Actinic keratoses (AKs) are precancerous lesions that generally result from excessive exposure to ultraviolet light, especially on sun-exposed areas of fair-skinned individuals.1 Early treatment of AKs may prevent progression to invasive squamous cell carcinoma (SCC).2 Classical treatments include cryotherapy, imiquimod, diclofenac, fluorouracil, ingenol mebutate, and photodynamic therapy.3 Tirbanibulin 1% ointment is a synthetic antiproliferative agent that binds tubulin, inhibits tubulin polymerization, and disrupts Src signaling in rapidly dividing cells. In December 2020, it was approved by the US Food and Drug Administration for treatment of AKs in a contiguous area of 25 cm2 as a once-daily topical treatment for 5 days.4 One hundred percent clearance was observed in 49% of patients by day 57, with statistically significant lesion reduction seen as early as day 8; local skin reactions were mostly mild to moderate.5
Case report
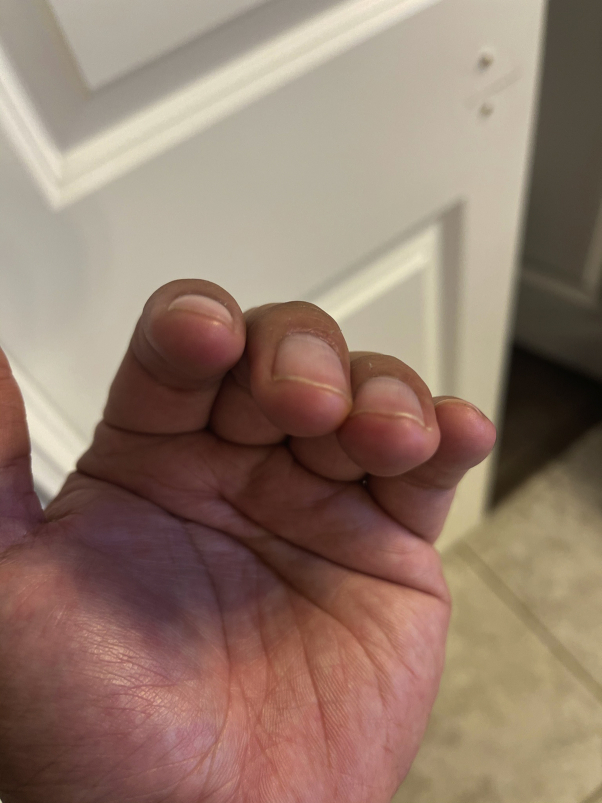
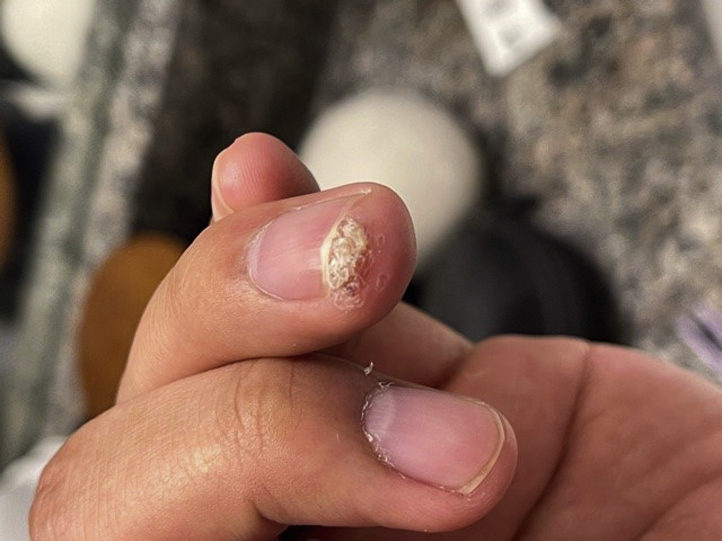
We report the case of a 29-year-old nonsmoking man whose biopsy-confirmed SCC in situ at the distal periungual tip of the left fourth fingernail (Fig 1) had been treated without resolution with imiquimod 5% in combination with monthly liquid nitrogen for 6 months. Before treatment with imiquimod and liquid nitrogen (Fig 1), the asymptomatic periungual verrucous lesion had been biopsied after the lesion had increased in size for >1 year despite liquid nitrogen for a previous clinical diagnosis of a recalcitrant wart. The patient had not previously received the human papilloma virus (HPV) vaccine. Tirbanibulin 1% ointment was applied for 5 days with complete resolution on the fifth day without reported erythema, edema, or irritation. After further extensive questioning, the patient reported mild desquamation at the lesion during the first 1 to 2 days of using the tirbanibulin ointment but no evidence of desquamation by day 5 (Fig 2). Upon follow-up 3 months later, no clinical evidence of recurrence was seen (Fig 3).
Fig 1.
Firm verrucous plaque at the distal periungual tip of the left fourth digit before treatment with tirbanibulin 1% ointment.
Fig 2.

Complete resolution of squamous cell carcinoma after 5 days of topical tirbanibulin 1% ointment.
Fig 3.
No evidence of recurrence of squamous cell carcinoma 3 months after a 5-day course of topical tirbanibulin 1% ointment.
