Key Points
Question
Is automatically measured coronary artery calcium (CAC) on radiotherapy planning computed tomographic (CT) imaging results associated with cardiovascular disease (CVD) in patients treated for breast cancer?
Findings
Among 15 915 patients included in this cohort study, a strong association between CAC and CVD was found, especially coronary artery disease; the association between CAC and CVD was strongest in patients treated with anthracyclines and patients who received a radiation boost.
Meaning
Automated CAC scoring on radiotherapy planning CT scan results might be used as a fast and low-cost tool to identify patients with breast cancer at increased CVD risk, allowing implementing CVD risk-mitigating strategies aimed to reduce CVD burden after breast cancer.
This cohort study evaluates the association of coronary artery calcium levels with cardiovascular disease and coronary artery disease in patients with breast cancer.
Abstract
Importance
Cardiovascular disease (CVD) is common in patients treated for breast cancer, especially in patients treated with systemic treatment and radiotherapy and in those with preexisting CVD risk factors. Coronary artery calcium (CAC), a strong independent CVD risk factor, can be automatically quantified on radiotherapy planning computed tomography (CT) scans and may help identify patients at increased CVD risk.
Objective
To evaluate the association of CAC with CVD and coronary artery disease (CAD) in patients with breast cancer.
Design, Setting, and Participants
In this multicenter cohort study of 15 915 patients with breast cancer receiving radiotherapy between 2005 and 2016 who were followed until December 31, 2018, age, calendar year, and treatment-adjusted Cox proportional hazard models were used to evaluate the association of CAC with CVD and CAD.
Exposures
Overall CAC scores were automatically extracted from planning CT scans using a deep learning algorithm. Patients were classified into Agatston risk categories (0, 1-10, 11-100, 101-399, >400 units).
Main Outcomes and Measures
Occurrence of fatal and nonfatal CVD and CAD were obtained from national registries.
Results
Of the 15 915 participants included in this study, the mean (SD) age at CT scan was 59.0 (11.2; range, 22-95) years, and 15 879 (99.8%) were women. Seventy percent (n = 11 179) had no CAC. Coronary artery calcium scores of 1 to 10, 11 to 100, 101 to 400, and greater than 400 were present in 10.0% (n = 1584), 11.5% (n = 1825), 5.2% (n = 830), and 3.1% (n = 497) respectively. After a median follow-up of 51.2 months, CVD risks increased from 5.2% in patients with no CAC to 28.2% in patients with CAC scores higher than 400. After adjustment, CVD risk increased with higher CAC score (hazard ratio [HR]CAC = 1-10 = 1.1; 95% CI, 0.9-1.4; HRCAC = 11-100 = 1.8; 95% CI, 1.5-2.1; HRCAC = 101-400 = 2.1; 95% CI, 1.7-2.6; and HRCAC>400 = 3.4; 95% CI, 2.8-4.2). Coronary artery calcium was particularly strongly associated with CAD (HRCAC>400 = 7.8; 95% CI, 5.5-11.2). The association between CAC and CVD was strongest in patients treated with anthracyclines (HRCAC>400 = 5.8; 95% CI, 3.0-11.4) and patients who received a radiation boost (HRCAC>400 = 6.1; 95% CI, 3.8-9.7).
Conclusions and Relevance
This cohort study found that coronary artery calcium on breast cancer radiotherapy planning CT scan results was associated with CVD, especially CAD. Automated CAC scoring on radiotherapy planning CT scans may be used as a fast and low-cost tool to identify patients with breast cancer at increased risk of CVD, allowing implementing CVD risk-mitigating strategies with the aim to reduce the risk of CVD burden after breast cancer.
Trial Registration
ClinicalTrials.gov Identifier: NCT03206333
Introduction
Cardiovascular disease (CVD) is common in patients diagnosed with breast cancer.1,2,3 In older patients, CVD competes with breast cancer as the leading cause of death.4 Some treatments, such as anthracyclines, targeted therapy, and radiotherapy are associated with an increased risk of CVD.5,6 Patients treated with anthracyclines have a 5-times higher risk of developing chronic heart failure or reduced left ventricular ejection fraction compared with those treated without.7 The risks of coronary artery disease (CAD) and myocardial infarction are increased in patients who received radiotherapy.8,9 Patients with breast cancer with preexisting CVD risk factors (eg, hypertension, obesity, diabetes) have the highest risk of treatment-induced cardiotoxic effects.10
Coronary artery calcium (CAC), as quantified on computed tomographic (CT) scans, is an independent risk factor for CVD.11,12 Most patients with breast cancer are treated with radiotherapy and undergo planning CT scans of the chest. An association between CAC on radiotherapy planning CT scans and acute coronary events has been reported.13 Coronary artery calcium scoring is usually performed manually and can be tedious and time-consuming, especially when many scans are involved or when the image quality is suboptimal (nongated scans). Our research group developed a deep-learning calcium scoring algorithm for automated CAC scoring on dedicated cardiac CT scans.14,15 Automatic quantification of CAC offers the opportunity for routine, fast, and low-cost identification of breast cancer patients with an increased CVD risk without additional diagnostic radiation exposure.
In the Bragatston study, we evaluate whether CAC, automatically measured on radiotherapy planning CT scans, is associated with an increased risk of CVD in patients treated for breast cancer.16
Methods
Study Population
Radiotherapy planning CT scans and clinical data were collected for patients who were irradiated for primary breast cancer between January 2005 and December 2016 in the University Medical Center Utrecht, the Erasmus MC, Rotterdam, and the Radboudumc, Nijmegen, the Netherlands. Patients were excluded when they had metastasis at presentation or when planning CT scans were obtained 1 year or longer after breast cancer diagnosis. For patients with multiple planning CT scans, the first scan was used. When 2 scans were made on the same day, the scan with breath-hold technique was used because of higher reproducibility of CAC scoring (ie, fewer motion artifacts).17
Through linkage with the Netherlands Cancer Registry (NCR), information was obtained on laterality, TNM stage, grade, receptor status, type of surgery, radiotherapy and chemotherapy, endocrine therapy, targeted therapy, and occurrence of other cancers.18
The institutional review boards of the participating hospitals decided that the Medical Research Involving Human Subjects Act did not apply. Requirement for informed consent was waived.
