Learning objectives.
By reading this article you should be able to:
-
•
Describe the role of shared decision making within the healthcare setting.
-
•
Explore ways to involve patients in decisions about high-risk surgery.
-
•
Outline the structure of a shared decision-making consultation.
-
•
Discuss the evidence for using shared decision making in perioperative practice.
Key points.
-
•
Shared decision making is a form of patient-centred care, combining clinical expertise with patients' personal values and preferences to choose an appropriate treatment.
-
•
Shared decision making can be used in perioperative medicine to guide decisions about high-risk surgery.
-
•
Clinicians need to be able to communicate the benefits and risks of different treatment options during a shared decision making consultation.
-
•
Patients who are involved in decisions about their care have fewer regrets and better health outcomes than those who are not.
-
•
Incorporating shared decision making into perioperative pathways may require culture change and reconfiguration of services.
Clinical Scenario A
Background
Mrs A is an 84-year-old female who presented to her family doctor with fatigue and was found to have an iron deficiency anaemia (haemoglobin 72 g L−1, ferritin 48 ng ml−1), which was treated with a blood transfusion and iron supplementation. Despite treatment her symptoms recurred, and a computed tomography (CT) colonoscopy found a non-obstructing mass (likely sigmoid adenocarcinoma). The colorectal multidisciplinary team (MDT) was concerned about the risks of surgery and so referred her to the perioperative medicine clinic before proceeding to a colonoscopy.
Benefits, risks, alternatives and doing nothing (BRAN)
In the clinic the CT findings and likely diagnosis were explained, and the possibility of surgery was introduced. She initially felt positive about the idea of an operation, having had multiple uneventful procedures in the past.
During the appointment an assessment of her fitness was performed–combining this information with her age and comorbidities she was predicted to have a 10% 30-day mortality following an open resection, with the risk of life-changing complications estimated to be approximately 20%. She was not suitable for laparoscopic surgery because of scarring from previous abdominal procedures. Deciding not to have surgery would avoid the risk of perioperative complications, but itself carried risks of intestinal obstruction, perforation or spread to other organs. Information about non-surgical options (e.g. chemotherapy or radiotherapy) could not be provided without a formal diagnosis but had been noted to be unlikely to help during the MDT meeting. Using a locally validated risk prediction tool we estimated Mrs A's median survival as 4 years.
When asked what mattered to her, Mrs A said that she and her husband still lived in their own home and managed to be self-sufficient. Although she initially felt that surgery would be a good option, she had not appreciated the chance of a complication that would prevent her from returning home or to her current quality of life. Her only symptom was tiredness, and this had improved with further iron supplementation. She did express concern that if she declined further investigations or surgery she would be seen as refusing treatment and would not be offered any help if she developed other symptoms. Dying in pain was a major worry, as she had previously watched her sister die from cancer with limited pain relief or support.
Decision and plan
After the clinic appointment, Mrs A requested some time at home to talk through her options. A letter detailing the conversation was sent to Mrs A, her family doctor and the referring surgeon, and she was reassured that she would have access to symptom management and palliative care if required. She eventually decided not to pursue any further investigations.
Clinical Scenario B
Background
Mr B is a 72-year-old male who was found to have a 6.9-cm infrarenal abdominal aortic aneurysm (AAA) after presenting with abdominal pain and weight loss. He was referred to the perioperative medicine clinic by the vascular team prior to a surgical appointment.
Benefits, risks, alternatives and doing nothing (BRAN)
At the clinic Mr B's fitness was assessed and combined with clinical information to provide a personalised risk assessment. His predicted 30-day mortality after an open AAA repair was 8%, whilst it was 3% following an endovascular aneurysm repair (EVAR). Median survival with best medical treatment was 2 years, with median survival following a surgical intervention predicted to be 7 years. There was a higher chance of morbidity in the perioperative period following the open procedure.
