Introduction
Basosquamous carcinoma (BSC) is a rare, aggressive tumor defined as a subtype of basal cell carcinoma (BCC), characterized by an aggressive subclinical spread with higher rates of recurrence and metastatic potential.1,2 There are no clear guidelines concerning BSC management.1,2 Treatments such as wide local excision, Mohs micrographic surgery, radiotherapy, and palliative chemotherapy have been reported.1,2 The present report describes the complete regression of an extensive and locally destructive BSC involving the nasal septum and sinuses in a patient after a 4-month regimen of intra-arterial (IA) infusion of low-dose cisplatin.3
Case description
A 90-year-old woman was referred to our clinic for IA infusion chemotherapy after a biopsy-proven unresectable BSC over the center of her face. She presented with an extensive mass with the destruction of the entire nose, which had been slowly progressive over 15 years (Fig 1, A). She did not seek treatment until her vision was significantly obstructed.
Fig 1.
A, Before treatment. B, After 4 months of treatment, the tumor had regressed dramatically and completely.
On admission, a physical examination revealed a fungating, ulcerative tumor (6 × 5 cm) with an elevated, irregular border over the central face. A computed tomography scan of the head area revealed a soft tissue mass at the nasal fossa with the destruction of the nasal septum, extending to the left maxillary antrum and ethmoid sinus (Fig 2, A and B). No locoregional lymphadenopathy was detected. Systemic evaluation, including chest X-ray, Gallium scan, and abdominal ultrasound, revealed no evidence of distant metastasis. The patient's past medical history included chronic pulmonary emphysema with exertional dyspnea, hypertension, and anemia.
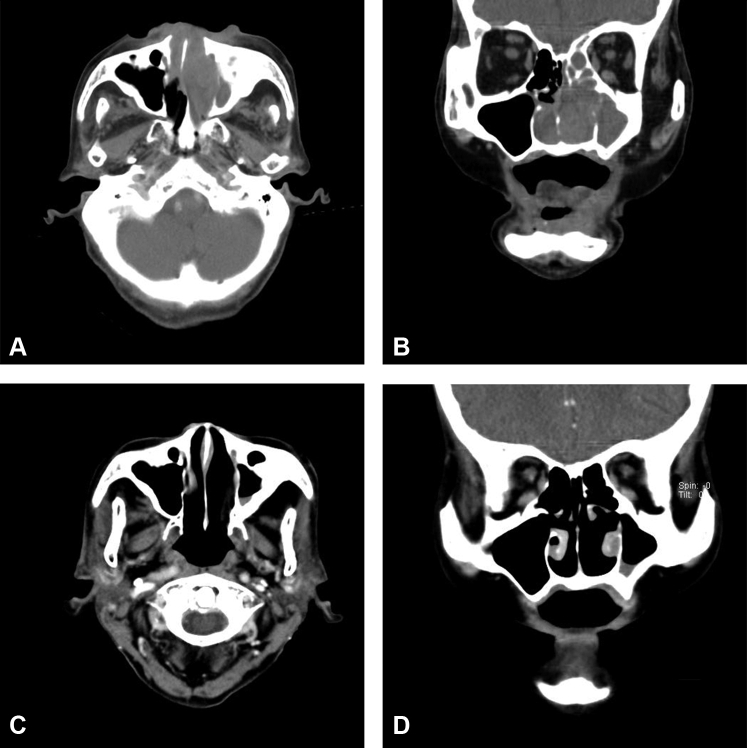
Fig 2.
A and B, Head computed tomography scan before treatment. C and D, Head computed tomography scan after treatment revealed no lesion with abnormal density.
After consideration of the risks and benefits as well as alternatives, including systemic chemotherapy and radiation therapy, the patient elected to undergo IA infusion chemotherapy. The implantable port-catheter system (Jet Port Plus Allround, PFM) was used for catheterization. The catheter with an inner diameter of 0.60 mm and an outer diameter of 1.05 mm was inserted through the right superficial temporal artery and moved in a retrograde manner into the external carotid artery. The tip of the catheter was placed proximally to the branching of the facial artery.3 Proper placement of the catheter was confirmed by Patent Blue V (Guerbet) injection through the catheter. After the catheter was properly placed and fixed, the distal end was embedded subcutaneously along the lateral neck and connected to the port, which was subcutaneously implanted near the infraclavicular region.4, 5, 6 The same procedure was also applied to the left side. The infusion therapy was performed using cisplatin (10 mg per side of the external carotid artery) every week at our patient clinic. After 4 months of weekly infusions of a total dose of 400 mg, the tumor dramatically regressed (Figs 1, B and 2, C and D). During the treatment course, side effects such as anorexia and malaise were reported, and these were mild and tolerable. No catheter-related complications were noted.
