Abstract
Amid the coronavirus disease 2019 (COVID-19) pandemic, there is an unprecedented increase in public avoidance of hospitals predominantly driven by fear of contracting the virus. Recent publications highlight a re-emergence of rare post–myocardial infarction complications. While mechanical complications are infrequent in the era of primary percutaneous coronary intervention, they are associated with high mortality rates. The concurrent occurrence of mechanical complications such as left ventricular aneurysm and ventricular septal rupture is an extremely rare entity. We hereby delineate a unique case of a 53-year-old Caucasian male who underwent successful concomitant closure of a ventricular septal rupture, left ventricular aneurysmectomy, and 3-vessel coronary artery bypass grafting. Due to a delayed initial presentation owing to the patient’s fear of contracting COVID-19, the surgery was carried out 3 months after the myocardial infarction. His postoperative evaluation confirmed normal contractility of the left ventricle and complete closure of the ventricular septal rupture. Six months postoperatively, the patient continues to do well. We also present a literature review of the mechanical complications following delayed presentation of myocardial infarction amid the COVID-19 pandemic. This article illustrates that clinicians should remain cognizant of these extremely rare but potentially lethal collateral effects during the ongoing global public-health challenge. Furthermore, it highlights a significant concern regarding the delay in first medical contact due to the reluctance of patients to visit the hospital during the COVID-19 pandemic.
Keywords: coronavirus disease 2019, ST-segment elevation myocardial infarction, left ventricular aneurysm, ventricular septal rupture, delayed MI presentation, mechanical complications
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has become a major global health challenge of this century with more than 183 million confirmed cases and over 3.97 million deaths to date. It has affected health care systems throughout the world even in the wake of recent advents such as the COVID-19 vaccine, thereby necessitating radical changes in therapeutic protocols. Consequently, the initial management of time-sensitive cardiovascular emergencies such as ST-elevation myocardial infarction (STEMI) has been limited to fibrinolytic therapy in some hospitals, often delaying the necessary percutaneous coronary intervention (PCI). 1 One study from the United States showed an estimated 38% decrease in STEMI activations during the early phase of the pandemic. 2 Similarly, a 40% decline was observed in STEMI interventions in Spain. 3 Global lockdowns, social distancing guidelines, and awareness campaigns to limit the spread of COVID-19 have resulted in a decline in timely myocardial infarction (MI) presentations worldwide. Several studies posit that the public fear of acquiring COVID-19 in the hospital might indeed be responsible for this exorbitant decline.2-4
It is notable that the incidence of serious post–MI mechanical complications has decreased remarkably over the past few decades due to early reperfusion using primary PCI. In this context, the re-emergence of once-grave but now antiquated entities such as mechanical complications after MI during COVID-19 pandemic is perplexing.5,6 The resurgence of mechanical complications can be attributed, in part, to delayed MI presentations resulting in a delay in revascularization. We chronicle here the case of a STEMI patient who reportedly avoided making first medical contact for over 3 months owing to his fear of contracting COVID-19 in the hospital. After a significantly delayed presentation, his workup confirmed the simultaneous presence of a left ventricular aneurysm (LVA) and a Becker type III ventricular septal rupture (VSR) complicating his STEMI. In addition, we undertake a systematic literature review of mechanical complications associated with delayed MI presentation amid the COVID-19 pandemic. This article highlights the need for improved public awareness and education to seek early medical care for emergent cardiovascular conditions.
Illustrative Case
Presentation
A 53-year-old obese Caucasian man presented to our medical center with a 3-month history of worsening shortness of breath and lower extremity edema. The patient described associated diaphoresis but denied any chest pain or dizziness. He did not seek medical attention early due to his apprehensions surrounding COVID-19. He denied alcohol intake or illicit drug dependence. He was not on therapy with any medications, denied recent hospitalization, and had not seen his primary care doctor in the last 10 years. At presentation, he was afebrile and hemodynamically stable.
Investigations
The patient underwent extensive diagnostic workup (Table 1). Electrocardiogram demonstrated ST-segment elevations in the inferior leads (Figure 1). He then underwent emergent coronary angiography, which divulged severe multi-vessel coronary artery disease, with complete occlusion of mid-right coronary artery (Figure 2; Supplementary Videos 1 and 2, available online). Left ventriculography revealed inferior wall hypokinesis of left ventricle with basilar inferior segment aneurysm and mural thrombus (Figure 3; Supplementary Video 3, available online). It also showed possible left-to-right shunt via an interventricular septum. The procedure was halted without PCI and the patient was admitted to coronary care unit for cardiothoracic surgery consultation. Transthoracic echocardiography showed mildly reduced biventricular function (left ventricular ejection fraction: 40% to 45%), with a basal inferior wall aneurysm and small VSR with left-to-right shunt (Supplementary Videos 4 and 5, available online). Cardiac magnetic resonance imaging was recommended by cardiothoracic surgery. It showed a wide-mouthed aneurysm in the base of the inferior wall, measuring 5.2 × 5.3 × 4.4 cm with an associated mural thrombus (Figure 4). There was a small-sized VSR in the inferior and basal aspect of interventricular septum, causing left-to-right shunt (Qp/Qs: 1.7; Table 2). Transmural delayed enhancement, involving mid and basal inferior septum, was suggestive of nonviable myocardium (Figure 5). No evidence of mitral regurgitation was present. Coronavirus testing via nasopharyngeal swab was negative.
Table 1.