Mr B understood the risks and benefits of the treatment options and was keen to have an operation. However, he was not sure that it was the right time for him to have surgery as his granddaughter was due to sit her A level examinations. If she did well, she would be the first person in their family to go to university. He and his wife were the main carers for their granddaughter, and Mr B wanted to be able to support her during this time.
Decision and plan
The risk prediction data from the perioperative clinic was used at the surgical appointment to go through the options with Mr B again. The surgeon and patient decided together to defer surgery for a 4-month period, balancing the risks of rupture with Mr B's wish to support his granddaughter. He opted for an EVAR to minimise short-term risks and recovery length after the operation. The surgery was performed uneventfully, and his granddaughter was accepted to university.
Shared decision making (SDM) is a process in which clinicians and patients work together to decide the best treatment for a condition. It combines clinical expertise and evidence with individual patients' experiences and preferences—when done properly SDM helps people to understand the treatment options available to them, and the risks and benefits of these choices. It can be used to guide all decision making in the non-emergency setting, including the option not to have treatment. Shared decision making moves beyond traditional consent and its focus on information provision, to a collaborative style which recognises an individual's role in managing their own health.1 The patient is placed at the centre of the process, with their concerns and personal circumstances playing a major part in decisions.2 Patients are viewed as competent decision makers, whilst clinicians provide information and support to help them to make a choice that is right for them.
The concept of SDM first appeared within the healthcare literature in 1982, and it has become increasingly prominent in recent years.3 The 2012 UK Health and Social Care Act mandates that individuals participate in decisions about their care, the National Institute for Health and Care Excellence (NICE) have produced advice on using SDM, and professional regulatory bodies such as the General Medical Council (GMC) endorse its use.4, 5, 6 In 2011, the King's Fund produced a document to encourage the adoption of SDM during patient-clinician interactions (‘Making shared decision making a reality’).7 More recently, the UK branch of Choosing Wisely—a global initiative aimed at improving conversations between patients and their doctors and nurses—proposed using SDM as a way to reduce unnecessary tests and treatments.8 Despite these efforts, the incorporation of SDM into clinical practice has been slow, and studies suggest that doctors are more likely than patients to believe that a consultation has involved a shared decision.9,10
Shared decision making is one element of the personalised care model for healthcare, and the NHS Long-term Plan has set a target of providing personalised care to 2.5 million people in the UK by 2024.11 NHS England has recently launched the Personalised Care Institute (PCI), a virtual organisation responsible for setting the standards for training and development in personalised care.12 The PCI offers accreditation in delivering personalised care programmes to training providers, and giving healthcare workers free access to relevant learning materials. It is hoped that this will help to drive the use of all components of personalised care, including SDM, by healthcare professionals and teams.
SDM in perioperative practice
Approximately 10 million people undergo surgery within the NHS each year, of whom 250,000 are classed as being ‘high risk’.13 Patients who are at a high risk of dying after an elective procedure (predicted 30-day mortality of >1%) should be identified by age, type of surgery, and coexisting medical conditions. They should have an SDM consultation to discuss their individual chance of benefit or harm and to identify their personal preference.8
An increasingly elderly population with more comorbidities means that the number of patients who are deemed to be high risk for surgery is likely to increase. One in three high-risk patients experience a significant complication during the perioperative period, which can lead to a long-term decline in health and quality of life.14 Most conditions have a variety of surgical and non-surgical treatment options, and each of these choices will have different possible outcomes and associated uncertainties. Traditional preoperative clinics provide patients with some of this information but can fail to acknowledge the interplay between such information and individual circumstances and wishes. Shared decision making offers an alternative approach and can be used by any clinician involved in perioperative medicine to provide personalised, evidenced-based care. This article details an approach to structuring an SDM conversation for high-risk surgery, based on our experiences in a perioperative medicine clinic at a UK district general hospital (Torbay and South Devon NHS Foundation Trust). Evidence for the use of SDM and structuring of an SDM service is also explored.
