Abstract
Objectives
Intensive health services’ utilization is common in older individuals affected by chronic diseases. This study assessed whether a structured family nurse-led educational intervention would be effective in reducing health services’ use (readmissions and/or emergency service access) among older people affected by chronic conditions.
Methods
This is a non-randomized before-after pilot study. A sample of 78 patients was recruited from two general practices in Italy and 70 among them were followed for 8 months. Standard home care was provided during the first four months’ period (months 1–4), followed by the educational intervention until the end of the study (months 5–8). The intervention, based on the teach-back method, consisted of by-weekly 60-min home sessions targeting aspects of the disease and its treatment, potential complications, medication adherence, and health behaviours. Rates of health services’ use were collected immediately before (T0), and after the interventions (T1). Differences in utilization rates were examined by the McNemar’s test. Potential factors associated with the risk of health services’ use were explored with a Cox proportional hazard regression model.
Results
The sample (n = 78) was predominantly female (n = 50, 64.1%), and had a mean age of 76.2 (SD = 4.8) years. Diabetes mellitus was the most frequent disease (n = 27, 34.6%). McNemar’s test indicated a significant reduction in health services’ use at T1 (McNemar χ2 = 28.03, P < 0.001). Cox regressions indicated that time and patient education, as well as their interaction, were the only variables positively associated with the probability of health services’ use.
Conclusion
A teach-back intervention led by a family nurse practitioner has the potential to reduce health services’ use in older patients with chronic diseases.
Keywords: Aged, Chronic disease, Facilities and services utilization, Family nurse practitioners, Patient readmission, Home care services, Health services
What is known?
-
•
The shift of patient care to home settings has favoured the specialization of key professionals across the continuity of care, such as the family nurse practitioners for care support of patients with chronic disease.
-
•
Involving the family nurse practitioner in the education of patients with chronic diseases has the potential to reduce health services’ use and the burden of the health-care systems.
What is new?
-
•
A teach-back educational intervention led by family nurse practitioners has the potential to reduce readmissions and emergency services’ use in patients with chronic diseases.
-
•
For being a risk factor of health services’ use, education levels should be screened routinely in patients with chronic diseases.
1. Introduction
As the population ages and lives longer, chronic diseases keep rapidly expanding worldwide [1]. This trend determines a high burden both on the individuals and the health care systems, which are mostly organized to deal with acute rather than long-term care [2].
Chronic diseases are characterized by long lasting and detrimental adverse effects on health. There are highly prevalent diseases such as diabetes mellitus (DM) and chronic obstructive pulmonary disease (COPD) that are particularly burdensome because they are associated with physical symptoms, complications, and exacerbations [[3], [4], [5]]. These are in turn responsible for recurrent accesses to care such as readmissions and emergency services’ use [6,7].
Self-management, defined by Barlow as the patients’ ability to manage symptoms, treatment, and the consequences of living with an illness [8], has been recognized as a means to reduce the burden of chronic diseases. Unfortunately, literature highlights that this ability is often difficult to achieve [9,10] and patients who show self-management deficits are more likely to be hospitalized and have adverse health-outcomes than those who are more compliant [11,12].
Self-management interventions have expanded substantially over the years, to incorporate approaches aimed at increasing patients’ ability to manage their health. In general, such interventions have shown to be promising, although for some categories such as older people, significant improvements can be more challenging to obtain [13]. This can happen for a variety of reasons but one amongst others is the poor level of health literacy, which is frequently exhibited by these populations; this in turn, hinders the assimilation of the information [14].
Teach-back is a method which has been found promising to reinforce self-management and health literacy [15]. This educational approach works by asking the patient to repeat the instructions they receive [16]. Final aim is to increase the understanding of the information delivered during the education sessions. A systematic review by Yen and Leasure [17] found that the teach-back was effective in improving disease self-management, quality of life, satisfaction and readmissions in patients with chronic conditions. However, based to our knowledge, this method has not been sufficiently investigated on older chronic individuals in the context of primary care.
There are several sound reasons to prioritize educational research on primary care. First, we are witnessing a progressive transition of the care from the hospitals to the communities as a result of a cheaper and more effective care delivery [18]. Second, primary care services are currently being reconsidered to reduce unnecessary admissions and optimise the use of health services in response to COVID-19 pandemic [19]. Lastly, the shift of patient care to home settings has favoured the specialization of key professionals across the continuity of care, such as the family nurse practitioners (FNP) [20]. Their role appears attractive as it covers health promotion, disease prevention, and care support of patients and families in the community [20,21].
The aim of the ADVICE study was to: (i) assess whether a structured family nurse-led educational intervention founded on the principles of the teach-back method was effective in reducing disease-related readmissions and/or emergency services’ use amongst older people affected by chronic conditions, and (ii) investigate the factors associated with the risk of health services’ use.
