Summary
Primary Epstein-Barr virus (EBV) infection may present with self-limiting abdominal involvement, characterized by hepatitis with mild elevation of aminotransferases, splenomegaly, and rarely with acute acalculous cholecystitis (AAC). Usually, treatment of EBV related AAC is symptomatic, without the need for surgery. Here, we describe a severe case of AAC occurring as the first manifestation of infectious mononucleosis in a young adult woman, receiving treatment with interleukin 6 receptor (IL-6r) inhibitor for rheumatoid arthritis (RA); moreover, we have performed a review of the literature on EBV-related AAC.
Keywords: EBV, Acute acalculous cholecystitis, Iimmunosuppressed patient, Cholecystitis, Hepatitis
Introduction
Epstein-Barr virus (EBV), a double-stranded DNA virus with a genome of about 172 kilobases, belonging to the Herpesviridae family, is one of the most common life-long viral infection, with almost 95% of the human population being infected [1]. In particular, EBV is classified within the gamma-herpesviruses subfamily, and is the prototype of the Lymphocrypto-virus genus, with its formal designation of human herpesvirus 4 (HHV-4) [1]. EBV was the first isolated human tumour virus, identified in 1964 in a cell line derived from Burkitt lymphoma [1]. After infection, EBV resides persistently in memory B-cells and is usually transmitted through saliva to and between young children, often from asymptomatic individuals [1, 2]. EBV displays a broad range of clinical pictures, from asymptomatic infection (especially during childhood) to benign infectious mononucleosis, to EBV-related lymphoma, EBV-related epithelial cancers, and post-transplant lymphoproliferative disease (PTLD) due to virus-induced persistent cell activation [1-3]. Infectious mononucleosis, when symptomatic, is a self-limiting disease occurring after an incubation period of four to seven weeks [3, 4]. Clinical manifestations may include fever, pharyngitis, malaise or fatigue, and diffuse lymphadenopathy. The most common presenting symptoms are the triad of subacute pharyngitis, high-grade fever and lymphadenopathy [4]. Self-limiting abdominal involvement, characterized by hepatitis with mild elevation of aminotransferases and splenomegaly, is also frequently reported [4, 5]. Acute acalculous cholecystitis (AAC), defined as the inflammation of the gallbladder in the absence of gallstones, is usually described in critically ill patients due to major trauma and/or infections [5]. In a few cases reported in the literature, AAC has been associated with primary EBV infection in both children and adults [6]. Here, we describe a severe case of AAC occurring as the first manifestation of infectious mononucleosis in a young woman receiving treatment with interleukin 6 receptor (IL-6r) inhibitor for rheumatoid arthritis (RA); moreover, we performed a review of the literature on EBV-related AAC.
Case report
A 24-years-old woman presented to the Emergency Department of IRCCS Sacro Cuore Don Calabria Hospital, Verona, Italy, in August 2020 complaining of low-grade fever, abdominal pain, nausea, and jaundice. She suffered from juvenile rheumatoid arthritis (diagnosed at the age of 8 months) in treatment since 2013 with tocilizumab 162 mg subcutaneously once a week (last administration one week before admission), without any hepatic side-effects reported, and methotrexate, since 2010, 10 mg once a week (discontinued 6 weeks before admission). In July 2020 she underwent right hip arthroplasty due to arthritis.
On admission to our hospital, an abdominal ultrasonography showed diffuse, severe thickening of the gallbladder’s walls with multi-layered appearance, associated with pericholecystic fluid, suggesting AAC (Fig. 1A). Splenomegaly (bipolar diameter 15 cm; normal value < 13 cm) was also reported.
Fig. 1.
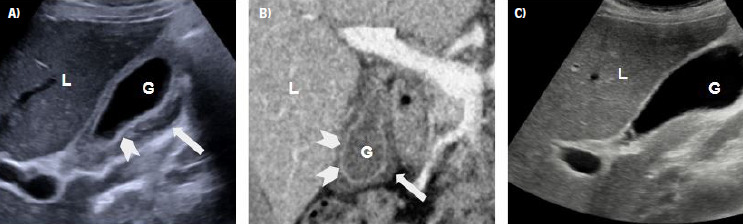
Ultrasound and CT scan images of EBV-related AAC. A) US b-mode, day 1: gallbladder distention and thickened wall > 3 mm (arrowhead), pericholecystic fluid (arrow); B) Contrast Enhanched CT, venous phase, day 2, mucosal hyperenhancement (arrowheads), pericholecystic fluid and inflammatory fat stranding (arrow); C) A) US b-mode, day 7, after terapy: gallbladder with regular wall, no more pericholecystic fluid visible (G: gallbladder lumen; L: liver).