Discussion
We initiated topical tirbanibulin 1% ointment because the patient wanted another nonsurgical option before undergoing surgical excision. In pivotal phase 3 studies, topical tirbanibulin 1% ointment completely cleared 44% and 54%, respectively, of AKs by day 57 in a 25-cm2 contiguous area containing 4 to 8 lesions after once-daily application for 5 consecutive days in 2 identically designed double-blind trials. Similar to the statistically significant lesion reduction seen in some AKs as early as day 8, our patient had significant response on day 5 of topical application of tirbanibulin ointment. Although the most common local reactions to tirbanibulin in the phase 3 trials were transient erythema in 91%, scaling in 82%, application-site pain in 10%, and pruritus in 9%, only mild desquamation of the lesion itself on the first 2 days of application was noted in our patient, and only after extensive follow-up questioning.
In terms of its mechanism of action, tirbanibulin is hypothesized to benefit AK and SCC because of its inhibition of Src, which is known to increase carcinogenesis.6 Tirbanibulin also inhibits tubulin polymerization and exerts potent antiproliferative and proapoptotic effects in immortalized keratinocytes and multiple tumor cell lines.7 In addition, oral tirbanibulin inhibits the growth of human keratinocytes in vitro with an IC50 of 32 nM7 and of solid tumors and leukemia in phase 1 clinical trials and in vivo.8, 9, 10 Because HPV 16 has been detected in periungual SCCs,11 and HPV 16 oncoproteins up-regulate the Src family kinases Src and Yes by posttranscriptional mechanisms,12 we speculated that inhibition of Src by tirbanibulin may specifically target the pathogenesis not only of SCC but also of the HPV trigger. Larger prospective studies of tirbanibulin for the treatment of SCC and warts are recommended.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
IRB approval status: Not applicable.
References
- 1.Salasche S.J. Epidemiology of actinic keratoses and squamous cell carcinoma. J Am Acad Dermatol. 2000;42(1 Pt 2):4–7. doi: 10.1067/mjd.2000.103342. [DOI] [PubMed] [Google Scholar]
- 2.Fernandez Figueras M.T. From actinic keratosis to squamous cell carcinoma: pathophysiology revisited. J Eur Acad Dermatol Venereol. 2017;31(suppl 2):5–7. doi: 10.1111/jdv.14151. [DOI] [PubMed] [Google Scholar]
- 3.Gupta A.K., Paquet M. Network meta-analysis of the outcome 'participant complete clearance' in nonimmunosuppressed participants of eight interventions for actinic keratosis: a follow-up on a Cochrane review. Br J Dermatol. 2013;169(2):250–259. doi: 10.1111/bjd.12343. [DOI] [PubMed] [Google Scholar]
- 4.Blauvelt A., Kempers S., Lain E. Phase 3 trials of tirbanibulin ointment for actinic keratosis. N Engl J Med. 2021;384(6):512–520. doi: 10.1056/NEJMoa2024040. [DOI] [PubMed] [Google Scholar]
- 5.Blauvelt A., Kempers S., Schlesinger T. Tirbanibulin ointment 1% for actinic keratosis (AK): pooled data from two phase 3 studies. SKIN J Cutan Med. 2020;4(6):s121. [Google Scholar]
- 6.Frame M.C. Src in cancer: deregulation and consequences for cell behaviour. Biochem Biophys Acta. 2002;1602(2):114–130. doi: 10.1016/s0304-419x(02)00040-9. [DOI] [PubMed] [Google Scholar]
- 7.Pitzonka L., Cutler M., Bu Y. Tirbanibulin, a novel anti-proliferative and pro-apoptotic agent for the treatment of actinic keratosis. J Invest Dermatol. 2021;141(5):S81. [Google Scholar]
- 8.Smolinski M.P., Bu Y., Clements J. Discovery of novel dual mechanism of action Src signaling and tubulin polymerization inhibitors (KX2-391 and KX2-361) J Med Chem. 2018;61(11):4704–4719. doi: 10.1021/acs.jmedchem.8b00164. [DOI] [PubMed] [Google Scholar]
- 9.Akar A., Bulent Tastan H., Erbil H., Arca E., Kurumlu Z., Gur A.R. Efficacy and safety assessment of 0.5% and 1% colchicine cream in the treatment of actinic keratoses. J Dermatol Treat. 2001;12:199–203. doi: 10.1080/09546630152696314. [DOI] [PubMed] [Google Scholar]
- 10.Naing A., Cohen R., Dy G.K. A phase I trial of KX2−391, a novel non-ATP competitive substrate pocket-directed SRC inhibitor, in patients with advanced malignancies. Investig New Drugs. 2013;31(4):967–973. doi: 10.1007/s10637-013-9929-8. [DOI] [PubMed] [Google Scholar]
- 11.Dika E., Venturoli S., Patrizi A. The detection of human papillomavirus–16 in squamous cell carcinoma of the nail unit: a case series. J Am Acad Dermatol. 2017;76(2):354–356. doi: 10.1016/j.jaad.2016.08.063. [DOI] [PubMed] [Google Scholar]
- 12.Szalmás A., Gyöngyösi E., Ferenczi A. Activation of Src, Fyn and Yes non-receptor tyrosine kinases in keratinocytes expressing human papillomavirus (HPV) type 16 E7 oncoprotein. Virol J. 2013;10(1):79. doi: 10.1186/1743-422X-10-79. [DOI] [PMC free article] [PubMed] [Google Scholar]