2. Methods
To report this study, we adhered to the Transparent Reporting of Evaluations with Nonrandomized Designs (TREND) statement checklist [22] retrieved on the Equator site (http://www.equator-network.org/).
2.1. Research setting
This pilot study was conducted at two large general practices located in Rome, Italy. These services essentially cover primary care, which is coordinated by general practitioners and a team of multidisciplinary specialists. The most prevalent populations encompass middle-aged adults and older individuals with a wide range of mental and chronic physical diseases.
2.2. Study design and sample
This was a pragmatic multicentric non-randomized before-after study, with collection of outcomes before (T0) and after the educational intervention (T1). Potential participants were recruited from the clinical record systems of the general practices during June 2019.
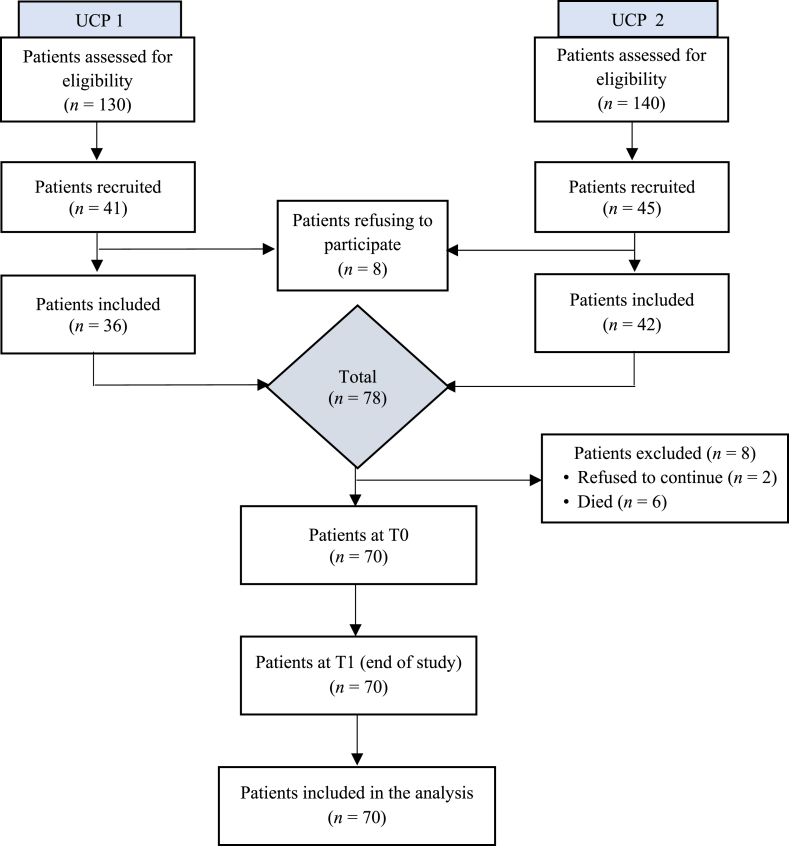
Inclusion criteria were adult patients aged ≥65 years, with at least one chronic condition (defined as an illness lasting more than 6 months) [23] and willing to participate. Exclusion criteria were important cognitive and/or neurological deficits, terminal disease, and/or cancer. Of the 86 patients recruited, 78 (90.7%) accepted to participate (Fig. 1). Written informed consent was obtained from all members during the first visit.
Fig. 1.
Flowchart for recruitment, enrollment and follow-up of study participants. T0 and T1 correspond to the end of months 1–4 and 5–8, respectively. UCP = Unità di Cure Primarie.
2.3. Procedures
All participants were followed for 8 months (from the beginning of July 2019 to the end of February 2020) by a total of ten nurses and two general practitioners. During the first study period (months 1–4) four registered nurses provided regular by-weekly standard home care visits, which generally included provision of functional support during activities of daily living, wound medications, vital sign checks, intravenous drug administrations, and blood samples’ taking.
In the second study period (months 5–8) four FNP provided the educational intervention, founded on the principles of the teach-back communication. It consisted of by-weekly face-to-face sessions aimed at targeting aspects of the disease and its treatment, potential complications, medication adherence, and health behaviours. The sessions had an average length of 60-min and were tailored to the care needs exhibited by the participants. The FNP started with a general assessment of the patient educational needs, during which one or more nursing diagnoses were also formulated. The diagnoses were based on the Clinical Care Classification system (CCC) [24] and served as a reference point for tailoring the teach-back intervention. To ensure quality and homogeneity of the education sessions, the FNP were required (for every session) to fill in a checklist, adapted from the Teach-back Observation Tool [25].