Automatic Calcification Quantification
Planning CT scans without contrast enhancement and without ECG-synchronization were acquired as part of clinical routine (typical parameters: 120 kVp, in-plane resolution 0.51-1.56 mm, and 1.5-5.0 mm slice thickness). Patient scans were reconstructed to 3.0-mm slice thickness and 1.5-mm increment. Levels of CAC were measured automatically using a deep-learning calcium scoring algorithm that detects and quantifies calcifications in the coronary arteries (eMethods in the Supplement).14,15 In our previous study,14 reproducibility of automatically vs manually measured calcium scores was rated as high (linearly weighted κ, 0.91; intraclass correlation coefficient, 0.85).
Coronary artery calcium was expressed as modified Agatston score, calculated by multiplying the calcification area (in mm2) by the weight (1, 130-199 Hounsfield Units [HU]; 2, 200-299 HU; 3, 300-399 HU; 4, >399 HU) determined by the maximum density of the area and summing the lesion scores over slices. A minimal lesion definition of 1.5 mm3 was maintained to eliminate noise. Patients were categorized into 5 categories: 0, 11 to 0, 11 to 100, 101 to 400, >400 Agatston units.19
Outcome Assessment
The primary outcome was incidence of fatal and nonfatal (ie, hospitalization for) CVD events between the date of the CT scan and end of follow-up (December 31, 2017). Other outcomes were fatal and nonfatal CAD (a subset of CVD), and all-cause mortality (including CVD deaths; follow-up until December 31, 2018).
Data on hospitalization for CVD and cancer (recurrence), and death was collected through linkage with national registries by Statistics Netherlands. Each hospital sent individual patient data to Statistics Netherlands and a pseudonym of the combination of national personal identification number, sex, date of birth, and postal code was used for linkage with national registries. Data on hospital admissions, including inpatient hospital care, day care and long-standing observation (≥4 hours), were obtained by linkage to the national basic registration hospital care (Landelijke Basisregistratie Ziekenhuiszorg, before 2013 Landelijke Medische Registratie), managed by Dutch Hospital Data. Dutch Hospital Data used the International Classification of Diseases, Ninth Revision (ICD-9) before 2013 and the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) from 2013 onward for disease classification.20 Diagnoses registered according to ICD-9 were converted to ICD-10 using the conversion table of the Dutch WHO-FIC Collaborating Centre.21 Cardiovascular disease was defined by ICD-10 codes I00-99 (eTable 1 in the Supplement). Lymphedema (I88-89) and varicose veins (I83-86) were not considered CVD events. Coronary artery disease was defined by codes I20-25 (eg, myocardial infarction and angina pectoris). Cancer, including recurrent disease or metastases, was defined by ICD-10 codes C00-99, and nonmelanoma skin cancer (C44) was not considered for analysis. Breast cancer hospitalizations in the LBZ/LMR within 1 year after the radiotherapy planning CT scan were considered as belonging to the initial breast cancer diagnosis and therefore not considered as recurrence or new breast cancer.
Mortality data were obtained from the National Death Register, which contains information on primary cause of death from all the deceased persons registered in the Netherlands. Causes of death were classified according to the ICD-10.20
Statistical Analysis
Follow-up time started at date of radiotherapy planning CT scan and ended at date of the event, censoring, or end of follow-up, whichever came first. Censored observations included noncardiovascular death for the CVD analyses and death other than death from CAD for the CAD analyses. In the CVD and CAD analyses, patients were also censored at time of diagnosis of breast cancer recurrence or other cancers, or at end of follow-up (December 31, 2017). For the all-cause mortality analyses, patients who did not die during follow-up were censored at the end of follow-up (December 31, 2018).
Cardiovascular disease, CAD, and all-cause mortality rates per 1000 person-years were calculated for each CAC category. Cox proportional hazards models were used to examine the association between CAC scores and fatal and nonfatal CVD, fatal and nonfatal CAD and all-cause mortality. Associations were expressed as hazard ratios (HRs) with 95% CIs. Models were stepwise adjusted for age at CT scan, calendar year of CT scan (ie, before 2012 vs 2012 and later), left-sided vs right-sided radiotherapy, treated with or without anthracyclines (ie, no chemotherapy, chemotherapy without anthracyclines, or type of chemotherapy unknown), and treated with trastuzumab (yes vs no). The proportional hazards assumption was assessed using visual inspection of Kaplan-Meier curves and Schoenfeld residuals for calendar year of CT scan, radiotherapy, chemotherapy with anthracyclines, and trastuzumab. Because the proportional hazards assumption was not met for calendar year of CT scan, Cox proportional hazards models were stratified by calendar year. To test the linearity assumption, Martingale residuals against age at CT scan were plotted. Because of a nonlinear association between age and mortality, natural splines with 3 knots were included in the all-cause mortality model.
The association between CAC and CVD was examined for patients with left-sided vs right-sided breast cancer, patients irradiated with vs without boost, and patients treated with vs without anthracyclines. The number of patients treated with trastuzumab was too small for subgroup analysis. Tests for interaction were performed by comparing models with an interaction term of CAC with covariates to the model without the interaction term using the likelihood ratio test. Also, subgroup analyses in patients with a planning CT scan after 2010 were performed (more complete outcome data). Lastly, we included CAC as continuous variable using log(CAC+1) due to the skewed distribution.
Treatment of new cancers or recurrence may change the probability of developing CVD. Also, death other than from CVD precludes the occurrence of CVD. To assess the effect of these competing events, sensitivity analyses were conducted comprising competing risk survival analysis.22 New cancers, recurrences and/or all-cause mortality (excluding death from CVD) were considered as competing risks. Results were presented as subdistribution hazard ratios (sHR) with 95% CIs and represent the instantaneous CVD risk in patients who had not yet experienced the event. Lastly, subgroup analyses into the association between CAC and CVD were performed in patients with and without preexisting CVD (hospitalization). Statistical analyses were conducted in SPSS statistical software (version 25; IBM, Inc) and R Statistical Software (version 3.6.2., R Foundation).
