This randomized clinical trial compares the efficacy of combined atropine and patching therapy vs patching alone in children with severe amblyopia.
Key Points
Question
Is combined atropine and patching therapy (CAPT) more efficacious than patching alone for children aged 3 to 12 years with severe amblyopia?
Findings
In this randomized clinical trial of 108 children, there was substantial improvement in both groups from baseline to 6 months and greater in the CAPT group.
Meaning
While the mean CAPT group amblyopic eye visual acuity improvement was superior to the patching group, the differences were relatively small and the clinical relevance of this difference cannot be determined by this trial.
Abstract
Importance
Patching is often less effective for severe amblyopia because of poor adherence. For the treatment of severe amblyopia, although combined atropine and patching therapy (CAPT) has been found to be efficacious, it is currently unknown whether CAPT is more efficacious than patching alone.
Objective
To compare the efficacy of CAPT vs patching alone in children aged 3 to 12 years with severe amblyopia.
Design, Setting, and Participants
This single-center randomized clinical trial was conducted from November 2018 to May 2020. The visual acuity (VA) examiner was masked to the treatment groups. The follow-up visits were at 3 months and 6 months. Participants aged 3 to 12 years with severe amblyopia (20/100 to 20/500) resulting from strabismus, anisometropia, or both were randomly assigned to CAPT or patching therapy.
Interventions
CAPT or patching alone for 6 months.
Main Outcomes and Measures
Change of the amblyopic eye VA from baseline to 6 months.
Results
Among 108 participants, the mean (SD) age was 5.2 (1.8) years, and 54 (50%) were female. Overall, 53 participants (49%) were randomized to CAPT and 55 (51%) were randomized to patching therapy. At baseline, the mean (SD) amblyopic eye VA was 0.95 (0.22) logMAR (approximately 20/200 [2.2 lines]). At 6 months, the CAPT group’s mean improvement in amblyopic eye VA was 0.72 logMAR (7.2 lines) compared with 0.58 logMAR (5.8 lines) in the patching alone group (difference, 0.14 logMAR [1.4 lines] greater in the CAPT group; 95% CI, 0.05-0.22 logMAR [0.5-2.2 lines]; P = .002). The amblyopic eye VA improvement in the CAPT group also was greater than that in the patching alone group at 3 months (difference in the means, 0.13 logMAR [1.3 lines]; 95% CI, 0.04-0.22 logMAR [0.4-2.2 lines]; P = .004). No participants were withdrawn because of adverse effects.
Conclusions and Relevance
CAPT resulted in more mean improvement of amblyopic eye VA than patching alone among participants enrolled in this trial, although the clinical relevance of this relatively small VA difference cannot be determined from this trial.
Trial Registration
Chinese Clinical Trial Registry Identifier: ChiCTR1800018663
Introduction
Amblyopia is one of the most common causes of monocular vision impairment in children, young adults, and middle-aged adults.1,2 Severe amblyopia refers to the best-corrected visual acuity (VA) of the amblyopic eye of 20/100 or worse.3,4 Although patching therapy is the first choice for treating severe amblyopia,3 it is often found to be less effective as a result of poor adherence, as patients may remove the eye patch earlier than recommended owing to the poor residual acuity when the fellow eye is occluded. Especially in children, who may not grasp the importance of the treatment, adherence may be even worse.
Adherence to atropine treatment, an alternative treatment for amblyopia, has been shown to be better than adherence to patching,5,6,7 but the use of atropine without patching was considered to be insufficient for severe amblyopia.5,8,9 A randomized clinical trial including children with amblyopia aged 7 to 12 years showed that participants who received optical correction with patching plus daily atropine therapy improved more in VA than participants with optical correction alone.10 According to this study, when combined atropine and patching therapy (CAPT) was applied to treat severe amblyopia, it could potentially solve the problem of treatment failure due to poor patching adherence, without the concern of insufficient blurring effect in the fellow eye by atropine. However, their trial included not only severe amblyopia, but also moderate amblyopia, and whether CAPT has advantages over patching alone has not been studied.
To study the treatment of severe amblyopia, which is a common problem encountered in clinical practice, we conducted a randomized clinical trial to compare the efficacy of CAPT vs patching alone therapy in children aged 3 to 12 years with severe amblyopia.