Blood examination showed lymphocytosis (70% of the total white blood cell count) with activated lymphocytes, hypertransaminasemia (AST 919 U/L and ALT 914 U/L; normal values < 50 U/L), and hyperbilirubinemia (total bilirubin 4.4 mg/dL, normal values 0.3-1 mg/dl; direct bilirubin 3 mg/dL, normal values 0-0.3 mg/dl). C-reactive protein was slightly increased (42 mg/dL; normal value < 5 mg/dL), while procalcitonin was negative. Major hepatitis virus tests (HAV, HBV, HCV) as well as serum B-D-glucan, to exclude opportunistic fungal infection, were negative. Stool culture, to investigate for salmonellosis, was also negative.
To cover empirically for bacterial cholecystitis, antibiotic therapy with piperacillin/tazobactam 4/0.5 g every 8 hours was started.
In the following three days, symptoms persisted despite fasting, antibiotic therapy and intravenous hydration. A computed tomography (CT) scan of the abdomen confirmed the ultrasound picture: a distended gallbladder with wall thickening, increased enhancement following administration of iodinated contrast medium, and no visible gallstones (Fig. 1B). The need for urgent cholecystectomy was discarded after surgical consultation, which suggested elective surgery depending on the clinical development.
Testing for minor hepatitis viruses revealed a negative serology for cytomegalovirus but positive serology for EBV, with an immunological profile characterized by positive anti-VCA IgM and anti-VCA IgG, negative anti-EBNA IgG, indicating acute infection.
Upon diagnosis of EBV infection, antibiotic therapy was discontinued. After 72 hours from admission, the patient improved spontaneously, with resolution of abdominal pain, normalization of liver function tests, and progressively resumed feeding.
Abdominal ultrasound before discharge showed resolution of the gallbladder walls’ thickening (Fig. 1C). The patient was discharged after 7 days from admission in good clinical condition and with no symptoms left.
Literature review
On 30 September 2020 we performed a MEDLINE/PubMed search using the following query ((EBV)OR(Epstein-Barr)OR(infective mononucleosis)) AND ((Cholecystitis)OR(gallbladder))”. No restrictions were applied regarding publication date or language; only original papers describing cases of human AAC caused by serology-confirmed EBV were included. Data regarding the number of patients, age (children or adults aged older than 18 ), immune status (immunocompetent or immunocompromised), and treatment were recorded.
Out of the 100 papers retrieved, 45 were excluded by title/abstract screening. The full-text of the remaining 55 papers was retrieved, the content examined for eligibility, and the references lists examined to individuate further potentially eligible papers. Eventually, data were extracted from the finally eligible 57 papers.
Details of the eligible papers are shown in Table I (review containing multiple case reports were reported excluding papers with the single case). Since 1987, the first reported case in an adult immunocompetent female patient by Hammond [7], 70 cases were retrieved, of whom 52 (74,2%) in females and 18 (25,8%) in males. Forty-four (62.8%) patients were children (3-18 years old), while 26 (37.2%) patients were adults. Immune status was available in 55 cases (78.5%), of which 4 (7.2%) were immunocompromised: 1 patient with previous major surgery (left adrenal gland resection, distal pancreatectomy, and splenectomy due to a large pheochromocytoma), 1 with seronegative spondyloartropathy in treatment with disease-modifying antirheumatic drugs (DMARDs), 1 with ulcerative colitis in treatment with azathioprine, and 1 patient with end-stage renal disease. Surgical management with colecistectomy was reported in 2 (2.8%) cases, of whom 1 was immunocompromised.
Tab. I.
Review of the published EBV case report.