Structure of an SDM consultation
The King's Fund document lists three essential components for effective SDM7:
-
(i)
The provision of reliable, evidence-based information outlining treatment options, outcomes, and uncertainties
-
(ii)
Decision support counselling to clarify options and preferences
-
(iii)
A system for recording, communicating and implementing a patient's preferences
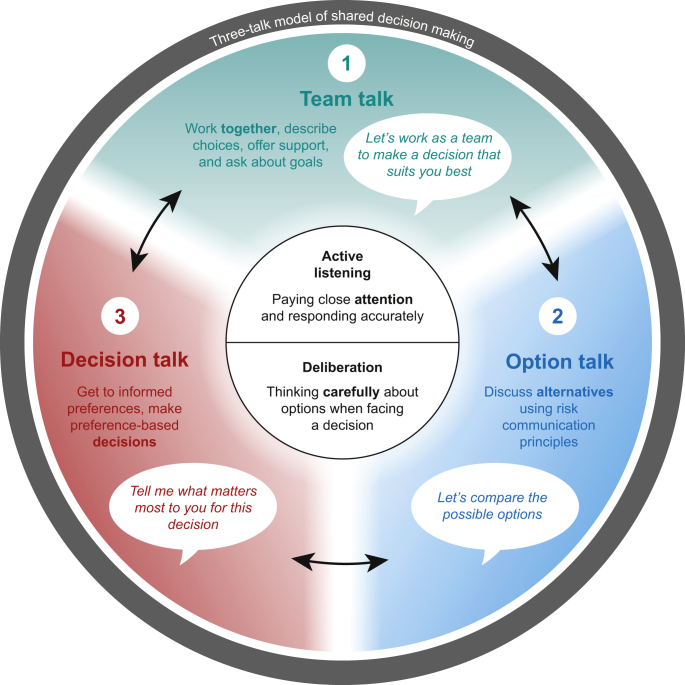
More recently, a three-talk model has been proposed by Elwyn and colleagues2 to help clinicians to structure an SDM consultation (Fig. 1). Although the phases are distinct in the model, a more fluid approach tends to be used in practice.
Fig 1.
The three-talk model of shared decision making.2
Shared decision making requires teamwork between patient and clinician, as both parties will bring different forms of expertise to the process. The clinician can provide information about diagnosis, prognosis, treatment options, and outcome probabilities, whilst the patient will know about the impact of the condition on their life and their personal attitude towards risk. They will also have unique values, preferences, and social circumstances that are likely to influence decision making. A simple example would be a patient who is a carer for their partner, and so is keen to avoid staying in hospital or have a protracted recovery. Clinicians should have a broad understanding of both the surgical and non-surgical options, or be able to refer onwards when more information is required. It is important that the patient realises the purpose of the consultation, as many people attending a perioperative medicine clinic may feel that a decision has already been made about proceeding to surgery. Telephone calls before the appointment, letters containing information about the consultation, and information in the waiting room can be used to help set the agenda and prepare the patient for an SDM consultation.
Starting with an open question will help to explore understanding and build a rapport—‘What do you understand about your condition?‘; ‘What do you know about the treatment options available?’ Using simple, non-emotive language is important, as is pausing and allowing time for the patient to process any information you provide. Clinicians must assess what the patient needs to know to make a decision, as it will often be impossible to share every possible risk, adverse effect, or complication. Finding out what matters to the patient requires open dialogue and an appropriate environment to allow them to relax and share their thoughts. We encourage people to attend the clinic with a relative or friend for support, and advise clinicians to facilitate communication by minimising any physical barriers such as desks or computers. There is often a difference between what a patient wants and what healthcare professionals believe they will want (‘preference misdiagnosis’).5 Exploring what they hope to gain from an operation, and assessing if this is a realistic hope, will help to ensure that you can work as a team to choose the most suitable treatment.