Results
Between 2005 and 2016, we identified 18 316 patients with 22 477 planning CT scans. After deduplication, linkage with the NCR and Statistics Netherlands, and excluding ineligible patients, 15 915 patients were available for analysis. Mean age at CT scan was 59.0 years (Table 1). A total of 11 179 (70.2%) patients had no CAC, 10% (n = 1584), 11.5% (n = 1825), 5.2% (n = 830), and 3.1% (n = 497) had CAC scores of 1 to 10, 11 to 100, 101 to 400, and greater than 400, respectively. Patients with higher CAC scores were on average older compared with patients without CAC.
Table 1. Baseline Characteristics of the Dutch Multicenter Cohort of 15 919 Patients Receiving Radiotherapy for Breast Cancer Between 2005 and 2016.
| Characteristic | Total | CAC score [Agatston units], No. (%) | ||||
|---|---|---|---|---|---|---|
| 0 | 1-10 | 11-100 | 101-400 | >400 | ||
| No. (%) | 15 915 | 11 179 (70.2) | 1584 (10.0) | 1825 (11.5) | 830 (5.2) | 497 (3.1) |
| Female sex | 15 879 (99.8) | |||||
| Age, mean (SD) | 59.0 (11.2) | 56.1 (10.4) | 62.4 (10.4) | 65.8 (9.5) | 69.5 (8.2) | 71.0 (7.9) |
| Follow-up time, median (IQR), moa | 51.2 (27.9-81.1) | 53.0 (29.4-81.7) | 54.3 (28.4-88.2) | 49.2 (27.3-82.4) | 43.8 (22.8-67.3) | 34.9 (19.2-61.5) |
| Menopausal status | ||||||
| Premenopausal | 1848 (12) | |||||
| Perimenopausal | 427 (3) | |||||
| Postmenopausalb | 5686 (36) | |||||
| Unknown | 7954 (50) | |||||
| Pathologic tumor stage | ||||||
| DCIS/T0 | 2152 (13.5) | 1595 (14.3) | 200 (12.6) | 216 (11.8) | 92 (11.1) | 49 (9.9) |
| T1 | 9540 (59.9) | 6561 (58.7) | 1010 (63.8) | 1157 (63.4) | 507 (61.0) | 305 (61.4) |
| T2 | 3436 (21.6) | 2456 (22.0) | 302 (19.1) | 379 (20.8) | 189 (22.8) | 110 (22.1) |
| ≥T3 | 567 (3.6) | 401 (3.6) | 50 (3.2) | 55 (3.0) | 31 (3.7) | 30 (6.0) |
| Unknown | 220 (1.4) | 166 (1.5) | 22 (1.4) | 18 (1.0) | 11 (1.3) | 3 (0.6) |
| Pathologic nodes stage | ||||||
| N0 | 10 760 (67.6) | 7471 (66.8) | 1080 (68.2) | 1267 (69.4) | 594 (71.6) | 348 (70.0) |
| N1m | 986 (6.2) | 700 (6.3) | 101 (6.4) | 109 (6.0) | 48 (5.8) | 28 (5.6) |
| N1 | 2369 (14.9) | 1728 (15.5) | 231 (14.6) | 247 (13.5) | 104 (12.5) | 59 (11.9) |
| N2 | 840 (5.3) | 605 (5.4) | 69 (4.4) | 96 (5.3) | 42 (5.1) | 28 (5.6) |
| N3 | 460 (2.9) | 320 (2.9) | 49 (3.1) | 53 (2.9) | 22 (2.7) | 16 (3.2) |
| Unknown | 500 (3.1) | 355 (3.2) | 54 (3.4) | 53 (2.9) | 20 (2.4) | 18 (3.6) |
| Laterality | ||||||
| Left-sidedc | 8223 (51.7) | 5780 (51.7) | 831 (52.5) | 938 (51.4) | 426 (51.4) | 248 (49.9) |
| Radiotherapy | ||||||
| Locoregional | ||||||
| With boost | 679 (4.3) | 538 (4.8) | 46 (2.9) | 62 (3.4) | 25 (3.0) | 8 (1.6) |
| Without boost | 1145 (7.2) | 785 (7.0) | 109 (6.9) | 132 (7.2) | 66 (8.0) | 53 (10.7) |
| Local | ||||||
| With boost | 4503 (28.3) | 3495 (31.3) | 362 (22.9) | 388 (21.3) | 175 (21.1) | 83 (16.7) |
| Without boost | 4179 (26.3) | 2657 (23.8) | 438 (27.7) | 556 (30.5) | 321 (38.7) | 207 (41.6) |
| Unknown | 5409 (34.0) | 3704 (33.1) | 629 (39.7) | 687 (37.6) | 243 (29.2) | 146 (29.4) |
| Chemotherapy | ||||||
| None | 9680 (60.8) | 6116 (54.7) | 1078 (58.1) | 1376 (75.4) | 675 (81.3) | 435 (87.5) |
| With anthracyclines | 4333 (27.2) | 3554 (31.8) | 325 (20.5) | 308 (16.9) | 109 (13.1) | 37 (7.4) |
| Without anthracyclines | 1119 (7.0) | 903 (8.1) | 95 (6.0) | 71 (3.9) | 32 (3.9) | 18 (3.6) |
| Type of chemotherapy unknown | 783 (4.9) | 606 (5.4) | 86 (5.4) | 70 (3.8) | 14 (1.7) | 7 (1.4) |
| Hormonal therapy | ||||||
| None | 8778 (55.1) | 6038 (54.0) | 917 (57.9) | 1050 (57.5) | 470 (56.6) | 300 (60.4) |
| Aromatase inhibitor | 592 (3.7) | 363 (3.2) | 69 (4.4) | 92 (5.0) | 50 (6.0) | 18 (3.6) |
| Tamoxifen | 4671 (29.3)d | 3442 (30.8) | 404 (35.5) | 461 (25.3) | 237 (28.6) | 127 (25.6) |
| Other or type unknown | 1877 (11.8) | 1336 (12.0) | 194 (12.2) | 222 (12.2) | 73 (8.8) | 52 (10.5) |
| Trastuzumab | ||||||
| Yes | 1257 (7.9) | 1034 (9.2) | 103 (6.5) | 75 (4.1) | 30 (3.6) | 15 (3.0) |
| Hospital admission before planning CT | ||||||
| Coronary artery disease | 517 (3.2) | 142 (1.3) | 27 (1.7) | 102 (5.6) | 81 (9.8) | 165 (33.2) |
| Heart failure | 61 (0.4) | 21 (0.2) | 6 (0.4) | 10 (0.5) | 9 (1.1) | 15 (3.0) |
| Other heart disease | 421 (2.6) | 203 (1.8) | 48 (3.0) | 78 (4.3) | 43 (5.2) | 49 (9.9) |
| Cerebrovascular disease | 198 (1.2) | 86 (0.8) | 14 (0.9) | 42 (2.3) | 27 (3.3) | 29 (5.8) |
| Disease of the arteries, arterioles and capillaries | 167 (1.0) | 56 (0.5) | 22 (1.4) | 30 (1.6) | 22 (2.5) | 38 (7.6) |
Abbreviations: CAC, coronary artery calcium; CT, computed tomography; IQR, interquartile range.