| Author (year) | Number of patient | Immunecompromised/immunecompetent | Adult/child | Sex | Surgical treatment |
|---|---|---|---|---|---|
| Langenohl et al. (2020) [8] | 1 | Immunecompetent | Child | M | No |
| Guri et al. (2020) [9] | 1 | Immunecompetent | Child | F | No |
| Ntelis et al. (2020) [10] | 1 | Immunecompetent | Child | F | No |
| Lamprianidis et al. (2020) [11] | 1 | Immunecompetent | Adult | F | No |
| Young et al. (2019) [12] | 1 | Immunecompetent | Child | F | No |
| Mazur-Melewska et al. (2019) [13] | 15 | Not available | Child | 9 M/ 6 F | No |
| Rezkallah et al. (2018) [14] | 1 | Immunecompetent | Adult | F | Laparoscopic cholecystectomy |
| Höhn et al. (2018) [15] | 1 | Previous major surgery | Adult | M | No |
| Cameron et al. (2018) [16] | 1 | Immunecompetent | Adult | F | No |
| Yesilbag et al. (2017) [17] | 1 | Immunecompetent | Adult | F | No |
| Rodà et al. (2017) [18] | 1 | Immunecompetent | Child | M | No |
| Khoury et al. (2017) [19] | 1 | Immunecompetent | Adult | M | No |
| Sheybani et al. (2016) [20] | 1 | Seronegative spondyloarthropathy | Adult | F | No |
| Ono et al. (2016) [21] | 1 | Immunecompetent | Adult | F | No |
| Majdalani et al. (2016) [22] | 1 | Immunecompetent | Child | F | No |
| Koufakis et al. (2016) [23] | 1 | Immunecompetent | Adult | M | No |
| Branco et al. (2015) [24] | 1 | Immunecompetent | Child | F | No |
| Hernández-Rodríguez J et al. (2014) [25] | 1 | Immunecompetent | Child | F | No |
| Pawłowska-Kamieniak et al. (2015) [26] | 1 | Immunecompetent | Child | F | No |
| Alkhoury et al. (2015) [27] | 1 | Immunecompetent | Child | F | No |
| Agergaard et al. (2015) [28] | 1 | Immunecompetent | Adult | F | No |
| Suga et al. (2014) [29] | 1 | Immunecompetent | Child | F | No |
| Gagneux-Brunon et al. (2014) [30] | 2 | Immunecompetent | Adult | 2F | No |
| Celik et al. (2014) [31] | 1 | Immunecompetent | Adult | F | No |
| Fretzayas et al. (2014) [32] | 2 | Immunecompetent | Child | 2F | No |
| Strehle et al. (2014) [33] | 1 | Immunecompetent | Child | F | No |
| Kim et al. (2014) [34] | 1 | Immunecompetent | Child | F | No |
| Hamdy et al. (2014) [35] | 1 | Immunecompetent | Child | F | No |
| Poddighe et al. (2014) [36] | 1 | Immunecompetent | Child | F | No |
| Teke et al. (2013) [37] | 1 | Immunecompetent | Child | F | No |
| Beltrame et al. (2012) [38] | 1 | Immunecompetent | Adult | F | No |
| Dylewski et al. (2012) [39] | 1 | Immunecompetent | Adult | F | No |
| Carrascosa et al. (2012) [40] | 1 | Immunecompetent | Adult | F | No |
| Nagdev and Ward (2011) [41] | 1 | Immunecompetent | Adult | F | No |
| Arya et al. (2010) [42] | 1 | Immunecompetent | Child | F | No |
| Yang et al. (2010) [43] | 1 | Immunecompetent | Adult | F | No |
| Attilakos et al. (2009) [44] | 2 | Immunecompetent | Child | 1 F /1 M | No |
| Hagel et al. (2009) [45] | 1 | Immunecompromised (ulcerative colitis) | Adult | F | Laparoscopic cholecystectomy |
| Cholongitas et al. (2009) [46] | 1 | Immunecompetent | Adult | F | No |
| Chalupa et al. (2009) [47] | 1 | Immunecompetent | Adult | F | No |
| Iaria et al. (2008) [48] | 1 | Immunecompetent | Adult | F | No |
| Pelliccia et al. (2008) [49] | 1 | Immunecompetent | Child | F | No |
| Koch et al. (2007) [50] | 1 | Immunecompetent | Adult | F | No |
| Prassouli et al. (2007) [51] | 1 | Immunecompetent | Child | F | No |
| Lagona et al. (2007) [52] | 1 | Immunecompetent | Child | F | No |
| Yoshie et al. (2004) [53] | 1 | Immunecompetent | Child | F | No |
| O’Donovan et al. (1996) [54] | 2 | Immunecompetent | Adult | 1 F/ 1 M | No |
| Maruyama et al. (1994) [55] | 2 | Immunecompetent | Child | 1 F /1 M | No |
| Sainsbury et al. (1994) [56] | 1 | Immunocompromised (end-stage renal disease) | Child | M | No |
| Sung et al. (1989) [57] | 1 | Immunecompetent | Child | F | No |
| Hammond et al. (1987) [7] | 1 | Immunecompetent | Adult | F | No |
Discussion
Acute acalculous cholecystitis contributes to 5-10% of all cholecystitis in adults and it is usually observed in patients with viral hepatitis, salmonellosis, major trauma, extensive burns, long term parenteral nutrition, critically ill patients and systemic diseases such as diabetes, malignancies, abdominal vasculitis, congestive heart failure, cholesterol embolization, and shock [6, 58]. EBV is a relatively rare cause of AAC; to the best of our knowledge, 4 patients with immunocompromised conditions and EBV-related AAC have been reported in the literature (Tab. I). It should be noted that the AAC could be potentially related to the acute hepatitis induced by EBV or to immunesuppressive agents. Our patient did not need any supplementary treatment or treatment adjustment (e.g. reduction of the immunosuppressive treatment) or surgical intervention, being only supporting treatment apparently of benefit, as highlighted in previous reports [59]. Moreover, in our case report, a mild case of EBV hepatitis with transient elevation of serum aminotransferases and jaundice has been noted, while it is occasionally reported in the literature (in 5% of cases), possibly caused by cholestasis or virus-induced haemolysis [60].