Patient Laboratory Values on Admission and During Hospitalization.
| Laboratory parameters, units | Normal value range | Day 1 | Day 2 | Day 3 | Day 4 | Day 5 |
|---|---|---|---|---|---|---|
| Aspartate transaminase, U/L | 3-40 | 429 | 255 | 192 | 139 | 98 |
| Alanine aminotransferase, U/L | 3-37 | 1329 | 1023 | 779 | 596 | 443 |
| Lactate dehydrogenase, U/L | 120-240 | 86 | 82 | 69 | 94 | 91 |
| Alanine aminotransferase/lactate dehydrogenase ratio | >1.50 | 15.4 | 12.5 | 11.3 | 6.3 | 4.8 |
| Total bilirubin, mg/dL | 0.30-1.00 | 3 | 2.4 | 2.3 | 1.4 | 1.1 |
| Creatine kinase, U/L | 30-200 | 77 | 86 | 81 | 80 | 96 |
| Troponin I, ng/L | 0.0-34.2 | 0.17 | 0.16 | 0.17 | 0.14 | 0.10 |
| White cell count, 103/µL | 4.0-10.0 | 14.5 | 13.2 | 10.4 | 8.8 | 7.9 |
| Hemoglobin, g/dL | 13.0-17.0 | 13.8 | 14.1 | 12.6 | 13 | 12.6 |
| Creatinine, mg/dL | 0.73-1.18 | 1.14 | 0.95 | 0.86 | 0.89 | 0.77 |
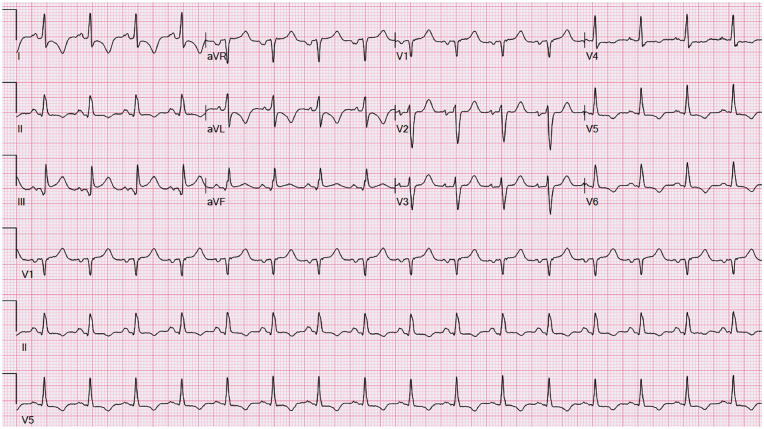
Figure 1.
Twelve-lead electrocardiography at presentation. A 12-lead electrocardiogram shows ST elevation in inferior leads (II, III, AVF) with reciprocal ST depressions in lateral leads (I, AVL, V4-V6).
Figure 2.
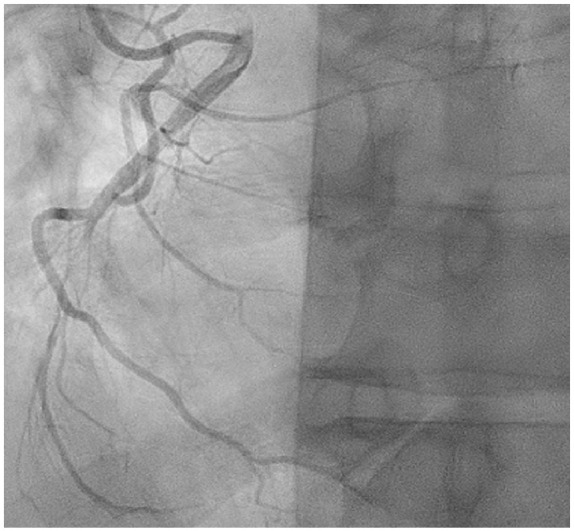
Angiography of right coronary artery (RCA) in left anterior oblique projection. It demonstrates complete occlusion of the mid vessel with the reconstitution of distal RCA from right to right collaterals.
Figure 3.
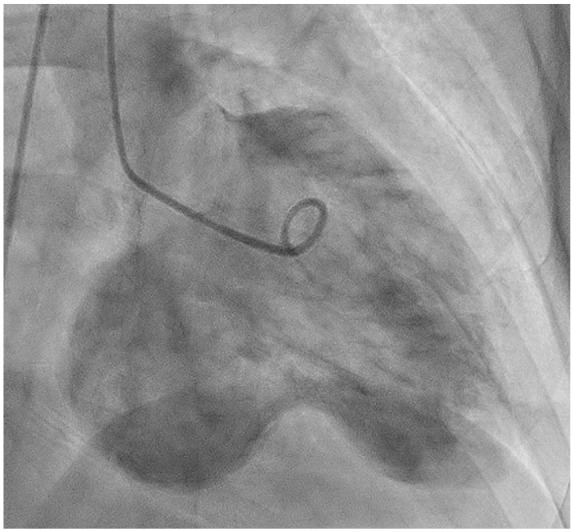
Left ventriculogram. Left ventriculogram in anterior oblique (RAO) projection demonstrating an inferobasal wall true aneurysm.
Figure 4.
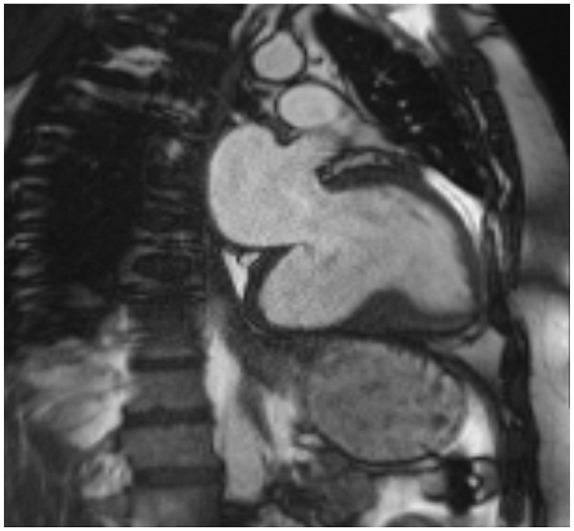
Cardiac magnetic resonance (CMR) imaging. CMR imaging in sagittal view (2-chamber view) demonstrating left ventricular true aneurysm.
Table 2.