An SDM consultation should provide a patient with a good understanding of the risks, benefits, and possible consequences of the different options available, and the ability to communicate risk is a key part of the process. This is particularly important as many individuals will overestimate the benefits of a medical intervention whilst underestimating any associated risks.15 There are a number of prediction models available online to help inform the conversation—commonly used versions include the surgical outcome risk tool (SORT) and the American College of Surgeons (ACS) risk calculator.16,17 In our perioperative medicine clinic we use a locally developed and validated model that includes long-term survival.18 In practical terms, using absolute risk is more helpful than relative risk, and numbers have been shown to work better than words.7 Risks should be discussed in context where possible—the ACS calculator provides this information by comparing an individual's personal risk profile with the average risk profile for that procedure. Symmetric framing can also provide clarity and help to minimise clinicians' bias—for example, if you say that 30 people in 100 are likely to experience complications then also say that 70 in 100 will not. Using pictures to aid discussions has been shown to be the most effective way to communicate risk effectively, and there are icon array tools available for free online to facilitate this.19
Recognising uncertainty is important, as knowledge about risk is based on population data and outcomes are unpredictable at an individual level.20 It is vital to check the patient's interpretation of risk, as a potential complication may be viewed as catastrophic by one person but not by another. This may make the difference between deciding to have surgery or opting for conservative management. Information provided by the patient will help to shape the discussion around risks and benefits—to give an example, an individual with a slow growing and asymptomatic tumour may be less willing to risk perioperative morbidity than someone who is incapacitated by their symptoms. Further information and training on communicating risk during the perioperative period can be accessed via a free e-learning module created by the Winton Centre in association with the Academy of Medical Royal Colleges.21
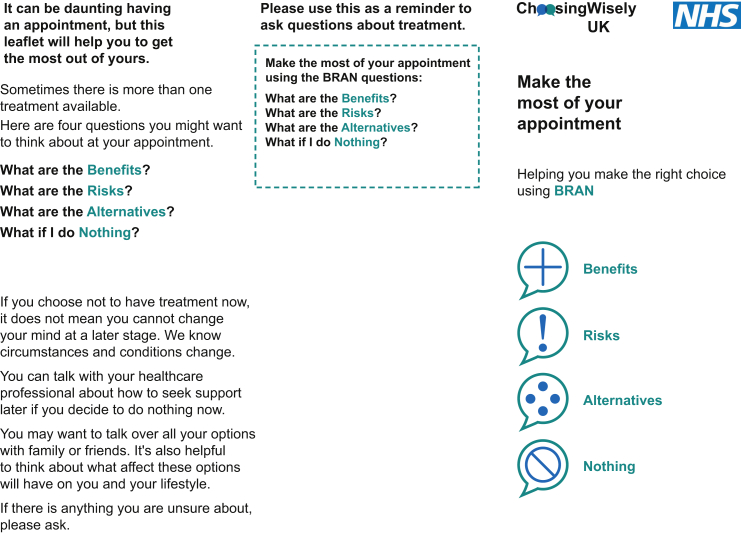
Throughout the consultation it is important to encourage questions—this may come naturally to some patients but not to others. If the patient is unsure what to ask it is often possible to guide them with open questions—‘what do you know about the benefits of the possible treatments?‘; ‘when it comes to thinking about what the treatment might offer you, or the possible risks of the treatment, what is the most important aspect for us to consider?‘7 Choosing Wisely UK advocates use of the BRAN tool to encourage patients to ask four key questions during a consultation (Fig. 2).22 Providing this leaflet in advance of a consultation will allow patients to prepare questions that are relevant to them—clinicians can then help an individual to consider their options by exploring their reactions to information and by discussing the potential impact of each choice on quality of life or on health goals. Decision aids for patients can also be used as part of this process and have been shown to increase patients' participation in decision making.23 They differ from traditional information leaflets by including outcome probabilities and acknowledging uncertainties, and can vary from a simple document to an interactive website. Decision aids are available for a variety of conditions and treatments—examples can be found at www.patient.co.uk or www.nice.org.uk.
Fig 2.
