Abstract
Latino people in the US are experiencing higher excess deaths during the COVID-19 pandemic than any other racial/ethnic group, but it is unclear which sociodemographic subgroups within this diverse population are most affected. Such information is necessary to target policies that prevent further excess mortality and reduce inequities. Using death certificate data for January 1, 2016 through February 29, 2020 and time-series models, we estimated the expected weekly deaths among Latino people in California from March 1 through October 3, 2020. We quantified excess mortality as observed minus expected deaths and risk ratios (RR) as the ratio of observed to expected deaths. We considered subgroups categorized by age, sex, nativity, country of birth, educational attainment, occupation, and combinations of these factors. Our results indicate that during the first seven months of the pandemic, Latino deaths in California exceeded expected deaths by 10,316, a 31% increase. Excess death rates were greatest for individuals born in Mexico (RR 1.44; 95% PI, 1.41, 1.48) or a Central American country (RR 1.49; 95% PI, 1.37, 1.64), with less than a high school degree (RR 1.41; 95% PI, 1.35, 1.46), or in food-and-agriculture (RR 1.60; 95% PI, 1.48, 1.74) or manufacturing occupations (RR 1.59; 95% PI, 1.50, 1.69). Immigrant disadvantages in excess death were magnified among working-age Latinos in essential occupations. In sum, the COVID-19 pandemic has disproportionately impacted mortality among Latino immigrants, especially those in unprotected essential jobs. Interventions to reduce these inequities should include targeted vaccination, workplace safety enforcement, and expanded access to medical care and economic support.
Keywords: COVID-19, Excess mortality, Structural inequality, Health disparities
Highlights
-
•
During the first seven months of the pandemic, Latino deaths in California exceeded expected deaths by 10316, a 31% increase.
-
•
Relative increases in mortality were greatest for Latinos born in Mexico or Central America, Latinos with less than a high school degree, and Latinos in food-and-agriculture or manufacturing occupations.
-
•
Immigrants in essential occupations had the highest relative increase in death during the pandemic among working-age Latinos.
-
•
Workplace exposure may be key contributor to the disproportionately high COVID-19 mortality experienced by Latinos in CA.
1. Introduction
Throughout the coronavirus disease 2019 (COVID-19) pandemic, Latino people in the US have been dying at disproportionately high rates. National all-cause mortality increased 53.6% for Latinos from the start of the pandemic through October – more than any other group and over four times more than the percent increase for non-Latino Whites (Rossen, 2020). However, aggregate national and state-level statistics obscure the vast diversity among Latinos in the US, making it difficult to intervene effectively to prevent further pandemic mortality (Page & Flores-Miller, 2020). Identifying subgroups at greatest risk for excess death could help guide targeted interventions including workplace protections, testing, vaccination and economic support.
Large variation in structural vulnerability exists among people who identify with the panethnic category Latino/Hispanic (Fenelon et al., 2017; Kauh et al., 2021; Mora, 2014). While race/ethnicity-specific COVID-19 statistics are generally only disaggregated by age, sex, and place, if at all (Frank & Do, 2021), further disaggregation by key social determinants can help clarify the structural drivers of COVID-19 disparities (Alcántara et al., 2021). Nativity, country of birth, occupation, and educational attainment are among the factors that intersect to differentiate the experiences of Latinos in California and we explore these in this study. Nativity and country of birth are important because these factors can determine individual rights and benefits which are consequential for health and they correspond to distinct cultural and political circumstances and racialization experiences (Fenelon et al., 2017; Garcia et al., 2018). Occupation can be conceptualized as a measure of relative power and access to resources and has determined risk of SARS-CoV2 exposure and access to testing and treatment (McClure et al., 2020; Yearby & Mohapatra, 2020). Similarly, educational disadvantage can restrict job opportunities and earning power, sorting people into less protected occupations and limiting the flexible social resources people can marshal to protect their health. Drawing on Crenshaw's intersectionality framework, these factors are best conceptualized as axes of stratification that intersect with racism to structure the positionality of various Latino identities in social hierarchies with consequences for health, and in this case, for mortality during the COVID-19 pandemic (Crenshaw, 1990; Laster Pirtle & Wright, 2021).
California is a critical setting to evaluate the drivers of Latino mortality during the COVID-19 pandemic. California is home to approximately one quarter of the U.S.‘s Latino population and its immigrant population. Latinos are 39% of California's population of 39.5 million residents, but they account for 48% of COVID-19-confirmed deaths through December 2020 (California Department of, 2020a). Even this remarkable death toll likely understates the impact of the pandemic on Latinos because COVID-19-confirmed deaths are understood to be a subset of the total deaths due to COVID-19 (Leon et al., 2020).
The current study estimates the impact of the COVID-19 pandemic on deaths among Latino people in California by estimating excess deaths that occurred between March 1, 2020 and October 3, 2020 compared to the four years prior to the COVID-19 pandemic. By examining death record data, this study overcomes the limitations of official COVID-19 death counts (Krelle et al., 2020). In addition, with the overarching goal of assisting public health efforts globally, we evaluate heterogeneous risk within the Latino population by examining excess death during the pandemic by age, sex, nativity, country of birth, educational attainment, and occupation.