Right Heart Catheterization Measurements.
| Hemodynamic parameters | Patient measurements |
|---|---|
| Aortic pressure, systolic/diastolic (mean), mm Hg | 139/78 |
| Right ventricle pressure, systolic/diastolic (mean), mm Hg | 60/27 |
| Pulmonary artery pressure, systolic/diastolic (mean), mm Hg | 57/31 |
| Right atrium pressure, mean, mm Hg | 14 |
| Pulmonary capillary wedge pressure, mean, mm Hg | 18 |
| Pulmonary blood flow, Qp, 1/min | 10 |
| Systemic blood flow, Qs, 1/min | 5.9 |
| Qp/Qs ratio | 1.7 |
Figure 5.
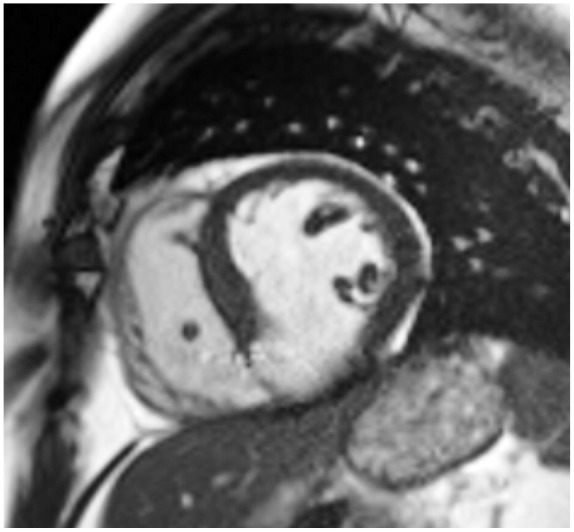
Cardiac magnetic resonance (CMR) imaging. Short-axis view of heart on CMR imaging showing ventricular septal rupture at inferobasal left ventricle.
Management
After multidisciplinary team discussion, cardiothoracic surgery planned curative resection. The patient remained hemodynamically stable and was started on heparin infusion. He underwent an uneventful removal of mural thrombus, aneurysmectomy, and VSR patch repair. The step-wise approach to the aneurysmectomy procedure is outlined in the flowchart (Figure 6). Furthermore, he also underwent 3-vessel coronary artery bypass grafting (CABG) for his multivessel disease. He tolerated the procedures well.
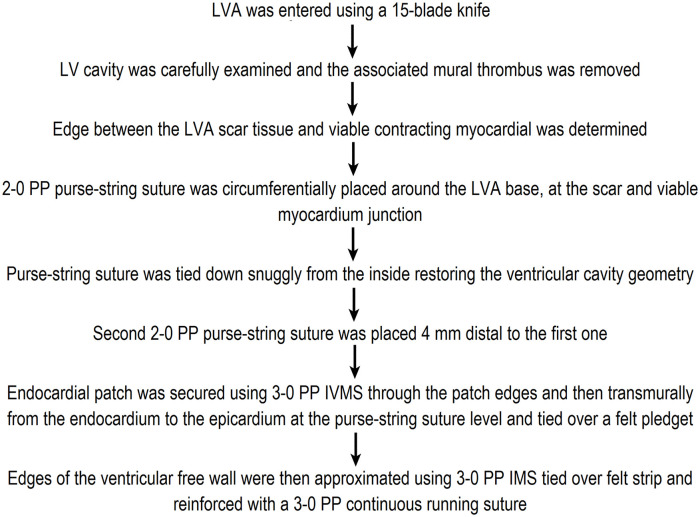
Figure 6.
The step-wise approach to the aneurysmectomy procedure. LVA, left ventricular aneurysm; PP, polypropylene; IVMS, interrupted vertical mattress sutures; IMS, interrupted mattress sutures.
Clinical Outcome and Follow-up
His hospital course was uncomplicated. After 5 days of postoperative monitoring, he was discharged from the hospital in a stable condition. At the 6-month follow-up, he did not report any chest pain or shortness of breath, and his surgical wounds appeared well-healed. The patient continues to do well to date.
Methods
In order to study trends of mechanical complications following delayed presentation of acute MI amid COVID-19 pandemic, we conducted a systematic search of medical databases, including MEDLINE (PubMed and Ovid), Embase, Scopus, and Cochrane. Furthermore, we reviewed conference papers from major cardiology scientific meetings. A comprehensive search strategy was constructed in order to identify relevant articles, using a combination of keywords. Search terminologies such as “mechanical complications,” “acute myocardial infarction,” “STEMI,” and “delayed presentation” were combined using the Boolean operators “AND” and “OR” with the terms “COVID-19,” “SARS-CoV-2,” “Coronavirus,” and “pandemic,” with all associated permutations. English-only articles were considered, without an application of a defined time filter. Two of the authors independently reviewed the titles and abstracts of the articles obtained from the initial search. For the eligibility of each study, full-text versions of potentially relevant articles were independently retrieved and reviewed by the other 2 authors. Concerns regarding the eligibility of individual studies were resolved after joint reassessment and consensus. The final inclusion of an article into quantitative analysis was based on a discussion headed by the senior author. The descriptive data are presented as mean ± standard deviation, range, or percentage, as applicable.
Results
Initial database search yielded a total of 217 articles. A vast majority of articles were excluded as they were redundant (n = 102), duplicate (n = 28), reported pre-COVID-19 results (n = 19), did not describe individual patient data (n = 16), or the language was other than English (n = 12). A total of 40 studies were accessed in the full-version form in order to determine eligibility. It resulted in the further exclusion of irrelevant studies (n = 19). Finally, a total of 21 articles were identified to be pertinent with regard to the scope of this study and were included in the final quantitative analysis.