Before the beginning of the study the FNP followed a certified course organized in three sessions, for a total duration of 12 h. The sessions addressed the methodology of the teach-back, including implementation, planning, management, and assessment. To facilitate the learning process, the training also included specific techniques such as role playing, simulations, and case studies.
2.4. Outcomes
The primary outcome of the study was the difference in rates of health services’ use before (T0) and after the intervention (T1). This information was asked directly to the patients and subsequently confirmed through the medical records. By “health services’ use” we defined two types of events: (i) readmissions, or any event related to chronic disease exacerbations in patients who were discharged from a hospital, which in turn, caused a readmission within the next 60 days and (ii) emergency services’ use, or any access to emergency services during the study period, which were related to chronic disease exacerbations. Sixty days was chosen as time frame for defining readmissions, considering the frequent use of this measure across studies [26,27].
No more than one readmission was counted on the same patient within each study period. The secondary outcome measure was satisfaction, assessed with the Unipolar Satisfaction Thermometer [28]. This instrument is composed of 5 points, ranging from “not at all satisfied” to “completely satisfied”, and participants were asked to tick the box that reflected most closely the satisfaction level related to the intervention.
2.5. Statistical analysis
Patients’ characteristics were summarized with descriptive statistics, including means and standard deviations for continuous outcomes, and proportions for categorical outcomes. The primary outcome (difference in health services’ use events before and after the intervention) was analysed with chi square goodness of fit test to understand the likelihood that the observed events (readmissions and/emergency services’ use) were equal to those expected (the probability of the event was assumed to be equal for all participants). McNemar-Bowker test was conducted to detect significant differences in proportions of health services’ use before and after the intervention. Odds ratio (OR) and effects size (Cohen’s D) were calculated as b/c and [(b/(b + c)]−0.5, respectively, where b and c were the discordant cells of the paired contingency table. Values higher than 0.50 for Cohen’s D were interpreted as large sizes [29]. Wilcoxon sign test rank was conducted to investigate differences in satisfaction scores between the two study periods. A multivariable Cox proportional hazard regression model was fitted to model the risk of health-care services’ use as a function of time, education, age, gender and living condition. To account for the different risk between the two study periods, time was considered as a proxy measure of treatment (0 = before the intervention, 1 = after the intervention) and introduced in the model as a time-varying covariate. Finally, unadjusted Kaplan-Meier estimates were produced for each study period. All parameters were considered significant at a 0.05 P-value level. Statistical analyses were conducted using STATA version 16.0 [30].
2.6. Ethical considerations
This study was approved at the ethics committee of ASL Roma 4 Rome Italy. Participants were approached by the research team during the routine home care visits and invited to join the study. Purposes and main strategies of the research were accurately explained, at the same time assuring that all data collected would be maintained strictly confidential. Informed consent form was obtained after verbal acceptance to participate. The study conforms to the ethical standards reported in the Declaration of Helsinki [31].
3. Results
From a total of 270 potentially eligible patients, 78 accepted to participate and sign the informed consent form. Fig. 1 shows the details of the selection process. The characteristics of the participants at baseline are reported in Table 1. Briefly, the sample (n = 78) was predominantly female (n = 50, 64.1%), with a mean age of 76.2 (SD = 4.8) years. All the participants were retired and most declared living not alone (n = 53, 68.0%). Diabetes mellitus was the most frequent disease (n = 27, 34.6%), followed by heart failure (n = 25, 32.1%) and COPD (n = 26, 33.3%). Within the first month, n = 8 (11.43%) patients dropped out without experiencing any event. Hence, they were not included in subsequent analyses. Table 2 reports the prevalence of health services’ use at the end of the two study periods. At T0, n = 50 (71.4%) patients used the health services at least once during the 4 months of observations. At T1, n = 20 (28.6%) patients used the health services at least once during the subsequent 4 months of observation. In the first and second study period an average of 28.2 and 70.0 days elapsed before the utilizations, respectively. The most prevalent nursing diagnoses formulated during the FNP visits were noncompliance of dietary regimen, knowledge deficit of disease process, and knowledge deficit of dietary regimen.
Table 1.