2. Materials and methods
2.1. Data
In order to forecast expected mortality trends during our time-period of interest, we drew on death certificate data from the California Department of Public Health for the period from January 3, 2016 to February 29, 2020 (pre-pandemic period) and from March 1, 2020 to October 3, 2020 (pandemic period). Our analyses included all deaths that occurred within the state of California for which Hispanic/Latino ethnicity was designated. (Only 0.29% of decedents during the pandemic period and 0.25% of decedents during the pre-pandemic period lacked information on ethnicity). Our analytic sample consisted of 43,576 total deaths among Latinos in California during the pandemic period and 220,986 during the pre-pandemic period. There was little missingness for the variables of interest and exclusions due to missingness were done on an available-case basis (0.021% of decedents were missing age, 0.003% were missing sex, 0.829% were missing country of birth, and 2.424% were missing educational attainment). The NIOSH Industry and Occupation Computerized Coding System (NIOCCS) was used to transform free text for occupation and industry from the death certificates into Census occupation codes, which were then grouped into occupational sectors by three independent coders and reconciled. Decedents with insufficient information on occupation or industry were included in all analyses and were grouped in the “unemployed or missing” category for occupational sector (3.31% of the working-age decedents had an unknown or missing occupational sector). Due to delays in complete cause of death data, we did not distinguish specific causes of death for this analysis.
We defined Latinos as any individual identified with Latino/a or Hispanic ethnicity on the death certificate, irrespective of race or country of birth. We do not use the more inclusive, gender-neutral terms Latinx or Latine in this paper because they were not used in death records.
We evaluated subgroups defined by: age at death in years (0–24, 25–54, 55–64, 65–74, 75–84, or 85+); sex (male or female); country of birth (4-categories: U.S., Mexico, a Central American country, or other country); nativity (U.S.-born or foreign-born); occupational sector (see below); educational attainment (4-categories: less than a high school degree, high school degree or GED, some college or Associate's degree, Bachelor's degree or higher; 2-categories: less than a high school degree, or high school or higher.
2.2. Outcome
We defined excess deaths as observed minus expected deaths due to all causes, with expected deaths based on historical trends over the previous four years using time series methods described below. For analyses stratified by educational attainment, following standard practice (Jacobs & Stoner-Eby, 1998), we restricted our analysis to decedents at least 25 years of age so most people would have completed schooling. For analyses stratified by occupational sector, we grouped individuals by the primary occupation over their life, a field included in the death certificate, and restricted analyses to decedents 18–65 years of age. We drew on the California Department of Public Health designations for essential work (California Department of, 2020b) to sort the occupation into one of seven sectors of high-risk or essential work, a category for non-essential, or a category for unemployed or missing data on occupation. Using this designation, we also compared individuals in essential occupational sectors to individuals in non-essential occupational sectors.
2.3. Statistical analyses
For the full population and for each subgroup of interest, we repeated the following procedure using the forecast package in R18 in order to estimate the number of excess deaths and the risk ratio for excess mortality. First, we aggregated the data to weekly death counts, restricting to the subgroup of interest. Next, to estimate expected deaths, we fit dynamic harmonic regression models with autoregressive integrated moving average (ARIMA) (Box et al., 2015) errors for the number of weekly deaths, using deaths occurring pre-pandemic. We iterated through models with up to 25 Fourier terms and selected the model that minimized the corrected Akaike information criterion, following an approach developed by Hyndman and Khandakar (Hyndman & Khandakar, 2008). We inspected the residuals from the preferred model using plots and the Ljung-Box test to confirm that minimal autocorrelation remained. Then, using the preferred model, we forecast the number of weekly deaths and the corresponding 95% prediction intervals (PI) for the pandemic period: March 1, 2020 through October 3, 2020. These forecasts provided the expected weekly deaths during the pandemic period for that subgroup, based on historical trends. To estimate the weekly excess deaths, we subtracted the number of expected deaths from the observed deaths for each week. We constructed a 95% PI for excess deaths by simulating the expected deaths model 10,000 times (varying based on uncertainty in the estimated coefficients for the time-series prediction model), selecting the 2.5 and 97.5 percentiles, and subtracting the total number of observed deaths. Risk ratios were estimated as observed deaths divided by expected deaths, with the pandemic as the exposure, and are also known as observed-to-expected mortality ratios. Risk ratios present the same information as percent excess deaths, as reported in previous studies (McClure et al., 2020; Rossen, 2020; Woolf et al., 2020). Because the estimates of excess deaths presented in Table 1 are generated through subgroup-specific models with varied population sizes and varied restrictions on age, they do not sum to a uniform total for excess deaths. We also calculated per capita excess mortality for each subgroup by dividing excess deaths by the corresponding population size, using estimates from the 2019 American Community Survey. We conducted all analyses in R version 3.6.3.
Table 1.
Cumulative excess deaths during the COVID-19 pandemic among Latinos in California: March through September 2020.
| Excess | Risk ratioa | Per 100,000 | |
|---|---|---|---|
| Entire state 10,316 (9570, 11,030) | 1.31 (1.28, 1.34) | 66 | |
| Age | |||
| 0–24 years old | 184 (−17, 376) | 1.10 (0.99, 1.23) | 3 |
| 25–54 years old | 2346 (1965, 2708) | 1.38 (1.30, 1.46) | 36 |
| 55–64 years old | 1986 (1689, 2271) | 1.40 (1.32, 1.48) | 146 |
| 65–74 years old | 2425 (2018, 2816) | 1.42 (1.33, 1.52) | 325 |
| 75–84 years old | 2110 (1809, 2398) | 1.35 (1.28, 1.41) | 641 |
| 85+ years old | 1978 (1472, 2464) | 1.26 (1.18, 1.35) | 1535 |
| Sex | |||
|
Female |
3745 (3101, 4360) | 1.25 (1.20, 1.31) | 48 |
| Male | 7092 (6214, 7937) | 1.39 (1.33, 1.46) | 90 |
| Country of Birth | |||
| United States | 3004 (2506, 3482) | 1.19 (1.16, 1.23) | 29 |
| Mexico | 5855 (5497, 6199) | 1.44 (1.41, 1.48) | 149 |
| Central America | 1311 (1068, 1543) | 1.49 (1.37, 1.64) | 144 |
| Other | 223 (91, 350) | 1.15 (1.06, 1.27) | 76 |
| Educationb | |||
|
No high school degree and no GED |
5936 (5375, 6471) | 1.41 (1.35, 1.46) | 193 |
| High school degree or GED | 2766 (2233, 3279) | 1.31 (1.23, 1.39) | 114 |
| Some college or associate degree | 1038 (719, 1344) | 1.23 (1.15, 1.32) | 44 |
| Bachelor's degree or beyond | 435 (245, 616) | 1.22 (1.11, 1.34) | 33 |
| Occupational Sectorc | |||
| Facilities | 883 (697, 1063) | 1.38 (1.28, 1.50) | 58 |
| Food and agriculture | 639 (551, 723) | 1.60 (1.48, 1.74) | 61 |
| Government and community | 249 (208, 288) | 1.42 (1.33, 1.53) | 33 |
| Health or emergency | 202 (128, 273) | 1.35 (1.20, 1.54) | 35 |
| Manufacturing | 519 (465, 573) | 1.59 (1.50, 1.69) | 101 |
| Retail | 244 (168, 318) | 1.29 (1.18, 1.41) | 35 |
| Transportation and logistics | 804 (660, 942) | 1.39 (1.30, 1.49) | 85 |
| Not essential | 1119 (921, 1310) | 1.30 (1.23, 1.36) | 55 |
| Unemployed or missing | 167 (96, 236) | 1.40 (1.19, 1.66) | 10 |
Risk ratio is observed/expected for all-cause mortality, comparing the ndemic period (March 1, 2020 to October 3, 2020) to previous years (January 3, 2016 to February 29, 2020).