Mechanical complications following delayed MI presentations were described in a total of 26 case reports only (level of clinical evidence: IV) in 21 selected articles included in this study, dating from June 2020 to May 2021.7-27 No gender predominance was noted as the male-to-female ratio was 1:1). The age of patients ranged from 37 to 87 years (mean ± standard deviation = 64.12 ± 53.70 years). Notably, 24 (92%) of 26 patients were over 50 years of age. This observation may facilitate enhanced suspicion of mechanical complications in elderly patients (50 years and over) admitting with delayed MI presentations. In terms of the temporal relationship between the MI occurrence and onset of aforementioned complications, 20 (77%) of 26 patients developed symptoms within the first week after MI. Chest pain 18 (69%), dyspnea 13 (50%), and lightheadedness 4 (15%) were among the frequently encountered clinical presentations. On cardiac catheterization, a variety of underlying coronary artery lesions were identified. With regard to the detection of post-MI mechanical complications, transthoracic echocardiography was usually the first investigation employed to identify the type, location, and subsequent hemodynamic sequelae. These patients may require prompt hemodynamic stabilization, which may necessitate a combination of medical therapy and mechanical circulatory support such as intra-aortic balloon pump 5 (19%), extracorporeal membrane oxygenation 2 (8%), and Impella 5.0 support 1 (4%). Surgery was performed in 17 (63%) patients. However, the optimal timing for surgical intervention remains to be determined in this setting. Notably, percutaneous therapeutic approaches were applied in 7 (27%) patients, denoting them as an emerging alternative treatment option for patients at prohibitive surgical risk. Of 26 patients for whom clinical outcomes were reported, a total of 8 (31%) patients died, whereas 2 (8%) patients remained under critical care. Notably, 16 (62%) patients recovered from these serious complications. The data regarding patient demographics, presenting symptoms, time from symptom onset to presentation, electrocardiographic features, anatomic findings, nature of mechanical complications, left ventricular ejection fraction, treatment, and clinical outcomes are summarized (Table 3).7-27
Table 3.
Literature Review of Mechanical Complications After Delayed Presentations of Acute MI During COVID-19 Pandemic.
| Authors | Publication time (month/year) | Age/sex (year) | Presenting symptoms | Time from symptom onset to presentation to ER | Electrocardiographic features | Anatomic findings | Complications | LVEF | Treatment | Clinical outcome |
|---|---|---|---|---|---|---|---|---|---|---|
| Gaballa et al 7 | June 2020 | 87/Female | Nonexertional, epigastric, nonradiating, sharp chest pain | Several days | Normal sinus rhythm with T-wave inversions in the anterolateral leads | Significant stenosis of the LAD s/p placement of a DES | VSR | 35% to 40% | Family decided to change goals of care to comfort care measures | Died |
| Masroor et al 8 | June 2020 | 48/Male | Persistent chest pain | 2 days | Inferolateral STEMI | Occlusion of the dominant RCA | VSR with Qp/Qs was 3 | 25% | PCI + IABP + surgical repair | Recovered |
| Atreya et al 9 | August 2020 | 52/Male | Dyspnea, chest pressure, and altered mental status | Sinus rhythm with ST-segment depression in the precordial leads | Thrombotic occlusion of the middle left circumflex artery | Severe MR with ruptured papillary muscle | Normal | Venoarterial ECMO + IABP + surgical mitral valve replacement | Recovered | |
| Albiero et al 10 | August 2020 | 72/Male | Severe chest pain | 5 days | Extensive anterolateral STEMI | Coronary angiography showed proximal LAD artery occlusion | Subacute LV free wall rupture with mural thrombus | 25% | PCI + surgical repair | Recovered |
| Shah et al 11 | August 2020 | 75/Female | Progressive chest pain | 7 days | Inferolateral STE Inferior Q waves Broad R waves V1-V2 |
Tortuous 100% mid-RCA occlusion with TIMI flow grade 0 80% distal left main 80% proximal LAD |
VSR Basal inferolateral wall pseudoaneurysm IABP | 50% to 55% | PCI with an IABP | The patient was sent for urgent CABG |
| Ahmed et al 12 | August 2020 | 82/Female | Worsening shortness of breath and leg swelling | 2 days | ST-segment elevations in leads V2-V6 with Q waves in leads I, aVL, V5-V6 | LHC revealed acute total occlusion of the proximal LAD, diffuse 40% stenosis in the LCx, 70% stenosis of ramus intermedius, and 40% stenosis of mid-RCA | VSR with Qp/Qs was 1.56 | 30% | Percutaneous closure of VSR | Recovered |
| Ahmed et al 13 | August 2020 | 65/Male | Shortness of breath | 3 days | ST-segment elevation in leads II, III, and aVF with small Q waves | LHC revealed a completely occluded RCA at the mid-segment | VSR with Qp/Qs was 4.6 | 40% | CABG + patch repair of VSR | Recovered |
| Joshi et al 14 | August 2020 | 72/Female | Substernal chest heaviness radiating to the back and bilateral upper limbs, and lightheadedness | 14 hours | ST-segment elevation in the inferior leads with associated Q waves and reciprocal ST-segment depressions in high lateral leads | Coronary angiography demonstrated acute thrombotic occlusion of the mid RCA stent and no obstructive CAD in the left main, LAD, and left circumflex arteries | VSR with Qp/Qs was 2.2 | Not reported | PCI of the mid RCA with 1 DES + comfort measures only as per patient’s wishes | Died |
| Alsidawi et al 15 | August 2020 | 67/Female | Chest pain, shortness of breath, and hypotension | 5 days | Inferior ST-segment elevation with Q waves | Dominant RCA was totally occluded | VSR with Qp/Qs was 1.6 | 50% | Complex ventricular septal repair + a right ventricular assist device | Remained critically ill in the ICU |