Sociodemographic and clinical characteristics of patients at baseline (n = 78).
| Characteristics | n (%) |
|---|---|
| Age, years, Mean ± SD (range) | 76.2 ± 4.8 (65–85) |
| Gender | |
| Male | 28 (35.9) |
| Female | 50 (64.1) |
| Education level | |
| ≥9 years | 25 (32.0) |
| <9 years | 53 (68.0) |
| Working condition | |
| Retired | 78 (100) |
| Marital status | |
| Married | 54 (69.2) |
| Never married | 8 (10.3) |
| Divorced | 13 (16.7) |
| Widowed | 3 (3.8) |
| Family condition | |
| Lives alone | 25 (32.0) |
| Lives with others | 53 (68.0) |
| Diagnosis at enrollmenta | |
| Hypertension | 42 (53.9) |
| Type 2 diabetes mellitus | 27 (34.6) |
| Heart failure | 25 (32.1) |
| Chronic obstructive pulmonary disease | 26 (33.3) |
| Chronic kidney disease | 4 (5.1) |
| Chronic venous insufficiency | 5 (6.4) |
| Dyslipidemia | 13 (16.7) |
Note: Data are n (%), unless otherwise indicated. a Based on the International Classification Disease (ICD), and the diagnoses are not mutually exclusive.
Table 2.
Prevalence of health services’ use before and after the intervention (n = 70).
| Study follow-up | Readmissions | Emergency services’ use | Total events |
|---|---|---|---|
| T0 | 23 (32.9) | 27 (38.6) | 50 (71.4) |
| T1 | 8 (11.4) | 12 (17.1) | 20 (28.6) |
Note: Data are n (%). T0 and T1 correspond to the end of month 4 and end of month 8, respectively.
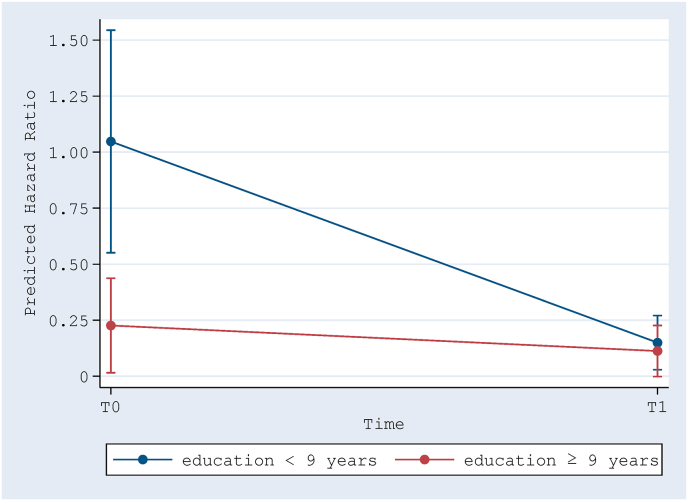
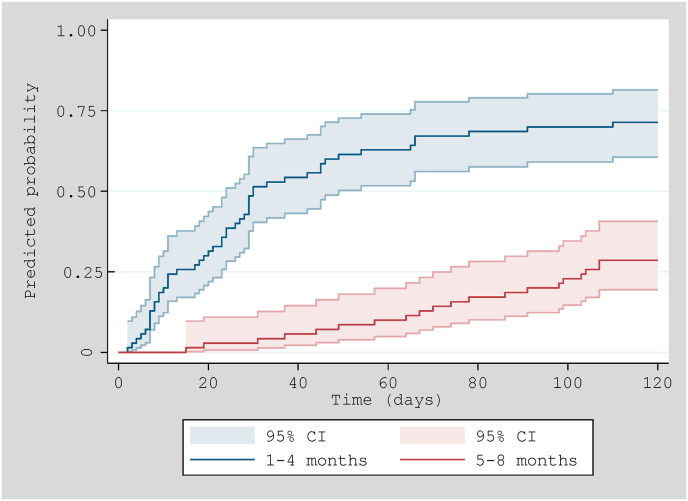
The Chi square goodness of fit test showed that at T0 the probability of health services’ use among the sample was 0.71, which was significantly different from 0.5 (equiprobability): [χ2(1) = 12.86, P < 0.001]. At T1 the probability significantly dropped to 0.29: [χ2 (1) = 12.86, P < 0.001]. McNemar test conducted on the sample who completed the two study periods (n = 70) indicated a significant reduction in the proportion of health services’ use between T0 and T1 (McNemar χ2 = 28.03, P < 0.001, OR = 0.016, Cohen’s D = 0.48). Wilcoxon matched-pairs signed-rank test indicated that satisfaction was significantly higher at T1 (Mean = 77.57) than at T0 (Mean = 56.86; Z = −10.33, P < 0.001). Multivariable Cox proportional hazard regression model indicated that being in the intervention period (i.e., months 5–8) (HR = 0.142, P < 0.001) and having an education level equal or greater than 9 years (HR = 0.216, P < 0.001) were associated with a lower risk of using health services (Table 3). The interaction between the two variables was also significant (HR = 3.479, P = 0.046), meaning that the risk predicted by education changed significantly by time (Fig. 2). The Kaplan-Meier curves for the two study periods clearly display a lower risk trend of health-care services’ use during the intervention period (Fig. 3).