Among decedents 25 years of age or older.
Among decedents 18–65 years of age.
Sources: California Department of Public Health Death Records; 2019 American Community Survey.
3. Results
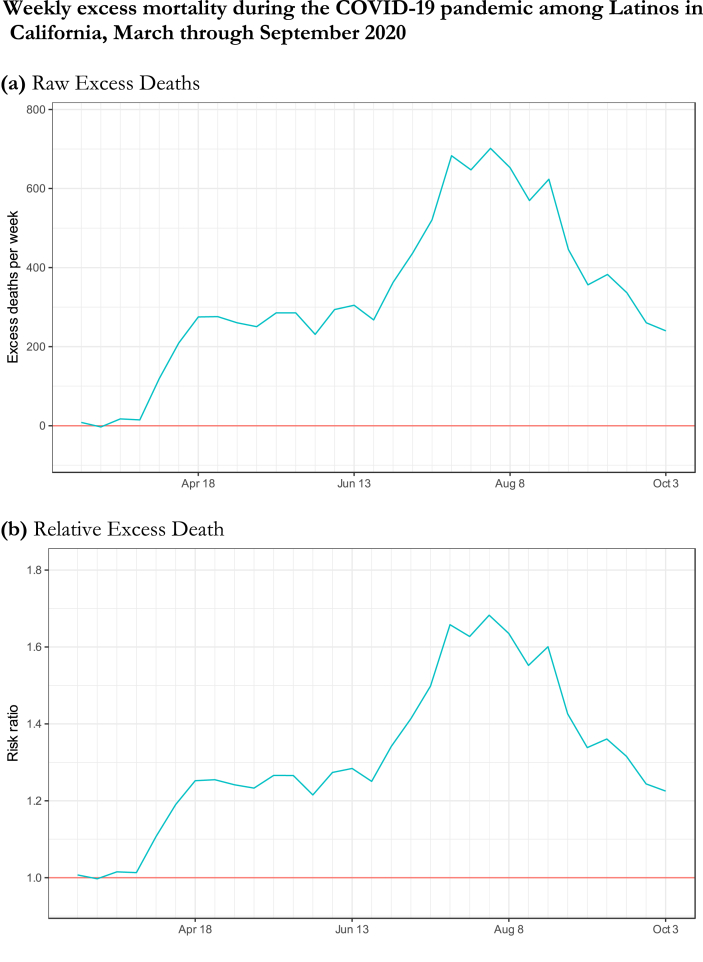
Between March 1 and October 3, 2020, Latino people in California experienced a 31% increase in mortality compared with historical trends, with an estimated 10,316 (95% PI, 9,570, 11,030) excess deaths (Table 1). COVID-19 was listed as a cause of death on 7,672 death certificates (74% of the estimated excess deaths). The number of excess deaths varied by week such that excess mortality was lowest during California's Shelter-in-Place period (March 19, 2020–May 7, 2020), then increased to a peak at the end of July with over 600 excess deaths per week, and began to decline by mid-August (Fig. 3), but the time trends varied by subgroup (Fig. 4). The observed excess death rate for Latinos aged 25 or older implies 1,185 additional deaths per million individuals. Excess deaths in Latinos were observed in all regions in California (Figure S1).
Fig. 3.
Note: Risk ratio is observed/expected for all-cause mortality, comparing the pandemic period (March 1, 2020 to October 3, 2020) to previous years (January 3, 2016 to February 29, 2020); Source: California Department of Public Health Death Records.
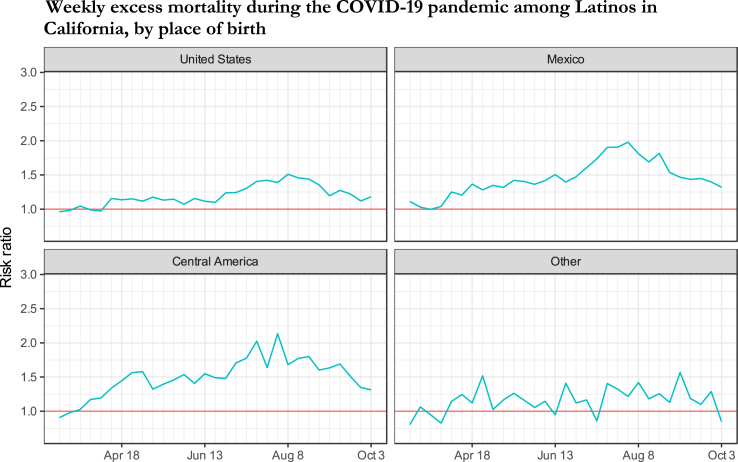
Fig. 4.