Time from radiotherapy planning CT scan until date of fatal and nonfatal cardiovascular disease or censoring (noncardiovascular disease, diagnosis of breast cancer recurrence or other cancers, or end of follow-up [December 31, 2017]).
Forty patients had chemotherapy-induced menopause.
Information about laterality was missing for 3 patients.
In combination with tamoxifen, 287 patients were also treated with aromatase inhibitor and 106 patient with other types of hormonal therapy.
Coronary Artery Calcium Levels and CVD
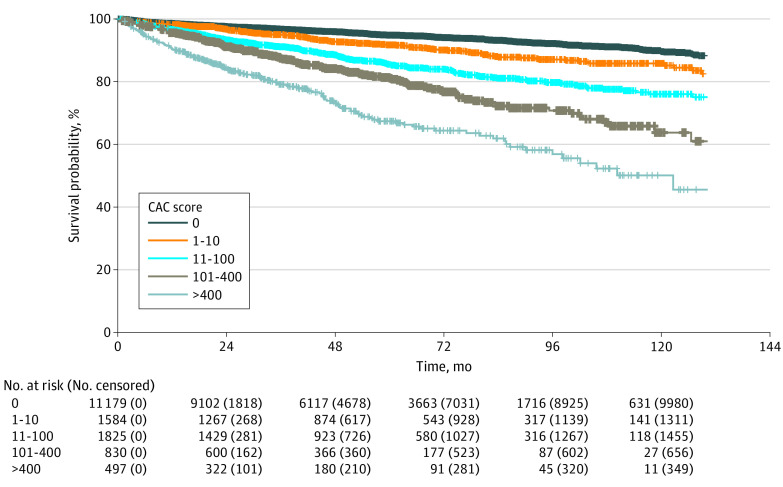
After a median follow-up time of 51.2 months (interquartile range [IQR], 27.9-81.1), 1341 (8.4%) patients were hospitalized for CVD and 113 (0.7%) patients died of CVD (eTables 2 and 3 in the Supplement). The risk of fatal and nonfatal CVD events increased with increasing CAC scores (Table 2). Five percent of the patients without CAC (n = 579/11 179) had CVD during follow-up, against 28.2% of the patients with a CAC score higher than 400 (n = 140/497) (Figure). The incidence rate of CVD increased from 10.7 per 1000 person-years in patients without CAC to 77.8 per 1000 person-years in patients with a CAC score higher than 400.
Table 2. Number and Incidence Rates of Cardiovascular Disease, Coronary Artery Disease, and Deaths by CAC Score Categorya.
| CAC score (Agatston units) | No. (%) | Cardiovascular disease | Coronary artery diseaseb | All-cause mortality | |||
|---|---|---|---|---|---|---|---|
| Events, No. (%) | Incidence rate, per 1000 person-years | Events, No. (%) | Incidence rate, per 1000 person-years | Deaths, No. (%) | Incidence rate, per 1000 person-years | ||
| 0 | 11 179 (70.2) | 579 (5.2) | 10.7 | 121 (1.1) | 2.2 | 760 (6.8) | 10.9 |
| 1-10 | 1584 (10.0) | 138 (8.7) | 17.4 | 37 (2.3) | 4.5 | 183 (11.6) | 17.7 |
| 11-100 | 1825 (11.5) | 253 (13.9) | 29.5 | 75 (4.1) | 8.3 | 222 (12.2) | 19.3 |
| 101-400 | 830 (5.2) | 148 (17.8) | 43.8 | 50 (6.0) | 13.8 | 146 (17.6) | 30.8 |
| >400 | 497 (3.1) | 140 (28.2) | 77.8 | 53 (10.7) | 26.7 | 139 (28.0) | 52.8 |
Abbreviation: CAC, coronary artery calcium.
Cardiovascular disease included all cardiovascular disease hospitalizations and death (International Statistical Classification of Diseases and Related Health Problems, Tenth Revision [ICD-10] codes I00-199, lymphedema and varicose veins excluded [I88-89 and I83-86 respectively]).
Coronary artery disease included all coronary artery disease hospitalizations and death (ICD-10 codes I20-25, including angina pectoris and myocardial infarction).
Figure. Kaplan-Meier Plot for Fatal and Nonfatal Cardiovascular Disease by Coronary Artery Calcium (CAC) Score Category.
After adjustment for age at planning CT scan, treatment and stratification for calendar year of CT scan, CAC was associated with CVD risk (Table 3). Compared with patients without CAC, patients with a CAC score of 1 to 10, 11 to 100, 101 to 400, and greater than 400 had a 1.1, 1.8, 2.1 and 3.4 higher risk of fatal and nonfatal CVD, respectively (Table 3). Results when using CAC as a continuous variable are shown in eTable 4 in the Supplement.