| Qureshi et al 16 | August 2020 | 68/Female | Lightheadedness, pre-syncope, and shoulder pain | 7 days | Posterior MI | 100% occlusion of an inferior distal branch of a large second obtuse marginal | Ventricular free wall rupture | 35% to 40% | IABP + blood evacuation from pericardium | Recovered |
| Qureshi et al 16 | August 2020 | 72/Female | Weakness, shortness of breath followed by a mechanical fall | 4 days | Remote inferior infarct and anterolateral ST segment elevations | Serial 70% and 99% stenoses of the mid LAD | VSR | 30% | Percutaneous closure of VSR but care was withdrawn by family | Died |
| Qureshi et al 16 | August 2020 | 53/Male | Worsening chest pain, shortness of breath, and diaphoresis | 5 days | Sinus tachycardia, with ST segment elevations in the inferior leads and reciprocal depressions in the lateral leads | A 100% proximal RCA occlusion with left to right collaterals | VSR | 35% | Surgical repair of VSR | Died |
| Qureshi et al 16 | August 2020 | 72/Female | Shortness of breath and chest pain | 7 days | A pulseless electrical activity arrest requiring several rounds of CPR before achieving return of spontaneous circulation | A severely stenotic LAD artery with evidence of thrombus | VSR | 35% to 40% | Stenting, percutaneous closure of the VSR | Died |
| Rimac et al 17 | August 2020 | 64/Female | Dyspnea and recurrent pleuritic chest pain | 30 days | Inferior T-wave inversion | A huge mass adjacent to the left ventricle, a severe culprit lesion within the RCA | A ruptured posterolateral myocardial wall with a giant pseudoaneurysm (90 × 80 mm) communicating through a 35-mm neck | — | Pseudoaneurysm + repair of the posterolateral myocardial wall with a pericardial patch + CABG | Recovered |
| Shah et al 11 | August 2020 | 75/Female | Chest discomfort | 7 days | Inferolateral STE Inferior Q waves Broad R waves V1-V2 |
Tortuous 100% mid-RCA occlusion with TIMI flow grade 0 80% distal left main 80% proximal LAD |
Post-MI VSD Basal inferolateral wall pseudoaneurysm IABP |
50% to 55% | PCI with an IABP | The patient was sent for urgent CABG |
| Parikh et al 18 | October 2020 | 67/Male | Epigastric pressure and dyspnea | 5 days | Inferior Q waves | An occluded RCA | VSR | — | Venoarterial ECMO | Died |
| Parikh et al 18 | October 2020 | 60/Female | Dyspnea, chest pain, and vomiting | 7-14 days | Anterior Q waves | LAD occlusion | VSR | — | Percutaneous VSR closure followed by surgical repair of apical extension | Recovered |
| Khanal et al 19 | November 2020 | 61/Male | Symptoms of CHF | 30 days | Sinus tachycardia, right axis deviation, ST elevation in lead III, T inversion in lead II, III, aVF, and V1 to V4 | A proximal 80% occlusion of the LCA and mid 90% occlusion of the RCA | LVA + VSR | 40% | CABG + left ventriculoplasty + VSR repair | Recovered |
| Pilato et al 20 | November 2020 | 58/Female | Cardiac surgery | 365 days | ST-elevated ACS | Sudden occlusion of the LAD | Subacute LV free wall rupture | — | Surgical repair | Recovered |
| Tan et al 21 | December 2020 | 65/Male | Exertional angina | 60 days | ST-elevation in the inferolateral leads | 100% occlusion of the mid LCx | LV wall rupture, LVP, and cardiac tamponade | 40% | Surgical repair | Recovered |
| Evans et al 22 | February 2021 | 37/Male | Worsening dyspnea | 7 days | Normal sinus rhythm with poor R-wave progression seen in the precordial leads | A completely occluded LAD just beyond a large diagonal branch and RCA with moderate proximal disease | Transmural infarct + pseudoaneurysm in the LAD + muscular VSD with was Qp:Qs 2:1 | 21% | Transcatheter VSD closure | Recovered |
| Fernandes et al 23 | August 2020 | 55/Female | Worsening heart failure symptoms and recurrent pleuritic chest pain | 2 days | Anterior wall MI | The middle segment occlusion of the LAD | Apical aneurysm with organized thrombus, and a small circumferential pericardial effusion | 25% | Aneurysmectomy | Recovered |
| Bakhshi et al 24 | March 2021 | 56/Male | Exertional angina and shortness of breath | 5 days | Anterolateral STEMI | LHC showed culprit 100% occlusion of the proximal LAD and chronic total occlusion of RCA | VSR with Qp/Qs was 1.3 + LV apical thrombus | 32% | Orthotopic heart transplantation | Recovered |
| Bakhshi et al 24 | March 2021 | 53/Male | Progressive exertional chest pain | 7 days | Anterolateral STEMI | LHC revealed 95% stenosis of the mid-LAD and first diagonal artery | A large apical VSR | 45% | Orthotopic heart transplantation | Recovered |
| Briani et al 25 | March 2021 | 70/Male | Dyspnea, fatigue, and ongoing hypotension | 42 days | Acute anterior MI | Absence of restenosis after prior PCI on proximal LAD | Apical aneurysm and MR | 30% | IABP + Impella 5.0 support + cardiac surgery | Recovered |
| Nasr et al 26 | April 2021 | 67/Male | Chest pain, collapsed | Several days | Inferior STEMI | RCA was opacified in the proximal segment with significant acute thrombosis | LV free wall rupture | Depressed | Cardiac surgery | Died |
| Briosa et al 27 | May 2021 | 69/Female | Crushing chest pain | Several days | Sinus tachycardia with inferior ST-segment elevation | An occluded proximal LCx | A flail posterior mitral valve leaflet due to chordae tendineae rupture with associated severe MR | — | PCI + IABP | Died |
Abbreviations: CABG, coronary artery bypass grafting; CAD, coronary artery disease; CHF, chronic heart failure; COVID-19, coronavirus disease 2019; CPR, cardiopulmonary resuscitation; DES, drug-eluting stent; ECMO, extracorporeal membrane oxygenation; ER, emergency room; IABP, intra-aortic balloon pump; ICU, intensive care unit; LAD, left anterior descending; LCA, left coronary artery; LCx, left circumflex; LHC, left heart catheterization; LV, left ventricular; LVA, left ventricular aneurysm; LVEF, left ventricular ejection fraction; MI, myocardial infarction; MR, mitral regurgitation; PCI, percutaneous coronary intervention; RCA, right coronary artery; STEMI, ST-elevation myocardial infarction; TIMI, thrombolysis in myocardial infarction; VSD; ventricular septal defect; VSR, ventricular septal rupture.