Note: Risk ratio (observed/expected) for all-cause mortality, comparing the pandemic period (March 1, 2020 to October 3, 2020) to previous years (January 3, 2016 to February 29, 2020); Source: California Department of Public Health Death Records.
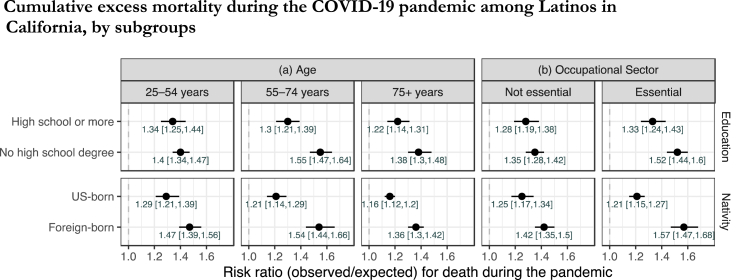
As shown in Table 1, relative increases in mortality ranged from 26 to 42% for all adults 25 and older and was of similar magnitude across adult age groups. Latino males had a greater relative increase in mortality than Latina females (RR 1.39 for males and 1.25 for females). The magnitude of excess mortality varied by nativity, country of birth, and educational attainment. Foreign-born Latinos had higher relative excess mortality than U.S.-born Latinos: deaths were 44% higher than expected among individuals born in Mexico (RR 95% PI, 1.41, 1.48) and 49% higher than expected among individuals born in a Central American country (RR 95% PI, 1.37, 1.64). By contrast, deaths among U.S.-born Latinos were 19% (RR 95% PI, 1.16, 1.23) higher than expected values. In every adult age group, foreign-born Latinos experienced at least double the relative increase in mortality experienced by U.S.-born Latinos (Fig. 1). Comparing sex-by-nativity subgroups revealed that foreign-born males experienced the highest relative increase in mortality during the pandemic (RR 1.55; 95% PI, 1.49, 1.61), followed by foreign-born females (RR 1.37; 95% PI, 1.31, 1.42), then U.S.-born males (RR 1.23, 95% PI, 1.18, 1.28), and finally U.S.-born females (RR 1.17; 95% PI, 1.13, 1.22) (Figure S2). Educational attainment was inversely associated with the magnitude of excess death during the pandemic period. Relative excess mortality was highest among Latinos with less than a high school degree (RR 1.41; 95% PI, 1.35, 1.46) and lowest among Latinos with a Bachelor's degree or higher (RR 1.22; 95% PI, 1.11, 1.34).
Fig. 1.
a: Among decedents 25 years of age at death or older.
b: Among decedents 25–65 years of age at death.
Note: Risk ratio is observed/expected for all-cause mortality, comparing the pandemic period (March 1, 2020 to October 3, 2020) to previous years (January 3, 2016 to February 29, 2020); Source: California Department of Public Health Death Records.
Among working-age adults (age 18–65 years), cumulative excess mortality RRs were highest in those working in food-and-agriculture (RR 1.60; 95% PI, 1.48, 1.74) and manufacturing (RR 1.59; 95% PI, 1.50, 1.69) (Table 1). During the summer surge, weekly excess mortality among workers in manufacturing was over 200 percent of expected values (Fig. 4).
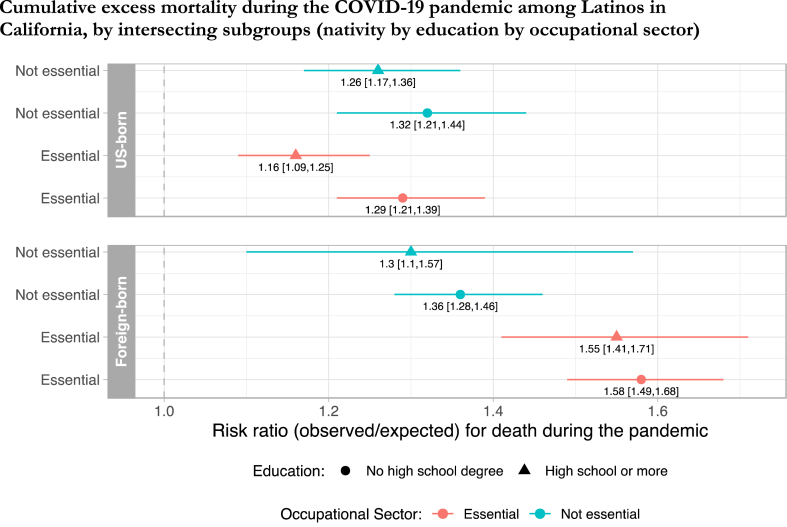
Disadvantages in excess mortality associated with foreign-born status and low educational attainment were more pronounced among Latinos in essential occupations and in the 55 to 74 age group. Among Latinos who worked in essential sectors, the percent excess in mortality for immigrants (RR 1.57; 95% PI, 1.47, 1.68) was more than double the percent excess for U.S.-born Latinos (RR 1.21; 95% PI, 1.15, 1.27) (Fig. 1). This 36-percent immigrant disadvantage was reduced to 17-percent among Latinos in non-essential occupations. Among Latinos in essential occupational sectors with less than a high school degree, mortality was 52% (95% PI, 44%, 60%) higher than expected, whereas for Latinos in the same occupational sectors with a high school credential or more, mortality was 33% (95% PI, 24%, 43%) higher than expected. Finally, pandemic mortality was 58% (95% PI, 49%, 68%) above expected in the subgroup of working-age Latinos with the combined factors of being foreign-born, with less than a high school degree, and in an essential occupation, but significantly lower in the subgroup of Latinos who were foreign-born and with less than a high school degree, yet not in an essential occupation (RR 1.36; 95% PI, 1.28, 1.48) (Fig. 2).