The BRAN tool from Choosing Wisely UK.22
All information provided to patients needs to be clear and aimed at the appropriate level. Most adults in the UK have the reading age of an average 11–14-yr-old, and so information should be targeted to this level of literacy.24 There are guides on how to achieve this available online—one example is the health literacy ‘how to’ guide created by Health Education England.24 Good communication often involves multiple modalities, and patient-specific preferences should be taken into account. Allowing individuals to record consultations and offering paper copies of any written or pictorial documentation of risk discussions can help to maximise understanding. Checking understanding can be achieved with the ‘teach back’ method, whereby the patient is asked to summarise the information they have just received. If there is any doubt about understanding, repeating the information or providing it in a different format as above can help. In our experience relatives are often able to communicate information in a way that the patient understands, and so can be invaluable in helping to ensure that key facts are conveyed effectively.
Decision making can be difficult, especially when the risks around treatment or doing nothing are perceived as high. It is important to allow time and try not to rush the process. Patients may want to go away to discuss their options with family and friends, and this should be encouraged when feasible. Additional information may sometimes be required after the initial consultation and may involve a further appointment to discuss symptom management or alternative surgical options. Such an approach requires collaboration and flexibility between specialties and services. We see patients at different times, with some having already seen a surgeon and others not yet aware of the results of their investigations. Whatever the stage of the process it is important to be clear that they have a choice, and that not having an operation may be a valid option for them. Patients may ask you to make a decision for them, and many clinicians involved in SDM will happily share their views. If doing this, it is important to emphasise that you may have different values and that these will influence your opinion. You should be aware of your own biases and how these may influence discussions—regular case reviews with other perioperative physicians will help to highlight and minimise any such issues. Some patients may not want to have any role in making decisions about their treatment, but all should be given the opportunity to be involved.
Evidence for using SDM
Many patients would like to be more involved in decisions about their care, and those who are involved in decision making have fewer regrets about their treatment, better perceived communication with clinicians, and improved treatment adherence.25,26 Shared decision making leads to increased confidence and coping skills, and greater comfort with making decisions.7 People with the lowest levels of health literacy have been shown to benefit most from SDM, helping to minimise health inequalities.26 The use of decision aids appears to improve knowledge and the accuracy of risk perception without incurring an increase in cost to the healthcare provider.25,27 People who are active participants in managing their health have also been shown to have better health outcomes than those who are passive recipients of care.7 Shared decision making can also limit unwarranted variation in clinical practice and may reduce complaints and litigation.28
Within the perioperative setting, SDM may lead to a reduction in the number of people opting for surgical treatment—patients are often more risk averse than clinicians, and informed patients will commonly choose a conservative treatment option.25 There is potential for an associated cost benefit, although evidence for this is not yet clear. Shared decision making consultations for high-risk surgery may require a longer clinic appointment than the traditional medical consultation. However, it does not seem that SDM extends the total time spent with patients. Three systematic reviews of SDM and patients' decision aids have found no increase in the overall time taken for consultations.25,29,30
Structuring a service
Incorporating SDM into the perioperative pathway for high-risk surgery requires investment in training and education to develop SDM skills. Services may need to be reconfigured, and cultural change may be necessary to move beyond a traditional approach to medical decision making. Including SDM from the start of the perioperative process will allow patients sufficient time to consider all available options, but may require considerable changes to current working practices and pathways. There is a need to reduce ‘silo’ specialty working, with the focus of care being centred around the patient rather than a specific team. NHS England have produced an implementation framework to help develop SDM within established services (Table 1); further details are available in the associated SDM summary guide and implementation checklist.1
Table 1.