Table 3.
Multivariable Cox regression model for factors predicting risk of health-care services’ use (patients = 70; observations = 140).
| Variables | HR | P | 95% CI |
|
|---|---|---|---|---|
| Lower | Upper | |||
| Time (T0 as reference) | 0.142 | <0.001 | 0.051 | 0.402 |
| Education (<9 year as reference) | 0.216 | <0.001 | 0.102 | 0.457 |
| Age (<77 as reference) | 1.235 | 0.486 | 0.682 | 2.236 |
| Gender (female as reference) | 0.841 | 0.580 | 0.456 | 1.552 |
| Living condition (not alone as reference) |
0.920 |
0.791 |
0.497 |
1.702 |
| Time∗Education | 3.479 | 0.046 | 1.019 | 11.871 |
| Time∗Age | 0.543 | 0.262 | 0.187 | 1.578 |
| Time∗Gender | 1.764 | 0.306 | 0.595 | 5.234 |
| Time∗Living condition | 1.491 | 0.484 | 0.488 | 4.559 |
Note: HR = hazard ratio.
Fig. 2.
Hazard ratio adjusted marginal means for the interaction effect between time and education. T0 and T1 correspond to the end of first (months 1–4) and second study period (months 5–8), respectively.
Fig. 3.
Kaplan-Meier estimates on time to health-care services’ use during the two study periods (months 1–4 and 5–9).
4. Discussion
The aim of this pilot study was to investigate whether a structured family nurse-led educational intervention embedded on the principles of the teach-back communication would be effective in reducing disease-related health services’ use (readmissions and/or emergency service access) among older people affected by chronic conditions. The study also aimed at identifying in the same sample, possible variables associated with the risk of health services’ use. The preliminary results look promising, as a significant reduction occurred during the intervention period compared to controls. This intervention was also effective in increasing satisfaction among the participants, and this is important since this outcome is considered a proxy measure of quality of care [32]. Moreover, we found that above and beyond the intervention itself, a higher patient education level was protective in terms of reducing the risk of using health services.
To our knowledge this is the first study attempting to investigate the effectiveness of a teach-back intervention led by FPN on patient outcomes. We believe our study had a series of “ingredients” that might have led to these positive results. Firstly, we chose trained FNP to deliver the interventions. These professionals had a family nurse certification achieved through a one-year of study and experience. As previously described, they also underwent a specific course before the study, which covered all the theory and practice of the teach-back education. It is likely that such curriculum had helped increasing the accuracy and individualization of the education plan. Second, before any education session, the FNP made use of the nursing diagnoses, which probably helped in detecting health problems and delivery tailored care plans. Not surprisingly, the use of nursing diagnoses have been associated to important patient and organizational outcomes such as quality of life, mortality and length of admissions [33]. Third, we adopted the teach-back method as a driver to implement the intervention. The effectiveness of this approach relies on a series of strategies to encourage the patients to take a more active role in their health care. In this study we planned the intervention in a way that the FNP could previously assess the educational needs before providing the sessions. In this way we achieved the “so-called” tailored education, which in addition, has revealed particularly promising for individuals with low health literacy [34]. Fourth, the topics addressed by the educational sessions were strictly focused on self-management abilities (e.g., medication adherence, recognition and management of signs and symptoms). There is strong evidence that patients who improve their self-management behaviours have also better outcomes, including lower readmissions and emergency services’ presentations [11,35,36].
This study also shows a few results which are worth commenting. Among the potential factors associated with the risk of health services’ use, we found that time and education were the only significant determinants. With regards to time, this was quite expected, because we considered this temporal variable as a proxy measure of the intervention itself. Like prior research has suggested, lower levels of education can be a risk factor for poor self-management [37]. However, not always the improvements in self-management abilities are directly attributable to improvements in education levels [38]. A study by van der Heide, Wang [39] has evidenced health literacy as a potential pathway between education level and health. This may indicate that our patients improved their health literacy via the teach-back approach, thus enhancing their self-management abilities and compensate possible deficits in education levels. Differently from time and education, the remainder factors we used in the models, namely age, gender and living condition did not turn significant. This is not consistent with was found in the literature, which highlights older age [40], female [41] and living alone [42] as predictors of health care utilization. However, our sample was small, and this may have led to concealment of possible significant relationships.