Fig. 2.
Note: Analysis restricted to decedents 25–65 years of age at death. Risk ratio is observed/expected for all-cause mortality, comparing the pandemic period (March 1, 2020 to October 3, 2020) to previous years (January 3, 2016 to February 29, 2020); Source: California Department of Public Health Death Records.
4. Discussion
Using data on all deaths among Latinos in California, USA from January 1, 2016 through October 3, 2020, we found 10,316 additional deaths occurred among California Latinos in the first 7 months of the pandemic compared with trends in the four years prior. In relative terms, this was an excess of 31 percent. Our findings reveal disparities in excess mortality by Latino subgroups. Foreign-born Latinos, those with less than a high school degree, and those working in essential occupations, in particular food/agriculture and manufacturing, were at markedly higher relative risk of excess death, especially in the presence of more than one of these factors. Employment in an essential occupational sector appeared to magnify existing social vulnerabilities by nativity and educational attainment.
We have previously shown that over the first 5 months of the pandemic, Latinos in California experienced higher relative excess mortality than other racial/ethnic groups, with a per capita excess nearly double that of non-Latino White people in California (Chen et al., 2020). This finding was a stark contrast to the well-established narrative of the “Latino Paradox” – the tendency for Latinos to have lower mortality rates than Non-Hispanic Whites despite lower socioeconomic status (Markides & Eschbach, 2005). Our current study's finding that excess mortality during the pandemic was even higher for particular Latino subgroups underscores the need for updated and nuanced conceptual models to understand mortality experiences among Latinos during the pandemic (Sáenz & Garcia, 2021). Intersectionality theory, especially recent elaborations by Brown (Brown, 2018) and others (Laster Pirtle & Wright, 2021), provides an excellent starting point for conceptualizing how measured factors such as nativity, educational attainment, and occupation, overlap with non-measured factors such as undocumented status, language isolation, and indigeneity to differentiate health experiences for Latinos.
Our current results show that the pandemic's impacts on mortality have been far worse for Latinos born in Mexico and Central American countries than U.S.-born Latinos; a disparity apparent within every age group, but worse among 55 to 74 year-olds. This finding that the nativity disparity in relative excess mortality is widest among 55 to 74 year-olds likely reflects a combination of influence from the age structure of the population and the vulnerability to COVID-19 death faced by older workers. Among foreign-born Latinos, males had worse relative excess mortality than females – this sex disparity was attenuated among U.S.-born Latinos. These are examples of how intersecting marginalized identities may compound risk of COVID-19 death in non-linear ways. Recognizing that gender shapes health inequities within the larger system of structural gendered racism (Laster Pirtle & Wright, 2021), the experiences of Latina women during the pandemic are distinct from the experiences of Latino men and distinct from the experiences of women and men racialized in other ways.
Foreign-born Latinos comprise 37% of California's Latino population, but an estimated 71% of Latino excess deaths during the pandemic period occurred among the foreign-born. The differential impact of nativity on excess mortality during the pandemic is notable given previously documented immigrant health advantages (Riosmena et al., 2017), and it is relevant to recent projections of declines in life expectancy for Latinos in the U.S. due to COVID-19 (Andrasfay & Goldman, 2021). The literature suggests recent Latino immigrants to the U.S. are less likely than their U.S.-born counterparts to have an underlying medical condition that would increase COVID-19 severity (Commodore‐Mensah et al., 2016). However, foreign-born Latinos may be more vulnerable to COVID-19 because of their concentration in high-exposure occupations with limited workplace protections (2019Bureau of Labor Statistics), barriers to health care and other social protections due to legal status and public charge inadmissibility (Page et al., 2020), and chilling effects that deter healthcare-seeking behavior due to fears spurred by anti-immigrant rhetoric and policy (Perreira & Pedroza, 2019).
The elevated mortality and stark disparities observed in essential occupational sectors underscores the potential role of workplace settings and worker marginalization as contributors to excess deaths among Latino people (Garcia et al., 2021; Laster Pirtle, 2020), and as shown in Fig. 2, particularly among immigrants. The risk ratios for excess death among those in health and emergency jobs or government and community jobs – where workplace safety measures are more consistently adopted (Hanage et al., 2020) -- were substantially lower than the risk ratios among those in sectors characterized by low-wage jobs such as manufacturing and agriculture. Notably, the disadvantages by nativity and education in pandemic-associated mortality were both magnified among Latinos in essential occupational sectors (Fig. 1). Subgroup analyses revealed that essential work dramatically increased the risk of excess death among foreign-born Latinos, but not among U.S.-born Latinos (Fig. 2).
Multiple structural inequalities may put foreign-born, less-than-high-school-educated Latinos employed in essential jobs and their family members at greater risk of exposure to SARS-CoV-2 and death from COVID-19. For instance, foreign-born Latinos earn 87% as much as their U.S.-born counterparts (2019Bureau of Labor Statistics). Extreme financial precarity coupled with low levels of unionization make it difficult to negotiate workplace protections and benefits (Patler et al., 2020), leading foreign-born and less-than-high-school-educated Latinos to participate in work settings where they are not protected from exposure. This structural disadvantage intersects with undocumented status and may help explain our finding that excess mortality differs not just by nativity, but by specific country of birth. Approximately 44% of Mexican immigrants in the U.S. (Passel & Cohn, 2020; Batalova & Zong, 2021), and 69% of Guatemalan immigrants in the U.S. are undocumented (Noe-Bustamante et al., 2020). The threat of detention or deportation combined with exclusion from Medicaid and Medicare result in delayed and inadequate medical care for many undocumented Latinos (Patler et al., 2020; Duncan & Horton, 2020). Among Latinos in California, half of undocumented adults and over 20 percent of legal permanent resident adults lacked health insurance prior to the pandemic (Bustamante et al., 2018). In addition to these structural factors, many Latinos for whom Spanish or an indigenous language is their preferred language may lack access to actionable health information about COVID-19 prevention and treatment (Rodriguez-Diaz et al., 2020). Larger households and denser living arrangements likely amplify occupational exposures and contribute to the elevated case and death rates among Latinos (Garcia et al., 2021). Within these intersecting factors are many opportunities for intervention.