Methods
This study was approved by the ethics committee of the Eye & ENT Hospital of Fudan University, Shanghai, China. The trial protocol is available in Supplement 1. Verbal consent was obtained from all the participants, and their parents gave written informed consent. The described research adhered to the tenets of the Declaration of Helsinki.11 Patients were enrolled from November 2018 and May 2020.
Participant Selection and Randomization
The eligibility criteria are shown in the Box. Children with myopia in either eye were excluded to blur the fellow eye vision at near fixation as much as possible after using atropine.
Box. Eligibility and Exclusion Criteria.
Eligibility criteria
Age 3 to 12 y
Best-corrected visual acuity of 20/100 or poorer in the worse eye
≥2 Lines interocular difference in best-corrected visual acuity
No previous treatment for amblyopia except refractive correction, and the correction is less than 1 mo
-
Amblyopia associated with strabismus, anisometropia, or both
Strabismic amblyopia: amblyopia in the presence of (1) strabismus at a distance and/or near fixation with/without spectacle correction or a history of strabismus surgery and (2) refractive error below the criteria for anisometropic amblyopia
Anisometropic amblyopia: amblyopia in the presence of (1) ≥1.00 D difference in hyperopia or ≥1.50 D difference in astigmatism in any meridian and (2) without strabismus at a distance and near fixation
Mixed amblyopia: amblyopia in the presence of (1) strabismus at a distance and/or near fixation with/without spectacle correction or a history of strabismus surgery and (2) anisometropia of ≥1.00 D difference in hyperopia or ≥1.50 D difference in astigmatism in any meridian
Exclusion criteria
Ocular causes for reduced visual acuity
Myopia in either eye of 0.50 D or more spherical equivalent
History of intraocular surgery
Allergic to atropine or other cycloplegics
Participants were stratified by age (3 to 6 years and 7 to 12 years). The 2 randomization sequences were generated in a 1:1 ratio using SPSS statistical software version 20 (SPSS Inc) by a statistician who was independent of our study. The statistician put allocation details in sequentially numbered, opaque, sealed envelopes, which were concealed from investigators. Only after the enrolled participants completed all baseline assessments were the corresponding envelopes opened by an investigator responsible for assigning the intervention. Then participants of each stratum were randomly assigned to either the CAPT group or the patching alone group.
Treatment Protocols
Once diagnosed, participants were prescribed spectacles (if needed) and started either CAPT or patching therapy simultaneously. We offered adhesive eye pads to all participants. No other compensation was offered. Parents were instructed to record the number of hours of patching in both groups and the day of using atropine in the CAPT group.
Children in the patching group received patching of the fellow eye for 6 hours per day and the patching time should have been continuous. Participants were instructed to do near-visual activities such as painting or playing video games for at least 1 hour when wearing the patch. Children allergic to the eye pads were prescribed a cloth patch mounted on the eyeglass frame.
Children in the CAPT group were prescribed patching of the fellow eye as mentioned above and 1 drop of atropine sulfate, 1%, eye gel once a day for the first 3 days and then once every 2 days (reasons for the frequency of atropine are available in Supplement 1). Parents were reminded that children should wear sunglasses or a hat when outdoors to avoid sunlight exposure.
If the amblyopic eye VA improved to be 1 line lower than the fellow eye VA at 3 months, the patching time would be decreased to 2 hours per day, and the use of atropine would be reduced to twice a week.
Baseline and Follow-up Measurements
The baseline examination included best-corrected VA measurement by a cycloplegic refraction with the Standard Logarithm Visual Acuity Chart (E optotype), ocular alignment with the simultaneous prism cover test and the alternate prism cover test, stereoacuity with the Titmus Stereo Test (Stereo Optical Co, Inc), and ocular examination. All examinations were completed within 14 days before the randomization.
The follow-up visits were at 3 months (±1 week) and 6 months (±1 week). At each visit, the best-corrected VA with a cycloplegic refraction was assessed monocularly in both eyes. The vision examiner was masked to the treatment groups. Ocular alignment and stereoacuity were measured at 6 months in the patching group and at a second visit after discontinuance of atropine for 2 weeks in the CAPT group.
Outcomes
The primary outcome was the change of amblyopic eye VA from baseline to 6 months. The secondary outcomes were as follows: (1) the change of amblyopic eye VA from baseline to 3 months, (2) the proportion of participants with amblyopic eye VA of 20/32 or better at 6 months, and (3) the proportion of participants with an fellow eye VA decrease of 1 line or more at 6 months.