Table 3. Risk of Cardiovascular Disease, Coronary Artery Disease, and All-Cause Mortality by CAC Score Category.
| CAC score (Agatston units) | HR (95% CI) | |||
|---|---|---|---|---|
| Unadjusted | Model 1a | Model 2b | Model 3c | |
| Cardiovascular diseased | ||||
| 0 | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 1-10 | 1.6 (1.4-2.0) | 1.2 (1.0-1.5)e | 1.2 (1.0-1.5)e | 1.1 (0.9-1.4) |
| 11-100 | 2.7 (2.4-3.2) | 1.8 (1.5-2.1) | 1.8 (1.5-2.1) | 1.8 (1.5-2.1) |
| 101-400 | 4.1 (3.4-4.9) | 2.2 (1.8-2.7) | 2.2 (1.8-2.7) | 2.1 (1.7-2.6) |
| >400 | 7.1 (5.9-8.6) | 3.6 (2.9-4.4) | 3.6 (3.0-4.4) | 3.4 (2.8-4.2) |
| Coronary artery diseasef | ||||
| 0 | 1 [Reference] | 1 [Reference] | 1 [Reference] | |
| 1-10 | 2.1 (1.4-3.0) | 1.7 (1.2-2.5) | 1.7 (1.2-2.5) | |
| 11-100 | 3.8 (2.8-5.0) | 2.9 (2.1-3.9) | 2.8 (2.1-3.9) | |
| 101-400 | 6.3 (4.5-8.8) | 4.3 (3.0-6.2) | 4.3 (3.0-6.1) | |
| >400 | 12.2 (8.8-16.8) | 7.9 (5.5-11.3) | 7.8 (5.5-11.2) | |
| All-cause mortality | ||||
| 0 | 1 [Reference] | 1 [Reference] | 1 [Reference] | |
| 1-10 | 1.6 (1.4-1.9) | 1.3 (1.1-1.6) | 1.4 (1.2-1.7) | |
| 11-100 | 1.8 (1.5-2.0) | 1.3 (1.1-1.5) | 1.3 (1.1-1.6) | |
| 101-400 | 2.9 (2.4-3.5) | 1.7 (1.4-2.1) | 1.8 (1.5-2.2) | |
| >400 | 5.1 (4.2-6.1) | 2.7 (2.3-3.3) | 2.8 (2.3-3.4) | |
Abbreviations: CAC, coronary artery calcium; CT, computed tomography; HR, hazard ratio.
Model 1: adjusted for age at time of CT scan and stratified by calendar year of CT scan. bModel 2: adjusted for age at time of CT scan, laterality, treated with anthracyclines and treated with trastuzumab, and stratified by calendar year of CT scan.
Model 3: adjusted for age at time of CT scan, laterality, treated with anthracyclines and treated with trastuzumab, and stratified by calendar year of CT scan; model included interaction between CAC and anthracyclines. Mortality model 1 and 2: age was transformed (natural spline with df = 3).
Cardiovascular disease included all cardiovascular disease hospitalizations and death (International Statistical Classification of Diseases and Related Health Problems, Tenth Revision [ICD-10] codes I00-199, lymphedema and varicose veins excluded [I88-89 and I83-86 respectively]).
95% CI lower limit >1.0.
Coronary artery disease included all coronary artery disease hospitalizations and death (ICD-10 codes I20-25, including angina pectoris and myocardial infarction).
When treated with anthracyclines, patients with a CAC score higher than 400 had a 5.8 times higher risk (95% CI, 3.0-11.4) than patients without CAC (Table 4). In patients not treated with anthracyclines, this risk was 3.5 times higher (95% CI, 2.8-4.3). The interaction between CAC and anthracyclines was significant. We did not observed a difference in the association between patients with left-sided and right-sided breast cancer (HR>400 = 3.8; 95% CI, 2.9-5.0 and HR>400 = 3.4; 95% CI, 2.5-4.5, respectively). Patients with a CAC score of over 400 who received a radiation boost had a 6-fold increased CVD risk, while this risk was 4 times higher in patients without a radiation boost (HR>400 = 6.1; 95% CI, 3.8-9.7 and HR>400 = 3.9; 95% CI, 2.7-5.4, respectively).
Table 4. Risk of Cardiovascular Disease by CAC Score Category, Stratified by Treatmenta.
| CAC score (Agatston units) | Radiotherapy | Radiation boost | Anthracyclines | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Left-sided (n = 8223) | Right-sided (n = 7688) | Yes (n = 5182) | No (n = 5324) | Yes (n = 4333) | No (n = 11 582) | |||||||
| Incidence rate, per 1000 person-years | HR (95% CI) | Incidence rate, per 1000 person-years | HR (95% CI) | Incidence rate, per 1000 person-years | HR (95% CI) | Incidence rate, per 1000 person-years | HR (95% CI) | Incidence rate, per 1000 person-years | HR (95% CI) | Incidence rate, per 1000 person-years | HR (95% CI) | |
| 0 | 11.5 | 1 [Reference] | 9.9 | 1 [Reference] | 9.9 | 1 [Reference] | 12.6 | 1 [Reference] | 9.3 | 1 [Reference] | 11.2 | 1 [Reference] |
| 1-10 | 16.8 | 1.1 (0.9-1.4) | 18.0 | 1.4 (1.0-1.8) | 19.0 | 1.5 (0.9-2.4) | 23.6 | 1.2 (0.8-1.8) | 20.9 | 1.7 (1.1-2.7) | 16.7 | 1.1 (0.9-1.4) |
| 11-100 | 30.9 | 1.8 (1.4-2.2) | 27.9 | 1.8 (1.4-2.2) | 30.3 | 2.5 (1.7-3.7) | 35.3 | 1.9 (1.4-2.6) | 21.0 | 1.5 (1.0-2.2)b | 30.8 | 1.8 (1.5-2.1) |
| 101-400 | 41.4 | 2.0 (1.5-2.6) | 46.7 | 2.5 (1.9-3.3) | 41.6 | 2.3 (1.4-3.9) | 45.3 | 1.9 (1.3-2.8) | 53.0 | 3.1 (1.9-5.1) | 42.7 | 2.1 (1.7-2.6) |
| >400 | 89.4 | 3.8 (2.9-5.0) | 66.9 | 3.4 (2.5-4.5) | 100.2 | 6.1 (3.8-9.7) | 92.8 | 3.9 (2.7-5.4) | 110.1 | 5.8 (3.0-11.4) | 76.1 | 3.5 (2.8-4.3) |
Abbreviations: CAC, coronary artery calcium; HR, hazard ratio.