4.1. Limits and strengths
This study has a few limitations. First, its preliminary nature led to the enrolment of a small sample of patients, and this issue might have suppressed the relationship between possible predictors and the main outcome. Second, the convenience sample, which led to the exclusion of younger patients and possibly the most severe cases, does not allow generalizability of the results. Third, important outcomes such as knowledge retention and self-management abilities were not investigated; thus, the mechanisms by which the intervention exerted its effectiveness in our sample remain unknown. Finally, since this was a before after study, it was not possible to control for the different risk exposures over time for those patients who had more than one readmission within the study periods. According to the concept of immortal bias, a repeated readmission event reduces the risk exposure of the subject, which in our study has probably inflated the effectiveness of the intervention to a certain degree. However, we are confident that this bias was not important, as we only observed two of such events in our study. Despite these limitations, our preliminary findings merit consideration, as they will help for the design of future randomized control trials on the field.
Strengths of the study include (i) the pragmatic and multicentric nature, which allowed to test the effectiveness of the intervention by mimicking real primary care practice; (ii) the before after design, which reduced the effect of interindividual variability, (iv) the enrolment of highly trained nurse interventionists, who also used nursing diagnoses, and finally (v) the adoption of the teach-back method, which elicited the active involvement of the patients.
4.2. Relevance to clinical practice
Involving the family health nurse to the education of patients with chronic diseases has the potential to reduce health services’ use and therefore, the burden of the health-care systems. Patients with an education level less than 9 years have more potential to improve their health literacy via the teach-back approach, thus enhance their self-management abilities and compensate possible deficits in education levels.
5. Conclusion
This pilot study has shown that a FNP intervention based on the teach-back communication has the potential to reduce health services’ use of older adults affected by chronic conditions. However, future trials with randomized and controlled designs are needed to strengthen these results and investigate possible effects on distal outcomes, such as knowledge retention and self-management abilities.
Funding
Nothing to declare.
Data availability statement
Authors declare the absence of shared data in the present study.
CRediT authorship contribution statement
Serenella Savini: Conceptualization, Methodology, Software. Paolo Iovino: Conceptualization, Methodology, Software, Data curation, Writing – original draft, Writing – review & editing, Supervision. Dario Monaco: Conceptualization, Methodology, Software, Data curation, Validation, Writing – original draft, Writing – review & editing. Roberta Marchini: Visualization, Investigation. Tiziana Di Giovanni: Visualization, Investigation. Giuseppe Donato: Supervision. Ausilia Pulimeno: Visualization, Investigation. Carmela Matera: Visualization, Investigation. Giuseppe Quintavalle: Supervision. Carlo Turci: Data curation, Writing – original draft.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We would also like to express our gratitude to the family nurses of Local Health Authority (Roma 4) and the Centre of Excellence for Nursing Scholarship, OPI Roma Italy.
Footnotes
Peer review under responsibility of Chinese Nursing Association.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2021.05.001.
Contributor Information
Serenella Savini, Email: serenella.savini@aslroma4.it.
Paolo Iovino, Email: paolo.iovino@uniroma2.it.
Dario Monaco, Email: dario.monaco@uniroma1.it.
Roberta Marchini, Email: roberta.marchini@aslroma4.it.
Tiziana Di Giovanni, Email: tiziana.digiovanni@aslroma4.it.
Giuseppe Donato, Email: giuseppe.donato@aslroma4.it.
Ausilia Pulimeno, Email: lia.pulimeno@gmail.com.
Carmela Matera, Email: carmela.matera@aslroma4.it.
Giuseppe Quintavalle, Email: giuseppe.quintavalle@aslroma4.it.