EBV-related AAC should be suspected when no other cause of AAC can could be identified, especially in young patients, who seem to be more prone to its development, and its diagnosis is suspectable in order to avoid unnecessary antibiotic treatment or more invasive and costly procedures [60] (Tab. I).
Likewise, if an EBV first-infection displays clinical symptoms compatible with cholecystitis, ultrasonographic examination should be performed in order to confirm or rule out the diagnosis of ACC [13, 38].
Conclusions
EBV primary infection can lead to acute acalculous cholecystitis, especially in adult immunocompromised patients: clinical suspicion, coupled with ultrasound of the gallbladder are needed for a correct and timely diagnosis. Conversely, when ultrasound of the gallbladder shows evidence of AAC, with coherent clinical presentation, EBV infection should be considered and serological test for EBV should be performed.
Figures and tables
Acknowledgements
Funding sources: this research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Conflicts of interest statement
The authors declare no conflict of interest.
Authors’ contributions
SR, SS, NR, MS took care of the patient, draft and approved the final version of the manuscript.
EO acquired radiological images, gave radiological consultation and approved the final version of the manuscript. FT, PB, MM and AF draft, reviewed and approved the final version of the manuscript.
References
- [1].IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Biological agents. Lyon (FR): International Agency for Research on Cancer 2012. Available from: https://www.ncbi.nlm.nih.gov/books/NBK304353
- [2].Macsween KF, Crawford DH. Epstein-Barr virus-recent advances. Lancet Infect Dis 2003;3:131-40. https://doi.org/10.1016/s1473-3099(03)00543-7 10.1016/s1473-3099(03)00543-7 [DOI] [PubMed] [Google Scholar]
- [3].Fugl A, Andersen CL. Epstein-Barr virus and its association with disease - a review of relevance to general practice. BMC Fam Pract 2019;20:62. https://doi.org/10.1186/s12875-019-0954-3 10.1186/s12875-019-0954-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Luzuriaga K, Sullivan JL. Infectious mononucleosis. N Engl J Med 2010;362:1993-2000. https://doi.org/10.1056/NEJMcp1001116 10.1056/NEJMcp1001116 [DOI] [PubMed] [Google Scholar]
- [5].Dunmire SK, Verghese PS, Balfour HH, Jr. Primary Epstein-Barr virus infection. J Clin Virol 2018;102:84-92. https://doi.org/10.1016/j.jcv.2018.03.001 10.1016/j.jcv.2018.03.001 [DOI] [PubMed] [Google Scholar]
- [6].Chen C-J, Huang F-C, Tiao M-M, Huang Y-H, Lin L-Y, Yu H-R, Yang KD, Huang Y-C, Chen C-C, Chang W-C, Kuo H. Sonographic gallbladder abnormality is associated with intravenous immunoglobulin resistance in Kawasaki disease. ScientificWorldJournal 2012;2012:485758 https://doi.org/10.1100/2012/485758.485758 10.1100/2012/485758.485758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Hammond DI, MacLean RS. Gallbladder wall thickening in an elderly woman with infectious mononucleosis. J Clin Ultrasound 1987;15:558-60. https://doi.org/10.1002/jcu.1870150811 10.1002/jcu.1870150811 [DOI] [PubMed] [Google Scholar]