Discussion
BSC is an uncommon nonmelanoma skin cancer that shares the characteristics of BCC and squamous cell carcinoma.7 The reported incidence of BSC in skin cancers ranges from 1.2% to 2.7%.1 The majority of lesions arise on the head and neck (80%), with the central part of the face and perinasal area being the most common locations.1 In some cases, patients present with an extensive ulcerating tumor of long-standing duration.2
Compared with BCC and squamous cell carcinoma, BSC is an aggressive neoplasm with a higher risk of recurrence and metastases.1,2 The surgical risk of incomplete excision in BSC appears to be similar to that of BCC, depending on the site, size, and whether primitive or recurrent.1,2 Published recurrent rates were 12% to 51% for surgical excision and 4% for Mohs micrographic surgery.1,2 The incidence of metastasis was at least 5%.2 Long-term follow-up for the detection of local recurrence and distant metastasis is recommended.1,2
Complete surgical excision is the treatment of choice.1 For larger lesions involving the nose, surgery becomes more complex and may require extensive resection with a skin graft or flap reconstruction.1,2 Our patient was frail and elderly and not suitable for surgical intervention. A noninvasive method of treatment was preferable. However, little data are available concerning the appropriate management of unresectable BSC. Vismodegib is an alternative treatment option for BSC of the face in cases wherein surgery is contraindicated; however, determining the precise effects of this drug on BSC requires further investigation.7 Because vismodegib is not reimbursed by our national health system, it was not used in this patient. In addition, because one of the manifestations of radiation toxicity is decreased visual acuity among patients who are irradiated on the head region, radiation therapy was not performed in this patient.8 Cisplatin-based chemotherapy has been reported to produce long-term remissions following treatment of advanced BCC.9 However, cisplatin is a well-known chemotherapeutic agent with nephrotoxic potential.10 Crucial factors that contribute to renal complications include the cancer stage and other risk factors for acute kidney injury, such as age and comorbidities.10 IA infusion chemotherapy has the potential to be used as an efficacious and tolerable treatment modality compared with systemic chemotherapy because of higher local drug concentrations and reduced systemic concentrations.6 IA infusion chemotherapy via the superficial temporal artery is technically feasible and safe and rarely leads to cerebrovascular accidents.3, 4, 5, 6 However, catheter-related complications, such as obstruction of the vessel infection and displacement of the catheter, sometimes occur.3 The side effects associated with the infusion chemotherapy are mild and tolerable.4, 5, 6 Although a 4-month period of disease-free survival cannot be considered to represent a long-term cure, it is noteworthy that the patient was in sustained complete remission for 4 months to the date of death from unrelated illness causes.
IA infusion chemotherapy represents a potential option for older patients with comorbidities who may be ineligible for radical surgery, radiotherapy, or systemic chemotherapy.4,6 Our patient was treated with an IA infusion of low-dose cisplatin, which resulted in excellent tumor response, a good cosmetic result, the preservation of function, and minimal side effects. The findings in this report encourage the performance of further prospective clinical trials.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
IRB approval status: Not applicable.
References
- 1.Garcia C., Poletti E., Crowson A.N. Basosquamous carcinoma. J Am Acad Dermatol. 2009;60(1):137–143. doi: 10.1016/j.jaad.2008.09.036. [DOI] [PubMed] [Google Scholar]
- 2.Shukla S., Khachemoune A. Reappraising basosquamous carcinoma: a summary of histologic features, diagnosis, and treatment. Arch Dermatol Res. 2020;312(9):605–609. doi: 10.1007/s00403-020-02058-1. [DOI] [PubMed] [Google Scholar]
- 3.Homma A., Onimaru R., Matsuura K., Robbins K.T., Fujii M. Intra-arterial chemoradiotherapy for head and neck cancer. Jpn J Clin Oncol. 2016;46(1):4–12. doi: 10.1093/jjco/hyv151. [DOI] [PubMed] [Google Scholar]
- 4.Chen Y.Y., Sheen Y.T., Lin C.P., Sheen M.C. Facial adenocarcinoma treated with intra-arterial chemotherapy. J Am Acad Dermatol. 2015;72(1):e31–e32. doi: 10.1016/j.jaad.2014.09.013. [DOI] [PubMed] [Google Scholar]
- 5.Sheen Y.T., Chen Y.Y., Sheen M.C. Case report of a huge lower lip cancer successfully treated with intra-arterial infusion chemotherapy. Int J Surg Case Rep. 2020;71:82–84. doi: 10.1016/j.ijscr.2020.04.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu C.F., Huang C.J., Chang K.P., Chen C.M. Continuous intra-arterial infusion chemotherapy as a palliative treatment for oral squamous cell carcinoma in octogenarian or older patients. Oral Oncol. 2010;46(7):559–563. doi: 10.1016/j.oraloncology.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 7.Sahuquillo-Torralba A., Llavador-Ros M., Caballero-Daroqui J., Botella-Estrada R. Complete response of a locally advanced basosquamous carcinoma with vismodegib treatment. Indian J Dermatol Venereol Leprol. 2019;85(5):549–552. doi: 10.4103/ijdvl.IJDVL_647_18. [DOI] [PubMed] [Google Scholar]
- 8.Nuzzi R., Trossarello M., Bartoncini S. Ocular complications after radiation therapy: an observational study. Clin Ophthalmol. 2020;14:3153–3166. doi: 10.2147/OPTH.S263291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guthrie T.H., Porubsky E.S., Luxenberg M.N., Shah K.J., Wurtz K.L., Watson P.R. Cisplatin-based chemotherapy in advanced basal and squamous cell carcinomas of the skin: results in 28 patients including 13 patients receiving multimodality therapy. J Clin Oncol. 1990;8(2):342–346. doi: 10.1200/JCO.1990.8.2.342. [DOI] [PubMed] [Google Scholar]
- 10.Jagieła J., Bartnicki P., Rysz J. Nephrotoxicity as a complication of chemotherapy and immunotherapy in the treatment of colorectal cancer, melanoma and non-small cell lung cancer. Int J Mol Sci. 2021;22(9):4618. doi: 10.3390/ijms22094618. [DOI] [PMC free article] [PubMed] [Google Scholar]