Adherence and Adverse Effects
Adherence to the treatment protocol was assessed using a daily record (the use of atropine and/or number of hours of patching) provided by parents. At each visit, the investigator assessed the participants’ adherence (excellent, >80%12,13,14 of the prescribed treatment completed; moderate, 60%-80%; and poor, <60%).
At each visit, parents were asked about the adverse effects as follows: skin irritation, ocular irritation such as conjunctival congestion, and systemic effects caused by atropine including dryness of the mouth and skin, fever, flushing, and tachycardia. In addition, for the child whose fellow eye VA decreased 1 line or more from the baseline at any visit, the VA would be tested again. If reverse amblyopia occurred in the fellow eye, it would be judged by the investigator whether the treatment should be continued, reduced, or stopped.
Statistical Methods
A sample size of 100 participants was needed to account for 80% power and a type I error of 5% to detect a group difference of 0.15 logMAR (1.5 lines) in primary outcome, assuming an SD of 0.25 logMAR4 and 10% loss to follow-up.
For primary and secondary outcomes, we used univariate linear regression to estimate the mean difference and log-binomial regression to estimate the relative risk, both with a 2-sided 95% CI. A change of 0.1 logMAR was equivalent to a change of 1 line in VA. Our primary analysis was based on the intention-to-treat principle without adjustment. The per-protocol analysis included participants who completed 6-month follow-up. The treatment groups were also compared using multivariate linear regression or log-binomial regression as appropriate in which the outcomes were adjusted for age, sex, and amblyopia cause. The subgroup analysis was used to assess treatment effects in the prespecified subpopulation of children aged 3 to 6 years and aged 7 to 12 years. We also performed subgroup analysis to detect the interaction between interventions and other baseline factors (sex, amblyopia cause, and amblyopic eye refractive error, etc) using the Wald test for the cross-product. P values (other than for the primary outcome) were not adjusted for multiple analyses. Therefore, all secondary outcomes and subgroup analyses should be considered exploratory.