- [8].Langenohl R, Young S, Couperus K. Acute acalculous cholecystitis from infection with epstein-barr virus in a previously healthy child: a case report. Clin Pract Cases Emerg Med 2020;4:393-6. https://doi.org/10.5811/cpcem.2020.4.46301 10.5811/cpcem.2020.4.46301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Guri A, Scheier E. Gallbladder wall thickening on bedside ultrasound in a child with Epstein-Barr virus infection BMJ Case Reports CP 2020;13:e234486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Ntelis K, Mazarakis D, Sapountzis A, Zissi D, Sparangi S, Xidia N, Velissaris D. Acute acalculous cholecystitis associated with epstein-barr infection: a case report and review of the literature. Case Rep Med 2020;2020:9029601. https://doi.org/10.1155/2020/9029601 10.1155/2020/9029601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Teopoulos Lamprianidis K, Easom N, Patch E, Thomas S. Acute Epstein-Barr infection presenting as cholecystitis with ascites. BMJ Case Rep 2020;13:e232562. https://doi.org/10.1136/bcr-2019-232562 10.1136/bcr-2019-232562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Young C, Lampe R. Primary Epstein-Barr Virus infection in an adolescent female complicated by acute acalculous cholecystitis. Cureus 2019;11:e5044. https://doi.org/10.7759/cureus.5044 10.7759/cureus.5044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Mazur-Melewska K, Derwich A, Mania A, Kemnitz P, Służewski W, Figlerowicz M. Epstein-Barr virus infection with acute acalculous cholecystitis in previously healthy children. Int J Clin Pract 2019;73:e13386. https://doi.org/10.1111/ijcp.13386 10.1111/ijcp.13386 [DOI] [PubMed] [Google Scholar]
- [14].Rezkallah KN, Barakat K, Farrah A, Rao S, Sharma M, Chalise S, Zdunek T. Acute Acalculous Cholecystitis due to primary acute Epstein-Barr virus infection treated with laparoscopic cholecystectomy; a case report. Ann Med Surg (Lond) 2018;35:189-91. https://doi.org/10.1016/j.amsu.2018.10.010 10.1016/j.amsu.2018.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Höhn P, Braumann C, Uhl W, Luu AM. Riddle me this: acalculous cholecystitis as an unusual complication of immunoglobulin M negative mononucleosis. Cureus 2018;10:e2505. https://doi.org/10.7759/cureus.2505 10.7759/cureus.2505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Cameron A, Akilan K, Carr D. Infectious mononucleosis - not always a benign condition: a case report of infectious mononucleosis-associated acute acalculous cholecystitis. CJEM 2019;21:154-6. https://doi.org/10.1017/cem.2018.15 10.1017/cem.2018.15 [DOI] [PubMed] [Google Scholar]
- [17].Yesilbag Z, Karadeniz A, Kaya FO. Acute acalculous cholecystitis: a rare presentation of primary Epstein-Barr Virus infection in adults-case report and review of the literature. Case Rep Infect Dis 2017;2017:5790102. https://doi.org/10.1155/2017/5790102 10.1155/2017/5790102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Rodà D, Huici M, Ricart S, Vila J, Fortuny C, Alsina L. Cholecystitis and nephrotic syndrome complicating Epstein-Barr virus primary infection. Paediatr Int Child Health 2017;37:74-7. https://doi.org/10.1080/20469047.2015.1135561 10.1080/20469047.2015.1135561 [DOI] [PubMed] [Google Scholar]
- [19].Khoury A, Porté F, Haq M. Epstein Barr virus, abdominal pain, and jaundice. BMJ 2017;358:j3386. https://doi.org/10.1136/bmj.j3386 10.1136/bmj.j3386 [DOI] [PubMed] [Google Scholar]
- [20].Sheybani F, Naderi H, Erfani SS, Gharib M. A complicated course of acute viral induced pharyngitis, icteric hepatitis, acalculous cholecystitis, and skin rash. Case Reports in Medicine 2016;2016:ID 6796094. https://doi.org/10.1155/2016/6796094 10.1155/2016/6796094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Ono S, Kobayashi T, Nishio K. A case of acute acalculous cholecystitis during infectious mononucleosis caused by the Epstein-Barr Virus in a young woman. Kansenshogaku Zasshi 2016;90:330-5. https://doi.org/10.11150/kansenshogakuzasshi.90.330 10.11150/kansenshogakuzasshi.90.330 [DOI] [PubMed] [Google Scholar]