Discussion
Acute STEMI is an established cause of significant mortality worldwide. Early detection followed by urgent management using PCI is effective in achieving optimal clinical outcomes. 28 In recent times, the COVID-19 pandemic has overwhelmed health care systems categorically, often masking the presence of other serious medical emergencies, including cardiac pathologies. 29 As per the data from several European nations, 25% to 40% decreased STEMI admissions were noted amid the pandemic.3,30,31 A similar trend has also been noted in the United States.32-34 An international study performed by the European Society of Cardiology demonstrated a significant reduction of >40% in the gross number of STEMI admissions. 35 Furthermore, a study from Hong Kong revealed an increase in the total time elapsed before the presentation of STEMI from 82.5 to 318 minutes due to excessive wariness surrounding the pandemic. 36 Imperatively, a dilatory presentation of MI may result in grave mechanical complications that were once considered extremely rare. 37 The present patient had no other deterrents to seeking medical attention, except for his fear of contracting COVID-19 from the hospital.
LVA is an established complication in patients with massive MI who have a delayed presentation. Currently, the incidence of this complication has been significantly decreased. As per the analysis of the National Inpatient Sample from 2000 to 2017, LVA complicated 0.2% of 11 622 528 admissions for acute MI. 38 It may pose a diagnostic challenge, particularly in its differentiation from a pseudoaneurysm. 39 Multimodality cardiac imaging is frequently required for accurate detection, which also helps in selection of the appropriate treatment. 38 After a significantly delayed presentation due to COVID-19, this patient’s workup also included cardiac magnetic resonance imaging that not only confirmed the LVA but also helped in the assessment of the myocardial viability. In patients with small-to-moderate size asymptomatic LVAs, medical therapy can be considered with an estimated 5-year survival of up to 90%. 40 The medical therapy should target afterload reduction using an angiotensin-converting enzyme inhibitor and anticoagulation in cases with a thrombus within the aneurysmal sac or left ventricle or if there is a remarkable left ventricular dysfunction. Surgical intervention such as aneurysmectomy in conjunction with CABG, as in this case, can be performed in LVA patients with ventricular arrhythmic and/or pump function failure refractory to medical and minimally invasive treatments. 41
VSR is also a serious post-MI complication, with a mortality rate bordering 50%. It has become exceedingly rare in the current era of PCI, with an incidence ranging from 0.17% to 0.31% following STEMI.42,43 This patient had a Becker type III VSR, which is predominantly caused by late presentation of acute MI and is not commonly attributed to reperfusion damage. This type of VSR lesions frequently occurs in the subacute phase, 3 to 5 days following acute MI. 43 In this patient, the exact timing of the VSR lesion could not be ascertained due to his significantly delayed initial presentation. Most of these lesions, as evidenced by the present case, occur after RCA infarction. VSRs are an established cause of left-to-right shunting, leading to pressure and volume overload in the right ventricle. Transthoracic echocardiography plays a vital role in detection, measurement of dimensions, and impact of the VSR as well as exclusion of probable etiologies. Furthermore, left ventriculography can aid in confirming the presence of VSR in cases with unexplained hemodynamic instability while undergoing primary PCI. On pulmonary artery catheterization, the Qp/Qs can be calculated using right ventricular step-up oxygen saturation. 43 In terms of management, surgical patch repair is the treatment of choice. 43 This patient showed excellent recovery after surgical intervention.
The present case is rare and unique in multiple ways. It has several pertinent clinical implications. First, aneurysms in the inferoposterior wall are uncommon. Second, VSR after MI rarely occurs in the inferior and basal portion of the interventricular septum. Third, the concurrent presence of a true LVA and VSR is an extremely rare clinicopathologic entity that can be particularly serious. Fourth, our patient presented a rare case of post-MI mechanical complications with chronic heart failure symptoms such as worsening shortness of breath and lower extremity edema. Fifth, this case demonstrates the clinical effectiveness of CABG, removal of mural thrombus, aneurysmectomy, and VSR patch repair for a favorable outcome despite late presentation. Sixth, it highlights the fear of patients to contract COVID-19 from hospitals that has led to reduction in hospitalization rates due to MI, resulting in re-emergence of life-threatening mechanical complications.
As indicated by the results of the literature review, severe post-MI mechanical complications are being reported across the globe now. With regard to the public awareness of these mechanical complications, several international organizations, such as the American Heart Association, the European Society of Cardiology, and a number of independent clinicians, have written opinion pieces in print media.44-47 Similarly, individual patient experiences regarding contracting severe mechanical complications after acute MI continue to be broadcasted.48,49 Due to the ongoing situation, it is exceedingly important to start mass information campaigns.50-53 All possible barriers in making first medical contact in MI patients need to be eradicated with comprehensive and urgent programs. The use of telemedicine has now proved to be effective in order to improve the MI prognosis and clinical outcomes during the ongoing COVID-19 pandemic. 42 Telemedicine should also be further studied in relation to the re-emergence of severe mechanical complications of MI that are missed due to delayed initial presentation. Eventually, innovative programs should be immediately launched for prompt detection of MI and to possibly circumvent serious mechanical complications amid the commotion elicited by the COVID-19 pandemic.
Learning Objectives
While acute MI presentations have considerably decreased during COVID-19 pandemic, delayed PCI presents a therapeutic dilemma after re-emergence of anachronistic post-MI complications. Clinicians should remain cognizant of rare mechanical complications, including simultaneous LVA and VSR in patients with delayed presentation of acute MI in order to institute prompt and appropriate treatment.
The COVID-19 pandemic and patients avoiding hospitals are causing detrimental effects in late presentation of acute MI, and leading to the resurging of catastrophic mechanical complications.
It is imperative to start educating the community about the formidable clinical value of making the first contact early in individuals with any concerning symptoms and signs despite the fear of acquiring COVID-19.