Missing data were treated as missing at random and imputed using multiple imputation. Statistical significance was defined as P values less than .05 with 2-sided testing for the primary outcome. Where Wilcoxon rank sum test was used, the effect size was given by rank-biserial correlation. Analyses were performed using the open-source statistical software R version 4.0.3 (R Foundation).
Results
Baseline Characteristics
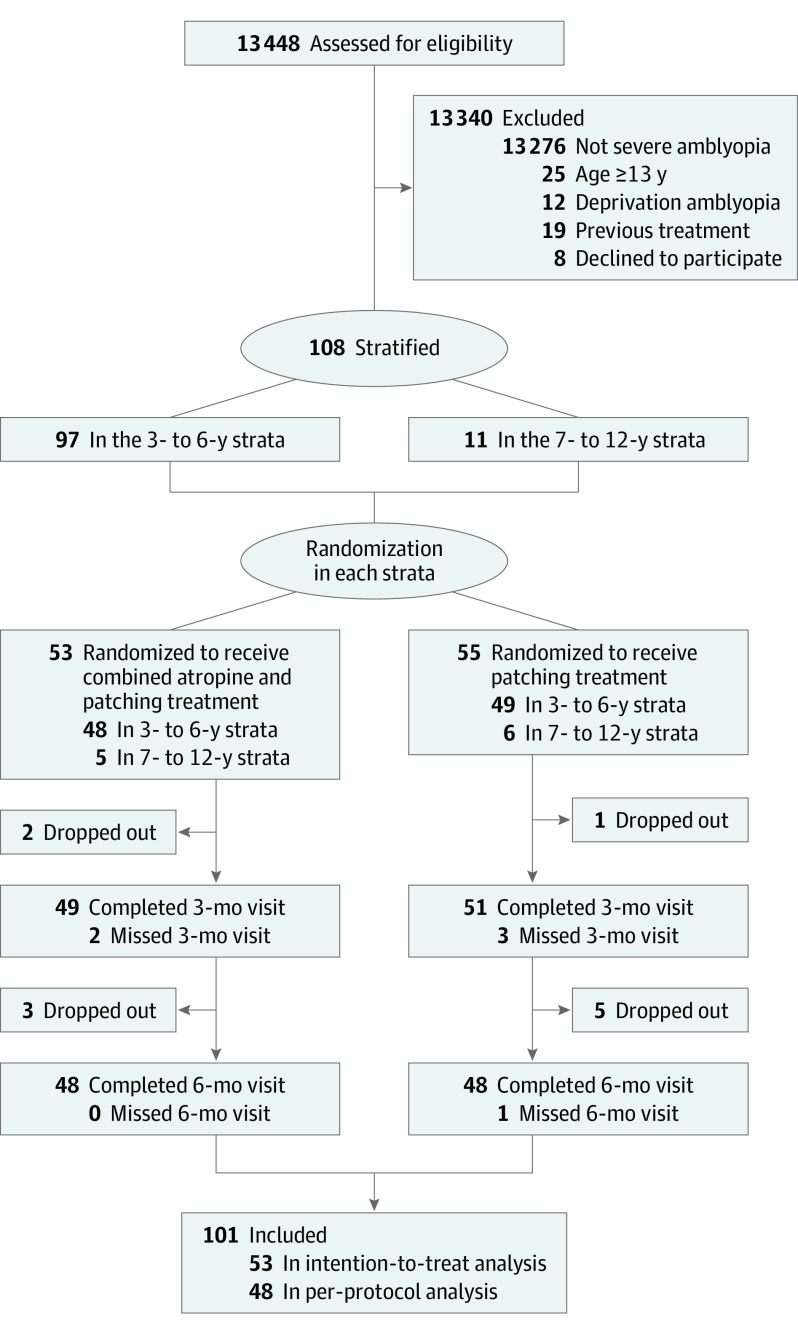
Overall, 108 participants aged 3 to 12 years were enrolled, with 53 randomly assigned to the CAPT group and 55 to the patching group (Figure). All the participants were Chinese. Baseline characteristics are showed in Table 1 and eTable 1 in Supplement 2.
Figure. CONSORT Flow Diagram.
Table 1. Baseline Characteristics According to Treatment Group (Intention-to-Treat Analysis).
| Characteristic | Group, No. (%) | |
|---|---|---|
| Combined atropine and patching | Patching | |
| Total No. | 53 | 55 |
| Sex | ||
| Male | 25 (47) | 29 (53) |
| Female | 28 (53) | 26 (47) |
| Age at enrollment, y | ||
| 3-<7 | 48 (91) | 49 (89) |
| 7-<13 | 5 (9) | 6 (11) |
| Mean (SD), y | 5.2 (1.3) | 5.1 (1.8) |
| Amblyopia cause | ||
| Strabismus | 10 (19) | 11 (20) |
| Anisometropia | 30 (57) | 34 (62) |
| Mixed | 13 (25) | 10 (18) |
| Type of strabismusa | ||
| Esotropia | 13 (57) | 12 (57) |
| Exotropia | 10 (43) | 9 (43) |
| Duration of prior amblyopia treatment, db | ||
| 0 | 47 (89) | 50 (91) |
| 1-15 | 4 (8) | 4 (7) |
| 16-30 | 2 (4) | 1 (2) |
| Distance VA in amblyopic eyec | ||
| 0.2 (20/100) | 5 (9) | 10 (18) |
| 0.16 (20/125) | 17 (32) | 23 (42) |
| 0.1 (20/200) | 20 (38) | 13 (24) |
| 0.05 (20/400) | 7 (13) | 5 (9) |
| 0.04 (20/500) | 4 (8) | 4 (7) |
| LogMAR, mean (SD) | 0.98 (0.22) | 0.93 (0.23) |
| VA in Snellen equivalent, mean | 20/200 + 1 | 20/200 + 3 |
| Distance VA in fellow eyec | ||
| 1.0 (20/20) | 22 (42) | 19 (35) |
| 0.8 (20/25) | 16 (30) | 18 (33) |
| 0.6 (20/32) | 9 (17) | 11 (20) |
| 0.5 (20/40) | 3 (6) | 0 (0) |
| 0.4 (20/50) | 3 (6) | 7 (13) |
| LogMAR, mean (SD) | 0.11 (0.12) | 0.13 (0.13) |
| VA in Snellen equivalent, mean | 20/32 + 4 | 20/32 + 3 |
| Interocular VA difference, mean (SD), line | 8.74 (2.47) | 7.95 (2.48) |
| Refractive error, mean (SD), Dd | ||
| Amblyopic eye | 6.04(2.30) | 6.71 (2.40) |
| Fellow eye | 2.63 (2.02) | 3.29 (2.10) |
Abbreviations: D, diopter; VA, visual acuity.