- [22].Majdalani M, Milad N, Sahli Z, Rizk S. Acute acalculous cholecystitis in a Lebanese girl with primary Epstein-Barr viral infection. BMJ Case Rep 2016;2016:10.1136/bcr-213829. https://doi.org/10.1136/bcr-2015-213829 10.1136/bcr-2015-213829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Koufakis T, Gabranis I. Another Report of acalculous cholecystitis in a Greek patient with infectious mononucleosis: a matter of luck or genetic predisposition? Case Reports Hepatol 2016;2016:6080832. https://doi.org/10.1155/2016/6080832 10.1155/2016/6080832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Branco L, Vieira M, Couto C, Coelho MD, Laranjeira C. Acute acalculouscholecystitis by Epstein-Barr Virus infection: a rare association. Infect Dis Rep 2015;7:6184. https://doi.org/10.4081/idr.2015.6184 10.4081/idr.2015.6184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Hernández-Rodríguez J, Tan CD, Rodríguez ER, Hoffman GS. Single-organ gallbladder vasculitis: characterization and distinction from systemic vasculitis involving the gallbladder. An analysis of 61 patients. Medicine (Baltimore) 2014;93:405-13. https://doi.org/10.1097/MD.0000000000000205. 10.1097/MD.0000000000000205 Erratum in: Medicine (Baltimore) 2014;93:414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Pawłowska-Kamieniak A, Mroczkowska-Juchkiewicz A, Gołyska D, Kominek K, Pac-Kozuchowska E. Acute acalculous cholecystitis in a 17-year-old girl with Epstein-Barr virus infection. Prz Gastroenterol 2015;10:54-6. https://doi.org/10.5114/pg.2015.48998 10.5114/pg.2015.48998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Alkhoury F, Diaz D, Hidalgo J. Acute acalculous cholecystitis (AAC) in the pediatric population associated with Epstein-Barr Virus (EBV) infection. Case report and review of the literature. Int J Surg Case Rep 2015;11:50-2. https://doi.org/10.1016/j.ijscr.2014.06.006 10.1016/j.ijscr.2014.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Agergaard J, Larsen CS. Acute acalculous cholecystitis in a patient with primary Epstein-Barr virus infection: a case report and literature review. Int J Infect Dis 2015;35:67-72. https://doi.org/10.1016/j.ijid.2015.04.004 10.1016/j.ijid.2015.04.004 [DOI] [PubMed] [Google Scholar]
- [29].Suga K, Shono M, Goji A, Matsuura S, Inoue M, Kawahito M, Mori K. A case of acute acalculous cholecystitis complicated by primary Epstein-Barr virus infection. J Med Invest 2014;61:426-9. https://doi.org/10.2152/jmi.61.426 10.2152/jmi.61.426 [DOI] [PubMed] [Google Scholar]
- [30].Gagneux-Brunon A, Suy F, Pouvaret A, Pillet S, Tarantino E, Bouchet D, Fresard A, Cazorla C, Guglielminotti C, Lucht F, Botelho-Nevers E. Acute acalculous cholecystitis, a rare complication of Epstein-Barr virus primary infection: report of two cases and review. J Clin Virol 2014;61:173-5. https://doi.org/10.1016/j.jcv.2014.05.019 10.1016/j.jcv.2014.05.019 [DOI] [PubMed] [Google Scholar]
- [31].Celik F, Tekin F, Yamazhan T, Gunsar F. Epstein-Barr Virüs Associated Acute Acalculous Cholecystitis. J Gastroenterol Hepatol Res 2014;3:1179-80 Available from: http://www.ghrnet.org/index.php/joghr/article/view/786 [Google Scholar]
- [32].Fretzayas A, Moustaki M, Attilakos A, Brozou T, Nicolaidou P. Acalculous cholecystitis or biliary dyskinesia for Epstein-Barr virus gallbladder involvement? Prague Med Rep 2014;115:67-72. https://doi.org/10.14712/23362936.2014.7 10.14712/23362936.2014.7 [DOI] [PubMed] [Google Scholar]