Cardiovascular disease included all cardiovascular disease hospitalizations and death (International Statistical Classification of Diseases and Related Health Problems, Tenth Revision [ICD-10] codes I00-199, lymphedema and varicose veins excluded [I88-89 and I83-86 respectively]). Models in patients who received left-sided or right-sided radiotherapy, and who were treated with and without anthracyclines were adjusted for age at time of CT scan and stratified by calendar year of CT scan. Models in patients who received radiotherapy with and without boost were adjusted for age at time of CT scan, laterality, treated with anthracyclines and treated with trastuzumab, and stratified by calendar year of CT scan; model included interaction between CAC and anthracyclines.
95% CI lower limit <1.0.
After stratification for preexisting CVD, patients with preexisting CVD had higher incidence rates of CVD compared with patients without preexisting CVD (respectively 103.7 and 58.8 per 1000 person-years in patients with a CAC score of >400) (eTables 5 and 6 in the Supplement). However, the association between CAC and CVD in patients without preexisting CVD was stronger than in patients with preexisting CVD (HR>400 = 3.2; 95% CI, 2.4-4.3 and HR>400 = 1.5; 95% CI, 1.1-2.0, respectively). Also, repeating the analysis in patients with a planning CT scan after 2010 did not change the interpretation of the results.
Coronary Artery Calcium Levels and CAD
Patients with a higher CAC score had a higher risk of CAD. Of the patient without CAC, 121 patients (1.1%) developed CAD, compared with 53 patients (10.7%) with a CAC score higher than 400 (eTable 2 in the Supplement). The incidence rate increased from 2.2 for patients without CAC to 26.7 per 1000 person-years for patients with a CAC score higher than 400 (Table 2), corresponding to an adjusted HR of 8 (95%CI, 5.5-11.2) (Table 3). The association between CAC and CAD was not different for patients with CT scans before 2012 vs 2012 and later, treated with left-sided vs right-sided radiotherapy, with or without anthracyclines (ie, interactions were not significant; eTable 7 in the Supplement). The association between CAC and CAD was stronger in patients irradiated with a boost than in those without.
Coronary Artery Calcium Levels and All-Cause Mortality
The incidence rate of all-cause mortality increased from 10.9 deaths per 1000 person-years in patients without CAC to 52.8 deaths per 1000 person-years in patients with CAC levels higher than 400 (Table 2). After adjustment, patients with a CAC score higher than 400 continued to have an increased mortality risk (HR = 2.8; 95% CI, 2.3-3.4) (Table 3). The association between CAC and all-cause mortality was not different for patients with CT scans before 2012 vs 2012 and later, treated with left-sided vs right-sided radiotherapy, when treated with vs without anthracyclines, and irradiated with vs without boost. The association between CAC and all-cause mortality was stronger in patients treated with anthracyclines compared with patients treated without (HR>400 = 4.6; 95% CI, 2.4-8.6 and HR>400 = 2.8; 95% CI, 2.2-3.4, respectively; eTable 8 in the Supplement), but test for interaction did not yield significant results.
Competing Risks
In competing risks analyses, CVD risk remained strongly associated with CAC (eTable 9; eFigure in the Supplement). Results were consistent with the results from the Cox proportional hazards analyses described above.
Discussion
Coronary artery calcium levels measured on radiotherapy planning CT scan results of patients with breast cancer were strongly associated with fatal and nonfatal CVD, especially in patients treated with anthracyclines and irradiated with a boost.23 The association between CAC and CAD was even stronger. Because patients with breast cancer planned for radiotherapy routinely undergo a planning CT scan, automated CAC scoring can be used as a fast and low-cost tool to identify patients at increased risk of CVD. Patients with an increased risk may be referred for complete CVD work up, lifestyle advice and/or initiation of cardioprotective pharmacotherapy.
In a meta-analysis including studies in general female populations, the incidence rate of CAD was 1.4 per 1000 person-years after a median follow-up of 7.0 to 11.6 years.12 In this study, the incidence rate of CAD was 2.2 after a median follow-up of 4.3 years. The higher risk of CAD in this breast cancer population may be explained by the fact that patients with breast cancer have been exposed to cardiotoxic cancer treatments, which are known to increase the risk of CAD, especially in patients with preexisting CVD risk factors.
These results are in line with a Dutch study13 including 939 patients with breast cancer (mean age, 58.4 years). The proportion of patients with CAC (manually quantified on radiotherapy planning CT) was lower than in our cohort (21.1% and 29.8%, respectively). Breast cancer patients with a CAC score of 100 or higher had a 5-times higher risk of acute coronary events compared with patients without CAC.
Limitations
The association of CAC with CVD and CAD was similar in patients treated with left-sided and right-sided radiotherapy. Previous studies have shown that left-sided radiotherapy increases the risk of CVD stronger than right-sided radiotherapy, and this risk increases with time since diagnosis.8,24 Our median follow-up of 51.2 months (ie, 4.3 years) may be too short to draw conclusions on a potential interaction between CAC and left-sided vs right-sided radiotherapy. Because of increased awareness of the potential damage of radiation dose to the heart and the introduction of the deep inspiration breath-hold technique in left-sided radiotherapy around 2010, the dose to the heart has been reduced and may have reduced the risk of CVD over years.25,26,27 Unfortunately, only irradiated patients were included in the study and therefore, we were not able to compare the risk of CVD in patients who received radiotherapy with patients who did not.