Type of strabismus includes patients with strabismic amblyopia or mixed amblyopia; thus, the total number of strabismus type is not 108.
Prior amblyopia treatment only refers to spectacle wear.
The distance visual acuity is measured by Standard Logarithm Visual Acuity Chart. Approximate Snellen equivalent is provided in parentheses.
Spherical equivalent in diopters.
Follow-up and Adherence
The 6-month visit was completed by 48 participants (91%) in the CAPT group and by 48 (87%) in the patching group (Figure). The VA examiner was masked to treatment group at all visits.
At 6 months, there was no significant difference of patching adherence between groups (P = .33; r = 0.09; 95% CI, 0-0.28; eTable 2 in Supplement 2). The prescribed patching regimen and atropine regimen remained the same throughout follow-up in both groups, except for 2 in the CAPT group and 3 in the patching group changing to 2-hour patching per day and atropine (for the CAPT group) twice a week, for their amblyopic eye VA was improved to be 1 line lower than the fellow eye VA at 3 months.
Primary Outcomes
At 6 months, the intention-to-treat analysis showed that the CAPT group’s mean improvement in amblyopic eye VA was 0.72 logMAR (7.2 lines) compared with 0.58 logMAR (5.8 lines) in the patching group (difference, 0.14 logMAR [1.4 lines] greater in the CAPT group; 95% CI, 0.05-0.22 logMAR [0.5-2.2 lines]; P = .002; Table 2 and eFigure 1 in Supplement 2). The result of the per-protocol analysis was consistent with the intention-to-treat analysis (eTable 3 in Supplement 2), and the comparisons of outcomes adjusted for sex, age, and amblyopia cause were consistent with the unadjusted analysis (eTables 4 and 5 in Supplement 2). The distribution of amblyopic eye VA is shown in eTable 6 in Supplement 2. It is noteworthy that there were 7 participants in the patching group but none in the CAPT group with an improvement of amblyopic eye VA of 0.30 logMAR (3 lines) or less at 6 months.
Table 2. Primary and Secondary Outcomes (Intention-to-Treat Analysis).
| Outcome | Combined atropine and patching group | Patching group | Mean difference, RR (95% CI) | P value |
|---|---|---|---|---|
| No. | 53 | 55 | NA | NA |
| Primary outcome | ||||
| Change in AE VA at 6 mo, mean (SD) | ||||
| LogMAR | 0.72 (0.20) | 0.58 (0.22) | 0.14 (0.05-0.22) | .002 |
| Line | 7.2 (2.0) | 5.8 (2.2) | 1.4 (0.5-2.2) | .002 |
| Secondary outcome | ||||
| Change in AE VA at 3 mo, mean (SD) | ||||
| LogMAR | 0.54 (0.24) | 0.41 (0.22) | 0.13 (0.04-0.22) | .004 |
| Line | 5.4 (2.4) | 4.1 (2.2) | 1.3 (0.4-2.2) | .004 |
| AE VA ≥20/32 at 6 mo, No. (%) | 32 (60) | 22 (40) | 1.48 (0.85-2.58) | .17 |
| FE VA decrease ≥1 line at 6 mo, No. (%)a | 0 | 0 | NA | NA |
Abbreviations: AE, amblyopic eye; FE, fellow eye; NA, not applicable; RR, relative risk; VA, visual acuity.
The number in both groups is 0, so the relative risk cannot be calculated.
No significant interaction was found between the treatment groups and the baseline characteristics of age, amblyopia cause, amblyopic eye VA, etc (eFigure 2 in Supplement 2; the subgroup analysis was not prespecified).
Secondary Outcomes
At 3 months, the intention-to-treat analysis showed that the amblyopic eye VA improvement in the CAPT group also was greater than that in the patching group (difference in the means, 0.13 logMAR [1.3 lines]; 95% CI, 0.04-0.22 logMAR [0.4-2.2 lines]; P = .004). At 6 months, the amblyopic eye VA improved to 20/32 or better for 32 participants (60%) and 22 participants (40%) in the CAPT group and patching group, respectively (relative risk, 1.48; 95% CI, 0.85-2.58; P = .17), and no participant in either group showed a fellow eye VA decrease of 1 line or more (Table 2; per-protocol analysis in eTable 3 in Supplement 2).