The two main strategies for pandemic control endorsed during the study period were individual behavior change (e.g., masking, distancing) and Shelter-in-Place orders to slow transmission. Our results suggest that neither pandemic control strategy has sufficiently protected Latinos from excess mortality. In fact, as our previous study demonstrated and our current study reinforces, California began reopening in May when excess deaths among Latinos had yet to decline and, as we show here, when excess death were rising for vulnerable subgroups. Distinct policies and investment are needed to protect foreign-born Latinos and reduce disparities in COVID-19-related death (Garcia et al., 2020; Gee & Ford, 2011; Márquez, 2012).
Our findings draw attention to four domains of promising policy response to reduce excess pandemic mortality among marginalized groups: workplace conditions, financial supports, healthcare coverage, and vaccine distribution. First, expanded action is needed, particularly in the manufacturing and food & agriculture sectors, to regulate and enforce workplace modifications to protect employees from SARS-CoV-2 exposure, provide workers with accurate information, and protect jobs if workers take leave when sick or negotiate for safer conditions (Michaels & Wagner, 2020). Second, most federal government programs in the U.S. to provide financial relief from the economic consequences of the pandemic, such as the direct payments from the CARES Act, have excluded undocumented individuals and the many Latinos in mixed status families. Including immigrant families in financial relief could enable more workers to refuse to work in unsafe settings, which might interrupt transmission and reduce mortality. Third, an immediate step that could improve access to medical care is extending emergency Medicaid coverage to all individuals with COVID-19 regardless of immigration status (Torres-Pinzon et al., 2020). Finally, as California moves toward complete reopening, it is critical that the vulnerable subgroups highlighted in our study receive extra support to access COVID -19 vaccination. Pandemic disparities are likely to widen in the U.S. and similar contexts unless action is taken to ensure true access to vaccination for marginalized populations, including undocumented immigrants, immigrants with limited English proficiency, low-wage workers, and people without health insurance, who face barriers to COVID-19 vaccination (Hamel et al., 2021).
This study is limited by the accuracy and comprehensiveness of the data on death certificates. The interpretation of excess deaths that did not list COVID-19 as a contributing cause is unclear; these deaths may be undiagnosed COVID-19 cases or they may reflect increased mortality due to other causes exacerbated by the pandemic. The proportion of COVID-confirmed deaths compared with overall excess mortality that we observed (approximately 74%) is similar or slightly higher than in national studies. Our analysis is also limited by the occupation field on death certificates which indicates primary occupation for most of the decedent's lifetime rather than most recent occupation. We did not have data to directly examine a number of plausible contributors to excess mortality among Latinos, for example household size, legal status, language isolation, or health insurance. Nor did we have access to data on indigenous ethnicity, another potentially important subgroup with high vulnerability (Sanchez, 1565). The invisibility or erasure of some populations or identities in surveillance data can lead to erroneous conclusions about the drivers of COVID disparities (Alcantara et al., 2021; Kauh et al., 2021; Small-Rodriguez, 2020). Still, this study's attention to heterogeneity among Latino/Hispanic individuals, as is possible using information available on death certificates, is a critical step toward understanding the full extent of COVID-19's impact on Latinos in the U.S. Finally, our results rest on the time-series model premise, that we can predict mortality rates in 2020 based on trends observed in the prior four years, accounting for factors such as seasonality and autocorrelation.
In summary, our study used data from individual death records to reveal that being foreign-born, having low educational attainment, and working in an essential job was associated with disproportionately high relative excess mortality during the COVID-19 pandemic for Latinos in California, especially when these factors occurred together. Policies enforcing COVID-19 safety in the workplace including paid time-off for testing or vaccination, especially for immigrant workers, policies extending high-quality healthcare to all people, including immigrants, and investment in vaccination campaigns designed to overcome the barriers to vaccination faced by Latinos (Hamel et al., 2021) may have the highest benefit for reducing COVID-19 mortality.
Author contributions
ARR, YC, and ECM had full access to the data and take responsibility for the analysis. Study design: All authors; Data analysis: Led by YC and reviewed by ARR and ECM; Data interpretation: All authors; First draft of manuscript: ARR; Revisions and approval of final draft of manuscript and tables/figures: All authors. Supervision: KBD.
Ethics statement
The study protocol was approved by the Committee for the Protection of Human Subjects (State of California), project number: 2020–109.
A previous version of this manuscript was deposited to the medRxiv preprint server.
Declaration of competing interest
Authors receive grant funding from the National Institutes of Health, but no competing interests are declared.
Acknowledgements
Dr. Riley's work was supported by a training grant from the National Institute on Aging: T32AG049663. Dr. Torres' work was supported by a K01 grant from the National Institute on Aging: AG056602.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2021.100860.