- [33].Strehle E, De Alwis Y, Saleem M. Epstein–Barr virus-associated acute cholecystitis in a teenager. Ultrasound 2014;22:123-5. https://doi.org/10.1177/1742271X13513223 10.1177/1742271X13513223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Kim A, Yang HR, Moon JS, Chang JY, Ko JS. Epstein-barr virus infection with acute acalculous cholecystitis. Pediatr Gastroenterol Hepatol Nutr 2014;17:57-60. https://doi.org/10.5223/pghn.2014.17.1.57 10.5223/pghn.2014.17.1.57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Hamdy RF, Stein RE, Larru B, Bellah RD, Grossman AB, Hodinka RL, Feemster KA. Gallbladder wall thickening in an adolescent with acute mononucleosis: a case report and brief review of the literature. J Pediatric Infect Dis Soc 2015;4:267-71. https://doi.org/10.1093/jpids/piu023 10.1093/jpids/piu023 [DOI] [PubMed] [Google Scholar]
- [36].Poddighe D, Cagnoli G, Mastricci N, Bruni P. Acute acalculous cholecystitis associated with severe EBV hepatitis in an immunocompetent child. BMJ Case Rep 2014;2014:bcr2013201166. https://doi.org/10.1136/bcr-2013-201166 10.1136/bcr-2013-201166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Aydın Teke T, Tanır G, Özel A, Timur ÖM, Ekşioğlu AS. A case of acute acalculous cholecystitis during the course of reactive Epstein-Barr virus infection. Turk J Gastroenterol 2013;24:571-2. [PubMed] [Google Scholar]
- [38].Beltrame V, Andres A, Tona F, Sperti C. Epstein-Barr virus - associated acute acalculous cholecystitis in an adult. Am J Case Rep 2012;13:153-6. https://doi.org/10.12659/AJCR.883245 10.12659/AJCR.883245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Dylewski J. Acute acalculous cholecystitis caused by Epstein-Barr virus infection. Clinical Microbiology Newsletter 2012;34:7-8. [Google Scholar]
- [40].Carrascosa MF, Caviedes JR, Soler-Dorda G, Saiz-Pérez C. Epstein-Barr virus acute cholecystitis. BMJ Case Rep 2012;2012:bcr0220125744. https://doi.org/10.1136/bcr.02.2012.5744 10.1136/bcr.02.2012.5744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Nagdev A, Ward J. Bedside ultrasound diagnosis of acalculous cholecystitis from epstein-barr virus. West J Emerg Med 2011;12:481-3. https://doi.org/10.5811/westjem.2010.7.1914 10.5811/westjem.2010.7.1914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Arya SO, Saini A, El-Baba M, Salimnia H, Abdel-Haq N. Epstein Barr Virus associated acute acalculous cholecystitis: a rare occurrence but favorable outcome. Clin Pediatr 2010;49:799-804. https://doi.org/10.1177/0009922810363729 10.1177/0009922810363729 [DOI] [PubMed] [Google Scholar]
- [43].Yang HN, Hong KW, Lee JS, Eom JS. A case of acute cholecystitis without cholestasis caused by Epstein-Barr virus in a healthy young woman. Int J Infect Dis 2010;14:e448-9. https://doi.org/10.1016/j.ijid.2009.06.004 10.1016/j.ijid.2009.06.004 [DOI] [PubMed] [Google Scholar]
- [44].Attilakos A, Prassouli A, Hadjigeorgiou G, Lagona E, Kitsiou-Tzeli S, Galla A, Stasinopoulou A, Karpathios T. Acute acalculous cholecystitis in children with Epstein-Barr virus infection: a role for Gilbert's syndrome? Int J Infect Dis 2009;13:e161-4. https://doi.org/10.1016/j.ijid.2008.08.009 10.1016/j.ijid.2008.08.009 [DOI] [PubMed] [Google Scholar]
- [45].Hagel S, Bruns T, Kantowski M, Fix P, Seidel T, Stallmach A. Cholestatic hepatitis, acute acalculous cholecystitis, and hemolytic anemia: primary Epstein-Barr virus infection under azathioprine. Inflamm Bowel Dis 2009;15:1613-6. https://doi.org/10.1002/ibd.20856 10.1002/ibd.20856 [DOI] [PubMed] [Google Scholar]
- [46].Cholongitas E, Katsogridakis K, Dasenaki M. Acalculous cholecystitis during the course of acute Epstein-Barr virus infection. Int J Infect Dis 2009;13:e129-30. https://doi.org/10.1016/j.ijid.2008.06.031 10.1016/j.ijid.2008.06.031 [DOI] [PubMed] [Google Scholar]
- [47].Chalupa P, Kaspar M, Holub M. Acute acalculous cholecystitis with pericholecystitis in a patient with Epstein-Barr Virus infectious mononucleosis. Med Sci Monit 2009;15:CS30-33. [PubMed] [Google Scholar]