Footnotes
Author Contributions: All authors contributed equally to the conception and design of the work; the acquisition, analysis, and interpretation of data for the work; and drafting the work or revising it critically for important intellectual content. All authors read and approved the final manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics Approval: Our institution does not require ethical approval for reporting individual cases or case series.
Informed Consent: Verbal informed consent was obtained from the patient for their anonymized information to be published in this article.
ORCID iD: Muhammad Ali Niaz  https://orcid.org/0000-0002-9795-2707
https://orcid.org/0000-0002-9795-2707
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Daniels MJ, Cohen MG, Bavry AA, Kumbhani DJ. Reperfusion of STEMI in the COVID-19 era—business as usual? Circulation. 2020;141:1948-1950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871-2872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rodríguez-Leor O, Alvarez-Álvarez B, Ojeda S, et al. Impacto de la pandemia de COVID-19 sobre la actividad asistencial en cardiología intervencionista en España [in Spanish]. REC Interv Cardiol. 2020;2:82-89. [Google Scholar]
- 4. De Filippo O, D’Ascenzo F, Angelini F, et al. Reduced rate of hospital admissions for ACS during covid-19 outbreak in Northern Italy. N Engl J Med. 2020;383:88-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lin TW, Tsai MT, Wu HY, Roan JN, Luo CY. Mechanical complications of acute myocardial infarction during the COVID-19 pandemic. Acta Cardiol Sin. 2021;37:114-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bryndza MA, Litwinowicz R, Bartuś S, et al. Incidence of mechanical complications following myocardial infarction during the first two months of the COVID-19 pandemic in the Southern Poland region: a multicenter study. Kardiol Pol. 2021;79:66-68. [DOI] [PubMed] [Google Scholar]
- 7. Gaballa S, AlJaf A, Patel K, Lindsay J, Hlaing KM. COVID-19 fears may be worse than the virus: a case of cardiogenic shock secondary to post-myocardial infarction ventricular septum rupture. Cureus. 2020;12:e8809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Masroor S. Collateral damage of COVID-19 pandemic: delayed medical care. J Card Surg. 2020;35:1345-1347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Atreya AR, Kawamoto K, Yelavarthy P, et al. Acute myocardial infarction and papillary muscle rupture in the COVID-19 era. JACC Case Rep. 2020;2:1637-1641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Albiero R, Seresini G. Subacute left ventricular free wall rupture after delayed STEMI presentation during the COVID-19 pandemic. JACC Case Rep. 2020;2:1603-1609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Shah K, Tang D, Ibrahim F, et al. Surge in delayed myocardial infarction presentations: an inadvertent consequence of social distancing during the COVID-19 pandemic. JACC Case Rep. 2020;2:1642-1647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ahmed T, Lodhi SH, Kapadia S, Shah GV. Community and healthcare system-related factors feeding the phenomenon of evading medical attention for time-dependent emergencies during COVID-19 crisis. BMJ Case Rep. 2020;13:e237817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ahmed T, Nautiyal A, Kapadia S, Nissen SE. Delayed presentation of STEMI complicated by ventricular septal rupture in the era of COVID-19 pandemic. JACC Case Rep. 2020;2:1599-1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Joshi S, Kazmi FN, Sadiq I, Azemi T. Post-MI ventricular septal defect during the COVID-19 pandemic. JACC Case Rep. 2020;2:1628-1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Alsidawi S, Campbell A, Tamene A, Garcia S. Ventricular septal rupture complicating delayed acute myocardial infarction presentation during the COVID-19 pandemic. JACC Case Rep. 2020;2:1595-1598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Qureshi WT, Al-Drugh S, Ogunsua A, et al. Post myocardial infarction complications during theCOVID-19 pandemic—a case series. Cardiovasc Revasc Med. Published online August 10, 2020. doi: 10.1016/j.carrev.2020.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rimac G, Marzouk M, Dumont É, Paradis JM. When a delayed cardiology consultation leads to a massive left ventricle pseudoaneurysm: collateral effects of the COVID-19 pandemic. Eur Heart J. 2020;41:3102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Parikh M, Busman M, Dickinson M, Wohns D, Madder RD. Ventricular septal rupture in 2 patients presenting late after myocardial infarction during the COVID-19 pandemic. JACC Case Rep. 2020;2:2013-2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Khanal S, Ghosh S, Mishra AK. A case report of a double catastrophe: true left ventricular aneurysm and ventricular septal rupture complicating acute myocardial infarction and presenting as chronic heart failure. Cureus. 2020;12:e11292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Pilato E, Pinna GB, Parisi V, Manzo R, Comentale G. Mechanical complications of myocardial infarction during COVID-19 pandemic: an Italian single-centre experience. Heart Lung. 2020;49:779-782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tan JH, Tong J, Ho HH. Delayed presentation of acute coronary syndrome with mechanical complication during COVID-19 pandemic: a case report. Eur Heart J Case Rep. 2020;5:ytaa506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Evans MC, Steinberg DH, Rhodes JF, et al. Ventricular septal defect complicating delayed presentation of acute myocardial infarction during COVID-19 lockdown: a case report. Eur Heart J Case Rep. 2021;5:ytab027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Fernandes RM, Mota T, Azevedo P, et al. Giant left ventricular (pseudo?) aneurysm complicating anterior myocardial infarction. J Am Col Cardiol Case Rep. 2021;2:334-338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bakhshi H, Gattani R, Ekanem E, et al. Ventricular septal rupture and cardiogenic shock complicating STEMI during COVID-19 pandemic: an old foe re-emerges. Heart Lung. 2020;50:292-295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Briani M, Torracca L, Crescenzi G, Barbone A. Impella 5.0 support before, during, and after surgical ventriculoplasty following acute myocardial infarction in the COVID-19 era: a case report. Eur Heart J Case Rep. 2021;5:ytab037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nasr GH, Glovaci D, Mikhail A, et al. Left ventricular free wall rupture as a result of delayed presentation of an inferior ST-elevation myocardial infarction due to fear of COVID-19: case report. J Cardiothorac Surg. 2021;16:106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Briosa E, Gala A, Hinton J, Sirohi R. Cardiogenic shock due to acute severe ischemic mitral regurgitation. Am J Emerg Med. 2021;43:292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ibanez B, James S, Agewall S, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39:119-177. [DOI] [PubMed] [Google Scholar]
