staubli A, Van Heerwaarden R. Osteotomies of the knee joint in patients with monocompartmental arthritis [in German]. Orthopade. 2009;38(8):755-769. [DOI] [PubMed] [Google Scholar]
- 19. Hooper JM, Walker P, Hsu TT, et al. Biomechanical implications of an oblique knee joint line. J Knee Surg. 2018;31(8):761-766. [DOI] [PubMed] [Google Scholar]
- 20. Hsu RW, Himeno S, Coventry MB, Chao EY. Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clin Orthop Relat Res. 1990;255:215-227. [PubMed] [Google Scholar]
- 21. Inderhaug E, Stephen JM, Williams A, Amis AA. Anterolateral tenodesis or anterolateral ligament complex reconstruction: effect of flexion angle at graft fixation when combined with ACL reconstruction. Am J Sports Med. 2017;45(13):3089-3097. [DOI] [PubMed] [Google Scholar]
- 22. Kim YT, Choi JY, Lee JK, Lee YM, Kim JI. Coronal tibiofemoral subluxation is a risk factor for postoperative overcorrection in high tibial osteotomy. Knee 2019;26:832-837. [DOI] [PubMed] [Google Scholar]
- 23. Kubota M, Kim Y, Sato T, et al. The actual knee function was not influenced by joint line obliquity after open-wedge high tibial osteotomy. SICOT J. 2020;6:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lagae KC, Robberecht J, Athwal KK, Verdonk PCM, Amis AA. ACL reconstruction combined with lateral monoloop tenodesis can restore intact knee laxity. Knee Surg Sports Traumatol Arthrosc. 2020;28(4):1159-1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lee KM, Chang CB, Park MS, Kang SB, Kim TK, Chung CY. Changes of knee joint and ankle joint orientations after high tibial osteotomy. Osteoarthritis Cartilage. 2015;23(2):232-238. [DOI] [PubMed] [Google Scholar]
- 26. Lind M, McClelland J, Wittwer JE, Whitehead TS, Feller JA, Webster KE. Gait analysis of walking before and after medial opening wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2013;21(1):74-81. [DOI] [PubMed] [Google Scholar]
- 27. Nakayama H, Iseki T, Kanto R, et al. Physiologic knee joint alignment and orientation can be restored by the minimally invasive double level osteotomy for osteoarthritic knees with severe varus deformity. Knee Surg Sports Traumatol Arthrosc. 2020;28(3):742-750. [DOI] [PubMed] [Google Scholar]
- 28. Nakayama H, Schroter S, Yamamoto C, et al. Large correction in opening wedge high tibial osteotomy with resultant joint-line obliquity induces excessive shear stress on the articular cartilage. Knee Surg Sports Traumatol Arthrosc. 2018;26(6):1873-1878. [DOI] [PubMed] [Google Scholar]
- 29. Niemeyer P, Koestler W, Kaehny C, et al. Two-year results of open-wedge high tibial osteotomy with fixation by medial plate fixator for medial compartment arthritis with varus malalignment of the knee. Arthroscopy. 2008;24(7):796-804. [DOI] [PubMed] [Google Scholar]
- 30. Oh KJ, Ko YB, Bae JH, Yoon ST, Kim JG. Analysis of knee joint line obliquity after high tibial osteotomy. J Knee Surg. 2016;29(8):649-657. [DOI] [PubMed] [Google Scholar]
- 31. Park JY, Chang CB, Kang DW, Oh S, Kang SB, Lee MC. Development and validation of a prediction model for knee joint line orientation after high tibial osteotomy. BMC Musculoskelet Disord. 2019;20(1):434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Schroter S, Ateschrang A, Lowe W, Nakayama H, Stockle U, Ihle C. Early full weight-bearing versus 6-week partial weight-bearing after open wedge high tibial osteotomy leads to earlier improvement of the clinical results: a prospective, randomised evaluation. Knee Surg Sports Traumatol Arthrosc. 2017;25(1):325-332. [DOI] [PubMed] [Google Scholar]
- 33. Schroter S, Nakayama H, Yoshiya S, Stockle U, Ateschrang A, Gruhn J. Development of the double level osteotomy in severe varus osteoarthritis showed good outcome by preventing oblique joint line. Arch Orthop Trauma Surg. 2019;139(4):519-527. [DOI] [PubMed] [Google Scholar]
- 34. Schuster P, Gesslein M, Schlumberger M, et al. Ten-year results of medial open-wedge high tibial osteotomy and chondral resurfacing in severe medial osteoarthritis and varus malalignment. Am J Sports Med. 2018;46(6):1362-1370. [DOI] [PubMed] [Google Scholar]
- 35. Seitz AM, Nelitz M, Ignatius A, Durselen L. Release of the medial collateral ligament is mandatory in medial open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2019;27(9):2917-2926. [DOI] [PubMed] [Google Scholar]
- 36. Shelburne KB, Torry MR, Pandy MG. Contributions of muscles, ligaments, and the ground-reaction force to tibiofemoral joint loading during normal gait. J Orthop Res. 2006;24(10):1983-1990. [DOI] [PubMed] [Google Scholar]
- 37. Willinger L, Foehr P, Achtnich A, et al. Effect of lower limb alignment in medial meniscus-deficient knees on tibiofemoral contact pressure. Orthop J Sports Med. 2019;7(2):2325967118824611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Willinger L, Lang JJ, Berthold D, et al. Varus alignment aggravates tibiofemoral contact pressure rise after sequential medial meniscus resection. Knee Surg Sports Traumatol Arthrosc. 2020;28(4):1055-1063. [DOI] [PubMed] [Google Scholar]
- 39. Wylie JD, Scheiderer B, Obopilwe E, et al. The effect of lateral opening wedge distal femoral varus osteotomy on tibiofemoral contact mechanics through knee flexion. Am J Sports Med. 2018;46(13):3237-3244. [DOI] [PubMed] [Google Scholar]