NHS England SDM implementation framework
| Shared decision making | |||
|---|---|---|---|
| Prepared public | Supportive systems and processes | Commissioned services | Trained teams |
| Ask three questions | Leadership at every level including clinical | Redesign pathways to incorporate SDM | Accredited training and SDM champions |
| It's ok to ask | Health-literate decision support tools | Align measures and incentivise SDM in local delivery plans and operational models | Mixed learning methods and mixed levels of learning |
There are many potential barriers to the development of an effective SDM service, including training in effective communication styles, learning to manage uncertainty, and a willingness to initiate emotionally difficult conversations with patients. In 2010, the making good decisions in collaboration (MAGIC) programme was created to identify and evaluate the best ways to embed SDM into clinical practice. This found that role-play and exercises that challenged established attitudes were the most effective ways to change practice and to increase the use of SDM.31 Encouragingly, attitudes were shown to be more effective than either skills or tools in driving change and establishing SDM within a service. NICE are due to publish formal guidance on implementing SDM in April 2021 and the PCI provide access to training in personalised care. There is also ongoing research exploring perceptions of patients and professionals about SDM for high-risk major surgery.32 All of these may inform the development of specific tools to support SDM in the future.
Summary
Shared decision making can be used in the perioperative setting to provide evidence-based, patient-centred care. It requires teamwork between patients and clinicians, allowing people to make fully informed decisions about their care based on what matters to them. Incorporating SDM into the traditional perioperative pathway may involve cultural change and service reconfiguration, but will increase patient knowledge and satisfaction and help to minimise health inequalities.
Declaration of interests
The authors declare that they have no conflicts of interest.
Biographies
Gillian Barnett FRCA is a clinical fellow in perioperative medicine at University College Hospital London and the Westmoreland Hospital.
Michael Swart FRCA EDICM FICM is a consultant in anaesthesia, intensive care, and perioperative medicine at Torbay Hospital. He is also joint clinical lead for the NHS Getting It Right First Time (GIRFT) programme for anaesthesia and perioperative medicine.
Matrix codes: 1F01, 2A08, 3I00
MCQs
The associated MCQs (to support CME/CPD activity) will be accessible at www.bjaed.org/cme/home by subscribers to BJA Education.
References
- 1.NHS England and NHS Improvement. Shared decision making, summary guide. Available from https://www.england.nhs.uk/shared-decision-making-summary-guide/(accessed 29 July 2020).
- 2.Elwyn G., Durand M.A., Song J. A three-talk model for shared decision making: multistage consultation process. BMJ. 2017;359:j4891. doi: 10.1136/bmj.j4891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.President’s Commission . US Government Printing Office; Washington DC: 1982. President’s commission for the study of ethical problems in medicine and biomedical and behavioural research making health care decisions. The ethical and legal implications of informed consent in the patient-practitioner relationship. [Google Scholar]
- 4.Health and social care Act 2012, section 13H. Available from https://www.legislation.gov.uk/ukpga/2012/7/pdfs/ukpga-20120007-en.pdf/(page 20; accessed 29 July 2020).
- 5.NICE advice on shared decision making. Available from https://www.nice.org.uk/advice/ktt23/resources/shared-decision-making-pdf-58758011521477/(accessed 29 July 2020).
- 6.General Medical Council, General medical practice. Available from https://www.gmc-uk.org/ethical-guidance/ethical-guidance-for-doctors/good-medical-practice/(accessed 29 July 2020).
- 7.Coulter A., Collins A. The King’s Fund; London: 2011. Making shared decision making a reality. No decision about me, without me. [Google Scholar]
- 8.Academy of Medical Royal Colleges, Choosing Wisely. Available from http://www.choosingwisely.co.uk/resources/(accessed 29 July 2020).
- 9.Stevenson F.A., Barry C.A., Britten N., Barber N., Bradley C.P. Doctor-patient communication about drugs: the evidence for shared decision making. Soc Sci Med. 2000;50:829–840. doi: 10.1016/s0277-9536(99)00376-7. [DOI] [PubMed] [Google Scholar]
- 10.De Mik S.M.L., Stubenrouch F.E., Balm R., Ubbink D.T. Systematic review of shared decision making in surgery. Br J Surg. 2018;105:1721–1730. doi: 10.1002/bjs.11009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.NHS England . 2019. NHS long term plan. Available from NHS long term plan. accessed. [Google Scholar]
- 12.Personalised care Institute, NHS England. Available from https://www.personalisedcareinstitute.org.uk (accessed 24 October 2020).