- 29. Rodriguez-Leor O, Cid-Alvarez B. ST-segment elevation myocardial infarction care during COVID-19: losing sight of the forest for the trees. JACC Case Rep. 2020;2:1625-1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Rangé G, Hakim R, Motreff P. Where have the STEMIs gone during COVID-19 lockdown? Eur Heart J Qual Care Clin Outcomes. 2020;6:223-224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Metzler B, Siostrzonek P, Binder RK, Bauer A, Reinstadler SJ. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J. 2020;41:1852-1853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Braiteh N, Rehman WU, Alom M, et al. Decrease in acute coronary syndrome presentations during the COVID-19 pandemic in upstate New York. Am Heart J. 2020;226:147-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Zitelny E, Newman N, Zhao D. STEMI during the COVID-19 pandemic—an evaluation of incidence. Cardiovasc Pathol. 2020;48:107232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Khot UN, Reimer AP, Brown A, et al. Impact of COVID-19 pandemic on critical care transfers for ST-segment-elevation myocardial infarction, stroke, and aortic emergencies. Circ Cardiovasc Qual Outcomes. 2020;13:e006938. [DOI] [PubMed] [Google Scholar]
- 35. Pessoa-Amorim G, Camm CF, Gajendragadkar P, et al. Admission of patients with STEMI since the outbreak of the COVID-19 pandemic: a survey by the European Society of cardiology. Eur Heart J Qual Care Clin Outcomes. 2020;6: 210-216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Tam CF, Cheung KS, Lam S, et al. Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment-elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13:e006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Trabattoni D, Montorsi P, Merlino L. Late STEMI and NSTEMI patients’ emergency calling in COVID-19 outbreak. Can J Cardiol. 2020;36:1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Vallabhajosyula S, Kanwar S, Aung H, et al. Temporal trends and outcomes of left ventricular aneurysm after acute myocardial infarction. Am J Cardiol. 2020;133:32-38. [DOI] [PubMed] [Google Scholar]
- 39. Inayat F, Ghani AR, Riaz I, et al. Left ventricular pseudoaneurysm: an overview of diagnosis and management. J Investig Med High Impact Case Rep. 2018;6:2324709618792025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Mourdjinis A, Olsen E, Raphael MJ, Mounsey JP. Clinical diagnosis and prognosis of ventricular aneurysm. Br Heart J. 1968;30:497-513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Levine GN, Bates ER, Bittl JA, et al. ACCF/AHA guideline for the management of ST-elevation myocardial infarction. Circulation. 2016;134:e123-e155. doi: 10.1161/CIR.0000000000000404 [DOI] [PubMed] [Google Scholar]
- 42. Swain E. Telehealth strategy improves STEMI care in Latin America, 2020. Accessed June 25, 2021. https://www.healio.com/news/cardiology/20200518/telehealth-strategy-improves-stemi-care-in-latin-america
- 43. Jones BM, Kapadia SR, Smedira NG, et al. Ventricular septal rupture complicating acute myocardial infarction: a contemporary review. Eur Heart J. 2014;35:2060-2068. [DOI] [PubMed] [Google Scholar]
- 44. European Society of Cardiology. Fear of COVID-19 keeping more than half of heart attack patients away from hospitals, 2020. Accessed June 25, 2021. https://www.escardio.org/The-ESC/Press-Office/Press-releases/Fear-of-COVID-19-keeping-more-than-half-of-heart-attack-patients-away-from-hospitals
- 45. CardioSmart. Coronavirus and your heart: don’t ignore heart symptoms. Accessed June 25, 2021. https://www.cardiosmart.org/assets/infographic/covid-19-don’t-ignore-heart-symptoms#:~:text=If%20you%20think%20you%20are,Getting%20care%20quickly%20is%20critical
- 46. Kolata G. Amid the coronavirus crisis, heart and stroke patients go missing, 2020. Accessed June 25, 2021. https://www.nytimes.com/2020/04/25/health/coronavirus-heart-stroke.html
- 47. American Heart Association. Knocking down fears, myths and misinformation about calling 911 in the pandemic. Accessed June 25, 2021. https://www.heart.org/en/coronavirus/coronavirus-covid-19-resources/knocking-down-fears-myths-and-misinformation-about-calling-911-in-the-pandemic
- 48. Wood S. Dire, unusual STEMI complications blamed on COVID-19 hospital avoidance. Accessed June 25, 2021. https://www.tctmd.com/news/dire-unusual-stemi-complications-blamed-covid-19-hospital-avoidance
- 49. Galante A. After man, 38, dies of heart attack, wife shares urgent message: “Go to the ER.” Accessed June 25, 2021. https://www.today.com/health/heart-attack-covid-19-why-young-father-didn-t-go-t184278
- 50. Chieffo A, Stefanini GG, Price S, et al. EAPCI position statement on invasive management of acute coronary syndromes during the COVID-19 pandemic. Eur Heart J. 2020;41:1839-1851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Ashraf S, Ilyas S, Alraies MC. Acute coronary syndrome in the time of the COVID-19 pandemic. Eur Heart J. 2020;41:2089-2091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Cleveland Clinic. Seek care for heart emergencies during COVID-19, 2020. Accessed June 25, 2021. https://newsroom.clevelandclinic.org/2020/04/23/seek-care-for-heart-emergencies-during-covid-19/
- 53. Roffi M, Guagliumi G, Ibanez B. The obstacle course of reperfusion for ST-segment-elevation myocardial infarction in the COVID-19 pandemic. Circulation. 2020;141:1951-1953. [DOI] [PMC free article] [PubMed] [Google Scholar]