Stereoacuity
No participant in either group had stereopsis at baseline. After 6 months, in the CAPT group and the patching group, there were 15 participants (28%) and 12 participants (22%) who had the stereoacuity of 400 arcsec or better, respectively (P = .81; r = 0.02; 95% CI, 0-0.22).
Adverse Effects
The distribution of fellow eye VA at 6 months is shown in eTable 7 in Supplement 2. There were 3 participants (6%) in the CAPT group and 2 (4%) in the patching group with fellow eye VA of 0.5 lines worse than that at baseline. The subsequent follow-up after 6 months showed that the fellow eye VA of all the 4 participants became better than at baseline level. One participant with intermittent exotropia in the CAPT group increased by 20 prism diopter at 6 months, which might be due to the natural development of exotropia or incomplete exposure of exotropia caused by strong fusion control at the baseline examination. None of the participants with strabismus, including the patient with an increase of 20 prism diopter, had surgical correction during the 6 months, as surgeries were arranged after amblyopic eye VA reached almost the same as that in the fellow eye.
No participants in this study changed treatment or quit owing to irreversible adverse effects, indicating that both therapies were well tolerated. In the CAPT group, adverse effects were reported by 6 participants (11%) for light sensitivity, 2 (4%) for conjunctival congestion, and 2 (4%) for facial flushing. Skin irritation caused by the eye patch was reported by 10 (18%) in the CAPT group and 9 (16%) in the patching group. All these symptoms relieved spontaneously.
Discussion
We conducted a randomized clinical trial to compare the efficacy of CAPT vs patching alone in 108 children aged 3 to 12 years with severe amblyopia. While the CAPT group mean amblyopic eye VA improvement was superior to the patching group at 3 months and 6 months, the differences were relatively small and the clinical relevance of this difference cannot be determined by this trial.
Our study population included 3- to 12-year-old children. However, the findings of our study should be interpreted with caution for the age strata of 7 to 12 years. First, we enrolled much fewer cases of this age strata than previously expected. Second, their amblyopic eye VA improvement between CAPT and patching showed little difference (0.01 logMAR [0.1 lines]; eFigure 2 in Supplement 2) in our limited sample size, although the interaction between interventions and age stratums (age 3-6 years and 7-12 years) was not significant (P = .34; the subgroup analysis was not prespecified). Therefore, a further study with a larger sample size for children aged 7 to 12 years is needed to determine a more precise estimate of the treatment effect and whether 1 management strategy has superiority over the other.
Efficacy of CAPT and Patching Therapy
The VA improvement with CAPT was 0.72 logMAR (7.2 lines, equivalent to 36 letters) at 6 months in our study. It was consistent with the results of a randomized study by the Pediatric Eye Disease Investigator Group,10 in which 36 participants (60%) aged 7 to 12 years with severe amblyopia improved at least 10 letters with CAPT. Although the Pediatric Eye Disease Investigator Group study and ours differed not only in the age group but also in the proportion of amblyopia cause (38% vs 59% of participants with pure anisometropia), both studies provide evidence that CAPT was efficacious for severe amblyopia.
However, while the Pediatric Eye Disease Investigator Group10 demonstrated the efficacy of CAPT, whether CAPT could produce greater VA improvement than patching alone remained unknown. At 6 months in our study, amblyopic eye VA with CAPT improved 0.14 logMAR (1.4 lines) more than with patching alone. In addition, the subgroup analysis (eFigure 2 in Supplement 2) showed no significant interaction between interventions and baseline VA subgroups (VA, ≤20/200 or >20/200), which suggested that CAPT achieved more improvement in amblyopic eye VA than patching in the initial 6-month treatment, even when baseline VA was as poor as 20/200 or lower. We speculate that atropine, as a cycloplegia that can prevent accommodation, could induce blurred vision in the fellow eye at near fixation to force participants to use the amblyopic eye more when the fellow eye was not covered.
In the patching group, amblyopic eye VA improved by 0.58 logMAR (5.8 lines) at 6 months. The VA improvement might be a little overestimated in both groups of our study because participants started the optical correction and the occlusion at the same time without a period to observe the effect of spectacle correction alone. However, the difference of VA improvement between the 2 groups would not be affected much because the proportion of participants who had not experienced optical correction before enrollment was similar in both groups (Table 1; eTable 1 in Supplement 2).