Carlo Turci, Email: carlo.turci@aslroma4.it.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.World Health Organization Noncommunicable diseases country profiles. 2018. https://www.who.int/publications-detail-redirect/ncd-country-profiles-2018
- 2.Kim H.S., Cho J.H., Yoon K.H. New directions in chronic disease management. Endocrinol Metab (Seoul) 2015;30(2):159–166. doi: 10.3803/EnM.2015.30.2.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rubin D.J. Correction to:hospital readmission of patients with diabetes. Curr Diabetes Rep. 2018;18(4):21. doi: 10.1007/s11892-018-0989-1. [DOI] [PubMed] [Google Scholar]
- 4.Ziaeian B., Fonarow G.C. The prevention of hospital readmissions in heart failure. Prog Cardiovasc Dis. 2016;58(4):379–385. doi: 10.1016/j.pcad.2015.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kong C.W., Wilkinson T.M.A. Predicting and preventing hospital readmission for exacerbations of COPD. ERJ Open Res. 2020;6(2) doi: 10.1183/23120541.00325-2019. 00325-2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dhamane A.D., Moretz C., Zhou Y., Burslem K., Saverno K., Jain G. COPD exacerbation frequency and its association with health care resource utilization and costs. Int J Chronic Obstr Pulm Dis. 2015;10:2609–2618. doi: 10.2147/COPD.S90148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rao A., Kim D., Darzi A., Majeed A., Aylin P., Bottle A. Long-term trends of use of health service among heart failure patients. Eur Heart J Qual Care Clin Outcomes. 2018;4(3):220–231. doi: 10.1093/ehjqcco/qcy013. [DOI] [PubMed] [Google Scholar]
- 8.Barlow J., Wright C., Sheasby J., Turner A., Hainsworth J. Self-management approaches for people with chronic conditions:a review. Patient Educ Counsel. 2002;48(2):177–187. doi: 10.1016/s0738-3991(02)00032-0. [DOI] [PubMed] [Google Scholar]
- 9.Mogre V., Johnson N.A., Tzelepis F., Shaw J.E., Paul C. A systematic review of adherence to diabetes self-care behaviours: evidence from low- and middle-income countries. J Adv Nurs. 2019;75(12):3374–3389. doi: 10.1111/jan.14190. [DOI] [PubMed] [Google Scholar]
- 10.Seid M.A., Abdela O.A., Zeleke E.G. Adherence to self-care recommendations and associated factors among adult heart failure patients. From the patients' point of view. PLoS One. 2019;14(2) doi: 10.1371/journal.pone.0211768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sahebi A., Mohammad-Aliha J., Ansari-Ramandi M., Naderi N. Investigation the relationship between self-care and readmission in patients with chronic heart failure. Res Cardiovasc Med. 2015;4(1) doi: 10.5812/cardiovascmed.25472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ausili D., Bulgheroni M., Ballatore P., Specchia C., Ajdini A., Bezze S. Self-care, quality of life and clinical outcomes of type 2 diabetes patients: an observational cross-sectional study. Acta Diabetol. 2017;54(11):1001–1008. doi: 10.1007/s00592-017-1035-5. [DOI] [PubMed] [Google Scholar]
- 13.Golinowska S., Groot W., Baji P., Pavlova M. Health promotion targeting older people. BMC Health Serv Res. 2016;16(Suppl 5):345. doi: 10.1186/s12913-016-1514-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Geboers B., de Winter A.F., Spoorenberg S.L., Wynia K., Reijneveld S.A. The association between health literacy and self-management abilities in adults aged 75 and older,and its moderators. Qual Life Res. 2016;25(11):2869–2877. doi: 10.1007/s11136-016-1298-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu Y.B., Li Y.F., Liu L., Chen Y.L. Effectiveness of the teach-back method for improving the health literacy of senior citizens in nursing homes. Jpn J Nurs Sci. 2018;15(3):195–202. doi: 10.1111/jjns.12192. Epub 2017/11/20. [DOI] [PubMed] [Google Scholar]
- 16.Jager A.J., Wynia M.K. Who gets a teach-back? Patient-reported incidence of experiencing a teach-back. J Health Commun. 2012;17(Suppl 3):294–302. doi: 10.1080/10810730.2012.712624. [DOI] [PubMed] [Google Scholar]
- 17.Yen P.H., Leasure A.R. Use and effectiveness of the teach-back method in patient education and health outcomes. Fed Pract. 2019;36(6):284–289. [PMC free article] [PubMed] [Google Scholar]
- 18.Watkins L., Hall C., Kring D. Hospital to home:a transition program for frail older adults. Prof Case Manag. 2012;17(3):117–123. doi: 10.1097/NCM.0b013e318243d6a7. quiz124-5. [DOI] [PubMed] [Google Scholar]
- 19.Krist A.H., DeVoe J.E., Cheng A., Ehrlich T., Jones S.M. Redesigning primary care to address the COVID-19 pandemic in the midst of the pandemic. Ann Fam Med. 2020;18(4):349–354. doi: 10.1370/afm.2557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bell J.M. Family nursing is more than family centered care. J Fam Nurs. 2013;19(4):411–417. doi: 10.1177/1074840713512750. [DOI] [PubMed] [Google Scholar]
- 21.World Health Organization The family health nurse: context, conceptual framework and curriculum. 2000. https://www.euro.who.int/__data/assets/pdf_file/0008/98414/E92058.pdf