Completeness of the registry on hospital admissions varied over the years. Not all hospital admissions were registered, and missing hospitalizations increased from 10.5% in 2006 to 25% in 2013. From 2014 onward, around 90% of all hospital admissions were covered. As such, the absolute risk of hospitalization was underestimated. However, since the probability of incomplete data on hospitalization was most likely nondifferential (ie, similar for patients with low and high CAC scores), the association between CAC and CVD events is unlikely to be distorted. Until 2011, linkage was based on sex, date of birth, and postal code and the combination of variables was not unique. Therefore, 3% of the hospital admissions could not be uniquely linked to 1 person and these patients had to be excluded. In addition, until 2015, CVD events that required hospitalization for 4 hours or longer without overnight stay were not registered as hospitalization, which may have resulted in an underestimation of CVD incidence.
Information on traditional CVD risk factors such as smoking, body mass index, low physical activity, and family history of CVD was lacking. In a previous study, we demonstrated that 28% of the patients with breast cancer with CAC scores higher than 100, had no other traditional CVD risk factors.28 Based on traditional risk factors, these patients would not have been identified as high-risk patients. This implies that CAC scoring may be of added value for the screening of patients at increased risk of CVD.
Given the strong association between automatically measured CAC on radiotherapy planning CT scans and the risk of CVD in patients with breast cancer, future research should focus on whether and how to implement CAC quantification in clinical practice. Until now, there is no evidence indicating that measuring CAC, and taking action in case of increased risk, improves patient outcomes. We do not know whether cardiovascular evaluation, followed by lifestyle or pharmaceutical interventions, reduces the risk of (death from) CVD. Neither do we know whether in patients with high CAC scores, the benefits of treatment deescalation (eg, changing radiotherapy technique or comprising target volumes, or chemotherapy dose reduction) outweigh the risks (impaired tumor control).
Conclusions
To conclude, the presence and extent of CAC, as automatically quantified on routinely performed radiotherapy planning CT scans, is strongly associated with CVD and allows identification of patients at increased risk of CVD. Timely and accurate identification of high-risk patients might allow mitigation of cardiovascular risk, including management of CVD risk factors and switching to less cardiotoxic treatment regimens.
eMethods. Coronary artery calcium scoring
eTable 1. ICD-10 codes used to identify patients that experienced a cardiovascular event
eTable 2. Number of hospitalizations of cardiovascular disease and deaths by CAC score category during a median follow-up of 4.3 years
eTable 3. Number of hospitalizations for other heart diseases (I30-49, I51) during a median follow-up of 4.3 years
eTable 4. Risk of cardiovascular disease by log(CAC+1)
eTable 5. Risk of coronary artery disease by CAC score category, stratified by treatment
eTable 6. Risk of all-cause mortality by CAC score category, stratified by treatment (follow-up until 2018)
eTable 7. Number of hospitalizations of cardiovascular disease and deaths by CAC score category in patients without and with CVD hospitalization before the radiotherapy planning CT scan
eTable 8. Risk of cardiovascular disease by CAC score category in patients without known cardiovascular disease before the radiotherapy planning CT scan
eTable 9. Competing risks survival analysis of cardiovascular disease by CAC category
eFigure 1. Cumulative incidence curves for CVD by CAC category in the presence of competing risks (Aalen-Johansen estimates and 95% intervals
References
- 1.Armenian SH, Lacchetti C, Barac A, et al. Prevention and monitoring of cardiac dysfunction in survivors of adult cancers: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol. 2017;35(8):893-911. doi: 10.1200/JCO.2016.70.5400 [DOI] [PubMed] [Google Scholar]
- 2.Sturgeon KM, Deng L, Bluethmann SM, et al. A population-based study of cardiovascular disease mortality risk in US cancer patients. Eur Heart J. 2019;40(48):3889-3897. doi: 10.1093/eurheartj/ehz766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bradshaw PT, Stevens J, Khankari N, Teitelbaum SL, Neugut AI, Gammon MD. Cardiovascular disease mortality among breast cancer survivors. Epidemiology. 2016;27(1):6-13. doi: 10.1097/EDE.0000000000000394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patnaik JL, Byers T, DiGuiseppi C, Dabelea D, Denberg TD. Cardiovascular disease competes with breast cancer as the leading cause of death for older females diagnosed with breast cancer: a retrospective cohort study. Breast Cancer Res. 2011;13(3):R64. doi: 10.1186/bcr2901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boekel NB, Jacobse JN, Schaapveld M, et al. Cardiovascular disease incidence after internal mammary chain irradiation and anthracycline-based chemotherapy for breast cancer. Br J Cancer. 2018;119(4):408-418. doi: 10.1038/s41416-018-0159-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Naaktgeboren WR, Linschoten M, de Graeff A, et al. Long-term cardiovascular health in adult cancer survivors. Maturitas. 2017;105:37-45. doi: 10.1016/j.maturitas.2017.05.014 [DOI] [PubMed] [Google Scholar]
- 7.Smith LA, Cornelius VR, Plummer CJ, et al. Cardiotoxicity of anthracycline agents for the treatment of cancer: systematic review and meta-analysis of randomised controlled trials. BMC Cancer. 2010;10:337. doi: 10.1186/1471-2407-10-337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cheng YJ, Nie XY, Ji CC, et al. Long-term cardiovascular risk after radiotherapy in women with breast cancer. J Am Heart Assoc. 2017;6(5):e005633. doi: 10.1161/JAHA.117.005633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hooning MJ, Botma A, Aleman BM, et al. Long-term risk of cardiovascular disease in 10-year survivors of breast cancer. J Natl Cancer Inst. 2007;99(5):365-375. doi: 10.1093/jnci/djk064 [DOI] [PubMed] [Google Scholar]