At the 6-month visit, there were 7 in the CAPT group and 2 in the patching group who achieved the same VA in both eyes. Their 9-month follow-up showed no VA regression. The remaining participants still needed to continue the treatment after a short-term therapy of 6 months, and whether the difference in VA improvement between the 2 groups can hold over long-term follow-up remains to be studied. However, a short-term better recovery of VA can improve patients’ quality of life,15 especially when the fellow eye is patched and, in our experience, give the parents more confidence in the amblyopia treatment.
Adherence of CAPT and Patching Therapy
In our study, participant adherence with patching time was similar in both groups (eTable 2 in Supplement 2). It indicated that the difference in VA change between the 2 groups was attributed to the effect of atropine treatment.
Participant adherence to the use of atropine was excellent in 75% of participants in the CAPT group. Moreover, there were 7 participants in the patching group with an improvement in amblyopic eye VA of 3 lines or less and none in the CAPT group at 6 months. These findings suggest that the CAPT would be more helpful for children who have poor adherence with patching. However, although CAPT is an alternative to patching therapy alone, this trial cannot determine if children with poor adherence to patching would have greater improvement with one vs the other strategy.
Limitations
In addition to the sample size shortage of children aged 7 to 12 years, there are other limitations in our study. First, we did not assess the fixation preference and the near VA with spectacles in the cycloplegic fellow eye; thus, whether participants in the CAPT group changed to use the amblyopic eye for fixation remains unknown. However, a study on VA in cycloplegic eyes16 showed that the near VA of a child with 0.50 diopters of hyperopia could be reduced to approximately 20/200 after cycloplegia. Consequently, given that most children in our study wore glasses 1.0 to 1.5 diopters less than full correction (except for those with accommodative esotropia wearing full-corrected spectacles), atropine could blur the vision at both near and distance fixation. We could expect that a child with hyperopia and with undercorrected spectacles at least sometimes preferred to fixate with the amblyopic eye, particularly at near distance. Even for children with accommodative esotropia who wear the full-corrected spectacles, they may choose the amblyopic eye for fixation because of the discomfort of looking at near objects after cycloplegia. Second, the VA improvement may be less in practical treatment than that in this study because participants may comply better with the treatment as a result of being required to keep a record of daily treatment and attend follow-up visits on schedule. Finally, the study was a single-center randomized clinical trial, so one should be careful when extending the results to other populations.
Conclusions
The current study indicates that both the CAPT and patching alone therapy were efficacious for children aged 3 to 12 years with severe amblyopia. CAPT resulted in more mean improvement of amblyopic eye VA than patching alone, although the differences were relatively small and the clinical relevance of this difference cannot be determined by this trial.
Trial Protocol.
eTable 1. Baseline Characteristics According to Treatment Group (Per-protocol Analysis)
eTable 2. Patient Adherence to the Prescribed Treatment (Intention-to-treat Analysis)
eTable 3. Primary and Secondary Outcomes (Per-protocol Analysis)
eTable 4. Adjusted Analysis for Primary and Secondary Outcomes (Intention-to-treat analysis)
eTable 5. Adjusted Analysis for Primary and Secondary Outcomes (Per-protocol Analysis)
eTable 6. Visual Acuity in the Amblyopic Eye at the Primary Outcome Examination
eTable 7. Visual Acuity in the Fellow Eye at 6 months (Intention-to-treat Analysis)
eFigure 1. Change of Amblyopic-eye Visual Acuity at 3 Months and 6 Months
eFigure 2. Subgroup Analysis of Change in Amblyopic-eye Visual Acuity at 6 Months (Intention-to-treat analysis)
Data Sharing Statement.
Footnotes
Abbreviation: D, diopter.