- 22.Des Jarlais D.C., Lyles C., Crepaz N., TREND Group Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions:the TREND statement. Am J Publ Health. 2004;94(3):361–366. doi: 10.2105/ajph.94.3.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nolte E., Knai Cc, McKee M. Managing chronic conditions: experience in eight countries: WHO regional office Europe. 2008. https://www.euro.who.int/__data/assets/pdf_file/0008/98414/E92058.pdf
- 24.Saba V. Springer Publishing Company; 2012. Clinical care classification (CCC) system version 2.5: user's guide. [Google Scholar]
- 25.Anderson K.M., Leister S., de Rego R. The 5Ts for teach back:an operational definition for teach-back training. Health Lit Res Pract. 2020;4(2):e94–e103. doi: 10.3928/24748307-20200318-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Quintana J.M., Antón-Ladislao A., Orive M., Esteban C., González N., García-Gutierrez S. Predictors of readmission at 60 days after an admission by a COPD exacerbated. Revue D'épidémiologie et De Santé Publique. 2018;66:S318. doi: 10.1016/j.respe.2018.05.211. [DOI] [Google Scholar]
- 27.Anderson K.M. Discharge clinical characteristics and 60-day readmission in patients hospitalized with heart failure. J Cardiovasc Nurs. 2014;29(3):232–241. doi: 10.1097/jcn.0b013e31828f0d25. [DOI] [PubMed] [Google Scholar]
- 28.Day R.L., Hunt H.K. Dept. of Marketing, School of Business, Indiana University; Chicago, Illinois: 1979. New dimensions of consumer satisfaction and complaining behavior: papers from the third annual conference on consumer satisfaction, dissatisfaction and complaining behavior. October 5-7, 1978. [Google Scholar]
- 29.Cohen J. Academic press; 2013. Statistical power analysis for the behavioral sciences. [Google Scholar]
- 30.Rodríguez G. Stata tutorial. 2011. https://data.princeton.edu/stata/
- 31.World Medical Association World Medical Association Declaration of Helsinki:ethical principles for medical research involving human subjects. J Am Med Assoc. 2013;310(20):2191–2194. doi: 10.1001/jama.2013.281053. [DOI] [PubMed] [Google Scholar]
- 32.Karaca A., Durna Z. Patient satisfaction with the quality of nursing care. Nurs Open. 2019;6(2):535–545. doi: 10.1002/nop2.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sanson G., Vellone E., Kangasniemi M., Alvaro R., D'Agostino F. Impact of nursing diagnoses on patient and organisational outcomes: a systematic literature review. J Clin Nurs. 2017;26(23–24):3764–3783. doi: 10.1111/jocn.13717. Epub 2017/02/23. [DOI] [PubMed] [Google Scholar]
- 34.Schapira M.M., Swartz S., Ganschow P.S., Jacobs E.A., Neuner J.M., Walker C.M. Tailoring educational and behavioral interventions to level of health literacy:A systematic review. MDM Policy Pract. 2017;2(1) doi: 10.1177/2381468317714474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.De Vito C., D'Addario M., Di Lascio A., Villari P., Damiani G. Are self-management interventions effective in reducing hospital readmissions in patients with heart failure? Results of a systematic review and meta-analysis Corrado De Vito. Eur J Publ Health. 2013;23(suppl 1) doi: 10.1093/eurpub/ckt126.037. ckt126.037. [DOI] [Google Scholar]
- 36.Zwerink M., Brusse-Keizer M., van der Valk P.D., Zielhuis G.A., Monninkhof E.M., van der Palen J. Self management for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2014;3 doi: 10.1002/14651858.CD002990.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Baji Z., Zamani A.F., Nouhjah S., Haghighizadeh M.H. Self-care behaviors and related factors in women with type 2 diabetes. Iran J Endocrinol Metab. 2015;16(6):303–401. [Google Scholar]
- 38.Gonzalez B., Lupon J., Domingo Mdel M., Cano L., Cabanes R., de Antonio M. Educational level and self-care behaviour in patients with heart failure before and after nurse educational intervention. Eur J Cardiovasc Nurs. 2014;13(5):459–465. doi: 10.1177/1474515113510810. [DOI] [PubMed] [Google Scholar]
- 39.van der Heide I., Wang J., Droomers M., Spreeuwenberg P., Rademakers J., Uiters E. The relationship between health,education,and health literacy:results from the Dutch Adult Literacy and Life Skills Survey. J Health Commun. 2013;18(Suppl 1):172–184. doi: 10.1080/10810730.2013.825668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Li C.L., Stanaway F.F., Lin J.D., Chang H.Y. Frailty and health care use among community-dwelling older adults with diabetes:a population-based study. Clin Interv Aging. 2018;13:2295–2300. doi: 10.2147/CIA.S183681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cameron K.A., Song J., Manheim L.M., Dunlop D.D. Gender disparities in health and healthcare use among older adults. J Wom Health. 2010;19(9):1643–1650. doi: 10.1089/jwh.2009.1701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dreyer K., Steventon A., Fisher R., Deeny S.R. The association between living alone and health care utilisation in older adults:a retrospective cohort study of electronic health records from a London general practice. BMC Geriatr. 2018;18(1):269. doi: 10.1186/s12877-018-0939-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Authors declare the absence of shared data in the present study.