Appendix A. Supplementary data
The following is the supplementary data to this article:
References
- Alcántara C., Suglia S.F., Ibarra I.P., Falzon A.L., McCullough E., Alvi T. Disaggregation of latina/o child and adult health data: A systematic review of public health surveillance surveys in the United States. Population Research and Policy Review. 2021;40(1):61–79. doi: 10.1007/s11113-020-09633-4. [DOI] [Google Scholar]
- Andrasfay T., Goldman N. Reductions in 2020 US life expectancy due to COVID-19 and the disproportionate impact on the Black and Latino populations. Proceedings of the National Academy of Sciences. 2021;118(5) doi: 10.1073/pnas.2014746118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batalova J., Zong J. 2021. Mexican Immigrants in the United States.https://www.migrationpolicy.org/article/mexican-immigrants-united-states-2017 migrationpolicy.org. Published October 5, 2018. Accessed May 27, 2021. [Google Scholar]
- Box G.E.P., Jenkins G.M., Reinsel G.C., Ljung G.M. John Wiley & Sons; 2015. Time series analysis: Forecasting and control. [Google Scholar]
- Brown T.H. Racial stratification, immigration, and health inequality: A life course-intersectional approach. Social Forces. 2018;96(4):1507–1540. doi: 10.1093/sf/soy013. [DOI] [Google Scholar]
- Bureau of Labor Statistics FOREIGN-BORN workers: Labor force CHARACTERISTICS—2019. https://www.bls.gov/news.release/pdf/forbrn.pdf
- Bustamante A.V., McKenna R.M., Viana J., Ortega A.N., Chen J. Access-to-care differences between Mexican-heritage and other Latinos in California after the affordable care Act. Health Affairs. 2018;37(9):1400–1408. doi: 10.1377/hlthaff.2018.0416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- California Department of Public Health All cases and deaths associated with COVID-19 by race and ethnicity. https://www.cdph.ca.gov/Programs/CID/DCDC/Pages/COVID-19/Race-Ethnicity.aspx
- California Department of Public Health Essential critical infrastructure workers list. https://files.covid19.ca.gov/pdf/EssentialCriticalInfrastructureWorkers.pdf
- Commodore‐Mensah Y., Nwakaego U., Olawunmi O., Aboagye J., Agyemang C., Reilly M.…Okosun S. Length of residence in the United States is associated with a higher prevalence of cardiometabolic risk factors in immigrants: A contemporary analysis of the national health interview Survey. Journal of the American Heart Association. 2016;5(11) doi: 10.1161/JAHA.116.004059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crenshaw K. Mapping the margins: Intersectionality, identity politics, and violence against women of color. Stanford Literature Review. 1990;43:1241. [Google Scholar]
- Chen Y.-H., Glymour M.M., Catalano R., Fernandez A., Nguyen, T., Kushel, M., et al. (2020) Excess mortality in California during the coronavirus disease pandemic, March to August 2020. JAMA internal medicine. Published online (in press). [DOI] [PMC free article] [PubMed]
- Duncan WL, Horton SB. Serious challenges and potential solutions for immigrant health during COVID-19. Health affairs blog. Published online April 18, 2020. doi:10.1377/hblog20200416.887086.
- Fenelon A., Chinn J.J., Anderson R.N. A comprehensive analysis of the mortality experience of hispanic subgroups in the United States: Variation by age, country of origin, and nativity. SSM - Population Health. 2017;3:245–254. doi: 10.1016/j.ssmph.2017.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank R., Do D. Using race- and age-specific COVID-19 case data to investigate the determinants of the excess COVID-19 mortality burden among Hispanic Americans. Demographic Research. 2021;44(29):699–718. [Google Scholar]
- Garcia M.A., Garcia C., Chiu C.-T., Raji M., Markides K.S. A comprehensive analysis of morbidity life expectancies among older hispanic subgroups in the United States: Variation by nativity and country of origin. Innovation in Aging. 2018;2(igy014) doi: 10.1093/geroni/igy014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia M.A., Homan P.A., García C., Brown T.H. The color of COVID-19: Structural racism and the disproportionate impact of the pandemic on older black and Latinx adults. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2021 doi: 10.1093/geronb/gbaa114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia M.A., Reyes A.M., García C., Chiu C.-T., Macias G. Nativity and country of origin variations in life expectancy with functional limitations among older hispanics in the United States. Research on Aging. 2020 doi: 10.1177/0164027520914512. [DOI] [PubMed] [Google Scholar]
- Gee G.C., Ford C.L. Structural racism and health inequities. Du Bois Review. 2011;8(1):115–132. doi: 10.1017/S1742058X11000130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamel L., Artiga S., Safarpour A., Stokes M., Brodie M. KFF COVID-19 vaccine monitor: COVID-19 vaccine access, information, and experiences among hispanic adults in the U.S. Kaiser family foundation. https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-access-information-experiences-hispanic-adults/ Published May 13, 2021. Accessed.
- Hanage W.P., Testa C., Chen J.T., Davis L., Pechter E., Seminario P.…Krieger N. COVID-19: US federal accountability for entry, spread, and inequities—lessons for the future. European Journal of Epidemiology. 2020;35(11):995–1006. doi: 10.1007/s10654-020-00689-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyndman R.J., Khandakar Y. Automatic time series forecasting: The forecast Package for R. Journal of Statistical Software. 2008;27(3):1–22. [Google Scholar]
- Jacobs J.A., Stoner-Eby S. Adult enrollment and educational attainment. The Annals of the American Academy of Political and Social Science. 1998;559(1):91–108. doi: 10.1177/0002716298559001008. [DOI] [Google Scholar]
- Kauh T.J., Read J.G., Scheitler A.J. The critical role of racial/ethnic data disaggregation for health equity. Population Research and Policy Review. 2021;40(1):1–7. doi: 10.1007/s11113-020-09631-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krelle H., Barclay C., Tallack C. Understanding excess mortality: What is the fairest way to compare COVID-19 deaths internationally? The health foundation. https://www.health.org.uk/news-and-comment/charts-and-infographics/understanding-excess-mortality-the-fairest-way-to-make-international-comparisons Published May 6, 2020. Accessed.