References
- 1.Simons K. Preschool vision screening: rationale, methodology and outcome. Surv Ophthalmol. 1996;41(1):3-30. doi: 10.1016/S0039-6257(97)81990-X [DOI] [PubMed] [Google Scholar]
- 2.Attebo K, Mitchell P, Cumming R, Smith W, Jolly N, Sparkes R. Prevalence and causes of amblyopia in an adult population. Ophthalmology. 1998;105(1):154-159. doi: 10.1016/S0161-6420(98)91862-0 [DOI] [PubMed] [Google Scholar]
- 3.Wallace DK, Repka MX, Lee KA, et al. Amblyopia preferred practice pattern. Ophthalmology. 2018;125(1):p105-p142. doi: 10.1016/j.ophtha.2017.10.008 [DOI] [PubMed] [Google Scholar]
- 4.Holmes JM, Kraker RT, Beck RW, et al. ; Pediatric Eye Disease Investigator Group . A randomized trial of prescribed patching regimens for treatment of severe amblyopia in children. Ophthalmology. 2003;110(11):2075-2087. doi: 10.1016/j.ophtha.2003.08.001 [DOI] [PubMed] [Google Scholar]
- 5.Foley-Nolan A, McCann A, O’Keefe M. Atropine penalisation versus occlusion as the primary treatment for amblyopia. Br J Ophthalmol. 1997;81(1):54-57. doi: 10.1136/bjo.81.1.54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Scheiman MM, Hertle RW, Kraker RT, et al. ; Pediatric Eye Disease Investigator Group . Patching vs atropine to treat amblyopia in children aged 7 to 12 years: a randomized trial. Arch Ophthalmol. 2008;126(12):1634-1642. doi: 10.1001/archophthalmol.2008.107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pediatric Eye Disease Investigator Group. A randomized trial of atropine vs. patching for treatment of moderate amblyopia in children. Arch Ophthalmol. 2002;120(3):268-278. doi: 10.1001/archopht.120.3.268 [DOI] [PubMed] [Google Scholar]
- 8.Repka MX, Ray JM. The efficacy of optical and pharmacological penalization. Ophthalmology. 1993;100(5):769-774. doi: 10.1016/S0161-6420(93)31577-0 [DOI] [PubMed] [Google Scholar]
- 9.Simons K, Stein L, Sener EC, Vitale S, Guyton DL. Full-time atropine, intermittent atropine, and optical penalization and binocular outcome in treatment of strabismic amblyopia. Ophthalmology. 1997;104(12):2143-2155. doi: 10.1016/S0161-6420(97)30048-7 [DOI] [PubMed] [Google Scholar]
- 10.Scheiman MM, Hertle RW, Beck RW, et al. ; Pediatric Eye Disease Investigator Group . Randomized trial of treatment of amblyopia in children aged 7 to 17 years. Arch Ophthalmol. 2005;123(4):437-447. doi: 10.1001/archopht.123.4.437 [DOI] [PubMed] [Google Scholar]
- 11.World Medical Association . World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191-2194. doi: 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
- 12.Fielder AR, Irwin M, Auld R, Cocker KD, Jones HS, Moseley MJ. Compliance in amblyopia therapy: objective monitoring of occlusion. Br J Ophthalmol. 1995;79(6):585-589. doi: 10.1136/bjo.79.6.585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Newsham D. Parental non-concordance with occlusion therapy. Br J Ophthalmol. 2000;84(9):957-962. doi: 10.1136/bjo.84.9.957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Newsham D. A randomised controlled trial of written information: the effect on parental non-concordance with occlusion therapy. Br J Ophthalmol. 2002;86(7):787-791. doi: 10.1136/bjo.86.7.787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen Y, Chen X, Chen J, Zheng J, Xu J, Yu X. Longitudinal impact on quality of life for school-aged children with amblyopia treatment: perspective from children. Curr Eye Res. 2016;41(2):208-214. doi: 10.3109/02713683.2015.1011280 [DOI] [PubMed] [Google Scholar]
- 16.Wallace DK. Visual acuity after cycloplegia in children: implications for atropine penalization. J AAPOS. 1999;3(4):241-244. doi: 10.1016/s1091-8531(99)70009-1 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol.
eTable 1. Baseline Characteristics According to Treatment Group (Per-protocol Analysis)
eTable 2. Patient Adherence to the Prescribed Treatment (Intention-to-treat Analysis)
eTable 3. Primary and Secondary Outcomes (Per-protocol Analysis)
eTable 4. Adjusted Analysis for Primary and Secondary Outcomes (Intention-to-treat analysis)
eTable 5. Adjusted Analysis for Primary and Secondary Outcomes (Per-protocol Analysis)
eTable 6. Visual Acuity in the Amblyopic Eye at the Primary Outcome Examination
eTable 7. Visual Acuity in the Fellow Eye at 6 months (Intention-to-treat Analysis)
eFigure 1. Change of Amblyopic-eye Visual Acuity at 3 Months and 6 Months
eFigure 2. Subgroup Analysis of Change in Amblyopic-eye Visual Acuity at 6 Months (Intention-to-treat analysis)
Data Sharing Statement.