- 13.The case for perioperative care. Describing the need. Available from https://www.cpoc.org.uk/node/396/(accessed 29 July 2020).
- 14.Centre for perioperative care: shared decision making and OSIRIS. Available from https://www.cpoc.org.uk/shared-decision-making-and-osiris/(accessed 29 July 2020).
- 15.Hoffmann T.C., Del Mar C. Patients’ expectations of the benefits and harms of treatments, screening and tests: a systematic review. JAMA Intern Med. 2015;175:274–286. doi: 10.1001/jamainternmed.2014.6016. [DOI] [PubMed] [Google Scholar]
- 16.Surgical outcome risk tool. Available from https://www.sortsurgery.com/(accessed 29 July 2020).
- 17.American College of Surgeons National Surgical Quality Improvement Program Surgical risk calculator. Available from https://www.riskcalculator.facs.org/RiskCalculator/(accessed 29 July 2020).
- 18.Carlisle J.B., Danjoux G., Kerr K., Snowden C., Swart M. Validation of long term survival prediction for scheduled abdominal aortic aneurysm repair with independent calculator using only preoperative variables. Anaesthesia. 2015;70:654–665. doi: 10.1111/anae.13061. [DOI] [PubMed] [Google Scholar]
- 19.Freeman A.L.J. How to communicate evidence to patients. Drug Ther Bull. 2019;57:119–124. doi: 10.1136/dtb.2019.000008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Elwyn G., Frosch D., Thomson R. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27:1361–1367. doi: 10.1007/s11606-012-2077-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Helping patients make informed decisions: communicating potential harms and benefits (perioperative care). Available from https://moodle.wintoncentre.uk (accessed 29 July 2020).
- 22.Santhirapala R., Fleisher L.A., Grocott M.P.W. Choosing wisely: just because we can, does it mean we should? Br J Anaesth. 2019;122:306–310. doi: 10.1016/j.bja.2018.11.025. [DOI] [PubMed] [Google Scholar]
- 23.Stacey D., Legare F., Lewis K. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017;4:CD001431. doi: 10.1002/14651858.CD001431.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Health literacy guide, health education England. Available from https://www.hee.nhs.uk/our-work/population-health-training-educational-resources (accessed 24 October 2020).
- 25.Care Quality Commission. Better care in my hands: a review of how people are involved in their care. Available from https://www.cqc.org.uk/sites/default/files/20160519_Better_care_in_my_hands_FINAL.pdf/(accessed 29 July 2020).
- 26.Durand M.A., Carpenter L., Dolan H. Do interventions designed to support shared decision making reduce health inequalities? A systematic review and meta-analysis. PLoS One. 2014;9 doi: 10.1371/journal.pone.0094670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.King J.S., Moulton B.W. Rethinking informed consent: the case for shared medical decision making. Am J Law Med. 2006;32:429–501. doi: 10.1177/009885880603200401. [DOI] [PubMed] [Google Scholar]
- 28.Legare F., Ratte S., Stacey D. Interventions for improving the adoption of shared decision making by healthcare professionals. Cochrane Database Syst Rev. 2014;9:CD006732. doi: 10.1002/14651858.CD006732.pub2. [DOI] [PubMed] [Google Scholar]
- 29.Legare F., Turcotte S., Stacey D. Patients’ perceptions of sharing in decisions: a systematic review of interventions to enhance shared decision making in routine clinical practice. Patient. 2012;5:1–19. doi: 10.2165/11592180-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 30.King E., Taylor J., Williams R., Vanson T. The Health Foundation; 2013. The MAGIC programme: evaluation.https://www.health.org.uk/publications/the-magic-programme-evaluation/ Available from. accessed. [Google Scholar]
- 31.Optimising shared decision making for high-risk major surgery. Available from https://www.osiris-programme.org/(accessed 29 July 2020).