- [48].Iaria C, Arena L, Di Maio G, Fracassi MG, Leonardi MS, Famulari C, Cascio A. Acute acalculous cholecystitis during the course of primary Epstein-Barr virus infection: a new case and a review of the literature. Int J Infect Dis 2008;12:391-5. https://doi.org/10.1016/j.ijid.2007.10.005 10.1016/j.ijid.2007.10.005 [DOI] [PubMed] [Google Scholar]
- [49].Pelliccia P, Savino A, Cecamore C, Di Marzio D, Chiarelli F, Primavera A, Schiavone C. Imaging spectrum of EBV-infection in a young patient. J Ultrasound 2008;11:82-4. https://doi.org/10.1016/j.jus.2008.01.002 10.1016/j.jus.2008.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Koch A. D., Van Den Bosch H. C. M., Bravenboer B. Epstein-Barr virus-associated cholecystitis. Ann Intern Med 2007;146:826-7. https://doi.org/10.7326/0003-4819-146-11-200706050-00024 10.7326/0003-4819-146-11-200706050-00024 [DOI] [PubMed] [Google Scholar]
- [51].Prassouli A, Panagiotou J, Vakaki M, Giannatou I, Atilakos A, Garoufi A, Papaevangelou V. Acute acalculous cholecystitis as the initial presentation of primary Epstein-Barr virus infection. J Pediatr Surg 2007;42:E11-3. https://doi.org/10.1016/j.jpedsurg.2006.11.004 10.1016/j.jpedsurg.2006.11.004 [DOI] [PubMed] [Google Scholar]
- [52].Lagona E, Sharifi F, Voutsioti A, Mavri A, Markouri M, Attilakos A. Epstein-Barr virus infectious mononucleosis associated with acute acalculous cholecystitis. Infection 2007;35:118-9. https://doi.org/10.1007/s15010-007-6115-y 10.1007/s15010-007-6115-y [DOI] [PubMed] [Google Scholar]
- [53].Yoshie K, Ohta M, Okabe N, Komatsu T, Umemura S. Gallbladder wall thickening associated with infectious mononucleosis. Abdom Imaging 2004;29:694-5. https://doi.org/10.1007/s00261-004-0173-8 10.1007/s00261-004-0173-8 [DOI] [PubMed] [Google Scholar]
- [54].O'Donovan N, Fitzgerald E. Gallbladder wall thickening in infectious mononucleosis: an ominous sign. Postgrad Med J 1996;72:299-300. https://doi.org/10.1136/pgmj.72.847.299 10.1136/pgmj.72.847.299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Maruyama K, Ushiku H, Kondou Y. Gallbladder wall thickening in children with infectious mononucleosis. J Clin Ultrasound 1994;22:576-8. https://doi.org/10.1002/jcu.1870220913 10.1002/jcu.1870220913 [DOI] [PubMed] [Google Scholar]
- [56].Sainsbury R, Smith PK, LeQuesne G, Davidson GP, Jureidini KF, Moore DJ. Gallbladder wall thickening with infectious mononucleosis hepatitis in an immunosuppressed adolescent. J Pediatr Gastroenterol Nutr 1994;19:123-5. https://doi.org/10.1097/00005176-199407000-00023 10.1097/00005176-199407000-00023 [DOI] [PubMed] [Google Scholar]
- [57].Sung RY, Peck R, Murray HG. Persistent high fever and gall-bladder wall thickening in a child with primary Epstein-Barr viral infection. Aust Paediatr J 1989;25:368-9. https://doi.org/10.1111/j.1440-1754.1989.tb02360.x 10.1111/j.1440-1754.1989.tb02360.x [DOI] [PubMed] [Google Scholar]
- [58].Barie PS, Eachempati SR. Acute acalculous cholecystitis. Curr Gastroenterol Rep 2003;5:302-9. https://doi.org/10.1007/s11894-003-0067-x 10.1007/s11894-003-0067-x [DOI] [PubMed] [Google Scholar]
- [59].Balmadrid B. Recent advances in management of acalculous cholecystitis. F1000Res 2018;7:F1000 Faculty Rev-1660. https://doi.org/10.12688/f1000research.14886.1 10.12688/f1000research.14886.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Jenson HB. Acute complications of Epstein-Barr virus infectious mononucleosis. Curr Opin Pediatr 2000;12:263-8. https://doi.org/10.1097/00008480-200006000-00016 10.1097/00008480-200006000-00016 [DOI] [PubMed] [Google Scholar]