- Laster Pirtle W.N. Racial capitalism: A fundamental cause of novel coronavirus (COVID-19) pandemic inequities in the United States. Health Education & Behavior. 2020 doi: 10.1177/1090198120922942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laster Pirtle W.N., Wright T. Structural gendered racism revealed in pandemic times: Intersectional approaches to understanding race and gender health inequities in COVID-19. Gender & Society. 2021;35(2):168–179. doi: 10.1177/08912432211001302. [DOI] [Google Scholar]
- Leon D.A., Shkolnikov V.M., Smeeth L., Magnus P., Pechholdová M., Jarvis C.I. COVID-19: A need for real-time monitoring of weekly excess deaths. The Lancet. 2020;395(10234):e81. doi: 10.1016/S0140-6736(20)30933-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markides K.S., Eschbach K. Aging, migration, and mortality: Current status of research on the hispanic paradox. Journal of Gerontology: Serie Bibliographique. 2005;60(Special_Issue_2):S68–S75. doi: 10.1093/geronb/60.Special_Issue_2.S68. [DOI] [PubMed] [Google Scholar]
- Márquez J.D. Latinos as the “living dead”: Raciality, expendability, and border militarization. Latino Studies. 2012;10(4):473–498. doi: 10.1057/lst.2012.39. [DOI] [Google Scholar]
- McClure E.S., Vasudevan P., Bailey Z., Patel S., Robinson W.R. Racial capitalism within public health—how occupational settings drive COVID-19 disparities. American Journal of Epidemiology. 2020;189(11):1244–1253. doi: 10.1093/aje/kwaa126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michaels D., Wagner G.R. Occupational safety and health administration (OSHA) and worker safety during the COVID-19 pandemic. Journal of the American Medical Association. 2020;324(14):1389. doi: 10.1001/jama.2020.16343. [DOI] [PubMed] [Google Scholar]
- Mora G.C. Cross-field effects and ethnic classification: The institutionalization of hispanic panethnicity, 1965 to 1990. American Sociological Review. 2014;79(2):183–210. doi: 10.1177/0003122413509813. [DOI] [Google Scholar]
- Noe-Bustamante L., Flores A., Shah S. Facts on Latinos of Guatemalan origin in the U.S. Pew research center's hispanic trends project. https://www.pewresearch.org/hispanic/fact-sheet/u-s-hispanics-facts-on-guatemalan-origin-latinos/
- Page K.R., Flores-Miller A. Lessons we’ve learned — covid-19 and the undocumented Latinx community. New England Journal of Medicine. 2020 doi: 10.1056/NEJMp2024897. [DOI] [PubMed] [Google Scholar]
- Page K.R., Venkataramani M., Beyrer C., Polk S. Undocumented U.S. Immigrants and covid-19. New England Journal of Medicine. 2020;382(21):e62. doi: 10.1056/NEJMp2005953. [DOI] [PubMed] [Google Scholar]
- Passel J., Cohn D. Mexicans decline to less than half the U.S. unauthorized immigrant population for the first time. Pew Research Center. https://www.pewresearch.org/fact-tank/2019/06/12/us-unauthorized-immigrant-population-2017/
- Patler C., Gleeson S., Schonlau M. Contesting inequality: The impact of immigrant legal status and education on legal knowledge and claims-making in low-wage labor markets. Social Problems. 2020 doi: 10.1093/socpro/spaa029. [DOI] [Google Scholar]
- Perreira K.M., Pedroza J.M. Policies of exclusion: Implications for the health of immigrants and their children. Annual Review of Public Health. 2019;40(1):147–166. doi: 10.1146/annurev-publhealth-040218-044115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riosmena F., Kuhn R., Jochem W.C. Explaining the immigrant health advantage: Self-selection and protection in health-related factors among five major national-origin immigrant groups in the United States. Demography. 2017;54(1):175–200. doi: 10.1007/s13524-016-0542-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez-Diaz C.E., Guilamo-Ramos V., Mena L., Hall E., Honerman B., Crowley J.…Millett G. Risk for COVID-19 infection and death among Latinos in the United States: Examining heterogeneity in transmission dynamics. Annals of Epidemiology. 2020 doi: 10.1016/j.annepidem.2020.07.007. 23, 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossen L.M. Excess deaths associated with COVID-19, by age and race and ethnicity — United States, January 26–October 3, 2020. MMWR Morb Mortal Wkly Rep. 2020;69 doi: 10.15585/mmwr.mm6942e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sáenz R., Garcia M.A. The disproportionate impact of COVID-19 on older Latino mortality: The rapidly diminishing Latino paradox. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2021 doi: 10.1093/geronb/gbaa158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez T. One Oakland neighborhood has seen a surge in positivity rates among Latino and indigenous populations. Why? San francisco chronicle. https://www.sfchronicle.com/bayarea/article/One-Oakland-neighborhood-has-seen-a-surge-in-15651955.php Accessed December 15, 2020.
- Small-Rodriguez, Dislorei . The University of Arizona; 2020. Remaking Collective Identities: Statistical Statecraft, Indigenous Erasure, and Tribal Citizenship.https://www.proquest.com/openview/cbffcdb3eb4288a9d2fed18586be5175/1?pq-origsite=gscholar&cbl=18750&diss=y Proquest Dissertations Publishing. [Google Scholar]
- Torres-Pinzon D.L., Solorzano W., Kim S.E., Cousineau M.R. Coronavirus disease 2019 and the case to cover undocumented immigrants in California. Health Equity. 2020;4(1):500–504. doi: 10.1089/heq.2020.0049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolf S.H., Chapman D.A., Sabo R.T., Weinberger D.M., Hill L., Taylor D.D.H. Excess deaths from COVID-19 and other causes, march-july 2020. Journal of the American Medical Association. 2020;324(15):1562. doi: 10.1001/jama.2020.19545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yearby R., Mohapatra S. Law, structural racism, and the COVID-19 pandemic. Journal of Law and the Biosciences. 2020;7(lsaa036) doi: 10.1093/jlb/lsaa036. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.