- 10.Hershman DL, Till C, Shen S, et al. Association of cardiovascular risk factors with cardiac events and survival outcomes among patients with breast cancer enrolled in SWOG clinical trials. J Clin Oncol. 2018;36(26):2710-2717. doi: 10.1200/JCO.2017.77.4414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Greenland P, Blaha MJ, Budoff MJ, Erbel R, Watson KE. Coronary calcium score and cardiovascular risk. J Am Coll Cardiol. 2018;72(4):434-447. doi: 10.1016/j.jacc.2018.05.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kavousi M, Desai CS, Ayers C, et al. Prevalence and prognostic implications of coronary artery calcification in low-risk women: a meta-analysis. JAMA. 2016;316(20):2126-2134. doi: 10.1001/jama.2016.17020 [DOI] [PubMed] [Google Scholar]
- 13.Roos CTG, van den Bogaard VAB, Greuter MJW, et al. Is the coronary artery calcium score associated with acute coronary events in breast cancer patients treated with radiotherapy? Radiother Oncol. 2018;126(1):170-176. doi: 10.1016/j.radonc.2017.10.009 [DOI] [PubMed] [Google Scholar]
- 14.van Velzen SGM, Lessmann N, Velthuis BK, et al. Deep learning for automatic calcium scoring in CT: validation using multiple cardiac CT and chest CT protocols. Radiology. 2020;295(1):66-79. doi: 10.1148/radiol.2020191621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lessmann N, van Ginneken B, Zreik M, et al. Automatic calcium scoring in low-dose chest CT using deep neural networks with dilated convolutions. IEEE Trans Med Imaging. 2018;37(2):615-625. doi: 10.1109/TMI.2017.2769839 [DOI] [PubMed] [Google Scholar]
- 16.Emaus MJ, Išgum I, van Velzen SGM, et al. ; Bragatston study group . Bragatston study protocol: a multicentre cohort study on automated quantification of cardiovascular calcifications on radiotherapy planning CT scans for cardiovascular risk prediction in patients with breast cancer. BMJ Open. 2019;9(7):e028752. doi: 10.1136/bmjopen-2018-028752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gernaat SAM, van Velzen SGM, Koh V, et al. Automatic quantification of calcifications in the coronary arteries and thoracic aorta on radiotherapy planning CT scans of Western and Asian breast cancer patients. Radiother Oncol. 2018;127(3):487-492. doi: 10.1016/j.radonc.2018.04.011 [DOI] [PubMed] [Google Scholar]
- 18.Netherlands Comprehensive Cancer Organisation . Accesseed November 16, 2018. https://www.iknl.nl.
- 19.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15(4):827-832. doi: 10.1016/0735-1097(90)90282-T [DOI] [PubMed] [Google Scholar]
- 20.World Health Organisation . International Statistical Classification of Diseases, Injuries and Related Health Problems. Tenth Revision. Geneva: World Health Organisation; 1992. [Google Scholar]
- 21.Collaborating Centre voor de WHO-Familie van Internationale Classificaties NL . Conversie CVZ'80 - ICD-10 2006. Accessed April 2020. https://www.whofic.nl/downloads-en-links/icd-10
- 22.Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94:496-509. doi: 10.1080/01621459.1999.10474144 [DOI] [Google Scholar]
- 23.Cai F, Luis MAF, Lin X, et al. Anthracycline-induced cardiotoxicity in the chemotherapy treatment of breast cancer: Preventive strategies and treatment. Mol Clin Oncol. 2019;11(1):15-23. doi: 10.3892/mco.2019.1854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Darby SC, Ewertz M, McGale P, et al. Risk of ischemic heart disease in women after radiotherapy for breast cancer. N Engl J Med. 2013;368(11):987-998. doi: 10.1056/NEJMoa1209825 [DOI] [PubMed] [Google Scholar]
- 25.Mast ME, Pekelharing JF, Heijenbrok MW, et al. Reduced increase of calcium scores using breath-hold in left-sided whole breast irradiation. Radiother Oncol. 2020;149:78-83. doi: 10.1016/j.radonc.2020.05.001 [DOI] [PubMed] [Google Scholar]
- 26.Simonetto C, Eidemüller M, Gaasch A, et al. Does deep inspiration breath-hold prolong life? Individual risk estimates of ischaemic heart disease after breast cancer radiotherapy. Radiother Oncol. 2019;131:202-207. doi: 10.1016/j.radonc.2018.07.024 [DOI] [PubMed] [Google Scholar]
- 27.Taylor C, McGale P, Brønnum D, et al. Cardiac structure injury after radiotherapy for breast cancer: cross-sectional study with individual patient data. J Clin Oncol. 2018;36(22):2288-2296. doi: 10.1200/JCO.2017.77.6351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gernaat SA, Išgum I, de Vos BD, et al. Automatic coronary artery calcium scoring on radiotherapy planning CT scans of breast cancer patients: reproducibility and association with traditional cardiovascular risk factors. PLoS One. 2016;11(12):e0167925. doi: 10.1371/journal.pone.0167925 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Coronary artery calcium scoring
eTable 1. ICD-10 codes used to identify patients that experienced a cardiovascular event
eTable 2. Number of hospitalizations of cardiovascular disease and deaths by CAC score category during a median follow-up of 4.3 years
eTable 3. Number of hospitalizations for other heart diseases (I30-49, I51) during a median follow-up of 4.3 years
eTable 4. Risk of cardiovascular disease by log(CAC+1)
eTable 5. Risk of coronary artery disease by CAC score category, stratified by treatment
eTable 6. Risk of all-cause mortality by CAC score category, stratified by treatment (follow-up until 2018)
eTable 7. Number of hospitalizations of cardiovascular disease and deaths by CAC score category in patients without and with CVD hospitalization before the radiotherapy planning CT scan
eTable 8. Risk of cardiovascular disease by CAC score category in patients without known cardiovascular disease before the radiotherapy planning CT scan
eTable 9. Competing risks survival analysis of cardiovascular disease by CAC category
eFigure 1. Cumulative incidence curves for CVD by CAC category in the presence of competing risks (Aalen-Johansen estimates and 95% intervals